Vitamin B12 Deficiency (Un-)Detected Using Newborn Screening in Norway
Abstract
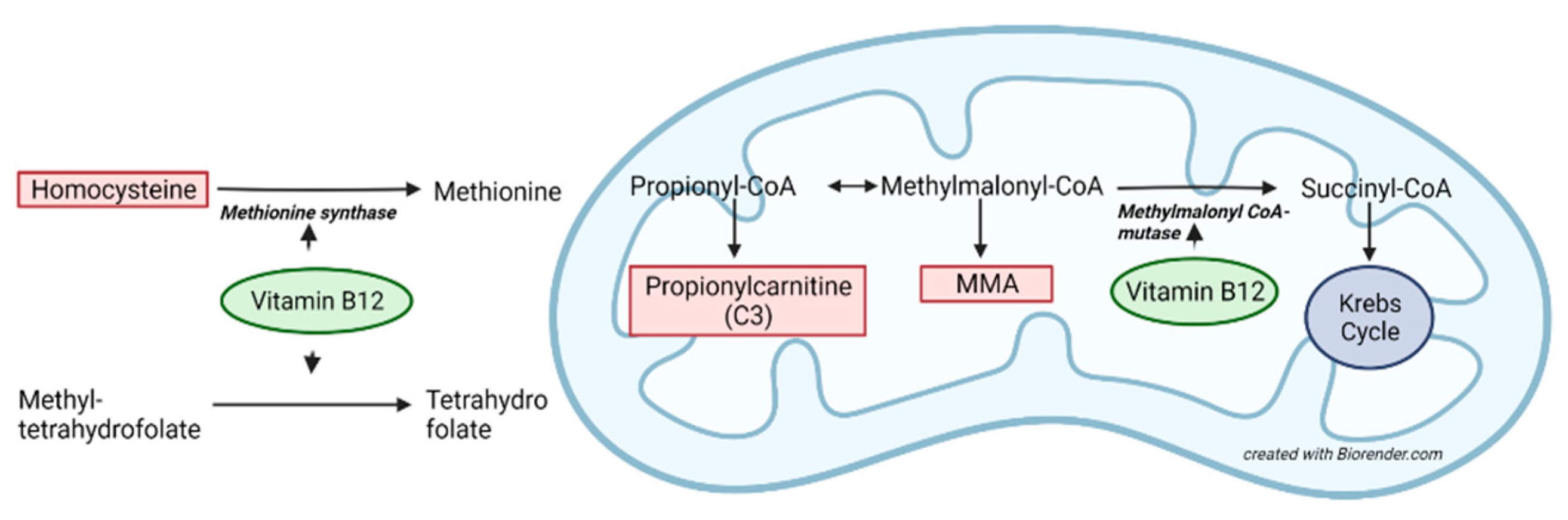
1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Newborn Screening DBS Analyses
2.3. Biochemical Analyses
2.4. Definitions
2.5. Statistics
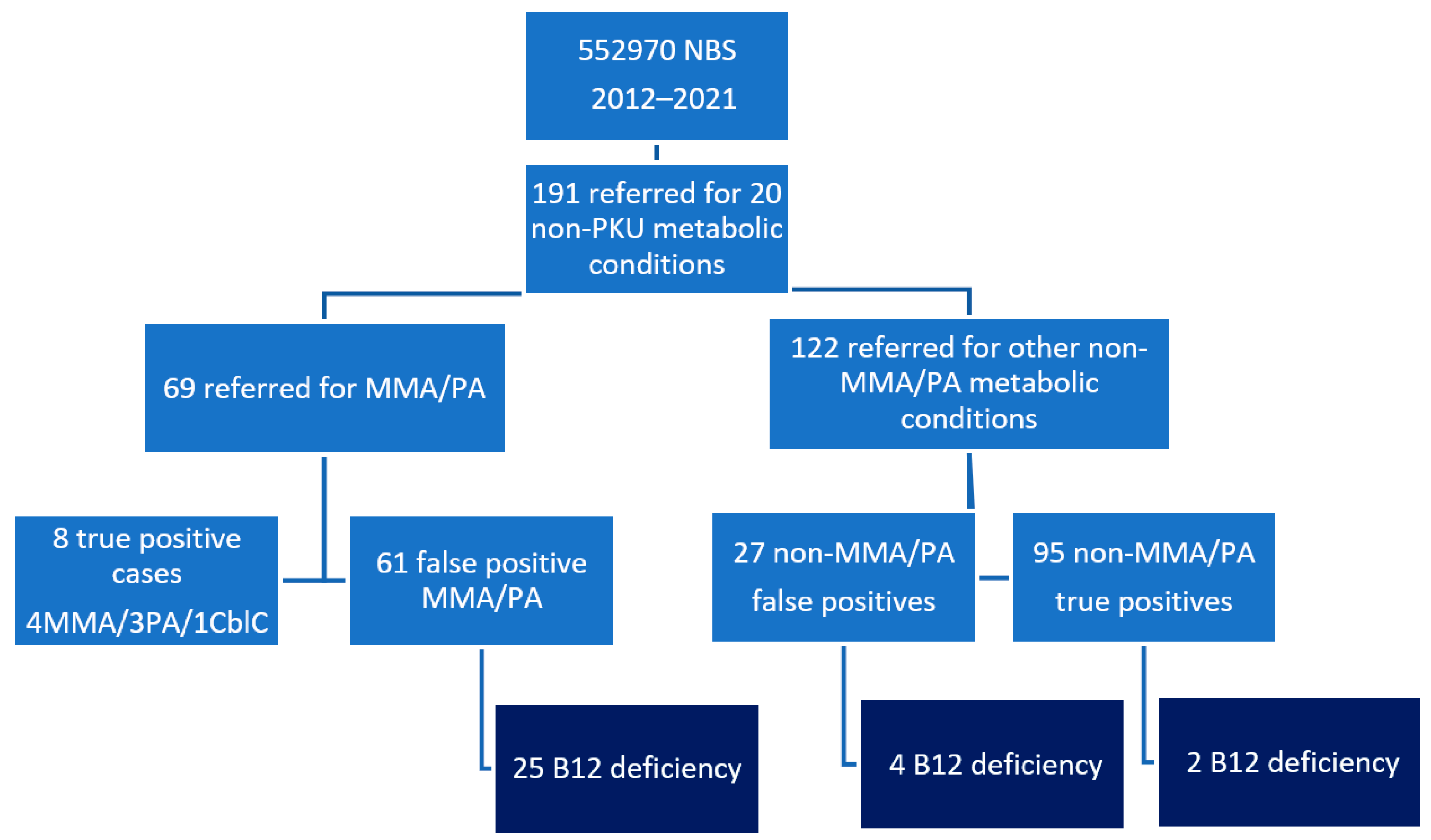
3. Results
3.1. Cohort of 61 False Positive Methylmalonic Acidemia and PA
DBS Second-Tier Analysis
3.2. Newborns Reported for Other Metabolic Diseases from NBS Diagnosed with B12 Deficiency
3.3. Two Clinically Ascertained Cases with Severe, Symptomatic B12 Deficiency
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bjørke Monsen, A.L.; Ueland, P.M.; Vollset, S.E.; Guttormsen, A.B.; Markestad, T.; Solheim, E.; Refsum, H. Determinants of cobalamin status in newborns. Pediatrics 2001, 108, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Green, R.; Allen, L.H.; Bjørke-Monsen, A.L.; Brito, A.; Guéant, J.L.; Miller, J.W.; Molloy, A.M.; Nexo, E.; Stabler, S.; Toh, B.H.; et al. Vitamin B(12) deficiency. Nat. Rev. Dis. Prim. 2017, 3, 17040. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.D.; Warren, M.J.; Refsum, H. Vitamin B(12). Adv. Food Nutr. Res. 2018, 83, 215–279. [Google Scholar] [PubMed]
- Rozmarič, T.; Mitulović, G.; Konstantopoulou, V.; Goeschl, B.; Huemer, M.; Plecko, B.; Spenger, J.; Wortmann, S.B.; Scholl-Bürgi, S.; Karall, D.; et al. Elevated Homocysteine after Elevated Propionylcarnitine or Low Methionine in Newborn Screening Is Highly Predictive for Low Vitamin B12 and Holo-Transcobalamin Levels in Newborns. Diagnostics 2020, 10, 626. [Google Scholar] [CrossRef]
- Gramer, G.; Fang-Hoffmann, J.; Feyh, P.; Klinke, G.; Monostori, P.; Okun, J.G.; Hoffmann, G.F. High incidence of maternal vitamin B(12) deficiency detected by newborn screening: First results from a study for the evaluation of 26 additional target disorders for the German newborn screening panel. World J. Pediatr. 2018, 14, 470–481. [Google Scholar] [CrossRef]
- Bjørke Monsen, A.L.; Ueland, P.M. Homocysteine and methylmalonic acid in diagnosis and risk assessment from infancy to adolescence. Am. J. Clin. Nutr. 2003, 78, 7–21. [Google Scholar] [CrossRef]
- Irevall, T.; Axelsson, I.; Naumburg, E. B12 deficiency is common in infants and is accompanied by serious neurological symptoms. Acta Paediatr. 2017, 106, 101–104. [Google Scholar] [CrossRef]
- Ljungblad, U.W.; Astrup, H.; Mørkrid, L.; Hager, H.B.; Lindberg, M.; Eklund, E.A.; Bjørke-Monsen, A.-L.; Rootwelt, T.; Tangeraas, T. Breastfed Infants With Spells, Tremor, or Irritability: Rule Out Vitamin B12 Deficiency. Pediatr. Neurol. 2022, 131, 4–12. [Google Scholar] [CrossRef]
- Jain, R.; Singh, A.; Mittal, M.; Talukdar, B. Vitamin B12 deficiency in children: A treatable cause of neurodevelopmental delay. J. Child Neurol. 2015, 30, 641–643. [Google Scholar] [CrossRef]
- Graham, S.M.; Arvela, O.M.; Wise, G.A. Long-term neurologic consequences of nutritional vitamin B12 deficiency in infants. J Pediatr. 1992, 121 Pt 1, 710–714. [Google Scholar] [CrossRef]
- Ray, J.G.; Goodman, J.; O’Mahoney, P.R.; Mamdani, M.M.; Jiang, D. High rate of maternal vitamin B12 deficiency nearly a decade after Canadian folic acid flour fortification. QJM 2008, 101, 475–477. [Google Scholar] [CrossRef] [PubMed]
- Varsi, K.; Ueland, P.M.; Torsvik, I.K.; Bjørke-Monsen, A.L. Maternal Serum Cobalamin at 18 Weeks of Pregnancy Predicts Infant Cobalamin Status at 6 Months-A Prospective, Observational Study. J. Nutr. 2018, 148, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Rashid, S.; Meier, V.; Patrick, H. Review of Vitamin B12 deficiency in pregnancy: A diagnosis not to miss as veganism and vegetarianism become more prevalent. Eur. J. Haematol. 2021, 106, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Hinton, C.F.; Ojodu, J.A.; Fernhoff, P.M.; Rasmussen, S.A.; Scanlon, K.S.; Hannon, W.H. Maternal and neonatal vitamin B12 deficiency detected through expanded newborn screening--United States, 2003–2007. J. Pediatr. 2010, 157, 162–163. [Google Scholar] [CrossRef] [PubMed]
- Reinson, K.; Künnapas, K.; Kriisa, A.; Vals, M.A.; Muru, K.; Õunap, K. High incidence of low vitamin B12 levels in Estonian newborns. Mol. Genet. Metab. Rep. 2018, 15, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Sarafoglou, K.; Rodgers, J.; Hietala, A.; Matern, D.; Bentler, K. Expanded newborn screening for detection of vitamin B12 deficiency. JAMA 2011, 305, 1198–1200. [Google Scholar] [CrossRef] [PubMed]
- Turgeon, C.T.; Magera, M.J.; Cuthbert, C.D.; Loken, P.R.; Gavrilov, D.K.; Tortorelli, S.; Raymond, K.M.; Oglesbee, D.; Rinaldo, P.; Matern, D. Determination of total homocysteine, methylmalonic acid, and 2-methylcitric acid in dried blood spots by tandem mass spectrometry. Clin. Chem. 2010, 56, 1686–1695. [Google Scholar] [CrossRef]
- Scolamiero, E.; Villani, G.R.; Ingenito, L.; Pecce, R.; Albano, L.; Caterino, M.; di Girolamo, M.G.; Di Stefano, C.; Franzese, I.; Gallo, G.; et al. Maternal vitamin B12 deficiency detected in expanded newborn screening. Clin. Biochem. 2014, 47, 312–317. [Google Scholar] [CrossRef]
- Held, P.K.; Singh, E.; Scott Schwoerer, J. Screening for Methylmalonic and Propionic Acidemia: Clinical Outcomes and Follow-Up Recommendations. Int. J. Neonatal Screen. 2022, 8, 13. [Google Scholar] [CrossRef]
- Gramer, G.; Fang-Hoffmann, J.; Feyh, P.; Klinke, G.; Monostori, P.; Mütze, U.; Posset, R.; Weiss, K.H.; Hoffmann, G.F.; Okun, J.G. Newborn Screening for Vitamin B(12) Deficiency in Germany-Strategies, Results, and Public Health Implications. J. Pediatr. 2020, 216, 165–172.e4. [Google Scholar] [CrossRef]
- Pajares, S.; Arranz, J.A.; Ormazabal, A.; Del Toro, M.; García-Cazorla, Á.; Navarro-Sastre, A.; López, R.M.; Meavilla, S.M.; Santos, M.M.d.L.; García-Volpe, C.; et al. Implementation of second-tier tests in newborn screening for the detection of vitamin B(12) related acquired and genetic disorders: Results on 258,637 newborns. Orphanet. J. Rare Dis. 2021, 16, 195. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.J.; Röschinger, W.; Blessing, H.; Lotz-Havla, A.S.; Schiergens, K.A.; Maier, E.M. Diagnostic Challenges Using a 2-Tier Strategy for Methylmalonic Acidurias: Data from 1.2 Million Dried Blood Spots. Ann. Nutr. Metab. 2020, 76, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Mütze, U.; Walter, M.; Keller, M.; Gramer, G.; Garbade, S.F.; Gleich, F.; Haas, D.; Posset, R.; Grünert, S.C.; Hennermann, J.B.; et al. Health Outcomes of Infants with Vitamin B(12) Deficiency Identified by Newborn Screening and Early Treated. J. Pediatr. 2021, 235, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Gramer, G.; Hoffmann, G.F. Vitamin B(12) Deficiency in Newborns and their Mothers-Novel Approaches to Early Detection, Treatment and Prevention of a Global Health Issue. Curr. Med. Sci. 2020, 40, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Hawthorne, S.; Levy, H.L. Can Newborn Screening for Vitamin B(12) Deficiency be Incorporated into All Newborn Screening Programs? J. Pediatr. 2020, 216, 9–11.e1. [Google Scholar] [CrossRef] [PubMed]
- Behandlingsprotokoller 2016. Available online: https://oslo-universitetssykehus.no/avdelinger/barne-og-ungdomsklinikken/nyfodtscreeningen/nyfodtscreening#behandlingsprotokoller (accessed on 3 March 2022).
- Tangeraas, T.; Sæves, I.; Klingenberg, C.; Jørgensen, J.; Kristensen, E.; Gunnarsdottir, G.; Hansen, E.V.; Strand, J.; Lundman, E.; Ferdinandusse, S.; et al. Performance of Expanded Newborn Screening in Norway Supported by Post-Analytical Bioinformatics Tools and Rapid Second-Tier DNA Analyses. Int. J. Neonatal Screen. 2020, 6, 51. [Google Scholar] [CrossRef]
- Fu, X.; Xu, Y.K.; Chan, P.; Pattengale, P.K. Simple, Fast, and Simultaneous Detection of Plasma Total Homocysteine, Methylmalonic Acid, Methionine, and 2-Methylcitric Acid Using Liquid Chromatography and Mass Spectrometry (LC/MS/MS). JIMD Rep. 2013, 10, 69–78. [Google Scholar]
- Ljungblad, U.W.; Lindberg, M.; Eklund, E.A.; Saeves, I.; Bjørke-Monsen, A.L.; Tangeraas, T. Nitrous oxide in labour predicted newborn screening total homocysteine and is a potential risk factor for infant vitamin B12 deficiency. Acta Paediatr. 2022, 111, 2315–2321. [Google Scholar] [CrossRef]
- Hannibal, L.; Lysne, V.; Bjørke-Monsen, A.L.; Behringer, S.; Grünert, S.C.; Spiekerkoetter, U.; Jacobsen, D.W.; Blom, H.J. Biomarkers and Algorithms for the Diagnosis of Vitamin B12 Deficiency. Front. Mol. Biosci. 2016, 3, 27. [Google Scholar] [CrossRef]
- Bjørke-Monsen, A.L. Assessment of cobalamin status. Tidsskr Nor Laegeforen 2020, 140. [Google Scholar] [CrossRef]
- Refsum, H.; Grindflek, A.W.; Ueland, P.M.; Fredriksen, A.; Meyer, K.; Ulvik, A.; Guttormsen, A.B.; Iversen, O.E.; Schneede, J.; Kase, B.F. Screening for serum total homocysteine in newborn children. Clin. Chem. 2004, 50, 1769–1784. [Google Scholar] [CrossRef] [PubMed]
- Minet, J.C.; Bisse, E.; Aebischer, C.P.; Beil, A.; Wieland, H.; Lutschg, J. Assessment of vitamin B-12, folate, and vitamin B-6 status and relation to sulfur amino acid metabolism in neonates. Am. J. Clin. Nutr. 2000, 72, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Monsen, A.L.; Refsum, H.; Markestad, T.; Ueland, P.M. Cobalamin status and its biochemical markers methylmalonic acid and homocysteine in different age groups from 4 days to 19 years. Clin. Chem. 2003, 49, 2067–2075. [Google Scholar] [CrossRef]
- Bjørke-Monsen, A.L.; Torsvik, I.; Saetran, H.; Markestad, T.; Ueland, P.M. Common metabolic profile in infants indicating impaired cobalamin status responds to cobalamin supplementation. Pediatrics 2008, 122, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Torsvik, I.; Ueland, P.M.; Markestad, T.; Bjørke-Monsen, A.L. Cobalamin supplementation improves motor development and regurgitations in infants: Results from a randomized intervention study. Am. J. Clin. Nutr. 2013, 98, 1233–1240. [Google Scholar] [CrossRef]
- Torsvik, I.K.; Ueland, P.M.; Markestad, T.; Midttun, Ø.; Bjørke Monsen, A.L. Motor development related to duration of exclusive breastfeeding, B vitamin status and B12 supplementation in infants with a birth weight between 2000–3000 g, results from a randomized intervention trial. BMC Pediatr. 2015, 15, 218. [Google Scholar] [CrossRef]
- Lipari Pinto, P.; Florindo, C.; Janeiro, P.; Santos, R.L.; Mexia, S.; Rocha, H.; de Almeida, I.T.; Vilarinho, L.; Gaspar, A. Acquired Vitamin B12 Deficiency in Newborns: Positive Impact on Newborn Health through Early Detection. Nutrients 2022, 14, 4379. [Google Scholar] [CrossRef]
- Zanardo, V.; Caroni, G.; Burlina, A. Higher homocysteine concentrations in women undergoing caesarean section under general anesthesia. Thromb. Res. 2003, 112, 33–36. [Google Scholar] [CrossRef]
- Bae, S.; West, A.A.; Yan, J.; Jiang, X.; Perry, C.A.; Malysheva, O.; Stabler, S.P.; Allen, R.H.; A Caudill, M. Vitamin B-12 Status Differs among Pregnant, Lactating, and Control Women with Equivalent Nutrient Intakes. J. Nutr. 2015, 145, 1507–1514. [Google Scholar] [CrossRef]
- Ljungblad, U.W.; Lindberg, M.; Eklund, E.A.; Sæves, I.; Sagredo, C.; Bjørke-Monsen, A.L.; Tangeraas, T. A Retrospective Evaluation of the Predictive Value of Newborn Screening for Vitamin B12 Deficiency in Symptomatic Infants Below 1 Year of Age. Int. J. Neonatal Screen. 2022, 8, 66. [Google Scholar] [CrossRef]
| Newborns without B12 Deficiency (n = 36) | Newborns with B12 Deficiency (n = 25) | |||
|---|---|---|---|---|
| Plasma/serum | Median [IQR] | Range | Median [IQR] | Range |
| Age at sampling | 6 [5–8.9] days | 3–14 | 7 [6–9] days | 2–68 |
| Vitamin B12 pmol/L | Vitamin B12 pmol/L | |||
| Newborns | 222 [200–286] (34 1) | 112–679 | 155 [109–223] (24 1) | 60–327 |
| Mothers | 213 [162–321] (32 1) | 90–563 | 171 [124–255] (21 1) | 90–333 |
| Folate nmol/L | Folate nmol/L | |||
| Newborns | 27 [22–31] (23) | 10–57 | 30 [22–36] (19) | 17–48 |
| Mothers | 13 [9.4–17] (25) | 4–41 | 11 [9.8–16] (19) | 3–29 |
| tHcy µmol/L | tHcy µmol/L | |||
| Newborns | 7 [6.1–8] (35) | 3.6–10 | 13.4 [11.1–20] (25) | 10–64 |
| Mothers | 9 [7.2–11] * (30) | 5–16 | 11.2 [10.0–15] * (21) | 7.7–19.3 |
| MMA µmol/L | MMA µmol/L | |||
| Newborns | 0.3 [0.25–0.5] ** (32) | 0.1–1.1 | 1.6 [0.79–6.1] ** (25) | 0.4–27.7 |
| Mothers | 0.23 [0.18–0.4] (30) | 0.1–0.8 | 0.49 [0.25–0.6] (19) | 0.1–3.2 |
| U-MMA (%) a | - | U-MMA (%) a | - | |
| Newborns | 1/31 2 (0.03) ** | 20/23 3 (87) ** |
| Variable | Newborns without B12 Deficiency (n = 36) | Newborns with B12 Deficiency (n = 25) | Controls (n = 89) | |||
|---|---|---|---|---|---|---|
| Median [IQR] | Range | Median [IQR] | Range | Median [IQR] | Range | |
| Gestational age (weeks) | 39 [37–40] | 27–42 | 39 [38–40] | 28–41 | 40 [38–41] | (35–42) |
| Female/male (%) | 22/14 (61/39) | 15/10 (60/40) | - | 46/48 (49/51) | - | |
| Birthweight (g) | 3322 [2923–3697] | 935–4465 | 3120 [2745–3797] | 1340–4880 | 3410 [3085–3780] | (2035–4680) |
| NBS DBSo | Median [IQR] | Range | Median [IQR] | Range | Median [IQR] | Range |
| C3 (µmol/L) | 9.4 [7.2–11.8] | 3.3–18.5 | 7.7 [6–9.9] | 3.8–17.2 | 1.8 [1.4–2.3] | 0.7–6.9 |
| C3/C2 | 0.27 [0.2–0.3] | 0.11–0.42 | 0.26 [0.21–0.3] | 0.17–0.60 | 0.08 [0.06–0.1] | 0.04–0.2 |
| Methionine (µmol/L) | 20 [17.3–22.0] | 12–30 | 17.9 [14–28] | 9–42 | 17.5 [14.3–20.1] | 9.4–32.9 |
| Met/Phe | 0.35 [0.3–0.42] | 0.22–0.68 | 0.31 [0.26–0.40] | 0.18–0.5 | 0.34 [0.29–0.38] | 0.18–0.57 |
| Age at NBS sampling (hours) | 55 [51–61] | 48–85 | 54 [51–66] | 48–1644 | 58.5 [53–64.2] | 48–110 |
| Age at reporting (days) | 5 [4–7] | 3–13 | 7 [5.5–8.5] | 3–72 | - | - |
| NBS DBSs 2021 | Median [IQR] | Range | Median [IQR] | Range | Median [IQR] | Range |
| DBS storage (y) | 6.9 [3.9–8.3] | 0.2–9.0 | 6.3 [1.4–8.3] (23) | 0.2–8.9 | 4.2 [3.3–6.2] | (2.2–8.9) |
| DBS MMA (µmol/L) | 0.0 [0.0–0.15] | 0.0–0.2 | 0.36 [0.12–3.1] (23) | 0.0–32 | 0.0 [0–0.09] | 0.0–0.9 |
| DBS tHcy (µmol/L | 7.9 [6.9–10.4] | 4.9–19 | 11.0 [7.3–14.5] (23) | 5.4–46 | 7.2 [5.9–8.9] | 3.6–18.9 |
| DBS MCA (µmol/L) | 0.2 [0.08–0.4] | 0.0–2.0 | 0.3 [0.07–0.5] (23) | 0.05–1.0 | 0.0 [0.0–0.05] | 0.0–1.3 |
| Patient (P) | DBS C3 µmol/L | DBS C3/C2 | DBS Met µmol/L | DBS Met/Phe | DBS * tHcy µmol/L | DBS * MMA µmol/L | Plasma B12 pmol/L | Plasma tHcy µmol/L | Plasma MMA µmol/L |
|---|---|---|---|---|---|---|---|---|---|
| P1 (f) | 2.40 | 0.14 | 14.5 | 0.38 | 24.1 | 2.11 | 60 | 167 | 30 |
| Mother P1 | - | - | - | - | - | - | 60 | 30 | 2.0 |
| P2 (m) | 3.05 | 0.40 | 14 | 0.24 | 22.7 | 41.1 | 80 | 110 | 231 |
| Mother P2 | - | - | - | - | - | - | 91 | 66 | 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tangeraas, T.; Ljungblad, U.W.; Lutvica, E.; Kristensen, E.; Rowe, A.D.; Bjørke-Monsen, A.-L.; Rootwelt-Revheim, T.; Sæves, I.; Pettersen, R.D. Vitamin B12 Deficiency (Un-)Detected Using Newborn Screening in Norway. Int. J. Neonatal Screen. 2023, 9, 3. https://doi.org/10.3390/ijns9010003
Tangeraas T, Ljungblad UW, Lutvica E, Kristensen E, Rowe AD, Bjørke-Monsen A-L, Rootwelt-Revheim T, Sæves I, Pettersen RD. Vitamin B12 Deficiency (Un-)Detected Using Newborn Screening in Norway. International Journal of Neonatal Screening. 2023; 9(1):3. https://doi.org/10.3390/ijns9010003
Chicago/Turabian StyleTangeraas, Trine, Ulf W. Ljungblad, Elma Lutvica, Erle Kristensen, Alex D. Rowe, Anne-Lise Bjørke-Monsen, Terje Rootwelt-Revheim, Ingjerd Sæves, and Rolf D. Pettersen. 2023. "Vitamin B12 Deficiency (Un-)Detected Using Newborn Screening in Norway" International Journal of Neonatal Screening 9, no. 1: 3. https://doi.org/10.3390/ijns9010003
APA StyleTangeraas, T., Ljungblad, U. W., Lutvica, E., Kristensen, E., Rowe, A. D., Bjørke-Monsen, A.-L., Rootwelt-Revheim, T., Sæves, I., & Pettersen, R. D. (2023). Vitamin B12 Deficiency (Un-)Detected Using Newborn Screening in Norway. International Journal of Neonatal Screening, 9(1), 3. https://doi.org/10.3390/ijns9010003






