Parental Depression and Anxiety Associated with Newborn Bloodspot Screening for Rare and Variable-Onset Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Eligibility
2.3. Recruitment and Survey Procedure
2.4. Measures
2.5. Statistical Analysis
3. Results
3.1. Description of the Study Sample
3.2. Levels of Depression
3.3. Levels of Parental Stress
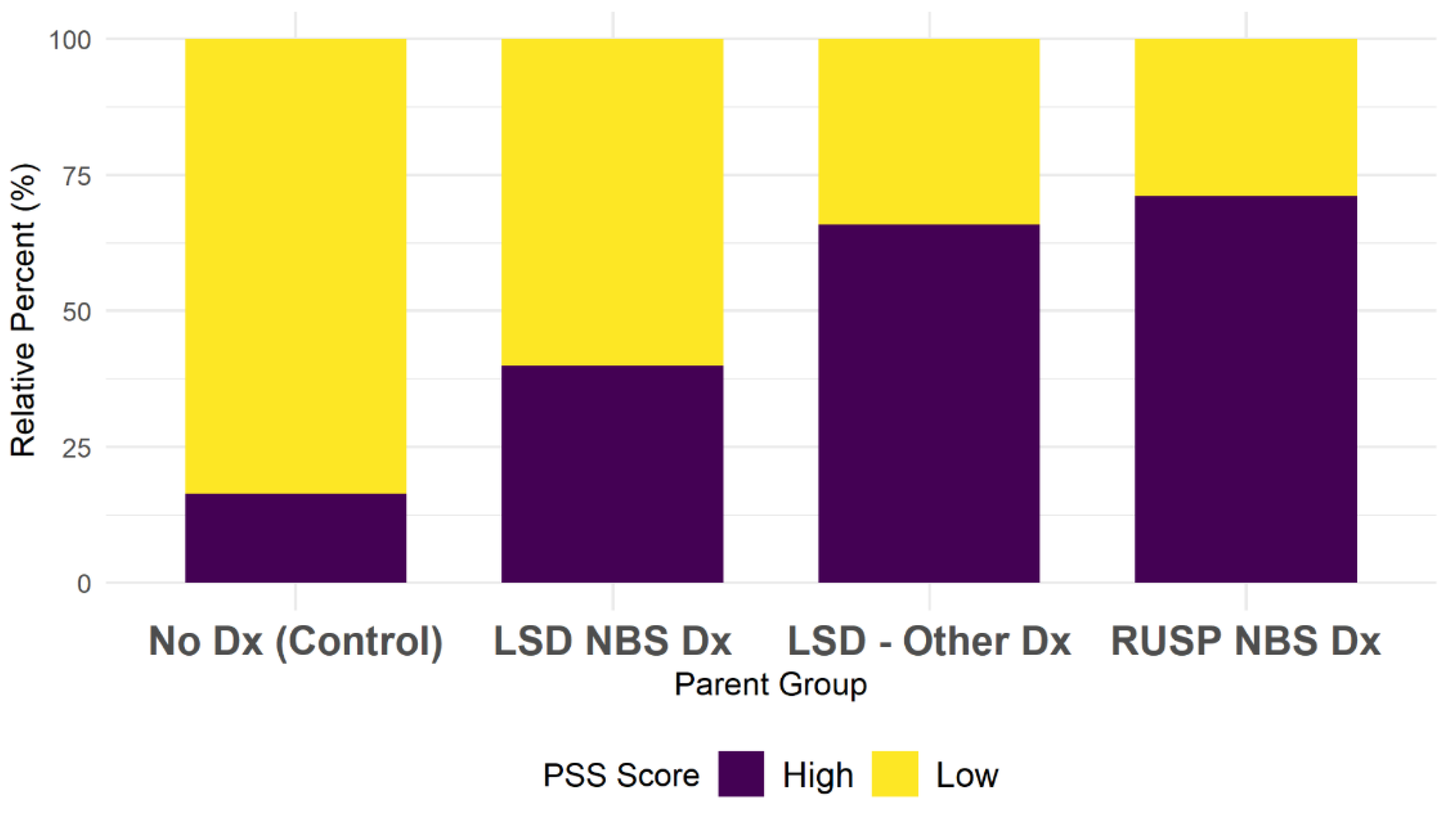
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilcken, B.; Wiley, V. Newborn screening. Pathology 2008, 40, 104–115. [Google Scholar] [CrossRef]
- Bailey, D.B., Jr.; Porter, K.A.; Andrews, S.M.; Raspa, M.; Gwaltney, A.Y.; Peay, H.L. Expert Evaluation of Strategies to Modernize Newborn Screening in the United States. JAMA Netw. Open 2021, 4, e2140998. [Google Scholar] [CrossRef] [PubMed]
- Staretz-Chacham, O.; Lang, T.C.; LaMarca, M.E.; Krasnewich, D.; Sidransky, E. Lysosomal Storage Disorders in the Newborn. Pediatrics 2009, 123, 1191–1207. [Google Scholar] [CrossRef] [PubMed]
- Spada, M.; Pagliardini, S.; Yasuda, M.; Tukel, T.; Thiagarajan, G.; Sakuraba, H.; Ponzone, A.; Desnick, R.J. High Incidence of Later-Onset Fabry Disease Revealed by Newborn Screening. Am. J. Hum. Genet. 2006, 79, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Wasserstein, M.P.; Orsini, J.J.; Goldenberg, A.; Caggana, M.; Levy, P.A.; Breilyn, M.; Gelb, M.H. The future of newborn screening for lysosomal disorders. Neurosci. Lett. 2021, 760, 136080. [Google Scholar] [CrossRef]
- Engelen, M.; Kemp, S.; De Visser, M.; Van Geel, B.M.; Wanders, R.J.A.; Aubourg, P.; Poll-The, B.T. X-linked adrenoleukodystrophy (X-ALD): Clinical presentation and guidelines for diagnosis, follow-up and management. Orphanet J. Rare Dis. 2012, 7, 51. [Google Scholar] [CrossRef]
- Moser, H.W.; Mahmood, A.; Raymond, G.V. X-linked adrenoleukodystrophy. Nat. Clin. Pract. Cardiovasc. Med. 2007, 3, 140–151. [Google Scholar] [CrossRef]
- Grosse, S.D.; Boyle, C.A.; Kenneson, A.; Khoury, M.J.; Wilfond, B.S. From Public Health Emergency to Public Health Service: The Implications of Evolving Criteria for Newborn Screening Panels. Pediatrics 2006, 117, 923–929. [Google Scholar] [CrossRef]
- Timmermans, S.; Buchbinder, M. Patients-in-Waiting: Living between Sickness and Health in the Genomics Era. J. Health Soc. Behav. 2010, 51, 408–423. [Google Scholar] [CrossRef]
- Schwan, K.; Youngblom, J.; Weisiger, K.; Kianmahd, J.; Waggoner, R.; Fanos, J. Family Perspectives on Newborn Screening for X-Linked Adrenoleukodystrophy in California. Int. J. Neonatal Screen. 2019, 5, 42. [Google Scholar] [CrossRef]
- Garrett, J.R.; Lantos, J.D.; Biesecker, L.G.; Childerhose, J.E.; Chung, W.K.; Holm, I.A.; Koenig, B.A.; McEwen, J.E.; Wilfond, B.S.; Brothers, K. Rethinking the “open future” argument against predictive genetic testing of children. Genet. Med. 2019, 21, 2190–2198. [Google Scholar] [CrossRef] [PubMed]
- Wasserstein, M.P.; Caggana, M.; Bailey, S.M.; Desnick, R.J.; Edelmann, L.; Estrella, L.; Holzman, I.; Kelly, N.R.; Kornreich, R.; Kupchik, S.G.; et al. The New York pilot newborn screening program for lysosomal storage diseases: Report of the First 65,000 Infants. Genet. Med. 2018, 21, 631–640. [Google Scholar] [CrossRef]
- Sulkers, E.; Tissing, W.J.; Brinksma, A.; Roodbol, P.F.; Kamps, W.A.; Stewart, R.E.; Sanderman, R.; Fleer, J. Providing care to a child with cancer: A longitudinal study on the course, predictors, and impact of caregiving stress during the first year after diagnosis. Psychooncology 2015, 24, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Berry, J.O.; Jones, W.H. The Parental Stress Scale: Initial Psychometric Evidence. J. Soc. Pers. Relatsh. 1995, 12, 463–472. [Google Scholar] [CrossRef]
- Rishi, P.; Rishi, E.; Maitray, A.; Agarwal, A.; Nair, S.; Gopalakrishnan, S. Hospital anxiety and depression scale assessment of 100 patients before and after using low vision care: A prospective study in a tertiary eye-care setting. Indian J. Ophthalmol. 2017, 65, 1203–1208. [Google Scholar] [CrossRef]
- Cronly, J.; Horgan, A.M.; Lehane, E.; Howe, B.; Duff, A.J.; Riekert, K.A.; Perry, I.J.; Fitzgerald, A.P.; Ni Chroinin, M.; Savage, E. Anxiety and Depression in Parent Caregivers of Children with Cystic Fibrosis. J. Child Fam. Stud. 2019, 28, 1304–1312. [Google Scholar] [CrossRef]
- Rahmani, A.; Azadi, A.; Pakpour, V.; Faghani, S.; Afsari, E.A. Anxiety and Depression: A Cross-sectional Survey among Parents of Children with Cancer. Indian J. Palliat. Care 2018, 24, 82–85. [Google Scholar] [PubMed]
- Pace, C.C.; Spittle, A.J.; Molesworth, C.M.; Lee, K.J.; Northam, E.A.; Cheong, J.L.; Davis, P.G.; Doyle, L.W.; Treyvaud, K.; Anderson, P.J. Evolution of depression and anxiety symptoms in parents of very preterm infants during the newborn period. Jama Pediatr. 2016, 170, 863–870. [Google Scholar] [CrossRef]
- Parental Stress Scale (PSS). Available online: https://www.corc.uk.net/outcome-experience-measures/parental-stress-scale-pss/ (accessed on 6 September 2022).
- Louie, D.; Cromer, L.D.; Berry, J.O. Assessing parenting stress: Review of the use and interpretation of the parental stress scale. Fam. J. 2017, 25, 359–367. [Google Scholar] [CrossRef]
- Shapiro, D.N.; Stewart, A.J. Parenting stress, perceived child regard, and depressive symptoms among stepmothers and biological mothers. Fam. Relat. 2011, 60, 533–544. [Google Scholar] [CrossRef]
- Pearce, N.; Foliaki, S.; Sporle, A.; Cunningham, C. Genetics, race, ethnicity, and health. BMJ 2004, 328, 1070–1072. [Google Scholar] [CrossRef] [PubMed]
- U.S. CensusCensus Regions and Divisions of the United States. 1984. Available online: https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf (accessed on 1 September 2022).
- Botkin, J.R.; Belmont, J.W.; Berg, J.S.; Berkman, B.E.; Bombard, Y.; Holm, I.A.; Levy, H.P.; Ormond, K.E.; Saal, H.M.; Spinner, N.B.; et al. Points to Consider: Ethical, Legal, and Psychosocial Implications of Genetic Testing in Children and Adolescents. Am. J. Hum. Genet. 2015, 97, 6–21. [Google Scholar] [CrossRef] [PubMed]
- COMMITTEE ON BIOETHICS. Ethical and Policy Issues in Genetic Testing and Screening of Children. Pediatrics 2013, 131, 620–622. [Google Scholar] [CrossRef]
- O’Connor, K.; Jukes, T.; Goobie, S.; DiRaimo, J.; Moran, G.; Potter, B.K.; Chakraborty, P.; Rupar, C.A.; Gannavarapu, S.; Prasad, C. Psychosocial Impact on Mothers Receiving Expanded Newborn Screening Results. Eur. J. Hum. Genet. 2018, 26, 477–484. Available online: https://idp.nature.com/authorize/casa?redirect_uri=https://www.nature.com/articles/s41431-017-0069-z&casa_token=UmUbw00hrCwAAAAA:_X6DjTbwfm5OLAdREPfktwoBdRJZ_oD5mwFfUIq8YCkiTd7wCGyG5TLFgWNk442OTwWPP_u5tyMBNo9Wtvw (accessed on 1 September 2022). [CrossRef]
- Waisbren, S.E.; Albers, S.; Amato, S.; Ampola, M.; Brewster, T.G.; Demmer, L.; Eaton, R.B.; Greenstein, R.; Korson, M.; Larson, C.; et al. Effect of Expanded Newborn Screening for Biochemical Genetic Disorders on Child Outcomes and Parental Stress. JAMA 2003, 290, 2564–2572. [Google Scholar] [CrossRef] [PubMed]
- Miller, D. The diagnostic odyssey: Our family’s story. Am. J. Hum. Genet. 2021, 108, 217–218. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy conception of anxiety. Anxiety Res. 1988, 1, 77–98. [Google Scholar] [CrossRef]
- Ross, E.; Mirowsky, J. Explaining the Social Patterns of Depression: Control and Problem Solving—Or Support and Talking? J. Health Soc. Behav. 1989, 30, 206–219. [Google Scholar] [CrossRef]
- Tluczek, A.; Zaleski, C.; Stachiw-Hietpas, D.; Modaff, P.; Adamski, C.R.; Nelson, M.R.; Reiser, C.A.; Ghate, S.; Josephson, K.D. A tailored approach to family-centered genetic counseling for cystic fibrosis newborn screening: The Wisconsin model. J. Genet. Couns. 2011, 20, 115–128. [Google Scholar] [CrossRef]
- Mandell, S.; Salzer, M.S. Who joins support groups among parents of children with autism? Autism 2016, 11, 111–122. [Google Scholar] [CrossRef] [PubMed]
- White, L.; Boardman, F.; McNiven, A.; Locock, L.; Hinton, L. Absorbing it all: A meta-ethnography of parents’ unfolding experiences of newborn screening. Soc. Sci. Med. 2021, 287, 114367. [Google Scholar] [CrossRef] [PubMed]
- Norton, S.; Cosco, T.; Doyle, F.; Done, J.; Sacker, A. The Hospital Anxiety and Depression Scale: A meta confirmatory factor analysis. J. Psychosom. Res. 2013, 74, 74–81. [Google Scholar] [CrossRef] [PubMed]

| All N = 174 | LSD-NBS Dx n = 20 | LSD-Other Dx n = 41 | RUSP-NBS Dx n = 52 | No Dx n = 61 | |
|---|---|---|---|---|---|
| Age, years (mean ± SD) | 30.00 ± 3.92 | 30.10 ± 3.57 | 30.34 ± 3.83 | 28.87 ± 3.55 | 30.70 ± 4.24 |
| Relationship to child | |||||
| Mother | 110 (63%) | 12 (60%) | 25 (61%) | 32 (62%) | 41 (67%) |
| Father | 64 (37%) | 8 (40%) | 16 (39%) | 20 (38%) | 20 (33%) |
| Relationship Status | |||||
| Married or living with a partner | 162 (93%) | 18 (90%) | 41 (100%) | 48 (92%) | 55 (90%) |
| Not married or living with a partner | 12 (7%) | 2 (10%) | 0 (0%) | 4 (8%) | 6 (10%) |
| N Children Born Between 2013–2018 | |||||
| One | 113 (65%) | 16 (80%) | 25 (61%) | 35 (67%) | 37 (61%) |
| More than one | 61 (35%) | 4 (20%) | 16 (39%) | 17 (33%) | 24 (39%) |
| Education | |||||
| Bachelor’s degree or higher a | 84 (48%) | 11 (55%) | 22 (54%) | 24 (46%) | 27 (44%) |
| Less than a bachelor’s degree b | 89 (51%) | 9 (45%) | 18 (44%) | 28 (54%) | 34 (56%) |
| Do not wish to answer | 1 (1%) | 0 (0%) | 1 (2%) | 0 (0%) | 0 (0%) |
| Employment | |||||
| Employed full-time or part-time | 147 (84%) | 16 (80%) | 37 (90%) | 47 (90%) | 47 (77%) |
| Stay at home parent | 22 (13%) | 3 (15%) | 3 (7%) | 4 (8%) | 12 (20%) |
| Unemployed or unable to work | 5 (3%) | 1 (5%) | 1 (2%) | 1 (2%) | 2 (5%) |
| Income (annual household) | |||||
| Less than $34,999 | 22 (13%) | 2 (10%) | 2 (5%) | 5 (10%) | 13 (21%) |
| $35,000–$49,999 | 42 (24%) | 2 (10%) | 13 (32%) | 15 (29%) | 12 (20%) |
| $50,000–$99,999 | 81 (47%) | 12 (60%) | 22 (54%) | 27 (52%) | 20 (33%) |
| More than $100,000 | 18 (10%) | 2 (10%) | 3 (7%) | 4 (8%) | 9 (15%) |
| Do not wish to answer | 11 (6%) | 2 (10%) | 1 (2%) | 1 (2%) | 7 (12%) |
| US Region | |||||
| Midwest | 32 (18%) | 2 (10%) | 8 (20%) | 6 (12%) | 16 (26%) |
| Northeast | 43 (25%) | 7 (35%) | 7 (17%) | 7 (13%) | 22 (36%) |
| South | 40 (23%) | 7 (35%) | 12 (29%) | 14 (27%) | 7 (11%) |
| West | 58 (33%) | 4 (20%) | 14 (34%) | 25 (48%) | 16 (26%) |
| Race | |||||
| White, non-Hispanic/Latino/a/x | 100 (57%) | 12 (60%) | 30 (73%) | 26 (50%) | 32 (52%) |
| Black/African American, non-Hispanic/Latino/a/x | 28 (16%) | 3 (15%) | 6 (15%) | 5 (10%) | 14 (23%) |
| All other races/multiple races, and/or Hispanic/Latino/a/x | 45 (26%) | 5 (25%) | 5 (12%) | 21 (40%) | 14 (23%) |
| Do not wish to answer | 1 (1%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (2%) |
| Ethnicity | |||||
| Hispanic or Latino/a/x | 14 (8%) | 2 (10%) | 1 (2%) | 6 (12%) | 5 (8%) |
| Not Hispanic or Latino/a/x | 159 (91%) | 18 (90%) | 40 (98%) | 46 (88%) | 55 (90%) |
| Do not wish to answer | 1 (1%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (2%) |
| HADS | |||||
|---|---|---|---|---|---|
| Chi-Square Statistic or Fisher’s Exact Test | p-Value | Cramer’s V | |||
| Region of the US | 15.63 | p = 0.001 *** | V = 0.30 | ||
| Income | 13.68 | p = 0.003 *** | V = 0.29 | ||
| Race | 5.82 | p = 0.05 * | V = 0.18 | ||
| Relationship to child | 2.69 | p = 0.10 | V = 0.12 | ||
| Number of children | 2.66 | p = 0.10 | V = 0.12 | ||
| Employment status | FET | p = 0.15 | V = 0.15 | ||
| Education | 0.75 | p = 0.39 | V = 0.07 | ||
| Ethnicity (Hispanic or Latino/a/x, y/n) | p = 0.42 | V = 0.06 | |||
| Major life events (y/n) | 0.44 | p = 0.51 | V = 0.05 | ||
| Relationship status | p = 0.80 | V = 0.02 | |||
| n | Mean | T-value (95% CI) | p-value | Cohen’s D | |
| Not considerable depression | 93 | 30.33 | −1.22 (−1.87–0.44) | 0.22 | −0.18 |
| Considerable depression | 81 | 29.62 | |||
| PSS | |||||
| Chi-Square Statistic or Fisher’s Exact Test | p-Value | Cramer’s V | |||
| Region of the US | 17.41 | p < 0.001 *** | V = 0.32 | ||
| Employment | FET | p = 0.006 *** | V = 0.22 | ||
| Major life events (y/n) | 5.76 | p = 0.02 ** | V = 0.18 | ||
| Income | 9.21 | p = 0.03 ** | V = 0.24 | ||
| Relationship to the child | 3.38 | p = 0.07 * | V = 0.14 | ||
| Relationship status | 1.98 | p = 0.16 | V = 0.11 | ||
| Race | 2.91 | p = 0.23 | V = 0.13 | ||
| Education | 0.74 | p = 0.48 | V = 0.07 | ||
| Number of children | 0.21 | p = 0.65 | V = 0.04 | ||
| Ethnicity (Hispanic or Latino/a/x y/n) | p = 0.84 | V = 0.02 | |||
| n | Mean | T-Value (95% CI) | p-Value | Cohen’s D | |
| Low PSS | 92 | 30.32 | −1.13 (−1.84–0.50) | 0.26 | −0.17 |
| High PSS | 82 | 29.65 | |||
| HADS Outcome | PSS Outcome | |
|---|---|---|
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | |
| LSD-Other | 6.06 (1.64–24.96) | 2.85 (0.82–10.37) |
| RUSP-NBS | 3.44 (1.00–12.88) | 3.20 (0.96–11.10) |
| Control | 0.49 (0.13–1.93) | 0.24 (0.09–1.16) |
| Northeast | 0.32 (0.08–1.14) | 0.92 (0.26–3.24) |
| South | 0.53 (0.15–1.77) | 2.13 (0.66–7.01) |
| West | 1.48 (0.47–4.64) | 1.80 (0.61–5.39) |
| Less than $34,999 | 0.37 (0.09–1.44) | 0.30 (0.07–1.21) |
| $50,000–$99,999 | 1.54 (0.61–3.97) | 0.78 (0.34–2.02) |
| More than $100,000 | 0.27 (0.05–1.24) | 0.93 (0.23–3.80) |
| All other races | 2.94 (0.80–11.37) | |
| White (Non-Hispanic) | 0.62 (0.20–1.90) | |
| Relationship to the child (mother) | 0.66 (0.29–1.46) | |
| Major life changes (yes) | 0.50 (0.14–1.63) | |
| Stay at home parent | 0.50 (0.11–1.97) | |
| Unemployed/unable to work | 6.52 (0.51–87.55) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boychuk, N.A.; Mulrooney, N.S.; Kelly, N.R.; Goldenberg, A.J.; Silver, E.J.; Wasserstein, M.P. Parental Depression and Anxiety Associated with Newborn Bloodspot Screening for Rare and Variable-Onset Disorders. Int. J. Neonatal Screen. 2022, 8, 59. https://doi.org/10.3390/ijns8040059
Boychuk NA, Mulrooney NS, Kelly NR, Goldenberg AJ, Silver EJ, Wasserstein MP. Parental Depression and Anxiety Associated with Newborn Bloodspot Screening for Rare and Variable-Onset Disorders. International Journal of Neonatal Screening. 2022; 8(4):59. https://doi.org/10.3390/ijns8040059
Chicago/Turabian StyleBoychuk, Natalie A., Niamh S. Mulrooney, Nicole R. Kelly, Aaron J. Goldenberg, Ellen J. Silver, and Melissa P. Wasserstein. 2022. "Parental Depression and Anxiety Associated with Newborn Bloodspot Screening for Rare and Variable-Onset Disorders" International Journal of Neonatal Screening 8, no. 4: 59. https://doi.org/10.3390/ijns8040059
APA StyleBoychuk, N. A., Mulrooney, N. S., Kelly, N. R., Goldenberg, A. J., Silver, E. J., & Wasserstein, M. P. (2022). Parental Depression and Anxiety Associated with Newborn Bloodspot Screening for Rare and Variable-Onset Disorders. International Journal of Neonatal Screening, 8(4), 59. https://doi.org/10.3390/ijns8040059






