Abstract
This study aimed to report the progress and results of the newborn screening program for congenital heart disease (CHD) in south Shanghai between 2019 and 2023, and to evaluate the accuracy of the dual-index method (pulse oximetry (POX) plus cardiac murmur auscultation) in clinical practice. Between 2019 and 2023, a total of 198,606 (99.89%) newborns were screened for CHD, of whom 3299 (1.66%) tested positive, 3043 (92.24%) underwent echocardiography for CHD diagnosis and 1109 were diagnosed with CHD in a timely manner. Among 195,307 infants with negative screening results using the dual-index method, 139 (0.07%) were later diagnosed with CHD, and none of these infants died. More than half of these false-negative infants (59.39%) were identified due to the detection of a heart murmur during routine physical examinations within six months after birth. Compared to POX testing alone, the dual-index method significantly improved the sensitivity of screening for CHD, and kept high specificity in clinical practice. This study demonstrated that newborn screening for CHD has been well conducted in Shanghai, and the dual-index method had high accuracy and reliability for neonatal CHD screening in clinical practice.
1. Introduction
Congenital heart disease (CHD) can affect approximately 150,000 births per year in China [1], and is a leading cause of infant death [2]. Approximately one-third of these patients have life-threatening major CHD, which requires surgery or invasive intervention within the first year of life to prevent severe complications and death [3]. Almost all life-threatening major CHD cases can be corrected if diagnosed and intervened in a timely manner, while delayed diagnosis is associated with severe complications, including acute cardiovascular collapse, heart failure, hypoxemia-induced acidosis, hypoxic–ischemic brain damage, recurrent pneumonia and infant death [4,5]. Therefore, the early detection of life-threatening major CHD is critical during the neonatal period.
Pulse oximetry (POX) is an easily accessible noninvasive test [6], and has been demonstrated to improve early detection of critical CHD (CCHD), thereby improving outcomes for affected newborns [7]. Our previous studies also demonstrated that POX is an effective screening method for CCHD with moderate sensitivity and high specificity in China, and additionally found that POX plus cardiac murmur auscultation (namely dual-index method) can significantly improve the detection rate of both CCHD and life-threatening major CHD during the early neonatal stage [8,9]. To reduce infant mortality and under-five mortality, the Shanghai Municipal Health Commission implemented newborn screening for CHD using the dual-index method in all birthing facilities, and established a systematic network to cover the entire city with partition management for screening, diagnosis and treatment in 2016 [10].
The Children’s Hospital of Fudan University, a large Grade A tertiary hospital (the highest level in China’s hospital classification system) located in the Minhang District of Shanghai, pioneered the dual-index method and demonstrated its accuracy and feasibility during the birth hospitalization. As one of the four diagnosis and treatment centers for CHD in Shanghai, the Children’s Hospital of Fudan University is responsible for the management, training and quality control of newborn screening program for CHD in the south Shanghai including five administrative districts (Xuhui, Minhang, Songjiang, Jinshan and Qingpu). The primary objective of this study was to update the progress and results of the newborn screening program for CHD in these five districts between 2019 and 2023. And the secondary aim was to evaluate the accuracy of the dual-index method and its continued impact on CHD detection in clinical practice, including an assessment of postnatally diagnosed CHD cases undetected by the dual-index method, over a five-year period in all delivery hospitals in the south Shanghai.
2. Materials and Methods
2.1. Study Design and Participants
This was a five-year retrospective cohort study involving all live births delivered at hospitals in the five districts of Shanghai from 1 January 2019 to 31 December 2023. The study included all consecutive newborns who participated in CHD screening using the dual-index method, regardless of gestational age or neonatal intensive care unit (NICU) admission status. Newborns who did not receive routine screening (e.g., parent refusal) were excluded from the present study (N = 219).
Before and after delivery, trained medical staff provided education for all participants’ parents and families regarding the risks of CHD, benefits and limitations of newborn screening for CHD, as well as short- and long-term follow-up recommendations. All participants’ parents gave written informed consent for their children before participating in newborn screening for CHD. This study was approved by the ethics committee of the Children’s Hospital of Fudan University.
2.2. Procedures
The screening methodology and procedures have been described in detail elsewhere [9,10]. Briefly, screening for CHD was performed in newborn babies aged 6–72 h. Cardiac murmur auscultation was conducted by a trained pediatrician in a quiet room using a stethoscope appropriate for newborns prior to POX screening to ensure that the auscultation result is not affected by noise or the POX result. Then, a trained nurse or pediatrician conducted POX screening using a pulse oximeter with a multisite sensor to measure oxygen saturations from the babies’ right hand and either foot. Dual-index screening for CHD was defined as positive if (a) cardiac murmur is grade II or above, (b) the pulse oximeter oxygen saturation (SpO2) is less than 90% in the right hand or either foot, (c) the SpO2 is less than 95% in the right hand or either foot on two measurements separated by 2~4 h or (d) a difference between the two extremities is more than 3% on two measurements, separated by 2~4 h. Standardized training and on-site supervision are conducted at least twice each year for medical staff in birthing facilities to ensure the accuracy and reliability of screening results and data registrations [10].
For newborns with positive screening results, clinicians immediately informed their parents of the necessity for echocardiography to rule out CHD. In accordance with the requirements of the Shanghai Newborn Congenital Heart Disease Screening Program [10], newborns who screened positive using the dual-index method were referred to the Children’s Hospital of Fudan University or other diagnosis and treatment centers for echocardiography within one week, and those diagnosed with CHD were further evaluated by pediatric cardiac experts. For infants with negative screening results, clinical follow-up and physical examinations were conducted at local community hospitals at 6 weeks, 3 months and 6 months of age, in combination with feedbacks from parents about cardiac symptoms such as cyanosis, tachypnea and feeding difficulty or medical chart review. Newborns diagnosed without CHD will stay in the track of Child Health Management, a basic public health service program for children under seven years of age in China [10].
During the COVID-19 pandemic, Shanghai implemented a range of effective policies (e.g., nucleic acid testing, vaccination availability, standard infection control measures) to ensure the safety of pregnant and postpartum women during childbirth, balancing infection control with the continuity of essential maternity care [11,12].
2.3. Data Source
The Information Management System of Newborn Screening for CHD (www.nchd.org.cn accessed on 16 May 2025) was used daily to register and track the results of CHD screening, diagnosis, and treatment. All delivery hospitals registered information on maternal and neonatal demographic characteristics (e.g., maternal name, maternal resident identity card, infant name, sex and birth date) and screening results (including the screening date, SpO2 values and grade of cardiac murmur). The Children’s Hospital of Fudan University uploaded echocardiography, and registered the results of diagnosis (including the diagnosis date, and CHD classification) and treatment (including the date, method and outcome of surgery or interventional catheterization) in this electronic registration system.
2.4. Defining Outcomes
As suggested by previous studies [8,13], CHD were classified as critical (requiring intervention or causing death within 28 days of age), serious (requiring intervention before 1 year of age, but not classified as critical), significant (defects persist longer than 6 months of age, but not classified as critical or serious), and non-significant (defects are not physically appreciable and do not persist after 6 months of age). For the purpose of the study analyses, we defined critical and serious CHD as life-threatening major CHD, while the remaining categories were classified as minor CHD.
In this study, the following conditions were excluded from the definition of CHD: (1) patent ductus arteriosus that closed spontaneously within 3 months, (2) atrial septal defect (ASD) < 5 mm in diameter at 3 months of age, (3) physiological pulmonary branch stenosis that resolved during follow-up, (4) pulmonary stenosis or aortic stenosis with a pressure gradient of <20 mmHg without further deterioration during follow-up and (5) simple patent foramen ovale [3].
2.5. Statistical Analyses
The results of newborn screening for CHD in each district per year are presented using the following key indicators: (1) screening rate = number of newborns screened/number of live births × 100%; (2) screened positive rate = number of newborns screened positive/number of newborns screened × 100%; (3) echocardiography examination rate = number of echocardiography in newborns screened positive/number of newborns screened positive × 100%; (4) diagnostic rate of CHD in newborns screened positive = number of newborns diagnosed with CHD in those screened positive/number of newborns screened positive × 100%; (5) CHD prevalence = number of CHD cases/number of live births × 100%.
We calculated the sensitivity, specificity, false-positive rate, positive and negative predictive value, consistency rate, Youden’s index and positive and negative likelihood ratios for both the dual-index method and POX alone in newborn screening for CHD. The Wilson method was used to calculate the 95% confidence interval (95% CI) of sensitivity and specificity. Additionally, we described the false-negative results of the dual-index method. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
3. Results
3.1. Results of Newborn Screening for CHD in South Shanghai
From 1 January 2019 to 31 December 2023, a total of 198,606 (99.89%) newborns were screened for CHD using the dual-index method across the five districts of south Shanghai (Table 1 and Figure 1). The annual CHD screening rate has exceeded 99% in all districts (Figure 2). Among the 198,606 newborns screened, 3299 (1.66%) tested positive, of whom 3043 (92.24%) underwent echocardiography for CHD diagnosis (Table 1). The echocardiography examination rate increased from 85.63% in 2019 to 97.51% in 2023 (Table 1), demonstrating an upward trend in nearly all districts (Figure 2).

Table 1.
Results of the newborn screening program for CHD in the five districts of Xuhui, Minhang, Songjiang, Jinshan and Qingpu in Shanghai from 2019 to 2023.
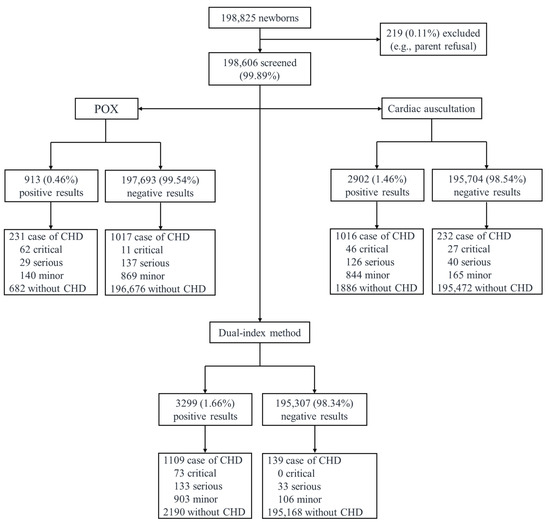
Figure 1.
Profile of newborn screening for congenital heart disease in the five districts of Xuhui, Minhang, Songjiang, Jinshan and Qingpu in Shanghai. Note: CHD, congenital heart disease; POX, pulse oximetry.
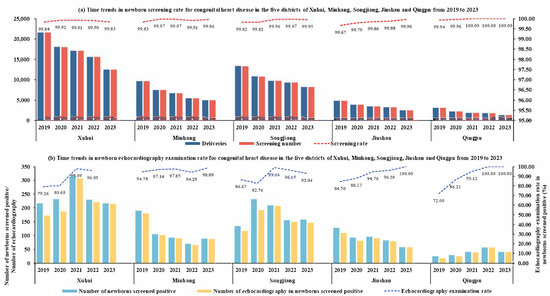
Figure 2.
Time trends in newborn screening rate and echocardiography examination rate for congenital heart disease in the five districts of Xuhui, Minhang, Songjiang, Jinshan and Qingpu from 2019 to 2023.
A total of 1109 (33.62%) screen-positive newborns were diagnosed with CHD, including 73 CCHD, 133 serious CHD and 903 minor CHD (Figure 1). As presented in Table 2, CCHD cases included pulmonary atresia (n = 20), total anomalous pulmonary venous drainage (n = 16), coarctation of the aorta (n = 11), transposition of the great arteries (n = 10), critical pulmonary stenosis (n = 7), interrupted aortic arch (n = 3), double outlet right ventricle (n = 2), hypoplastic left heart syndrome (n = 2) and single ventricle (n = 2). Serious CHD cases included ventricular septal defect (n = 71), Tetralogy of Fallot (n = 20), pulmonary stenosis (n = 18), patent ductus arteriosus (n = 15), atrioventricular septal defect (n = 6), coarctation of the aorta (n = 2) and partial anomalous pulmonary venous connection (n = 1).

Table 2.
Types of life-threatening major congenital heart disease in infants with positive and negative screening results using the dual-index method.
3.2. CHD in Infants with Negative Screening Results of the Dual-Index Method
Among 195,307 infants with negative screening results from the dual-index method, 139 (0.07%) were subsequently diagnosed with CHD. More than half of these false-negative infants (59.39%) were identified due to the detection of a heart murmur during routine physical examinations within six months after birth. The remaining cases were diagnosed through echocardiography, which was arranged for conditions such as preterm birth, low birth weight, pneumonia or other medical concerns.
Fortunately, among these 139 infants, none were diagnosed with CCHD, and 33 infants were diagnosed with serious CHD requiring surgery before the age of one year. These cases included patent ductus arteriosus (n = 17), ventricular septal defect (n = 12), atrioventricular septal defect (n = 1), coarctation of the aorta (n = 1), cor triatriatum (n = 1) and partial anomalous pulmonary venous connection (n = 1, Table 2). There were no deaths among infants with negative screening results using the dual-index method.
3.3. Accuracy of Screening Methods for CCHD and Life-Threatening Major CHD
The accuracy of POX and the dual-index method for the detection of CCHD, life-threatening major CHD, and all types of CHD is presented in Table 3. In this retrospective cohort, POX alone as a screening method was able to identify 62 of 73 (84.93%) cases of CCHD, but only 91 of 239 (38.08%) cases of major CHD. The specificity of POX was 99.57% and 99.59% for CCHD and life-threatening major CHD, respectively. The dual-index method could detect 73 of 73 (100.00%) cases of CCHD and 206 of 239 (86.19%) cases of life-threatening major CHD. Compared to POX testing alone, the dual-index method significantly improved the sensitivity of screening for CCHD and life-threatening major CHD. Additionally, the dual-index method could achieve similarly high specificities (CCHD: 98.38%, major CHD: 98.44%), and had similarly high consistency rates.

Table 3.
Accuracy of screening methods for detecting critical and major congenital heart disease, and all types of congenital heart disease (N = 198,606).
The positive predictive value of POX was 6.79% for CCHD and 9.97% for life-threatening major CHD, while the positive predictive value of the dual-index method was 2.21% for critical CHD, and 6.24% for life-threatening major CHD.
4. Discussion
Using real-world data from a five-year clinical practice, this study detailed the progress and results of the newborn screening program for CHD in the five administrative districts of south Shanghai between 2019 and 2023, and evaluated the accuracy and reliability of the dual-index method and its continued impact on CHD detection in clinical practice. Nearly all live births in these five districts were screened for CHD using the dual-index method, and the echocardiography examination rate and diagnostic rate of CHD in newborns screened positive have reached 92.24% and 33.62%, respectively. Furthermore, this study confirmed that the dual-index method had high sensitivities and specificities for detecting both CCHD and life-threatening major CHD in clinical practice.
Between 2019 and 2023, almost all newborns were screened for CHD using the dual-index method in the five administrative districts of south Shanghai, and the annual screening rate for CHD has exceeded 99% in all five districts. The mean screened positive rate (1.66%) was consistent with findings from our previous multicenter screening studies [8,9]. The echocardiography examination rate among newborns who screened positive in the south Shanghai was 92.24%, showing an upward trend from 85.63% in 2019 to 97.51% in 2023, which was higher than the citywide average (89.88%) between 2017 and 2021 [10]. The overall prevalence of CHD in the five districts (6.28‰) was slightly lower than the prevalence (7.93‰) reported in our previous multicenter prospective screening study conducted at 15 birthing facilities in Shanghai, while the prevalence of life-threatening major CHD (1.20‰) in this study was comparable to that of our previous study (1.21‰) [9]. These findings suggest that while some CHD may be missed or underreported in clinical practice using the dual-index method, life-threatening major CHD cases are consistently identified. Overall, the high screening rate, echocardiography examination rate and the fact that 202 children with CHD received timely and effective treatment indicated that the newborn screening program for CHD has been well implemented in the five districts of south Shanghai and a sound integrated network for neonatal CHD screening, diagnosis and treatment has been established. These findings also underscored that, despite the challenges to the Shanghai healthcare system posed by COVID-19 [14], the newborn screening program for CHD effectively adapted to maintain high standards of care, ensuring the early detection and timely treatment of CHD in newborns.
In our study, the post-discharge diagnosis rate of CCHD was 4/100,000, which aligns with the results from our previous screening study in Shanghai [9] and a UK regional study [15], but lower than the rate in the rest of China [3,8]. The observed differences in the prevalence of CCHD may be attributed to a combination of advanced prenatal diagnosis and regional healthcare disparities. In Shanghai, prenatal diagnosis for CHD is a routine part of pregnancy management. A study by Zhang et al. (2020) found that regions like Zhejiang, which share a similar healthcare infrastructure to Shanghai, reported 90% prenatal detection rates for CCHD [16]. Additionally, genetic studies in Shanghai have shown a high incidence of chromosomal abnormalities in fetuses with CCHD [17], which may influence parental decisions regarding pregnancy termination [18]. Higher maternal education and access to advanced healthcare in Shanghai further contribute to the lower CCHD prevalence. [19].
POX screening for CCHD has been widely recommended and adopted in many countries [20]. In the present study, we found that POX had moderate sensitivity (84.93%) and high specificity (99.57%) for CCHD, consistent with our previous multicenter screening studies [8,9], and with findings from studies conducted in developed countries [6]. However, POX alone as a screening method was only able to identify only 38.08% of cases of major CHD. The sensitivity of POX screening for major CHD in this study was lower than that in our previous studies conducted at 15 birthing facilities in Shanghai (44.3%) [9], and 18 hospitals in 10 provinces of China (58.7%) [3], but higher than a 5-year observational study from the UK (33%) [15]. This study, along with previous research, suggested that POX alone as a screening method may lead to missed diagnoses of many major CHD cases, such as large ventricular septal defects and tetralogy of Fallot [21,22]. Therefore, all major CHD should be regarded as targets for newborn screening to prevent heart failure or irreversible pulmonary vascular disease.
In the present study, the sensitivity and specificity of the dual-index method was 100.00% and 98.38% for CCHD, which were consistent with the findings of our previous multicenter screening studies [8,9]. Although the sensitivity of the dual-index method for major CHD (86.19%) in this study was slightly lower than that in our previous studies [8,9], our findings demonstrated that the dual-index method could significantly improve the sensitivities for CCHD and major CHD compared to using POX testing alone. Additionally, the false-positive rates of the dual-index method for the detection of CCHD and major CHD remained at a low level. These findings provide valuable insights that address concerns in countries like the UK about the missed diagnosis of major CHD using only POX testing and the high false-positive rate. It is also noteworthy that the positive predictive value of the dual-index method for all types of CHD exceeded one-third, indicating that over 30 out of 100 infants with a positive screening result using the dual-index method would be diagnosed and treated in a timely manner. Infants with early detection of CHD may benefit from subsequent timely intervention and intensive surveillance [10]. Importantly, only 0.08% (139 of 195,307) of infants with negative screening results using the dual-index method were later diagnosed with CHD, of whom 33 were identified with major CHD, and there were no deaths among these infants. Over half of these false-negative infants (59.39%) were found to have a heart murmur during routine physical examination within six months after birth, suggesting that infants with negative screening results using the dual-index method should be aware of follow-up physical examination.
Our study has several strengths. First, the present study utilized real-world data from a five-year clinical practice across all delivery hospitals in the five administrative districts of Shanghai, which enhances the applicability of the results to everyday clinical practice. Second, our study comprehensively described the postnatal diagnoses of all types of CHD in infants with both positive and negative results using the dual-index method over a five-year period, and described what cardiac conditions lead to false-negative results using the dual-index method. Third, this study benefited from a relatively large sample size, enabling us to assess whether the accuracy of the dual-index method in clinical practice aligns with findings from our previous large-scale, prospective, multicenter screening studies. Inevitably, the present study also has several limitations. First, as a retrospective database study based on real-world clinical practice, it may be constrained by the lack of direct control and the inherent heterogeneity of the population. Second, 139 infants with negative screening results using the dual-index method were later diagnosed with CHD through clinical follow-up and medical chart review, which indicated that there was a possibility of false-negative results. Third, the low prevalence of CCHD in the current study would be expected to impact the positive predictive value of screening. Future studies should further validate the accuracy of the dual-index method in screening for CCHD in clinical practice.
5. Conclusions
In the present study, we detailed the progress and results of the newborn screening program for CHD in the five administrative districts of south Shanghai between 2019 and 2023, and demonstrated that newborn screening program for CHD has been effectively implemented. Additionally, this retrospective cohort study based on clinical practice further confirmed that the dual-index method had high sensitivity and specificity, and a low false-positive rate. Our study suggests that the dual-index method could be applied in common hospital settings in other regions, and that infants with negative screening results should be aware of follow-up physical examination.
Author Contributions
Conceptualization, project administration, and supervision, G.H. and Y.Y.; methodology and formal analysis, Y.T.; investigation and data curation, Q.G.; software and validation, X.H., X.G., X.M., M.Y. (Miao Yang) and P.J.; writing—original draft preparation, Y.T.; writing—review and editing, all authors; funding acquisition, G.H. and Y.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Key Research and Development Program of China (grant numbers 2016YFC1000500 and 2021YFC2701004), the National Natural Science Foundation of China (grant number 82270312), the Shanghai Science and Technology Innovation Action Plan—Technical Standard Project (23DZ2203000, 24DZ2202800), the Shanghai Health Commission of Health Industry Clinical Research Project (20234Y0211), and the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (2019-I2M-5-002).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Children’s Hospital of Fudan University [2023 (132)] (Approval date: 20 June 2023).
Informed Consent Statement
Written informed consent was obtained from the patient(s) prior to publishing this paper.
Data Availability Statement
The datasets used and analyzed in this study are available from the corresponding author on reasonable request.
Acknowledgments
We would like to thank all the medical staff involved in the Newborn Screening Program for Congenital Heart Disease in Shanghai.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| CHD | Congenital heart disease |
| POX | Pulse oximetry |
| CCHD | Critical congenital heart disease |
| NICU | Neonatal intensive care unit |
| SpO2 | Pulse oximeter oxygen saturation |
| ASD | Atrial septal defect |
References
- Thoracic and Cardiovascular Surgery Branch of Chinese Medical Association. National consensus in China on perinatal diagnosis, evaluation and clinical disposal of cardiac birth defects. Chin. J. Pediatr. Surg. 2018, 39, 163–170. (In Chinese) [Google Scholar] [CrossRef]
- Tian, Y.; Hu, X.; Gu, Q.; Yang, M.; Jia, P.; Ma, X.; Ge, X.; Zhao, Q.; Liu, F.; Ye, M.; et al. Temporal trend in mortality due to congenital heart disease in China from 2008 to 2021. Chin. Med. J. 2025, 138, 693–701. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.M.; Liu, F.; Wu, L.; Ma, X.J.; Niu, C.; Huang, G.Y. Prevalence of Congenital Heart Disease at Live Birth in China. J. Pediatr. 2019, 204, 53–58. [Google Scholar] [CrossRef]
- Brown, K.L.; Ridout, D.A.; Hoskote, A.; Verhulst, L.; Ricci, M.; Bull, C. Delayed diagnosis of congenital heart disease worsens preoperative condition and outcome of surgery in neonates. Heart 2006, 92, 1298–1302. [Google Scholar] [CrossRef]
- Liberman, R.F.; Getz, K.D.; Lin, A.E.; Higgins, C.A.; Sekhavat, S.; Markenson, G.R.; Anderka, M. Delayed Diagnosis of Critical Congenital Heart Defects: Trends and Associated Factors. Pediatrics 2014, 134, E373–E381. [Google Scholar] [CrossRef]
- Plana, M.N.; Zamora, J.; Suresh, G.; Fernandez-Pineda, L.; Thangaratinam, S.; Ewer, A.K. Pulse oximetry screening for critical congenital heart defects. Cochrane Database Syst. Rev. 2018, 3, CD011912. [Google Scholar] [CrossRef] [PubMed]
- Abouk, R.; Grosse, S.D.; Ailes, E.C.; Oster, M.E. Association of US State Implementation of Newborn Screening Policies for Critical Congenital Heart Disease with Early Infant Cardiac Deaths. JAMA-J. Am. Med. Assoc. 2017, 318, 2111–2118. [Google Scholar] [CrossRef]
- Zhao, Q.M.; Ma, X.J.; Ge, X.L.; Liu, F.; Yan, W.L.; Wu, L.; Ye, M.; Liang, X.C.; Zhang, J.; Gao, Y.; et al. Pulse oximetry with clinical assessment to screen for congenital heart disease in neonates in China: A prospective study. Lancet 2014, 384, 747–754. [Google Scholar] [CrossRef]
- Hu, X.J.; Ma, X.J.; Zhao, Q.M.; Yan, W.L.; Ge, X.L.; Jia, B.; Liu, F.; Wu, L.; Ye, M.; Liang, X.C.; et al. Pulse Oximetry and Auscultation for Congenital Heart Disease Detection. Pediatrics 2017, 140, e20171154. [Google Scholar] [CrossRef]
- Ma, X.J.; Tian, Y.P.; Ma, F.C.; Ge, X.L.; Gu, Q.; Huang, M.; Zhang, Y.Q.; Sun, K.; Hu, X.J.; Yang, M.; et al. Impact of Newborn Screening Programme for Congenital Heart Disease in Shanghai: A five-year observational study in 801,831 newborns. Lancet Reg. Health-West. Pac. 2023, 33, 100688. [Google Scholar] [CrossRef]
- Zhou, F.Y.; Li, C.; Qin, K.Z.; Luo, C.; Huang, H.F.; Wu, Y.T. Delivery and neonatal outcomes of pregnant women during the Shanghai lockdown: A retrospective analysis. Front. Pediatr. 2023, 11, 992908. [Google Scholar] [CrossRef] [PubMed]
- Deng, H.M.; Jin, Y.P.; Sheng, M.M.; Liu, M.; Shen, J.; Qian, W.; Zou, G.; Liao, Y.X.; Liu, T.F.; Ling, Y.; et al. Safety and efficacy of COVID-19 vaccine immunization during pregnancy in 1024 pregnant women infected with the SARS-CoV-2 Omicron virus in Shanghai, China. Front. Immunol. 2024, 14, 1303058. [Google Scholar] [CrossRef]
- Ewer, A.K.; Middleton, L.J.; Furmston, A.T.; Bhoyar, A.; Daniels, J.P.; Thangaratinam, S.; Deeks, J.J.; Khan, K.S.; Grp, P.S. Pulse oximetry screening for congenital heart defects in newborn infants (PulseOx): A test accuracy study. Lancet 2011, 378, 785–794. [Google Scholar] [CrossRef]
- Sun, S.Y.; Xie, Z.; Yu, K.T.; Jiang, B.Q.; Zheng, S.W.; Pan, X.T. COVID-19 and healthcare system in China: Challenges and progression for a sustainable future. Glob. Health 2021, 17, 14. [Google Scholar] [CrossRef] [PubMed]
- Singh, Y.; Chen, S.E. Impact of pulse oximetry screening to detect congenital heart defects: 5 years’ experience in a UK regional neonatal unit. Eur. J. Pediatr. 2022, 181, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.H.; Sun, Y.; Zhu, J.J.; Zhu, Y.N.; Qiu, L.Q. Epidemiology, prenatal diagnosis, and neonatal outcomes of congenital heart defects in eastern China: A hospital-based multicenter study. BMC Pediatr. 2020, 20, 416. [Google Scholar] [CrossRef]
- Li, M.; Ye, B.; Chen, Y.; Gao, L.; Wu, Y.; Cheng, W. Analysis of genetic testing in fetuses with congenital heart disease of single atria and/or single ventricle in a Chinese prenatal cohort. BMC Pediatr. 2023, 23, 577. [Google Scholar] [CrossRef]
- Tomek, V.; Jicinska, H.; Pavlicek, J.; Kovanda, J.; Jehlicka, P.; Klaskova, E.; Mrazek, J.; Cutka, D.; Smetanova, D.; Brestak, M.; et al. Pregnancy Termination and Postnatal Major Congenital Heart Defect Prevalence After Introduction of Prenatal Cardiac Screening. JAMA Netw. Open 2023, 6, e2334069. [Google Scholar] [CrossRef]
- Liu, Y.J.; Chen, S.; Zühlke, L.; Black, G.C.; Choy, M.K.; Li, N.X.; Keavney, B.D. Global birth prevalence of congenital heart defects 1970-2017: Updated systematic review and meta-analysis of 260 studies. Int. J. Epidemiol. 2019, 48, 455–463. [Google Scholar] [CrossRef]
- Abbas, A.; Ewer, A.K. New born pulse oximetry screening: A global perspective. Early Hum. Dev. 2021, 162, 105457. [Google Scholar] [CrossRef]
- Ailes, E.C.; Gilboa, S.M.; Honein, M.A.; Oster, M.E. Estimated Number of Infants Detected and Missed by Critical Congenital Heart Defect Screening. Pediatrics 2015, 135, 1000–1008. [Google Scholar] [CrossRef] [PubMed]
- Oddie, S.; Stenson, B.; Wyllie, J.; Ewer, A.K. UK consultation on pulse oximetry screening for critical congenital heart defects in newborns. Lancet 2019, 394, 103–104. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the International Society for Neonatal Screening. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).