Central Precocious Puberty in Boys and Girls: Similarities and Differences
Abstract
1. Introduction
2. Epidemiology
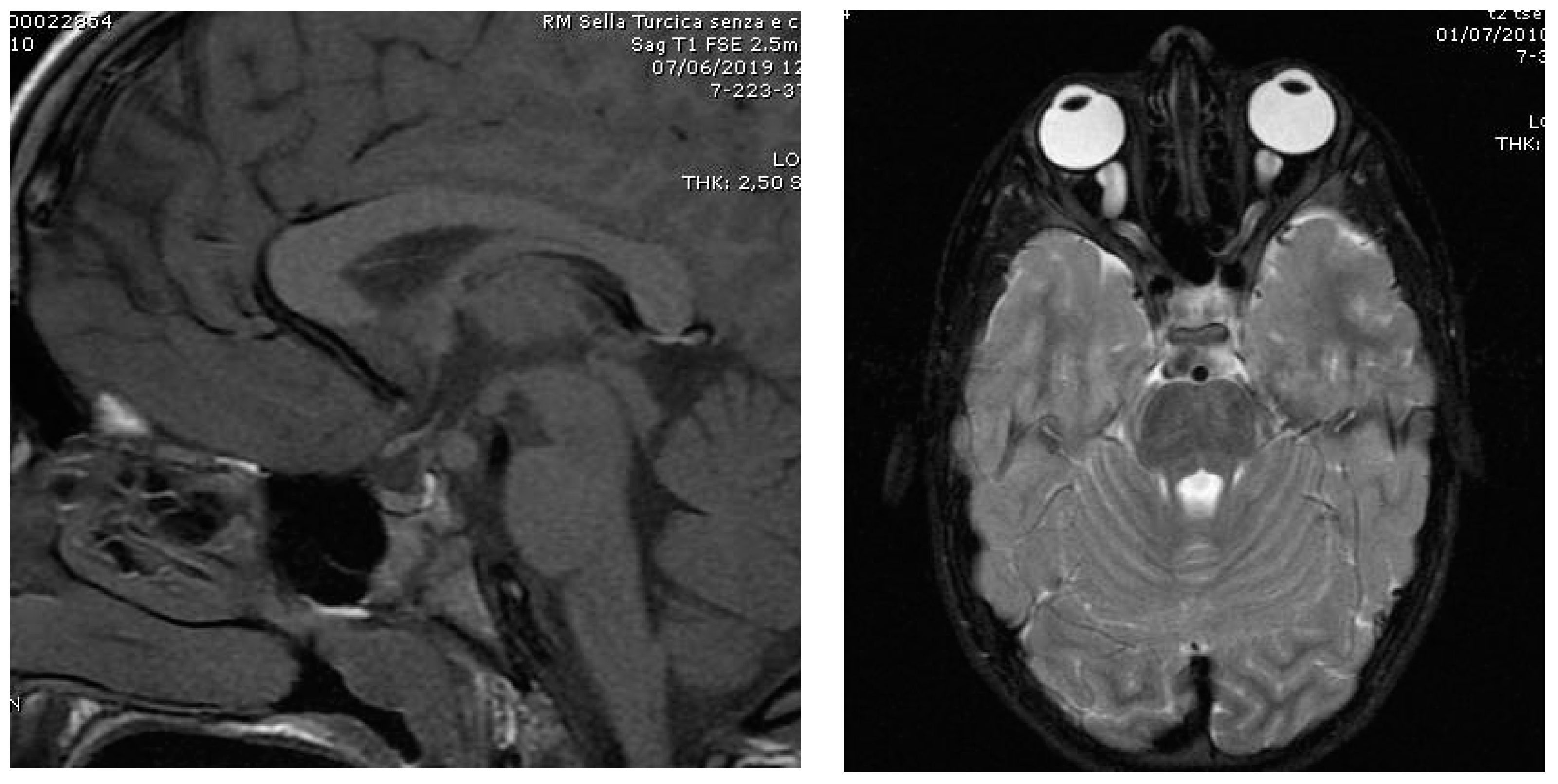
3. Etiology
| Author | Year | Country | N * | Organic/Idiopathic (%) | F:M Ratio | |
|---|---|---|---|---|---|---|
| Boys | Girls | |||||
| Thamdrup [18] | 1961 | Netherland | 56 | 64/36 | 24/76 | 4.1:1 |
| UCSF ° [19] | 1981 | USA | 205 | 67/33 | 27/73 | 4.2:1 |
| Bridges et al. [20] | 1994 | UK | 95 | 100/- | 6/94 | 23.0:1 |
| ISGPP ^ [21,22] | 2000 | Italy | 473 | 40/60 | 18/82 | 9.5:1 |
| Chemaitilly et al. [23] | 2001 | France | 256 | 73/27 | 19/81 | 8.8:1 |
| Klein et al. [24] | 2001 | USA | 98 | 83/17 | 32/68 | 4.4:1 |
| Lee et al. [25] | 2011 | USA | 54 | — | — | 9.8:1 |
| Jaruratanasirikul et al. [26] | 2011 | Thailand | 73 | 100/- | 15/85 | 13.6:1 |
| Soriano-Guillén et al. [6] | 2010 | Spain | 250 | 33/67 | 11/89 | 9.4:1 |
| Alikasifoglu et al. [12] | 2015 | Turkey | 100 | 26/74 | — | — |
| Lee et al. [13] | 2018 | Korea | 71 | 38/62 | — | — |
| Yoon et al. [14] | 2018 | Korea | 138 | 6/132 | — | — |
| Choi et al. [15] | 2013 | Korea | 23 | 6/17 | — | — |
| Topor et al. [16] | 2018 | USA | 50 | 64/36 | — | — |
| Harbulot et al. [17] | 2021 | France | 395 | 60/40 | 12/88 | 10.6:1 |
4. Clinical Presentation
5. Laboratory Assessment
| Author | Method | LH (IU/L) | |||
|---|---|---|---|---|---|
| Girls | Boys | ||||
| B | P | B | P | ||
| Brito et al. [41] | IFMA | 0.6 | 6.9 | 0.6 | 9.6 |
| Lee et al. [42] | IRMA | 1.1 | 5 | — | — |
| Neely et al. [43] | ICMA | 0.15 | 5 | 0.15 | 5 |
| Pasternak et al. [44] | ICMA | 0.1 | 4.9 | — | — |
| Resende et al. [45] | IFMA | 0.6 | 4.2 | 0.6 | 3.3 |
| ICMA | 0.1 | 3.3 | 0.3 | 4.1 | |
| Wankanit et al. [46] | CMIA | 0.2 | 5.0 * | — | — |
6. Clinical Consequences of Untreated CPP
| Author | Year | Adult Height, Males | Adult Height, Females | ||||
|---|---|---|---|---|---|---|---|
| n | cm | SDS a | n | cm | SDS a | ||
| Thamdrup [18] | 1961 | 8 | 155.4 ± 8.3 | −2.9 | 26 | 151.3 ± 8.8 | −1.8 |
| Sigurjonsdottir et al. [47] | 1968 | 11 | 156.0 ± 7.3 | −2.8 | 40 | 152.7 ± 8.0 | −1.6 |
| Bovier-Lapierre et al. [48] | 1972 | 5 | 155.8 ± 2.8 | −2.8 | 4 | 150.5 ± 1.6 | −1.9 |
| Paul et al. [49] | 1995 | 4 | 159.6 ± 8.7 | −3.7 b | 8 | 153.8 ± 6.8 | −2.4 |
| Pisa [50] | 2008 | 4 | 156.0 ± 4.7 | −2.8 | 7 | 151.4 ± 4.7 | −1.8 |
| Swaiss et al. [51] | 2017 | 2 | 149.0 ± 12.7 | −3.9 | 11 | 151.2 ± 8.4 | −1.8 |
7. Therapy
| Triptorelin, 3.75 mg | Leuprorelin, 3.75 mg | ||||||
|---|---|---|---|---|---|---|---|
| Authors | AH | AH-PH | AH-TH | Authors | AH | AH-PH | AH-TH |
| cm | cm | ||||||
| Adan et al. [59] | 159.5 ± 5.3 | 3.5 | −1.7 | Brito et al. [60] | 155.3 ± 6.9 | −5.3 | −2.2 |
| Arrigo et al. [61] | 158.4 ± 5.8 | 2.9 | −2.9 | Cho et al. [62] | 161.5 ± 4.6 | 8.4 | 2.2 |
| Carel et al. [63] | 161.1 ± 5.9 | 4.7 | 1.0 | Lee et al. [25] | 160.1 ± 5.0 | 4.0 | 0.8 |
| Faienza et al. [64] | 160.6 ± 3.4 | 2.2 | −0.2 | Tanaka et al. [65] | 154.5 ± 5.7 | −0.4 | −0.4 |
| Heger et al. [66] | 160.6 ± 8.0 | 5.7 | −2.0 | Vuralli et al. [67] * | −0.6 ± 0.8 a | 2.0 | 0.6 |
| Kauli et al. [68] | 159.6 ± 6.3 | 2.7 | 1.9 | −0.7 ± 0.9 b | 1.0 | 0.2 | |
| Pasquino et al. [69] | 159.8 ± 5.3 | 9.5 | 2.4 | −1.0 ± 0.7 c | 0.6 | −0.5 | |
| Authors | GnRH Analog (Dose) | AH | AH-PH | AH-TH |
|---|---|---|---|---|
| cm | ||||
| Klein et al. [24] | Deslorelin (4 mg/kg/day) | 171.1 ± 8.7 | 15.0 | −7.2 |
| Mul et al. [70] | Triptorelin (3.75 mg/28 days) | 172.9 ± 6.6 | 6.2 | −2.2 |
| Shim et al. [71] | Leuprorelin or triptorelin (3.75 µg/28 days) | 173.4 ± 5.8 | 3.3 | 2.5 |
| Tanaka et al. [65] | Leuprorelin (10–90 µg/28 days) | 163.2 ± 13.0 | 1.1 | −4.4 |
8. Short- and Long-Term Safety
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brito, V.N.; Spinola-Castro, A.M.; Kochi, C.; Kopacek, C.; Da Silva, P.C.A.; Guerra-Júnior, G. Central precocious puberty: Revisiting the diagnosis and therapeutic management. Arch. Endocrinol. Metab. 2016, 60, 163–172. [Google Scholar] [CrossRef]
- Latronico, A.C.; Brito, V.N.; Carel, J.-C. Causes, diagnosis, and treatment of central precocious puberty. Lancet Diabetes Endocrinol. 2016, 4, 265–274. [Google Scholar] [CrossRef]
- Bertelloni, S.; I Baroncelli, G. Current pharmacotherapy of central precocious puberty by GnRH analogs: Certainties and uncertainties. Expert Opin. Pharmacother. 2013, 14, 1627–1639. [Google Scholar] [CrossRef]
- Gonzales, E.R. For puberty that comes too soon, new treatment highly effective. J. Am. Med. Assoc. 1982, 248, 1149–1152. [Google Scholar] [CrossRef]
- Teilmann, G. Prevalence and incidence of precocious pubertal development in Denmark: An epidemiologic study based on national registries. Pediatrics 2005, 116, 1323–1328. [Google Scholar] [CrossRef]
- Soriano-Guillén, L.; Corripio, R.; Labarta, J.I.; Cañete, R.; Castro-Feijóo, L.; Espino, R.; Argente, J. Central precocious puberty in children living in Spain: Incidence, prevalence, and influence of adoption and immigration. J. Clin. Endocrinol. Metab. 2010, 95, 4305–4313. [Google Scholar] [CrossRef]
- Le Moal, J.; Rigou, A.; Le Tertre, A.; De Crouy-Channel, P.; Léger, J.; Carel, J.-C. Marked geographic patterns in the incidence of idiopathic central precocious puberty: A nationwide study in France. Eur. J. Endocrinol. 2018, 178, 33–41. [Google Scholar] [CrossRef]
- Kim, S.H.; Huh, K.; Won, S.; Lee, K.-W.; Park, M.-J. A significant increase in the incidence of central precocious puberty among Korean girls from 2004 to 2010. PLoS ONE 2015, 10, e0141844. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Kwon, A.; Jung, M.K.; Kim, K.E.; Suh, J.; Chae, H.W.; Kim, D.H.; Ha, S.; Seo, G.H.; Kim, H.-S. Incidence and prevalence of central precocious puberty in Korea: An epidemiologic study based on a national database. J. Pediatr. 2019, 208, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Stagi, S.; De Masi, S.; Bencini, E.; Losi, S.; Paci, S.; Parpagnoli, M.; Ricci, F.; Ciofi, D.; Azzari, C. Increased incidence of precocious and accelerated puberty in females during and after the Italian lockdown for the coronavirus 2019 (COVID-19) pandemic. Ital. J. Pediatr. 2020, 46, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wannes, S.; Elmaleh-Bergès, M.; Simon, D.; Zénaty, D.; Martinerie, L.; Storey, C.; Gelwane, G.; Paulsen, A.; Ecosse, E.; De Roux, N.; et al. High prevalence of syndromic disorders in patients with non-isolated central precocious puberty. Eur. J. Endocrinol. 2018, 179, 373–380. [Google Scholar] [CrossRef]
- Alikasifoglu, A.; Vuralli, D.; Gonc, E.N.; Ozon, A.; Kandemir, N. Changing etiological trends in male precocious puberty: Evaluation of 100 cases with central precocious puberty over the last decade. Horm. Res. Paediatr. 2015, 83, 340–344. [Google Scholar] [CrossRef]
- Lee, J.; Kim, J.; Yang, A.; Cho, S.Y.; Jin, D.-K. Etiological trends in male central precocious puberty. Ann. Pediatr. Endocrinol. Metab. 2018, 23, 75–80. [Google Scholar] [CrossRef]
- Yoon, J.S.; So, C.H.; Lee, H.S.; Lim, J.S.; Hwang, J.S. The prevalence of brain abnormalities in boys with central precocious puberty may be overestimated. PLoS ONE 2018, 13, e0195209. [Google Scholar] [CrossRef]
- Choi, K.H.; Chung, S.J.; Kang, M.J.; Yoon, J.Y.; Lee, J.E.; Lee, Y.A.; Shin, C.H.; Yang, S.W. Boys with precocious or early puberty: Incidence of pathological brain magnetic resonance imaging findings and factors related to newly developed brain lesions. Ann. Pediatr. Endocrinol. Metab. 2013, 18, 183–190. [Google Scholar] [CrossRef]
- Topor, L.S.; Bowerman, K.; Machan, J.T.; Gilbert, C.L.; Kangarloo, T.; Shaw, N.D. Central precocious puberty in Boston boys: A 10-year single center experience. PLoS ONE 2018, 13, e0199019. [Google Scholar] [CrossRef]
- Harbulot, C.; Lessim, S.; Simon, D.; Martinerie, L.; Storey, C.; Ecosse, E.; De Roux, N.; Carel, J.-C.; Léger, J. Prevalence and clinical characteristics of isolated forms of central precocious puberty: A cohort study at a single academic center. Eur. J. Endocrinol. 2021, 184, 243–251. [Google Scholar] [CrossRef]
- Thamdrup, E. Precocious sexual development: A clinical study of one hundred children. Dan. Med. Bull. 1961, 8, 104–105. [Google Scholar]
- Grumbach, M.M.; Styne, D.M. Puberty: Ontogeny, neuroendocrinology, physiology, and disorders. In Williams Textbook of Endocrinology, 9th ed.; Saunders W.B.: Philadelphia, PA, USA, 1998; pp. 1509–1625. [Google Scholar]
- Bridges, N.A.; Christopher, J.A.; Hindmarsh, P.C.; Brook, C.G. Sexual precocity: Sex incidence and aetiology. Arch. Dis. Child. 1994, 70, 116–118. [Google Scholar] [CrossRef]
- Cisternino, M.; Arrigo, T.; Pasquino, A.; Tinelli, C.; Antoniazzi, F.; Beduschi, L.; Bindi, G.; Borrelli, P.; De Sanctis, V.; Farello, G.; et al. Etiology and age incidence of precocious puberty in girls: A multicentric study. J. Pediatr. Endocrinol. Metab. 2000, 13, 695–701. [Google Scholar] [CrossRef]
- De Sanctis, V.; Corrias, A.; Rizzo, V.; Bertelloni, S.; Urso, L.; Galluzzi, F.; Pasquino, A.; Pozzan, G.; Guarneri, M.; Cisternino, M.; et al. Etiology of central precocious puberty in males: The results of the Italian study group for physiopathology of puberty. J. Pediatr. Endocrinol. Metab. 2000, 13, 687–694. [Google Scholar] [CrossRef]
- Chemaitilly, W.; Trivin, C.; Adan, L.; Gall, V.; Sainte-Rose, C.; Brauner, R. Central precocious puberty: Clinical and laboratory features. Clin. Endocrinol. 2001, 54, 289–294. [Google Scholar] [CrossRef]
- Klein, K.O.; Barnes, K.M.; Jones, J.V.; Feuillan, P.P.; Cutler, G.B.C., Jr. Increased final height in precocious puberty after long-term treatment with LHRH agonists: The national institutes of health experience. J. Clin. Endocrinol. Metab. 2001, 86, 4711–4716. [Google Scholar] [CrossRef]
- Lee, P.A.; Neely, E.K.; Fuqua, J.; Yang, D.; Larsen, L.M.; Mattia-Goldberg, C.; Chwalisz, K. Efficacy of leuprolide acetate 1-month depot for central precocious puberty (CPP): Growth outcomes during a prospective, longitudinal study. Int. J. Pediatr. Endocrinol. 2011, 2011, 7. [Google Scholar] [CrossRef] [PubMed]
- Jaruratanasirikul, S.; Thaiwong, M. Outcome of gonadotropin-releasing analog treatment for children with central precocious puberty: 15-year experience in Southern Thailand. J. Pediatr. Endocrinol. Metab. 2011, 24, 519–523. [Google Scholar] [CrossRef]
- Carel, J.-C.; Eugster, E.A.; Rogol, A.; Ghizzoni, L.; Palmert, M.R. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics 2009, 123, e752–e762. [Google Scholar] [CrossRef]
- Pedicelli, S.; Alessio, P.; Scirè, G.; Cappa, M.; Cianfarani, S. Routine screening by brain magnetic resonance imaging is not indicated in every girl with onset of puberty between the ages of 6 and 8 years. J. Clin. Endocrinol. Metab. 2014, 99, 4455–4461. [Google Scholar] [CrossRef]
- Cantas-Orsdemir, S.; Garb, J.L.; Allen, H.F. Prevalence of cranial MRI findings in girls with central precocious puberty: A systematic review and meta-analysis. J. Pediatr. Endocrinol. Metab. 2018, 31, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Burcher, G.C.; Liang, H.; Lancaster, R.; Cross, J.H.; Tisdall, M.; Varadkar, S.; Spoudeas, H.A.; Caredda, E.; Bennett, S.; Heyman, I. Neuropsychiatric profile of pediatric hypothalamic hamartoma: Systematic review and case series. Dev. Med. Child Neurol. 2019, 61, 1377–1385. [Google Scholar] [CrossRef]
- Harrison, V.S.; Oatman, O.; Kerrigan, J.F. Hypothalamic hamartoma with epilepsy: Review of endocrine comorbidity. Epilepsia 2017, 58, 50–59. [Google Scholar] [CrossRef]
- Virdis, R.; Sigorini, M.; Laiolo, A.; Lorenzetti, E.; Street, M.; Villani, A.; Donadio, A.; Pisani, F.; Terzi, C.; Garavelli, L. Neurofibromatosis Type 1 and precocious puberty. J. Pediatr. Endocrinol. Metab. 2000, 13, 841–844. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, R.S.; Eugster, E.A. Central precocious puberty: From genetics to treatment. Best Pract. Res. Clin. Endocrinol. Metab. 2018, 32, 343–354. [Google Scholar] [CrossRef] [PubMed]
- Bessa, D.S.; Macedo, D.B.; Brito, V.N.; França, M.M.; Montenegro, L.R.; Cunha-Silva, M.; Silveira, L.G.; Hummel, T.; Bergadá, I.; Braslavsky, D.; et al. High frequency of MKRN3 mutations in male central precocious puberty previously classified as idiopathic. Neuroendocrinology 2017, 105, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Macedo, D.B.; Brito, V.N.; Latronico, A.C. New causes of central precocious puberty: The role of genetic factors. Neuroendocrinology 2014, 100, 1–8. [Google Scholar] [CrossRef]
- Abreu, A.P.; Dauber, A.; Macedo, D.B.; Noel, S.D.; Brito, V.N.; Gill, J.C.; Cukier, P.; Thompson, I.R.; Navarro, V.M.; Gagliardi, P.C.; et al. Central precocious puberty caused by mutations in the imprinted gene MKRN. N. Engl. J. Med. 2013, 368, 2467–2475. [Google Scholar] [CrossRef]
- Grandone, A.; Capristo, C.; Cirillo, G.; Sasso, M.; Umano, G.R.; Mariani, M.; Del Giudice, E.M.; Perrone, L. Molecular screening of MKRN3, DLK1, and KCNK9 genes in girls with idiopathic central precocious puberty. Horm. Res. Paediatr. 2017, 88, 194–200. [Google Scholar] [CrossRef]
- Simon, D.; Ba, I.; Mekhail, N.; Ecosse, E.; Paulsen, A.; Zenaty, D.; Houang, M.; Perelroizen, M.J.; De Filippo, G.-P.; Salerno, M.; et al. Mutations in the maternally imprinted gene MKRN3 are common in familial central precocious puberty. Eur. J. Endocrinol. 2016, 174, 1–8. [Google Scholar] [CrossRef]
- Brito, V.N.; Latronico, A.C.; Arnhold, I.J.P.; Mendonça, B.B. Update on the etiology, diagnosis and therapeutic management of sexual precocity. Braz. Soc. Endocrinol. Metab. 2008, 52, 18–31. [Google Scholar] [CrossRef]
- Ab Rahim, S.N.; Omar, J.; Ismail, T.S.T. Gonadotropin-releasing hormone stimulation test and diagnostic cutoff in precocious puberty: A mini review. Ann. Pediatr. Endocrinol. Metab. 2020, 25, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Brito, V.N.; Batista, M.C.; Borges, M.F.; Latronico, A.C.; Kohek, M.B.F.; Thirone, A.C.P.; Jorge, B.H.; Arnhold, I.J.P.; Mendonca, B.B. Diagnostic value of fluorometric assays in the evaluation of precocious puberty. J. Clin. Endocrinol. Metab. 1999, 84, 3539–3544. [Google Scholar] [CrossRef][Green Version]
- Resende, E.A.M.R.; Lara, B.H.J.; Reis, J.D.; Ferreira, B.P.; Pereira, G.A.; Borges, M.F. Assessment of basal and gonadotropin-releasing hormone-stimulated gonadotropins by immunochemiluminometric and immunofluorometric assays in normal children. J. Clin. Endocrinol. Metab. 2007, 92, 1424–1429. [Google Scholar] [CrossRef] [PubMed]
- Wankanit, S.; Mahachoklertwattana, P.; Pattanaprateep, O.; Poomthavorn, P. Basal serum luteinising hormone cut-off, and its utility and cost-effectiveness for aiding the diagnosis of the onset of puberty in girls with early stages of breast development. Clin. Endocrinol. 2020, 92, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Park, H.K.; Ko, J.H.; Kim, Y.J.; Hwang, J.S. Utility of basal luteinizing hormone levels for detecting central precocious puberty in girls. Horm. Metab. Res. 2012, 44, 851–854. [Google Scholar] [CrossRef] [PubMed]
- Neely, E.; Hintz, R.L.; Wilson, D.M.; Lee, P.A.; Gautier, T.; Argente, J.; Stene, M. Normal ranges for immunochemiluminometric gonadotropin assays. J. Pediatr. 1995, 127, 40–46. [Google Scholar] [CrossRef]
- Pasternak, Y.; Friger, M.; Loewenthal, N.; Haim, A.; Hershkovitz, E. The utility of basal serum LH in prediction of central precocious puberty in girls. Eur. J. Endocrinol. 2012, 166, 295–299. [Google Scholar] [CrossRef]
- Sigurjonsdottir, T.J.; Hayles, A.B. Precocious puberty. A report of 96 cases. Am. J. Dis. Child. 1968, 115, 309. [Google Scholar] [CrossRef]
- Bovier-Lapierre, M.; Sempé, M.; David, M. Etiological, clinical and biological aspects of precocious puberty of central origin. Pediatrie 1972, 27, 587–609. [Google Scholar]
- Paul, D.; Conte, F.A.; Grumbach, M.M.; Kaplan, S.L. Long-term effect of gonadotropin-releasing hormone agonist therapy on final and near-final height in 26 children with true precocious puberty treated at a median age of less than 5 years. J. Clin. Endocrinol. Metab. 1995, 80, 546–551. [Google Scholar] [CrossRef][Green Version]
- Bertelloni, S.; Mul, D. Treatment of central precocious puberty by GnRH analogs: Long-term outcome in men. Asian J. Androl. 2008, 10, 525–534. [Google Scholar] [CrossRef]
- Swaiss, H.H.; Khawaja, N.M.; Farahid, O.H.; Batieha, A.M.; Ajlouni, K.M. Effect of gonadotropin-releasing hormone analogue on final adult height among Jordanian children with precocious puberty. Saudi Med. J. 2017, 38, 1101–1107. [Google Scholar] [CrossRef]
- Tanner, J.M.; Whitehouse, R.H. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch. Dis. Child. 1976, 51, 170–179. [Google Scholar] [CrossRef]
- Wojniusz, S.; Callens, N.; Sütterlin, S.; Andersson, S.; De Schepper, J.; Gies, I.; Vanbesien, J.; De Waele, K.; Van Aken, S.; Craen, M.; et al. Cognitive, emotional, and psychosocial functioning of girls treated with pharmacological puberty blockage for idiopathic central precocious puberty. Front. Psychol. 2016, 7, 1053. [Google Scholar] [CrossRef]
- Lahlou, N.; Carel, J.-C.; Chaussain, J.-L.; Roger, M. Pharmacokinetics and pharmacodynamics of GnRH agonists: Clinical implications in pediatrics. J. Pediatr. Endocrinol. Metab. 2000, 13, 723–738. [Google Scholar] [CrossRef] [PubMed]
- Bertelloni, S.; Mucaria, C.; Baroncelli, G.I.; Peroni, D. Triptorelin depot for the treatment of children 2 years and older with central precocious puberty. Expert Rev. Clin. Pharmacol. 2018, 11, 659–667. [Google Scholar] [CrossRef]
- Bereket, A. A critical appraisal of the effect of gonadotropin-releasing hormon analog treatment on adult height of girls with central precocious puberty. J. Clin. Res. Pediatr. Endocrinol. 2018, 9, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Durand, A.; Tauber, M.; Patel, B.; Dutailly, P. Meta-Analysis of paediatric patients with central precocious puberty treated with intramuscular triptorelin 11.25 mg 3-month prolonged-release formulation. Horm. Res. Paediatr. 2017, 87, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Klein, K.; Freire, A.; Gryngarten, M.G.; Kletter, G.B.; Benson, M.; Miller, B.S.; Dajani, T.S.; A Eugster, E.; Mauras, N. Phase 3 trial of a small-volume subcutaneous 6-month duration leuprolide acetate treatment for central precocious puberty. J. Clin. Endocrinol. Metab. 2020, 105, e3660–e3671. [Google Scholar] [CrossRef]
- Adan, L.; Chemaitilly, W.; Trivin, C.; Brauner, R. Factors predicting adult height in girls with idiopathic central precocious puberty: Implications for treatment. Clin. Endocrinol. 2002, 56, 297–302. [Google Scholar] [CrossRef]
- Brito, V.N.; Latronico, A.C.; Cukier, P.; Teles, M.G.; Silveira, L.F.G.; Arnhold, I.J.P.; Mendonca, B.B. Factors determining normal adult height in girls with gonadotropin-dependent precocious puberty treated with depot gonadotropin-releasing hormone analogs. J. Clin. Endocrinol. Metab. 2008, 93, 2662–2669. [Google Scholar] [CrossRef]
- Arrigo, T.; Cisternino, M.; Galluzzi, F.; Bertelloni, S.; Pasquino, A.M.; Antoniazzi, F.; Borrelli, P.; Crisafulli, G.; Wasniewska, M.; De Luca, F. Analysis of the factors affecting auxological response to GnRH agonist treatment and final height outcome in girls with idiopathic central precocious puberty. Eur. J. Endocrinol. 1999, 141, 140–144. [Google Scholar] [CrossRef]
- Cho, A.Y.; Ko, S.Y.; Lee, J.H.; Kim, E.Y. Relationship between final adult height and birth weight after gonadotropin-releasing hormone agonist treatment in girls with central precocious puberty. Ann. Pediatr. Endocrinol. Metab. 2020, 25, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Carel, J.-C.; Roger, M.; Ispas, S.; Tondu, F.; Lahlou, N.; Blumberg, J.; Chaussain, J.-L. Final height after long-term treatment with triptorelin slow release for central precocious puberty: Importance of statural growth after interruption of treatment. J. Clin. Endocrinol. Metab. 1999, 84, 1973–1978. [Google Scholar] [CrossRef] [PubMed]
- Faienza, M.F.; Brunetti, G.; Acquafredda, A.; DelVecchio, M.; Lonero, A.; Gaeta, A.; Bulzis, P.S.; Corica, D.; Velletri, M.R.; De Luca, F.; et al. Metabolic outcomes, bone health, and risk of polycystic ovary syndrome in girls with idiopathic central precocious puberty treated with gonadotropin-releasing hormone analogues. Horm. Res. Paediatr. 2017, 87, 162–169. [Google Scholar] [CrossRef]
- Tanaka, T.; Niimi, H.; Matsuo, N.; Fujieda, K.; Tachibana, K.; Ohyama, K.; Satoh, M.; Kugu, K. Results of long-term follow-up after treatment of central precocious puberty with leuprorelin acetate: Evaluation of effectiveness of treatment and recovery of gonadal function. The TAP-144-SR japanese study group on central precocious puberty. J. Clin. Endocrinol. Metab. 2005, 90, 1371–1376. [Google Scholar] [CrossRef]
- Heger, S.; Partsch, C.-J.; Sippell, W.G. Long-term outcome after depot gonadotropin-releasing hormone agonist treatment of central precocious puberty: Final height, body proportions, body composition, bone mineral density, and reproductive function. J. Clin. Endocrinol. Metab. 1999, 84, 4583–4590. [Google Scholar] [CrossRef][Green Version]
- Vuralli, D.; Gonc, N.E.; Ozon, Z.A.; Kandemir, N.; Alikasifoglu, A. Which parameters predict the beneficial effect of GnRHa treatment on height in girls with central precocious puberty? Clin. Endocrinol. 2021. [Google Scholar] [CrossRef]
- Kauli, R.; Galatzer, A.; Kornreich, L.; Lazar, L.; Pertzelan, A.; Laron, Z. Final height of girls with central precocious puberty, untreated versus treated with cyproterone acetate or GnRH analogue. Horm. Res. 1997, 47, 54–61. [Google Scholar] [CrossRef]
- Pasquino, A.M.; Pucarelli, I.; Accardo, F.; Demiraj, V.; Segni, M.; Di Nardo, R. Long-Term observation of 87 girls with idiopathic central precocious puberty treated with gonadotropin-releasing hormone analogs: Impact on adult height, body mass index, bone mineral content, and reproductive function. J. Clin. Endocrinol. Metab. 2008, 93, 190–195. [Google Scholar] [CrossRef]
- Mul, D.; Bertelloni, S.; Carel, J.-C.; Saggese, G.; Chaussain, J.; Oostdijk, W. Effect of gonadotropin-releasing hormone agonist treatment in boys with central precocious puberty: Final height results. Horm. Res. 2002, 58, 1–7. [Google Scholar] [CrossRef]
- Shim, Y.S.; Lim, K.I.; Lee, H.S.; Hwang, J.S. Long-term outcomes after gonadotropin-releasing hormone agonist treatment in boys with central precocious puberty. PLoS ONE 2020, 15, e0243212. [Google Scholar] [CrossRef]
- Vincenzo, D.S.; Ashraf, T.S.; Salvatore, D.M.; Nada, S.; Heba, E.; De Sanctis, V.; Soliman, A.T.; Di Maio, S.; Soliman, N.; Elsedfy, H. Long-term effects and significant adverse drug reactions (ADRs) associated with the use of gonadotropin-releasing hormone analogs (GnRHa) for central precocious puberty: A brief review of literature. Acta Biomed. 2019, 90, 345–359. [Google Scholar]
- Manasco, P.K.; Pescovitz, O.H.; Feuillan, P.P.; Hench, K.D.; Barnes, K.M.; Jones, J.; Hill, S.C.; Loriaux, D.L.; Cutler, G.B. Resumption of puberty after long term luteinizing hormone-releasing hormone agonist treatment of central precocious puberty. J. Clin. Endocrinol. Metab. 1988, 67, 368–372. [Google Scholar] [CrossRef]
- Magiakou, M.A.; Manousaki, D.; Papadaki, M.; Hadjidakis, D.; Levidou, G.; Vakaki, M.; Papaefstathiou, A.; Lalioti, N.; Kanaka-Gantenbein, C.; Piaditis, G.; et al. The efficacy and safety of gonadotropin-releasing hormone analog treatment in childhood and adolescence: A single center, long-term follow-up study. J. Clin. Endocrinol. Metab. 2010, 95, 109–117. [Google Scholar] [CrossRef]
- Chiavaroli, V.; Liberati, M.; D’Antonio, F.; Masuccio, F.; Capanna, R.; Verrotti, A.; Chiarelli, F.; Mohn, A. GNRH analog therapy in girls with early puberty is associated with the achievement of predicted final height but also with increased risk of polycystic ovary syndrome. Eur. J. Endocrinol. 2010, 163, 55–62. [Google Scholar] [CrossRef]
- Ramos, C.O.; Latronico, A.C.; Cukier, P.; Macedo, D.B.; Bessa, D.S.; Cunha-Silva, M.; Arnhold, I.J.; Mendonca, B.B.; Brito, V.N. Long-Term outcomes of patients with central precocious puberty due to hypothalamic hamartoma after GnRHa treatment: Anthropometric, metabolic, and reproductive aspects. Neuroendocrinology 2018, 106, 203–210. [Google Scholar] [CrossRef]
- Grinspon, R.P.; Andreone, L.; Bedecarrás, P.; Ropelato, M.G.; Rey, R.A.; Campo, S.M.; Bergadá, I. Male central precocious puberty: Serum profile of anti-müllerian hormone and inhibin B before, during, and after treatment with GnRH analogue. Int. J. Endocrinol. 2013, 2013, 823064. [Google Scholar] [CrossRef]
- Nam, H.-K.; Kim, H.R.; Rhie, Y.-J.; Lee, K.-H. Serum anti-müllerian hormone levels in precocious puberty girls according to stage of GnRH agonist treatment. J. Korean Med. Sci. 2017, 32, 475–479. [Google Scholar] [CrossRef]
- Luo, X.; Liang, Y.; Hou, L.; Wu, W.; Ying, Y.; Ye, F. Long-term efficacy and safety of gonadotropin-releasing hormone analog treatment in children with idiopathic central precocious puberty: A systematic review and meta-analysis. Clin. Endocrinol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Şahin, N.M.; Dikmen, A.U.; Çetinkaya, S.; Aycan, Z. Subnormal growth velocity and related factors during GnRH analog therapy for idiopathic central precocious puberty. J. Clin. Res. Pediatr. Endocrinol. 2018, 10, 239–246. [Google Scholar] [CrossRef]
- Pasquino, A.M.; Pucarelli, I.; Segni, M.; Matrunola, M.; Cerrone, F. Adult height in girls with central precocious puberty treated with gonadotropin-releasing hormone analogues and growth hormone. J. Clin. Endocrinol. Metab. 1999, 84, 449–452. [Google Scholar] [CrossRef]
- Liu, S.; Liu, Q.; Cheng, X.; Luo, Y.; Wen, Y. Effects and safety of combination therapy with gonadotropin-releasing hormone analogue and growth hormone in girls with idiopathic central precocious puberty: A meta-analysis. J. Endocrinol. Investig. 2016, 39, 1167–1178. [Google Scholar] [CrossRef] [PubMed]
- Gu, Q.; Luo, Y.; Ye, J.; Shen, X. Comparative efficacy and safety of three current clinical treatments for girls with central precocious puberty: A network meta-analysis. Endocr. Pract. 2019, 25, 717–728. [Google Scholar] [CrossRef] [PubMed]
| Author | Years of Assessment | Country | Girls | Boys | ||
|---|---|---|---|---|---|---|
| Age, Years | Incidence * | Age, Years | Incidence * | |||
| Teilman et al. [5] | 1993–2001 | Denmark a | <9 | 8.0 ° | <10 | 1.0–2.0 |
| Soriano-Guillen et al. [6] | 1997–2009 | Spain b | <8 | 0.1 | <9 | 0.01 |
| Le Moal et al. [7] | 2011–2013 | France c | <9 | 2.7 | <10 | 0.2 |
| Kim et al. [8] | 2004–2010 | Korea d | <8 | 1.5 | <9 | 0.06 |
| Kim et al. [9] | 2008–2014 | Korea e | <9 | 26.3 | <10 | 0.7 |
| Idiopathic forms. |
| CNS abnormalities: |
| Arachnoid cyst, septo-optic dysplasia |
| Cerebral palsy |
| Hydrocephalus, myelo-meningocele |
| Hypothalamic hamartoma |
| Infections (congenital, acquired) |
| Malignancy (craniopharyngioma, gliomas, meningiomas, ependymoma, germinoma, astrocytoma, pineal tumor) |
| Trauma, Irradiation, Intracranial bleeding |
| Type 2 Chiari malformation |
| Syndromes/genetic variants: |
| Chromosomal microdeletion (1p36; 9p) |
| Neurofibromatosis, type 1, Tuberous sclerosis |
| Sturge-Weber, Williams-Beuren, Temple syndromes, RASopathies |
| Gain of function mutations (MKRN3, DLK1) |
| Environmental factors: |
| Endocrine disruptors |
| International adoption |
| Withdrawal of sex hormone exposure |
| Agonist | Structural Change a | Potency b | Formulation | Dose |
|---|---|---|---|---|
| Goserelin | D-Ser(tBu)/AzaGly | 100 | Monthly | 3.6 mg/28 days |
| Quarterly | 10.8 mg/90 days | |||
| Histrelin | D-His(Bzl)/N-ethylamide | 210 | Implant | 50 mg/12 months |
| Leuprorelin | D-Leu/N-ethylamide | 20 | Monthly | 3.75/7.5 mg/28 days |
| Quarterly | 11.25 mg/90 days | |||
| Half-year | 45.0 mg/180 days | |||
| Triptorelin | D-Trp/— | 35 | Monthly | 3.75 mg/28 days |
| Quarterly | 11.25 mg/90 days | |||
| Half year | 22.5 mg/180 days |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mucaria, C.; Tyutyusheva, N.; Baroncelli, G.I.; Peroni, D.; Bertelloni, S. Central Precocious Puberty in Boys and Girls: Similarities and Differences. Sexes 2021, 2, 119-131. https://doi.org/10.3390/sexes2010010
Mucaria C, Tyutyusheva N, Baroncelli GI, Peroni D, Bertelloni S. Central Precocious Puberty in Boys and Girls: Similarities and Differences. Sexes. 2021; 2(1):119-131. https://doi.org/10.3390/sexes2010010
Chicago/Turabian StyleMucaria, Cristina, Nina Tyutyusheva, Giampiero I. Baroncelli, Diego Peroni, and Silvano Bertelloni. 2021. "Central Precocious Puberty in Boys and Girls: Similarities and Differences" Sexes 2, no. 1: 119-131. https://doi.org/10.3390/sexes2010010
APA StyleMucaria, C., Tyutyusheva, N., Baroncelli, G. I., Peroni, D., & Bertelloni, S. (2021). Central Precocious Puberty in Boys and Girls: Similarities and Differences. Sexes, 2(1), 119-131. https://doi.org/10.3390/sexes2010010






