The Benign Mimickers of Carcinoma on Breast MRI
Abstract
Introduction
Discussion
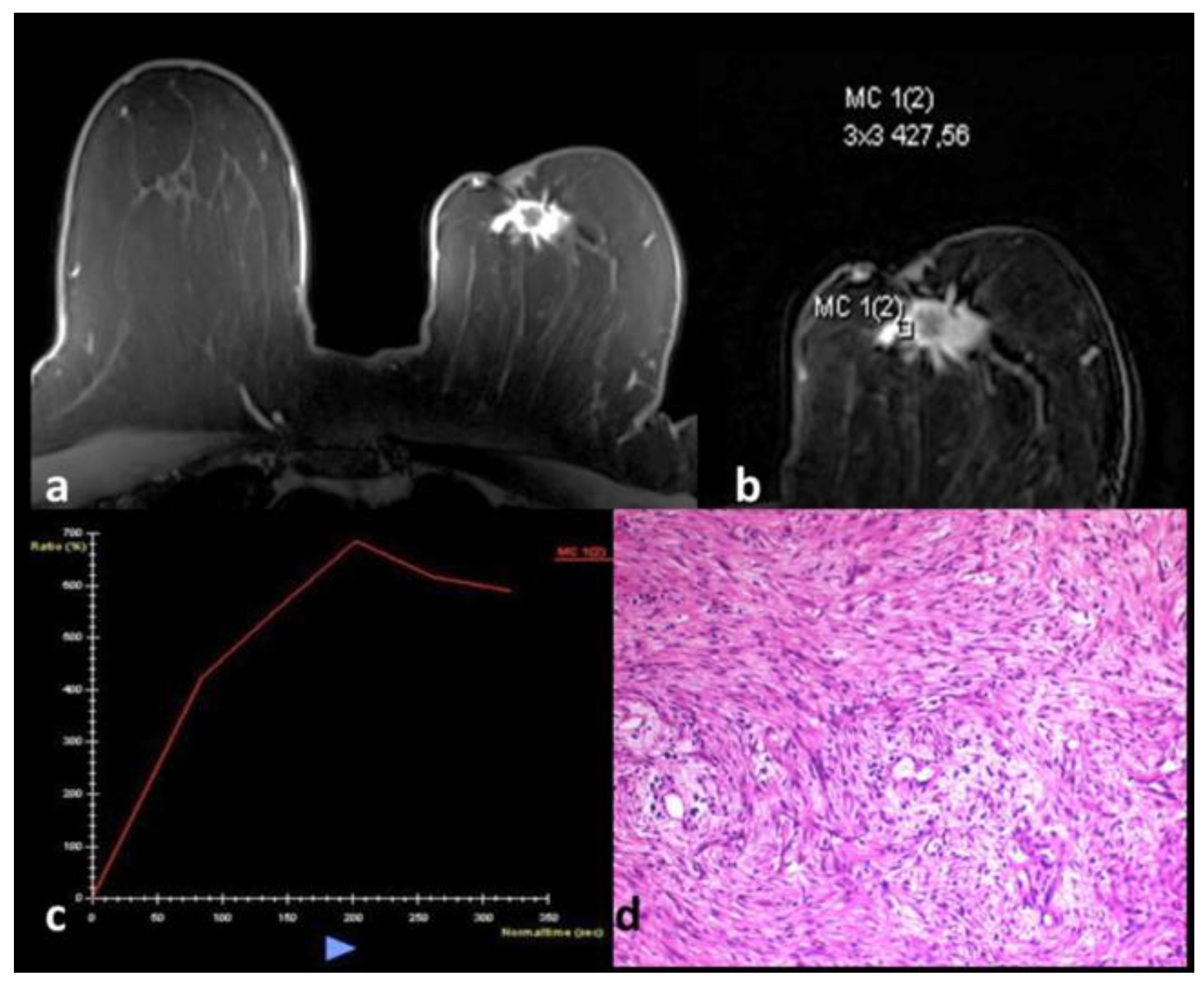
Adenomyoepithelioma
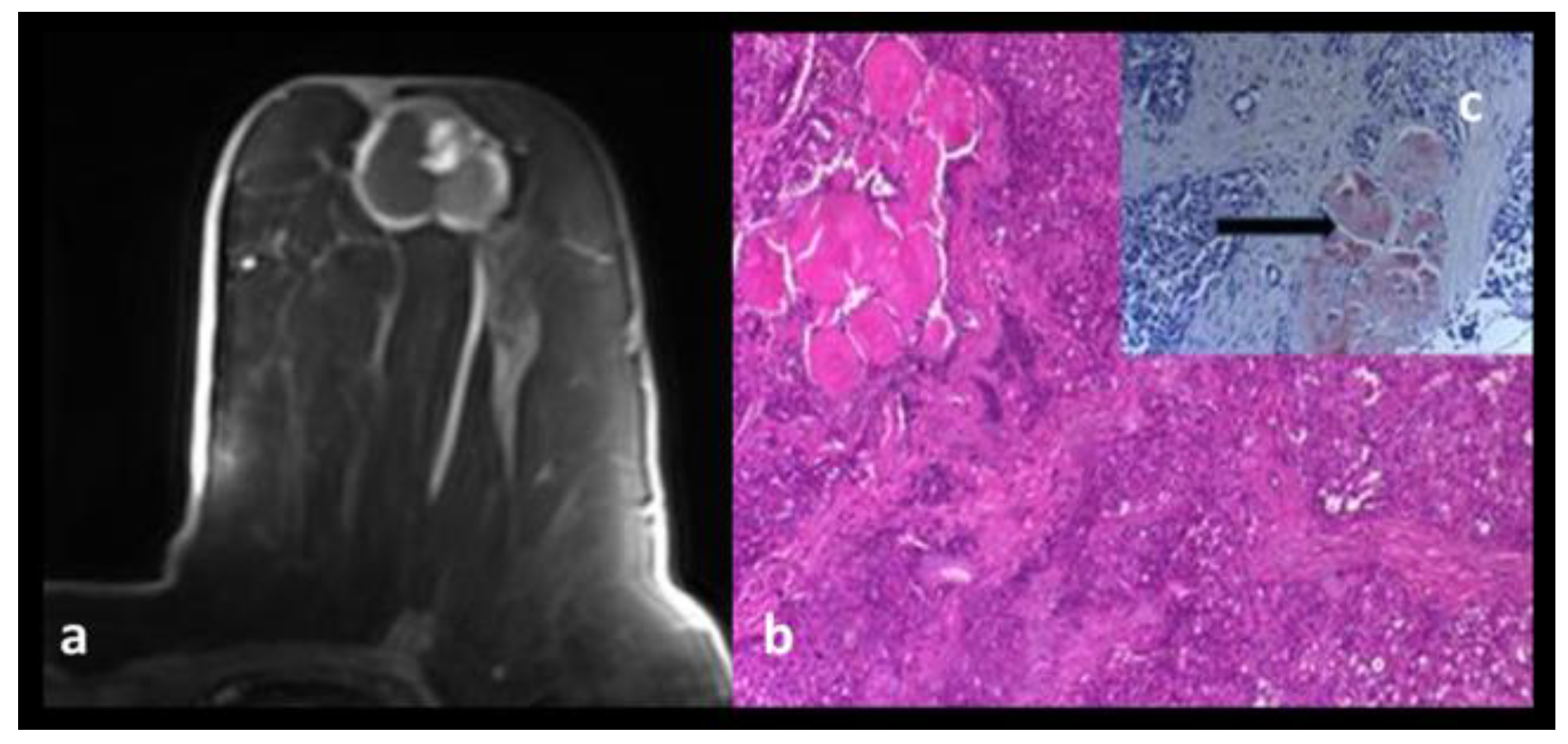
Amyloidosis
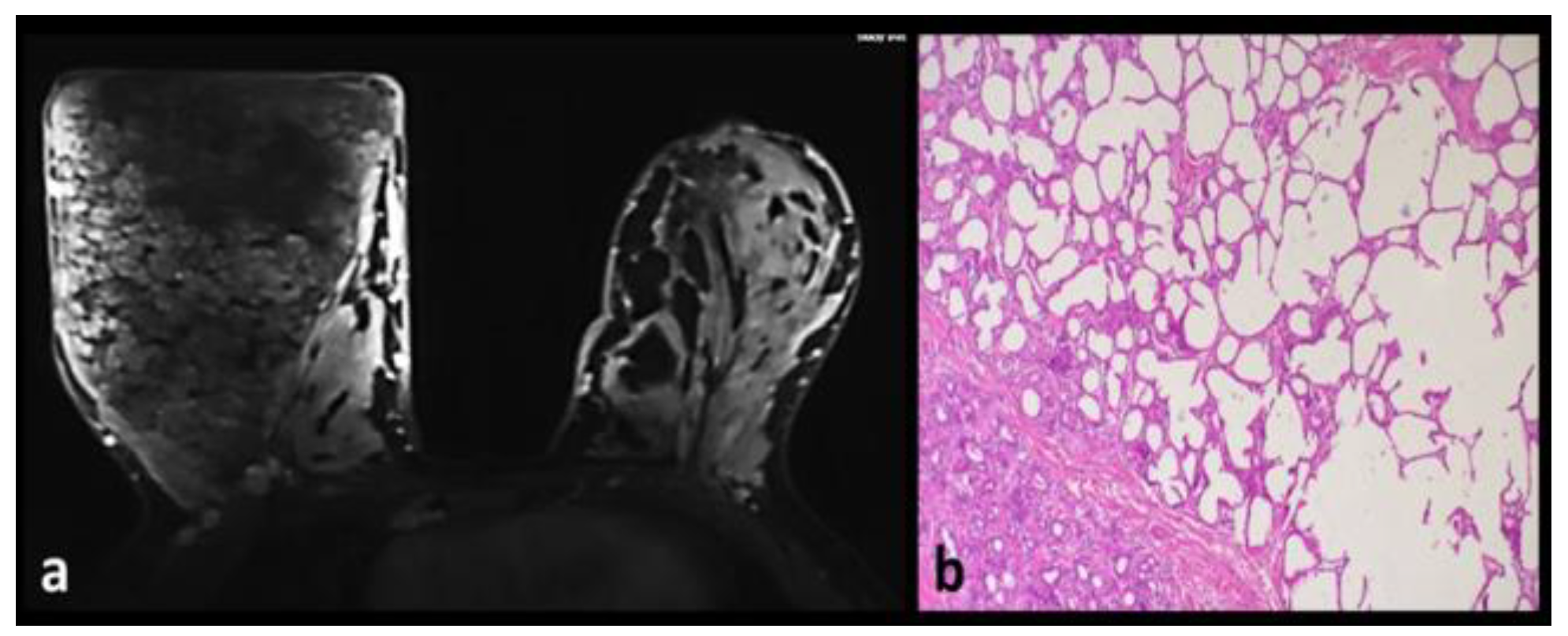
Angiolipoma
Apocrine Metaplasia
Breast Abscesses
Diabetic Mastopathy
Fat Necrosis
Fibrocystic Changes
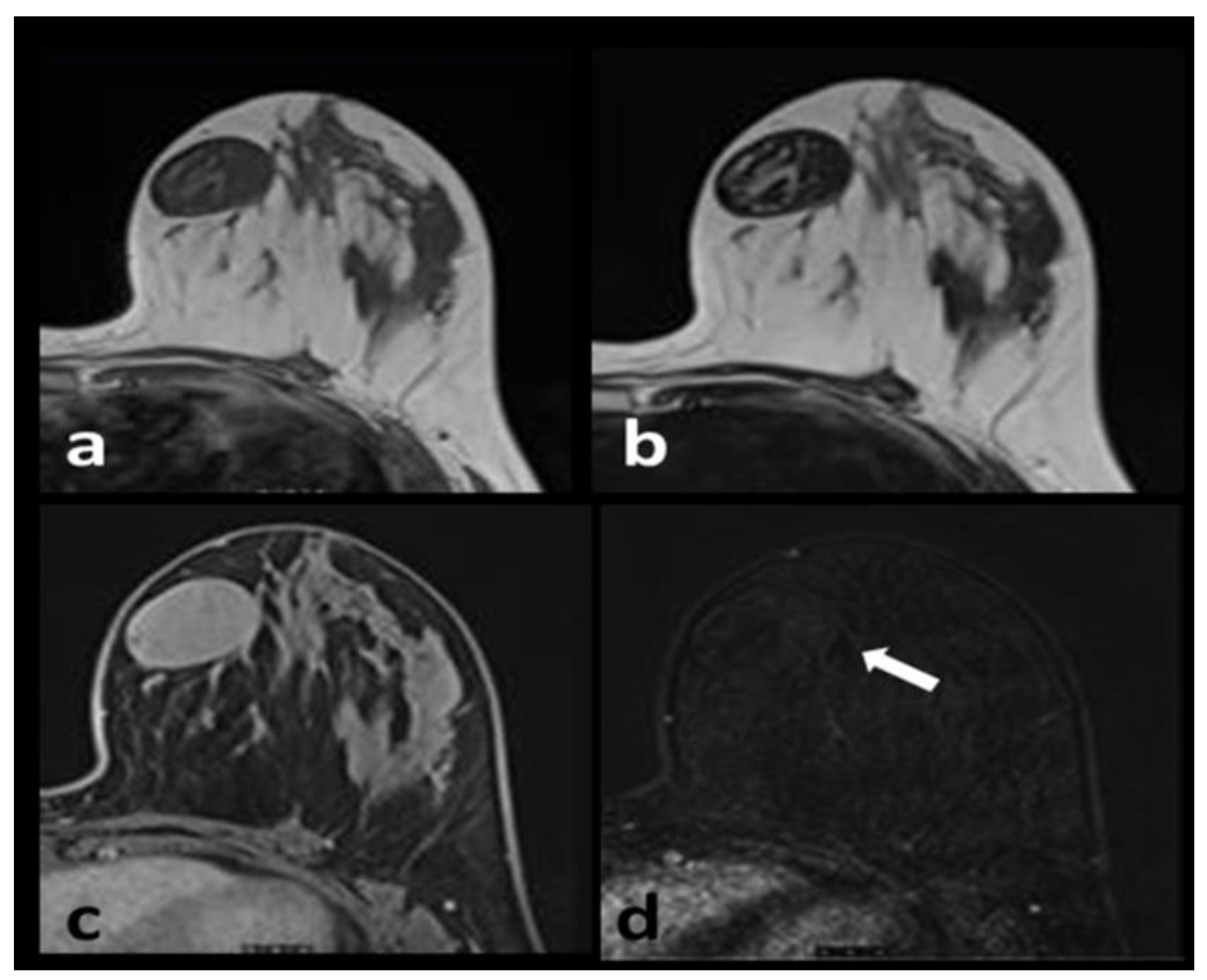
Fibromatosis
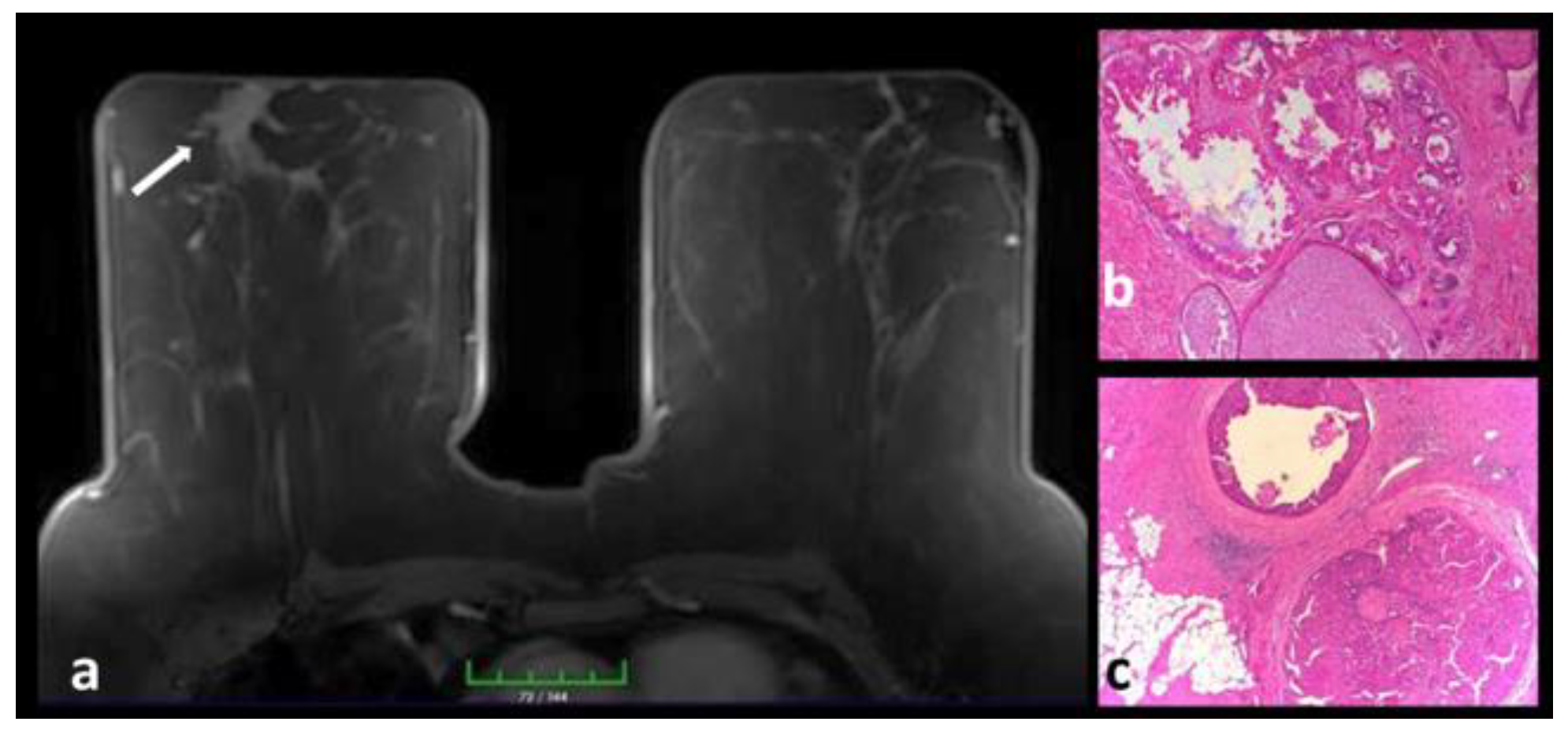
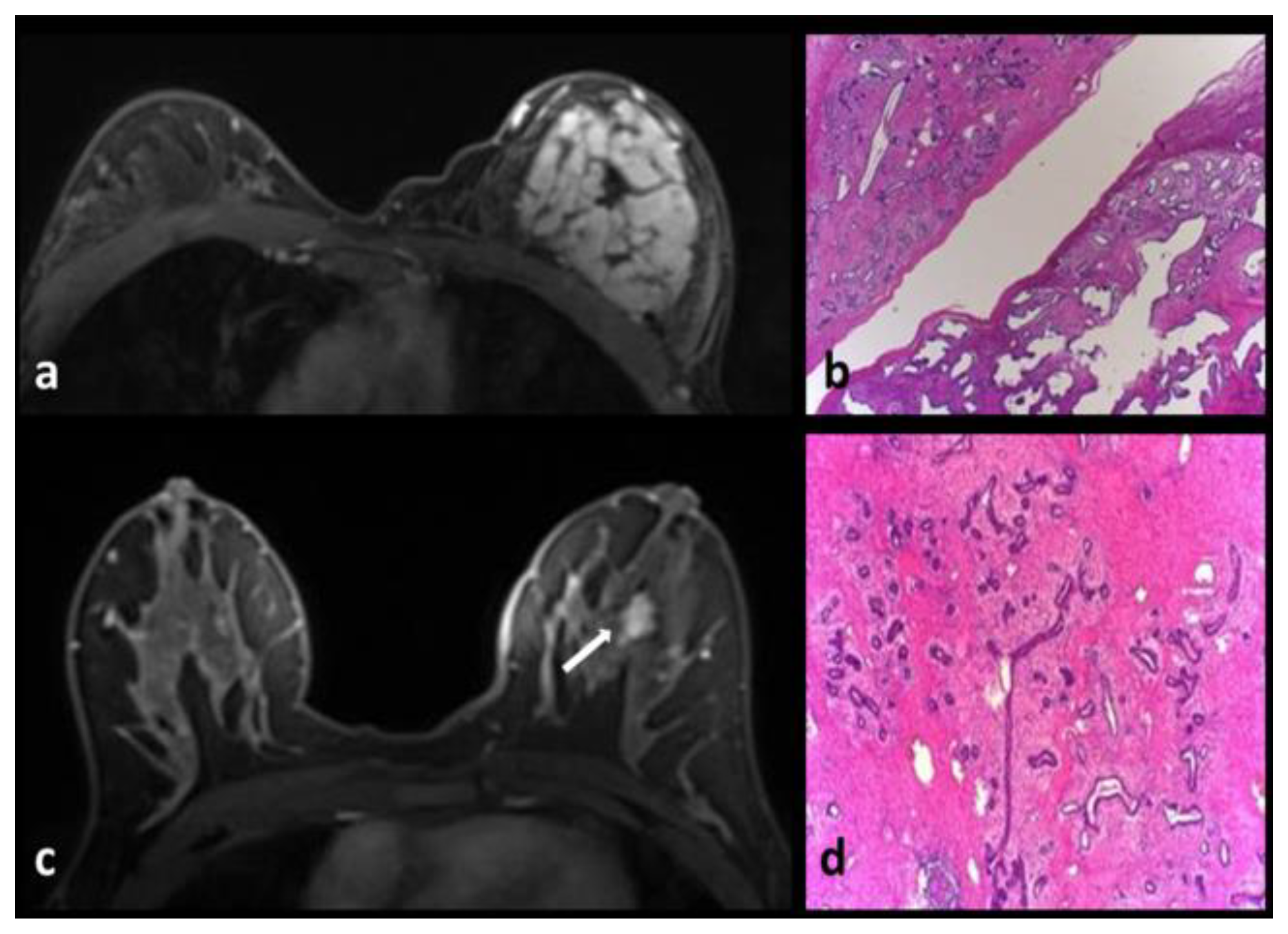
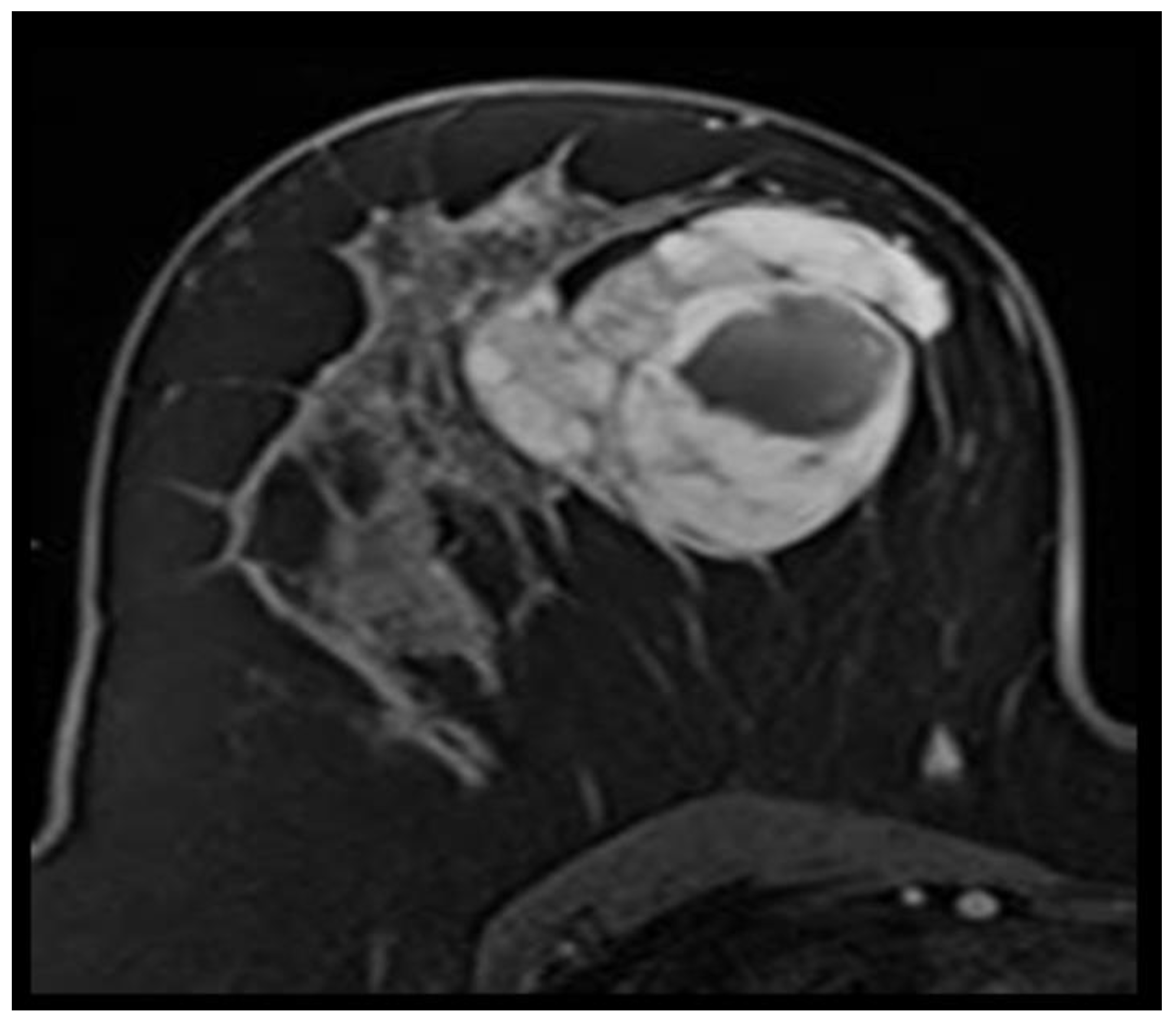
Juvenile Papillomatosis
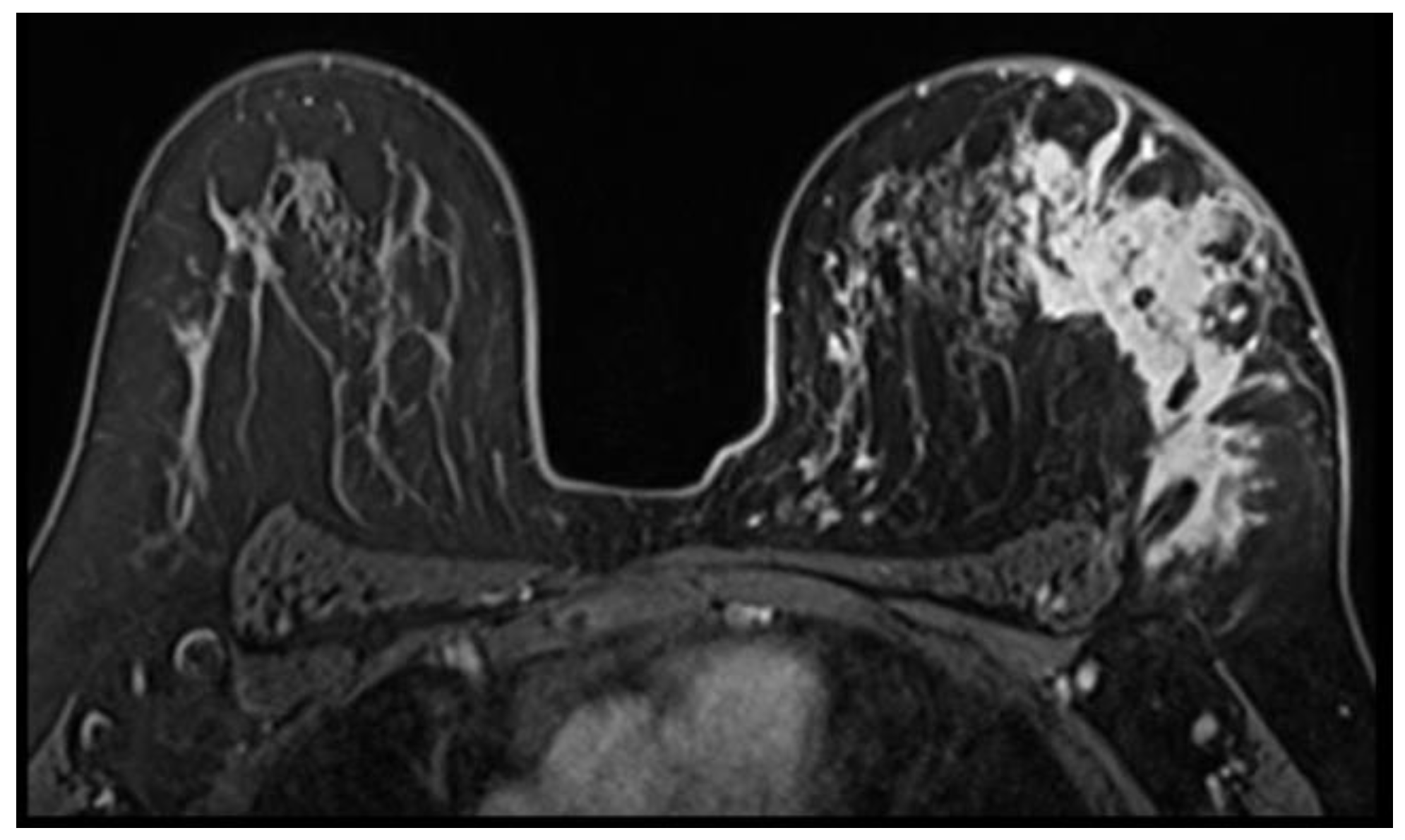
Idiopathic Granulomatous Mastitis
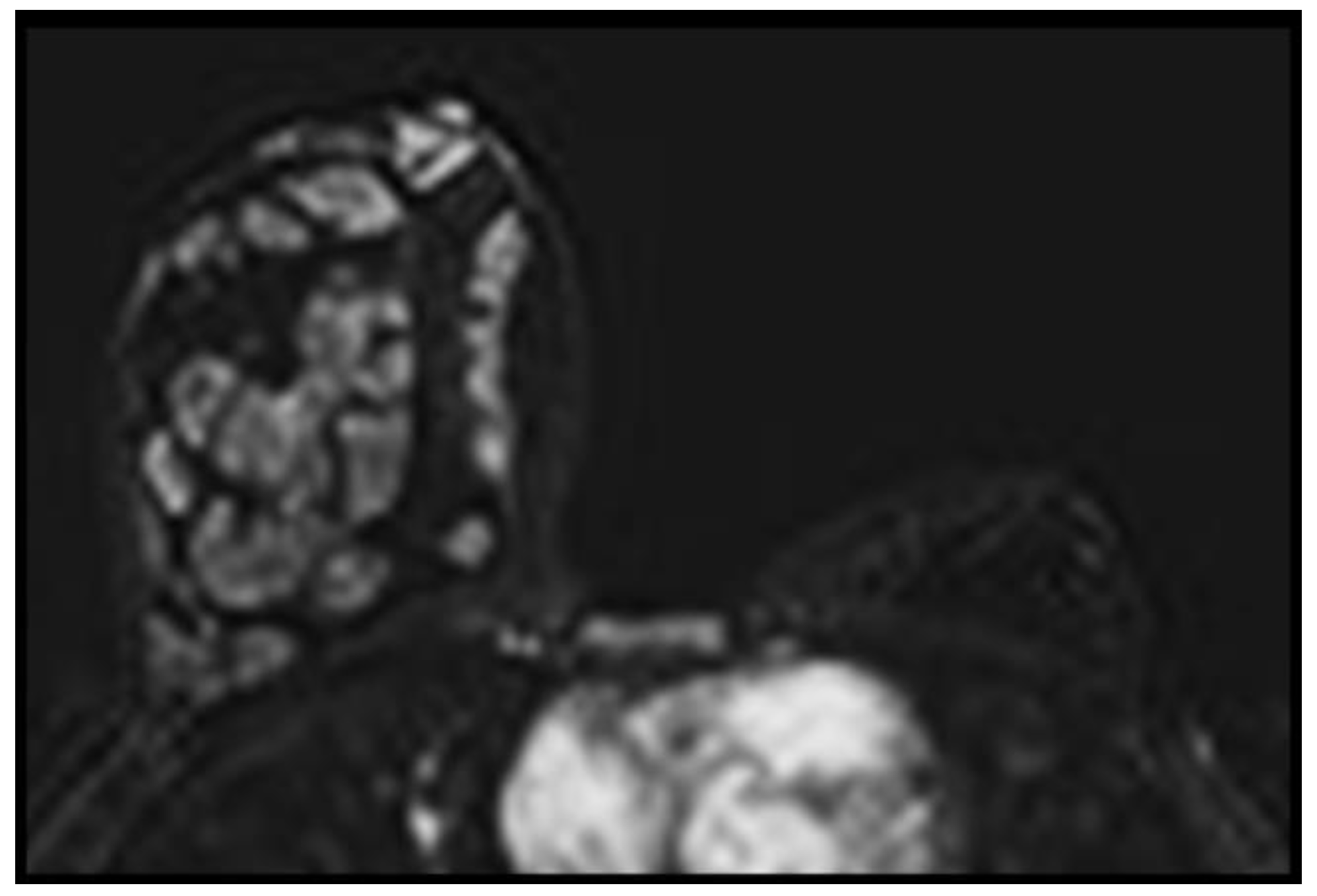
Intraductal Papilloma-Intraductal Papillomatosis
Intramammary Lymph Node
Lactating Adenoma
Phyllodes tumors
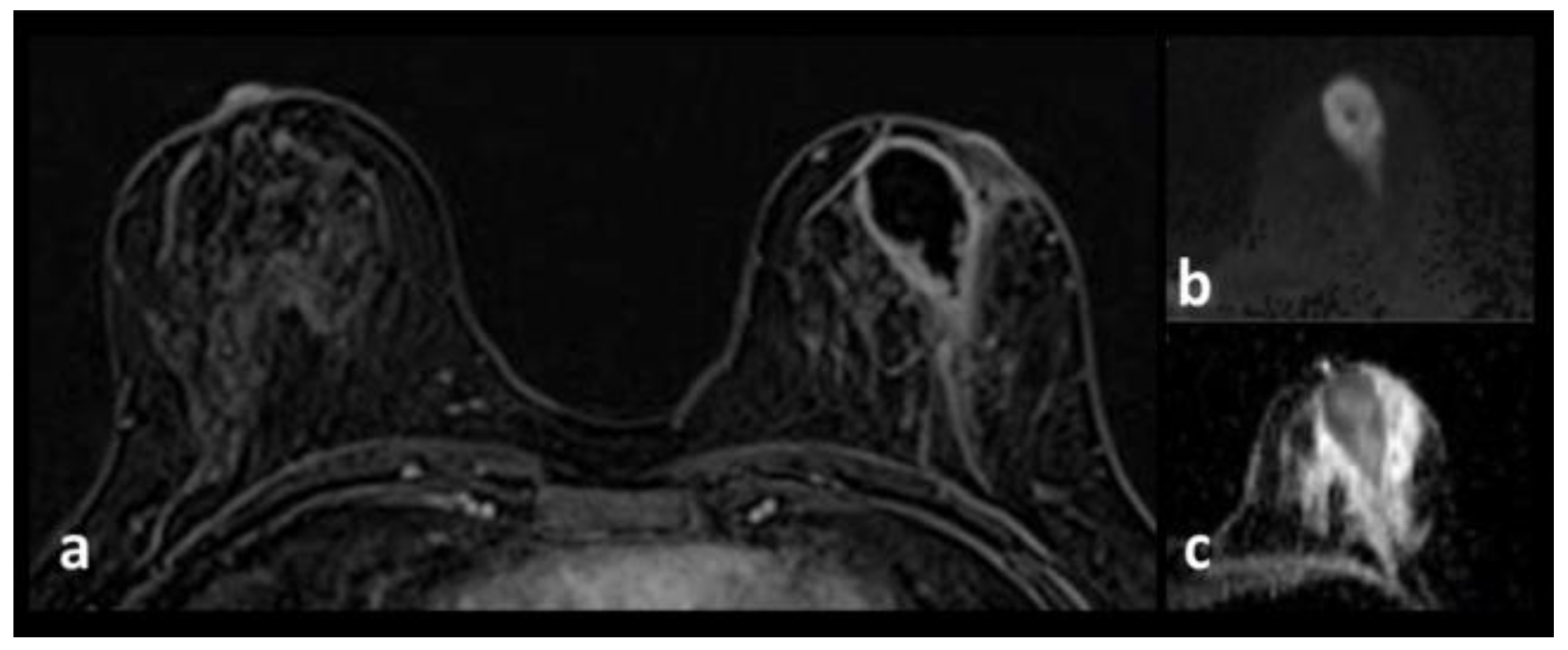
Pseudoangiomatous stromal hyperplasia
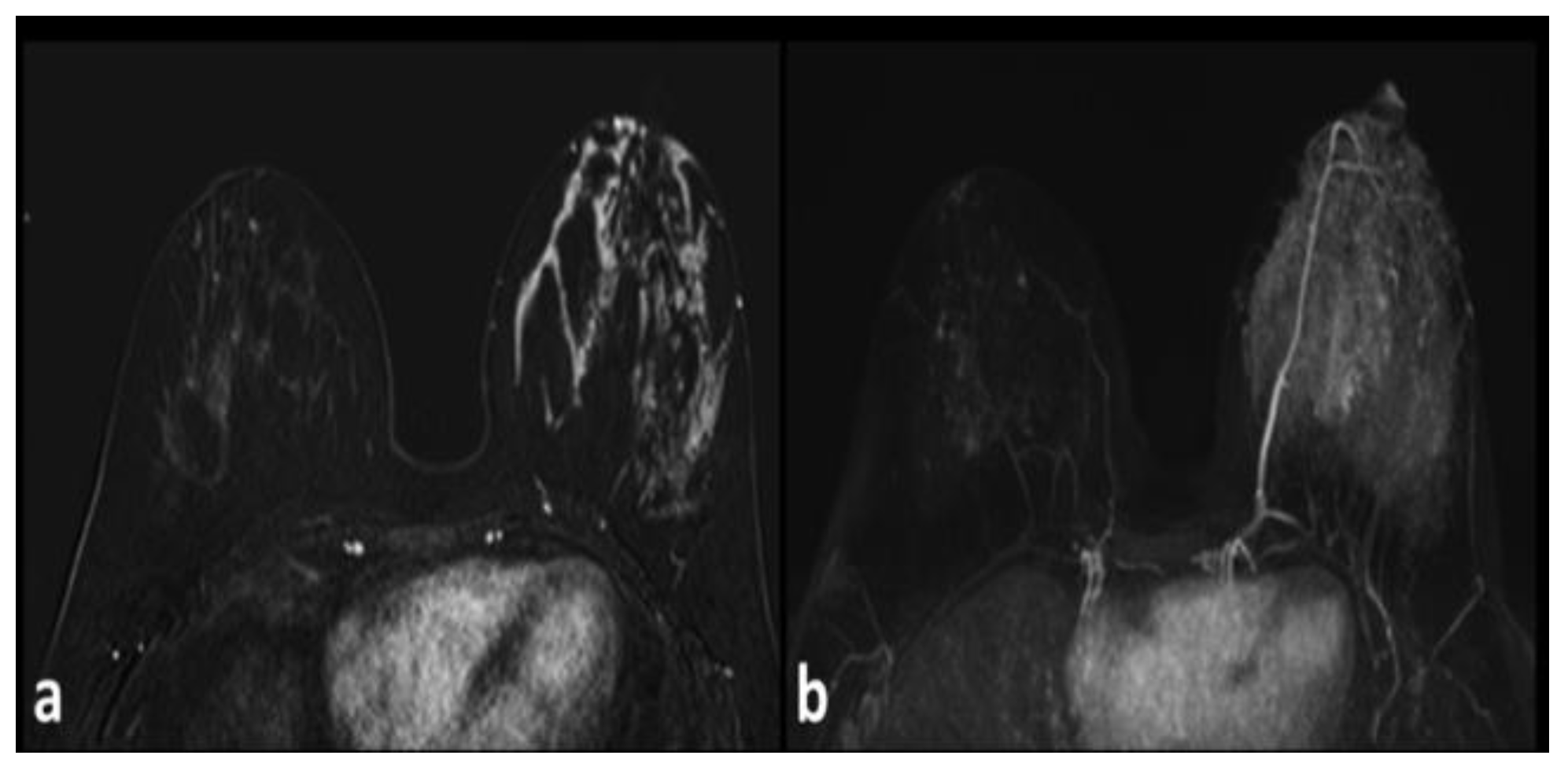
Unilateral Lactation
Sclerosing Adenosis
Surgery and Radiotherapy
Conclusions
Conflict of interest disclosure
Compliance with ethical standards
Acknowledgments
Author contribution statement
References
- Ruiz-Delgado, M.L.; López-Ruiz, J.A.; Eizaguirre, B.; Saiz, A.; Astigarraga, E.; Fernández-Temprano, Z. Benign adenomyoepithelioma of the breast: imaging findings mimicking malignancy and histopathological features. Acta Radiol. 2007, 48, 27–29. [Google Scholar] [CrossRef] [PubMed]
- O'Brien, J.; Aherne, S.; McCormack, O.; Jeffers, M.; McInerney, D. MRI features of bilateral amyloidosis of breast. Breast J. 2013, 19, 338–339. [Google Scholar] [CrossRef] [PubMed]
- Killian, J.K.; Merino, M.; Bondy, C.; Bakalov, V.; Chow, C. MRI of angiolipoma of the breast in Turner's syndrome. AJR Am J Roentgenol. 2004, 183, 1843–1844. [Google Scholar] [CrossRef]
- Gao, Y.; Dialani, V.; DeBenedectis, C.; Johnson, N.; Brachtel, E.; Slanetz, P. Apocrine Metaplasia Found at MR Biopsy: Is There Something to be Learned? Breast J. 2017, 23, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Durur-Subasi, I.; Durur-Karakaya, A.; Karaman, A.; Seker, M.; Demirci, E.; Alper, F. Is the necrosis/wall ADC ratio useful for the differentiation of benign and malignant breast lesions? Br J Radiol. 2017, 90, 20160803. [Google Scholar] [CrossRef]
- Accurso, A.; Della Corte, G.A.; Rocco, N.; Varone, V.; Buonaiuto, R.; Compagna, R.; Tari, D.U.; Amato, B.; Riccardi, A. Unusual breast lesion mimicking cancer: diabetic mastopathy. Int J Surg. 2014, 12 (Suppl 1), S79–82. [Google Scholar] [CrossRef][Green Version]
- Kuhl, C.K. Concepts for differential diagnosis in breast MR imaging. Magn Reson Imaging Clin N Am. 2006, 14, 305–328. [Google Scholar] [CrossRef]
- Lazar, A.L.; Vulturar, R.; Fodor, A.; et al. The molecular mechanisms linking metabolic syndrome to endometrial and breast cancers. J Mind Med Sci. 2021, 8, 167–178. [Google Scholar] [CrossRef]
- Chen, J.H.; Nalcioglu, O.; Su, M.Y. Fibrocystic change of the breast presenting as a focal lesion mimicking breast cancer in MR imaging. J Magn Reson Imaging. 2008, 28, 1499–1505. [Google Scholar] [CrossRef]
- Xu, Y.; Liu, P.; Lu, H.; Zhang, S.; Zhu, Y. Imaging manifestation of mammary fibromatosis. Breast J. 2013, 19, 673–675. [Google Scholar] [CrossRef]
- Yalagachin, G.; Lakshmikantha, N.; Mashal, S.B.; Yalagachin, G.; Lakshmikantha, N.; Mashal, S.B. Prevalence of nodular goiter in patients with breast diseases. J Clin Invest Surg. 2020, 5, 91–95. [Google Scholar] [CrossRef]
- Durur-Subasi, I.; Alper, F.; Akcay, M.N.; Demirci, E.; Gundogdu, C. Magnetic resonance imaging findings of breast juvenile papillomatosis. Jpn J Radiol. 2013, 31, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Durur-Subasi, I. DW-MRI of the breast: a pictorial review. Insights Imaging. 2019, 10, 61. [Google Scholar] [CrossRef] [PubMed]
- van Oers, H.; Schlebusch, L. Indicators of psychological distress and body image disorders in female patients with breast cancer. J Mind Med Sci. 2020, 7, 179–187. [Google Scholar] [CrossRef]
- Ucar, E.A.; Durur-Subasi, I.; Yilmaz, K.B.; Arikok, A.T.; Hekimoglu, B. Quantitative perfusion parameters of benign inflammatory breast pathologies: A descriptive study. Clin Imaging. 2020, 68, 249–256. [Google Scholar] [CrossRef]
- Durur-Subasi, I.; Durur-Karakaya, A.; Alper, F.; Karaman, A.; Kılıc, R.M.; Sipal, S.; Demirci, E.; Akcay, M.N. Breast lesions with high signal intensity on T1-weighted MR images. Jpn J Radiol. 2013, 31, 653–661. [Google Scholar] [CrossRef]
- Duman, L.; Gezer, N.S.; Balcı, P.; Altay, C.; Başara, I.; Durak, M.G.; Sevinç, A.I. Differentiation between Phyllodes Tumors and Fibroadenomas Based on Mammographic Sonographic and MRI Features. Breast Care (Basel). 2016, 11, 123–127. [Google Scholar] [CrossRef]
- Jones, K.N.; Glazebrook, K.N.; Reynolds, C. Pseudoangiomatous stromal hyperplasia: imaging findings with pathologic and clinical correlation. AJR Am J Roentgenol. 2010, 195, 1036–1042. [Google Scholar] [CrossRef]
- Marinescu, S.A.; Bejinariu, C.G.; Şapte, E.; Marinaş, M.C.; Giuglea, C. Complications related to breast reconstruction after mastectomy using multiple surgical techniques - a national and international comparative analysis. Rom J Morphol Embryol. 2019, 60, 87–93. [Google Scholar]
- Motofei, I.G. Biology of cancer; from cellular and molecular mechanisms to developmental processes and adaptation. Semin Cancer Biol 2021, S1044-579X(21)00253-4. [Google Scholar] [CrossRef]
- Andrei, C.A.; Scăunașu, R.V.; Simionescu, A.A.; Burcoș, T.; Lupușoru, M.D.; Lica, G. The incidence of haemorrhagic and thrombo-embolic events after breast cancer surgery in patients treated with pharmacological thrombo-prophylaxis. J Clin Invest Surg. 2019, 4, 10–18. [Google Scholar] [CrossRef]
- Miricescu, D.; Diaconu, C.C.; Stefani, C.; Stanescu, A.M.A.; Totan, A.; Rusu, I.R.; et al. The Serine/Threonine Protein Kinase (Akt)/ Protein Kinase B (PkB) Signaling Pathway in Breast Cancer. J Mind Med Sci. 2020, 7, 34–39. [Google Scholar] [CrossRef]

© 2022 by the author. 2022 Irmak Durur-Subasi, Adem Karaman, Elif Demirci, Sare Sipal, Mufide Nuran Akcay
Share and Cite
Durur-Subasi, I.; Karaman, A.; Demirci, E.; Sipal, S.; Akcay, M.N. The Benign Mimickers of Carcinoma on Breast MRI. J. Mind Med. Sci. 2022, 9, 96-101. https://doi.org/10.22543/7674.91.P96101
Durur-Subasi I, Karaman A, Demirci E, Sipal S, Akcay MN. The Benign Mimickers of Carcinoma on Breast MRI. Journal of Mind and Medical Sciences. 2022; 9(1):96-101. https://doi.org/10.22543/7674.91.P96101
Chicago/Turabian StyleDurur-Subasi, Irmak, Adem Karaman, Elif Demirci, Sare Sipal, and Mufide Nuran Akcay. 2022. "The Benign Mimickers of Carcinoma on Breast MRI" Journal of Mind and Medical Sciences 9, no. 1: 96-101. https://doi.org/10.22543/7674.91.P96101
APA StyleDurur-Subasi, I., Karaman, A., Demirci, E., Sipal, S., & Akcay, M. N. (2022). The Benign Mimickers of Carcinoma on Breast MRI. Journal of Mind and Medical Sciences, 9(1), 96-101. https://doi.org/10.22543/7674.91.P96101


