An Enhanced Self-Care Protocol for People Affected by Moderate to Severe Lymphedema
Abstract
1. Introduction
2. Enhanced-Care Protocol Development and Study Approval
3. Study Design and Participants
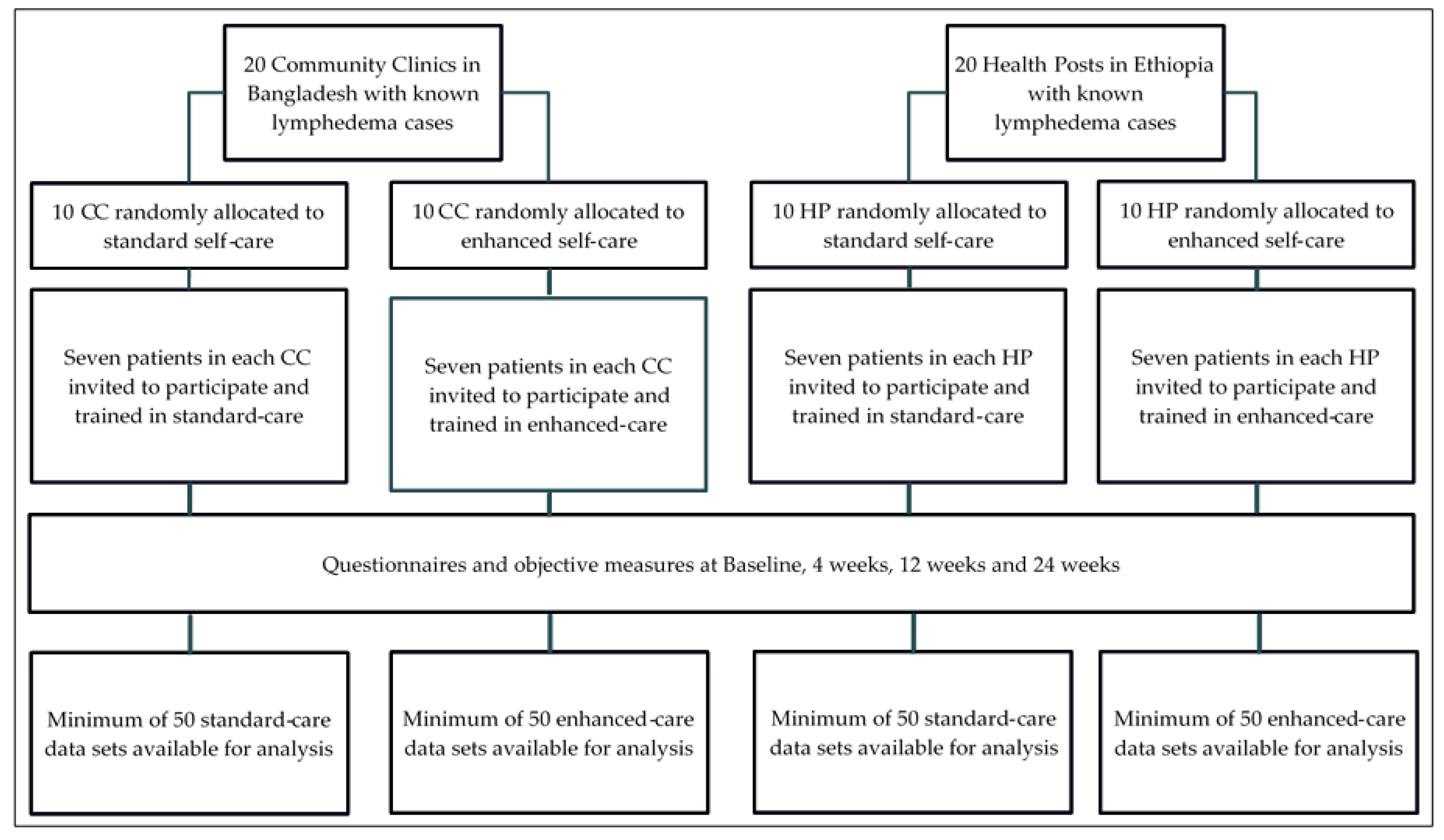
3.1. Study Design
3.2. Outcomes
3.3. Participants at Baseline
4. Lymphedema Self-Care Protocols
4.1. Standard-Care
4.1.1. Hygiene and Skin Care
4.1.2. Seated Exercises
4.1.3. Standing Exercises
4.1.4. Elevation
4.1.5. Managing Acute Attacks
4.1.6. Support services
4.2. Enhanced-Care
4.2.1. Deep Breathing Exercises
4.2.2. Lying Down Exercises
4.2.3. Skin and Tissue Mobilization
4.2.4. Lymphatic Massage
4.2.5. Walking, Drinking Water, and Eating Fresh Fruits and Vegetables
5. Participant Training
Material and Resources
6. Expected Results
7. Future Directions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- World Health Oganization. Progress Report 2000–2009 and strategic plan 2010–2020 of the global programme to eliminate lymphatic filariasis: Halfway towards eliminating lymphatic filariasis. In WHO Library Catalogue; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Deribe, K.; Cano, J.; Trueba, M.L.; Newport, M.J.; Davey, G. Global epidemiology of podoconiosis: A systematic review. PLoS Negl. Trop. Dis. 2018, 12, e0006324. [Google Scholar] [CrossRef]
- Ramaiah, K.D.; Ottesen, E.A. Progress and impact of 13 years of the global programme to eliminate lymphatic filariasis on reducing the burden of filarial disease. PLoS Negl. Trop. Dis. 2014, 8, e3319. [Google Scholar] [CrossRef]
- Mackenzie, C.D.; Lazarus, W.M.; Mwakitalu, M.E.; Mwingira, U.; Malecela, M.N. Lymphatic filariasis: Patients and the global elimination programme. Ann. Trop. Med. Parasitol. 2009, 103 (Suppl. 1), S41–S51. [Google Scholar] [CrossRef]
- World Health Organization. Global Programme to Eliminate Lymphatic Filariasis; Annual Report of Lymphatic Filariasis 2000; Rio, D.F., Ed.; Department of Communicable Disease Prevention, Control and Eradication: Geneva, Switzerland, 1999.
- WHO. Lymphatic Filariasis: Managing Morbidity and Preventing Disability: An Aide-Mémoire for National Programme Managers; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Douglass, J.; Kelly-Hope, L. Comparison of staging systems to assess lymphedema caused by cancer therapies, lymphatic filariasis, and podoconiosis. Lymphat. Res. Biol. 2019. [Google Scholar] [CrossRef]
- Nutman, T.B. Insights into the pathogenesis of disease in human lymphatic filariasis. Lymphat. Res. Biol. 2013, 11, 144–148. [Google Scholar] [CrossRef]
- Dreyer, G.; Addiss, D.; Roberts, J.; Noroes, J. Progression of lymphatic vessel dilatation in the presence of living adult Wuchereria bancrofti. Trans. R. Soc. Trop. Med. Hyg. 2002, 96, 157–161. [Google Scholar] [CrossRef]
- Davey, G. Podoconiosis, non-filarial elephantiasis, and lymphology. Lymphology 2010, 43, 168–177. [Google Scholar]
- Davey, G.; Tekola, F.; Newport, M.J. Podoconiosis: Non-infectious geochemical elephantiasis. Trans. R. Soc. Trop. Med. Hyg. 2007, 101, 1175–1180. [Google Scholar] [CrossRef]
- Jullien, P.; Somé, J.D.; Brantus, P.; Bougma, R.W.; Bamba, I.; Kyelem, D. Efficacy of home-based lymphoedema management in reducing acute attacks in subjects with lymphatic filariasis in burkina faso. Acta Trop. 2011, 120, S55–S61. [Google Scholar] [CrossRef]
- Dreyer, G.; Medeiros, Z.; Netto, M.J.; Leal, N.C.; de Castro, L.G.; Piessens, W.F. Acute attacks in the extremities of persons living in an area endemic for bancroftian filariasis: Differentiation of two syndromes. Trans. R. Soc. Trop. Med. Hyg. 1999, 93, 413–417. [Google Scholar] [CrossRef]
- Negussie, H.; Molla, M.; Ngari, M.; Berkley, J.A.; Kivaya, E.; Njuguna, P.; Fegan, G.; Tamiru, A.; Kelemework, A.; Lang, T.; et al. Lymphoedema management to prevent acute dermatolymphangioadenitis in podoconiosis in northern ethiopia (golbet): A pragmatic randomised controlled trial. Lancet Glob. Health 2018, 6, e795–e803. [Google Scholar] [CrossRef]
- Martindale, S.; Mackenzie, C.; Mkwanda, S.; Smith, E.; Stanton, M.; Molyneux, D.; Kelly-Hope, L. “Unseen” caregivers: The disproportionate gender balance and role of females in the home- based care of lymphatic filariasis patients in Malawi. Front. Women's Health 2017, 2, 1–3. [Google Scholar]
- Cassidy, T.; Worrell, C.M.; Little, K.; Prakash, A.; Patra, I.; Rout, J.; Fox, L.M. Experiences of a community-based lymphedema management program for lymphatic filariasis in odisha state, India: An analysis of focus group discussions with patients, families, community members and program volunteers. PLoS Negl. Trop. Dis. 2016, 10, e0004424. [Google Scholar] [CrossRef][Green Version]
- Stocks, M.E.; Freeman, M.C.; Addiss, D.G. The effect of hygiene-based lymphedema management in lymphatic filariasis-endemic areas: A systematic review and meta-analysis. PLoS Negl. Trop. Dis. 2015, 9, e0004171. [Google Scholar] [CrossRef]
- Douglass, J.; Graves, P.; Gordon, S. Self-care for management of secondary lymphedema: A systematic review. PLoS Negl. Trop. Dis. 2016, 10, e0004740. [Google Scholar] [CrossRef]
- Moseley, A.L.; Piller, N.B.; Carati, C.J. The effect of gentle arm exercise and deep breathing on secondary arm lymphedema. Lymphology 2005, 38, 136–145. [Google Scholar]
- Barclay, J.; Vestey, J.; Lambert, A.; Balmer, C. Reducing the symptoms of lymphoedema: Is there a role for aromatherapy? Eur. J. Oncol. Nurs. 2006, 10, 140–149. [Google Scholar] [CrossRef]
- Sikorski, C.; Ashine, M.; Zeleke, Z.; Davey, G. Effectiveness of a simple lymphoedema treatment regimen in podoconiosis management in Southern Ethiopia: One year follow-up. PLoS Negl. Trop. Dis. 2010, 4, e902. [Google Scholar] [CrossRef]
- Lehman, L.F.; Geyer, M.J.; Bolton, L. Ten Steps. A Guide for Health Promotion and Empowerment of People Affected by Neglected Tropical Diseases. Available online: https://leprosy.org/ten-steps/ (accessed on 26 June 2019).
- Chan, A.-W.; Tetzlaff, J.M.; Gøtzsche, P.C.; Altman, D.G.; Mann, H.; Berlin, J.A.; Dickersin, K.; Hróbjartsson, A.; Schulz, K.F.; Parulekar, W.R.; et al. Spirit 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ Br. Med. J. 2013, 346, e7586. [Google Scholar] [CrossRef]
- World Medical Association. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Dreyer, G.; Addiss, D.; Dreyer, P.; Noroes, J. Basic Lymphoedema Management, Treatment and Prevention Problems Associated with Lymphatic Filariasis; Hollis Publishing Company: Hollis, NH, USA, 2002. [Google Scholar]
- Hartung, C.; Lerer, A.; Anokwa, Y.; Tseng, C.; Brunette, W.; Borriello, G. Open data kit: Tools to build information services for developing regions. In Proceedings of the 4th ACM/IEEE International Conference on Information and Communication Technologies and Development, London, UK, 13–16 December 2010; pp. 1–12. [Google Scholar]
- Choi, B.C.; Pak, A.W.; Choi, J.C. Daily step goal of 10,000 steps: A literature review. Clin. Investig. Med. 2007, 30, E146–E151. [Google Scholar] [CrossRef]
| Activity | Description | Frequency |
|---|---|---|
| Leg washing and drying | Thoroughly wash and dry both legs including skin folds and interdigital spaces | ≥ twice per day |
| Attending to entry lesions | Careful inspection of legs, feet and toe spaces to identify broken or damaged skin | ≥ twice per day |
| Applying medicated cream | Apply antifungal cream to interdigital lesions Apply antibiotic cream (Bangladesh) or petroleum jelly (Ethiopia) to entry lesions | ≥ twice per day |
| Trimming nails | Trim broken or long toenails | As needed |
| Standing exercises | Slowly rise up and down on the toes | ≥ once per day |
| Seated exercises | Passive ROM exercises for the ankle Active ROM exercises for the ankle Sets of 5 in each direction with each leg | ≥ once per day |
| Daytime elevation | Place the affected leg(s) on a stool or cushion so the foot is higher than the hip | Whenever sitting |
| Night-time elevation | Raise the end of the bed or sleeping mat so the feet are higher than the head | Every night |
| Managing acute attacks | Seek symptomatic relief such as cooling a hot limb and taking pain medication Rest and cease the exercises until the attack has resolved, continue all hygiene practices Use medicated cream and take oral medication (antibiotic or anti-inflammatory) if required | As needed |
| Accessing support services | Attend the health facility for help or advice Attend lymphedema support groups | As needed |
| Activity | Description | Frequency |
|---|---|---|
| Deep breathing exercises | Inhale deep into the abdomen using the diaphragm so that the belly pushes out without allowing the chest to rise | 5 breaths ≥5 times per day |
| Lying down exercises | Knees bent and using one leg at a time: 1: Draw the knee firmly into the chest during the exhale, returning the foot to the floor during the inhale 2: Lift the lower leg up and down without touching the floor | Repeat each movement 5 times with each leg ≥ once per day |
| Mobilizing the skin and tissue | Gently move and roll any skin or underlying tissue that feels hard | ≥ once per day |
| Lymphatic massage | Massage both legs beginning with the least affected leg Use a flat hand-over-hand stroking technique in a distal to proximal direction Edible vegetable oil can be used as a massage medium (optional) | ≥ once per day |
| Walking | Walk as much as possible, ideally for ≥45 minutes per day | Daily |
| Drinking clean water | Drink ≥5 glasses of clean water | Daily |
| Eating fresh fruits and vegetables | Eat at least once serve of fresh fruit or vegetables | ≥4 days per week |
| Activity | Bangladesh | Ethiopia |
|---|---|---|
| Leg washing and drying | Soap* 2 wash cloths 2 drying cloths | Large wash bowl 1 Soap* 1 wash cloth 1 1 drying cloth 1 |
| Attending to entry lesions | Antifungal cream Antibiotic cream Gauze bandage | Whitfield® cream 2 Vaseline® |
| Trimming nails | Nail clippers | Nail clippers 1 |
| Lymphatic massage | 250 ml coconut oil (enhanced-care group only) | 1 litre vegetable oil 1 (enhanced-care group only) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Douglass, J.; Mableson, H.E.; Martindale, S.; Kelly-Hope, L.A. An Enhanced Self-Care Protocol for People Affected by Moderate to Severe Lymphedema. Methods Protoc. 2019, 2, 77. https://doi.org/10.3390/mps2030077
Douglass J, Mableson HE, Martindale S, Kelly-Hope LA. An Enhanced Self-Care Protocol for People Affected by Moderate to Severe Lymphedema. Methods and Protocols. 2019; 2(3):77. https://doi.org/10.3390/mps2030077
Chicago/Turabian StyleDouglass, Janet, Hayley E. Mableson, Sarah Martindale, and Louise A. Kelly-Hope. 2019. "An Enhanced Self-Care Protocol for People Affected by Moderate to Severe Lymphedema" Methods and Protocols 2, no. 3: 77. https://doi.org/10.3390/mps2030077
APA StyleDouglass, J., Mableson, H. E., Martindale, S., & Kelly-Hope, L. A. (2019). An Enhanced Self-Care Protocol for People Affected by Moderate to Severe Lymphedema. Methods and Protocols, 2(3), 77. https://doi.org/10.3390/mps2030077





