Non-Dental Oral Cavity Findings in Gastroesophageal Reflux Disease: A Systematic Review and Meta-Analysis
Abstract
Introduction
Discussions
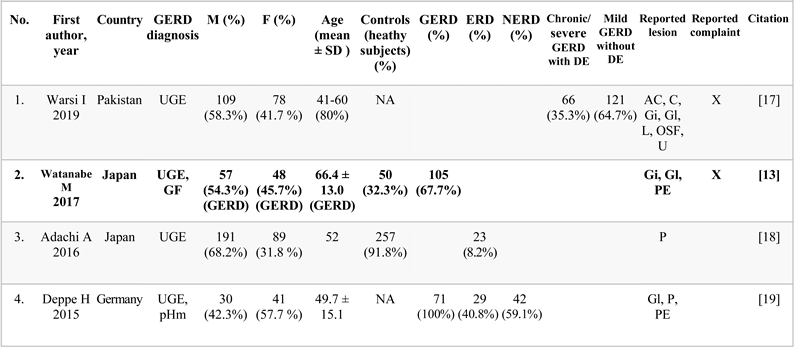
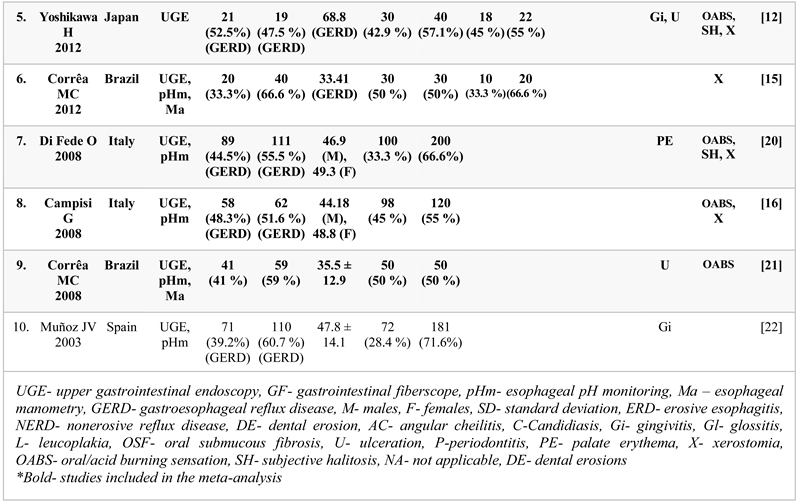
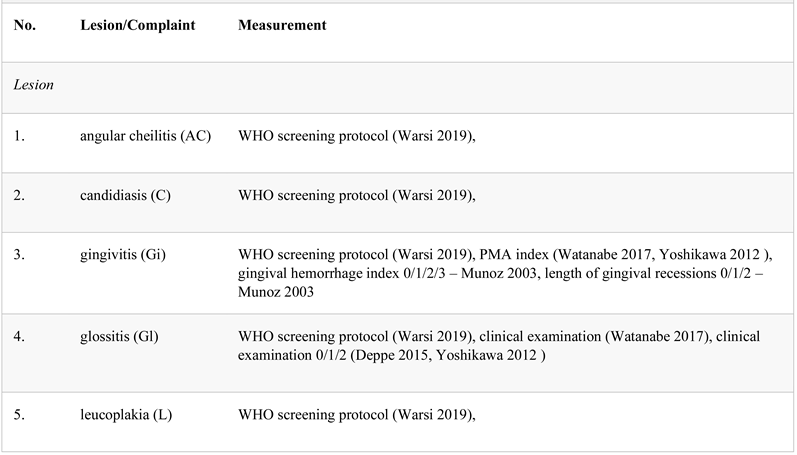
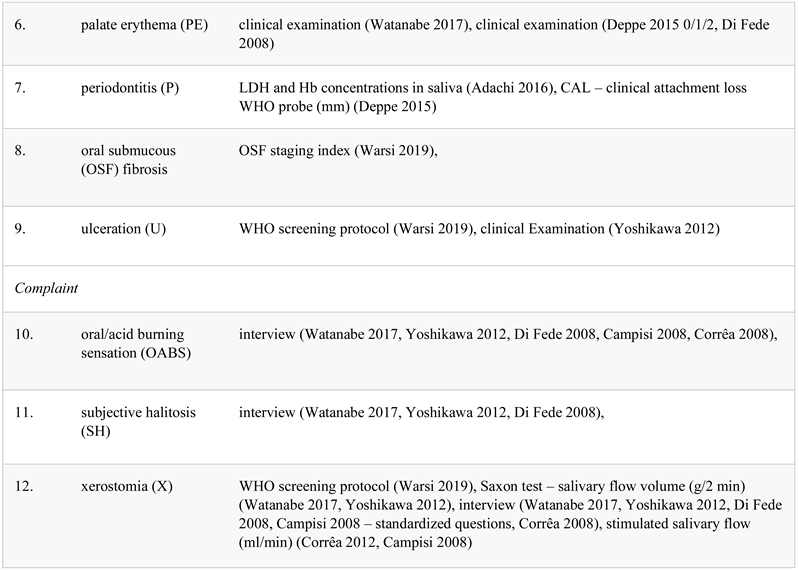
WHO- World Health Organization, PMA- papillary marginal attachment index, LDH- lactate dehydrogenase, Hb- hemoglobin, OSF- oral submucous fibrosis
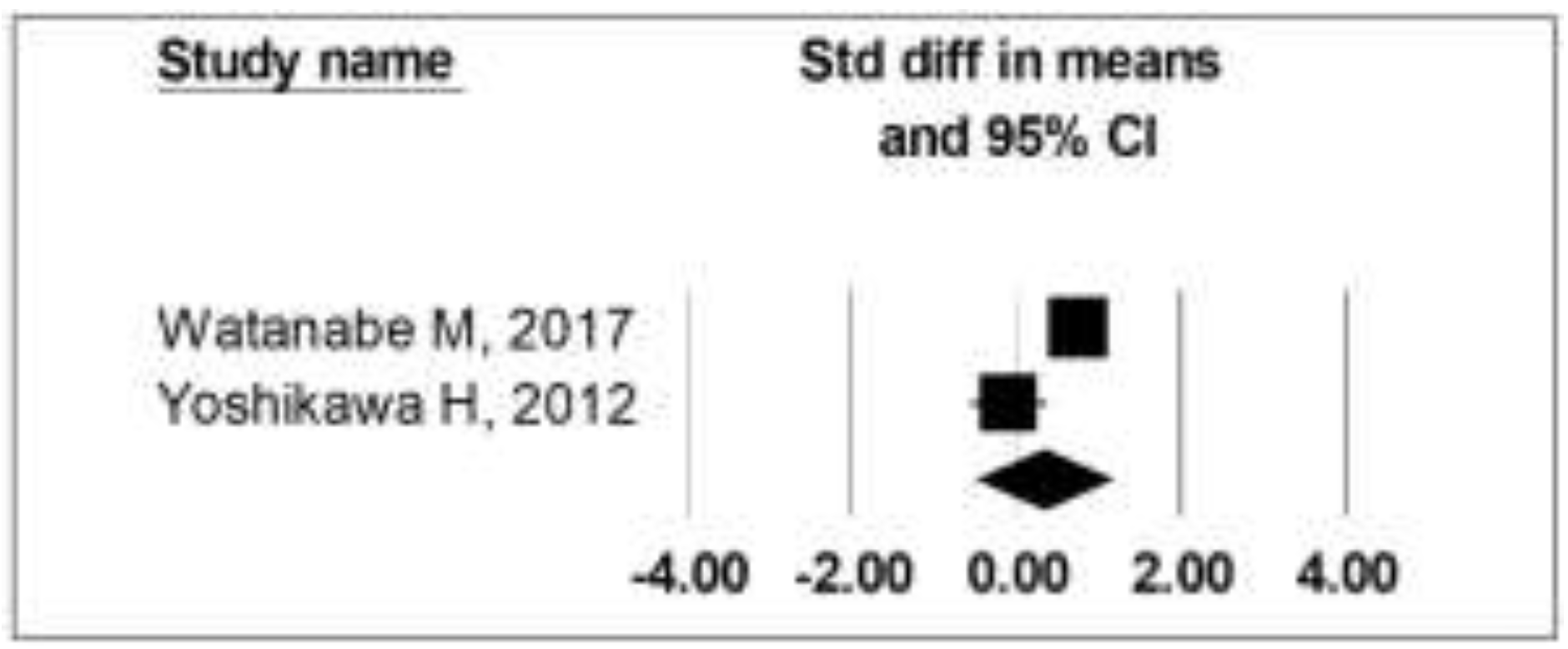
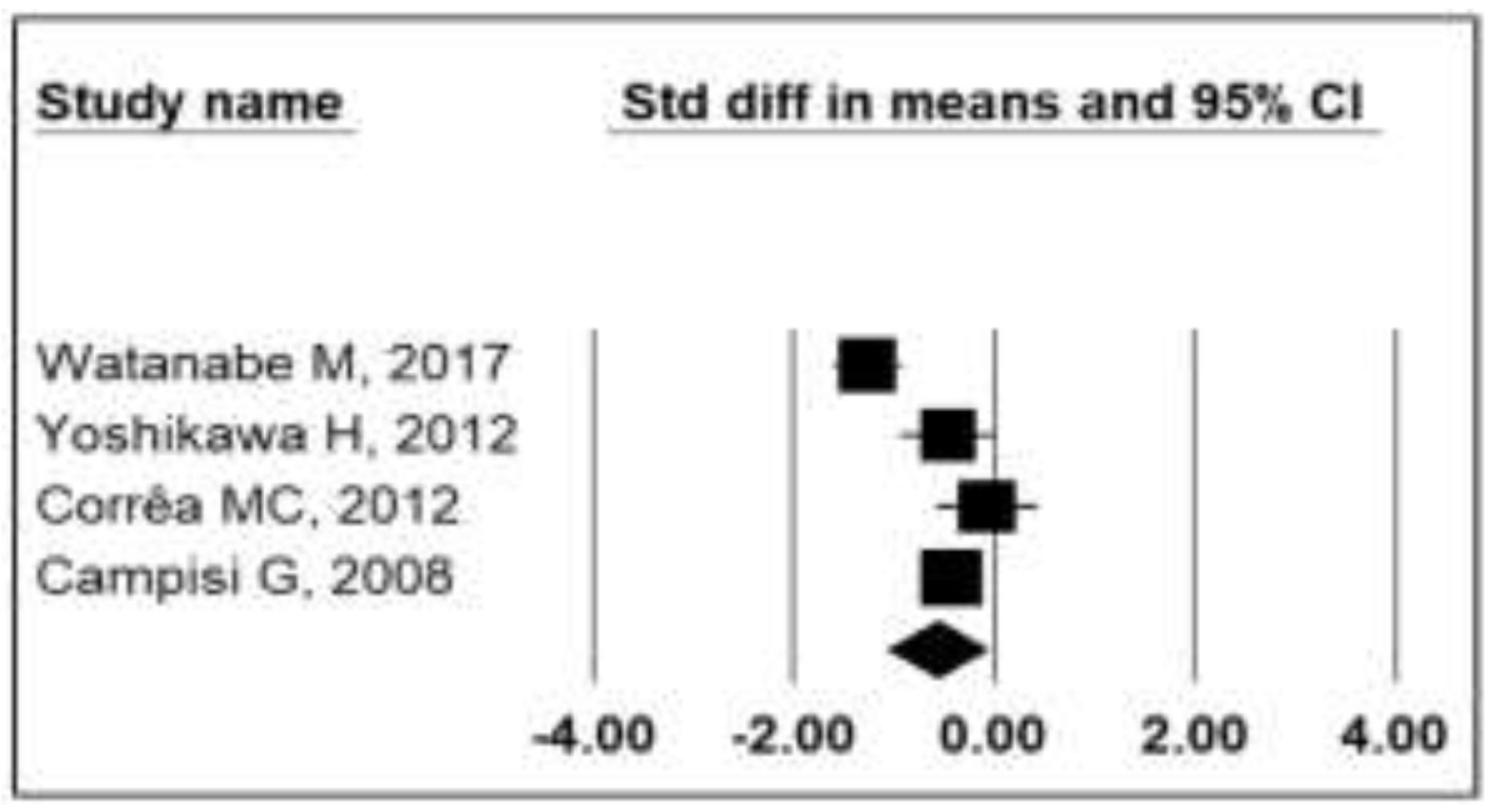
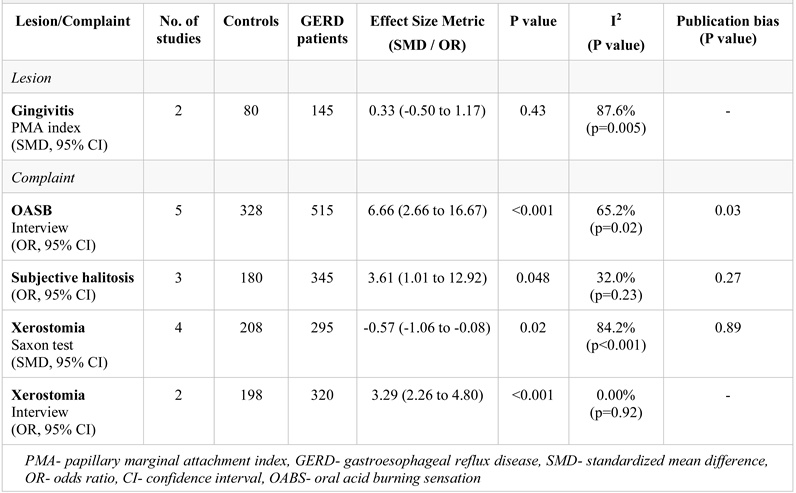
PMA- papillary marginal attachment index, GERD- gastroesophageal reflux disease, CI- confidence interval
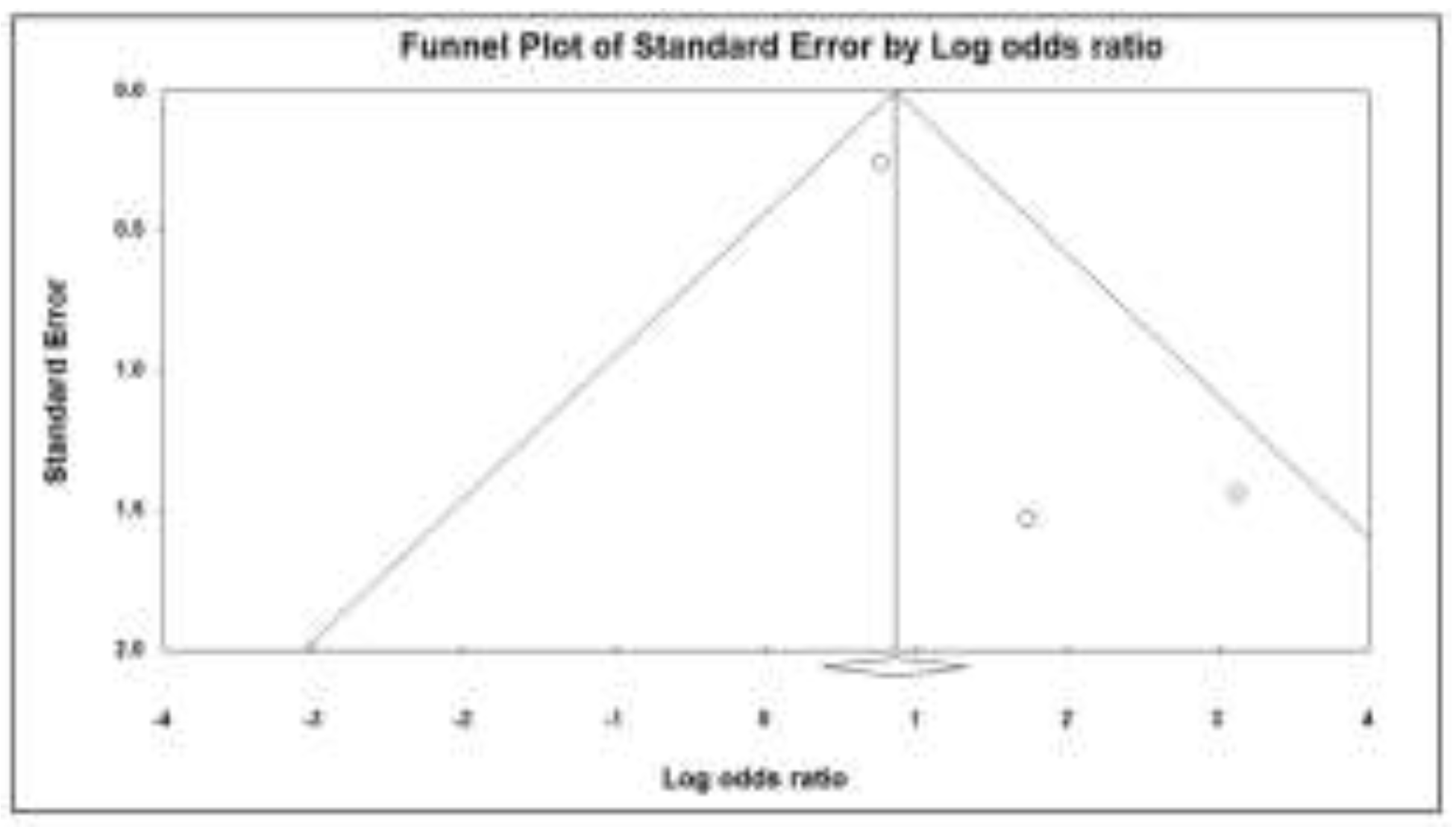
OABS- oral acid burning sensation, GERD- gastroesophageal reflux disease
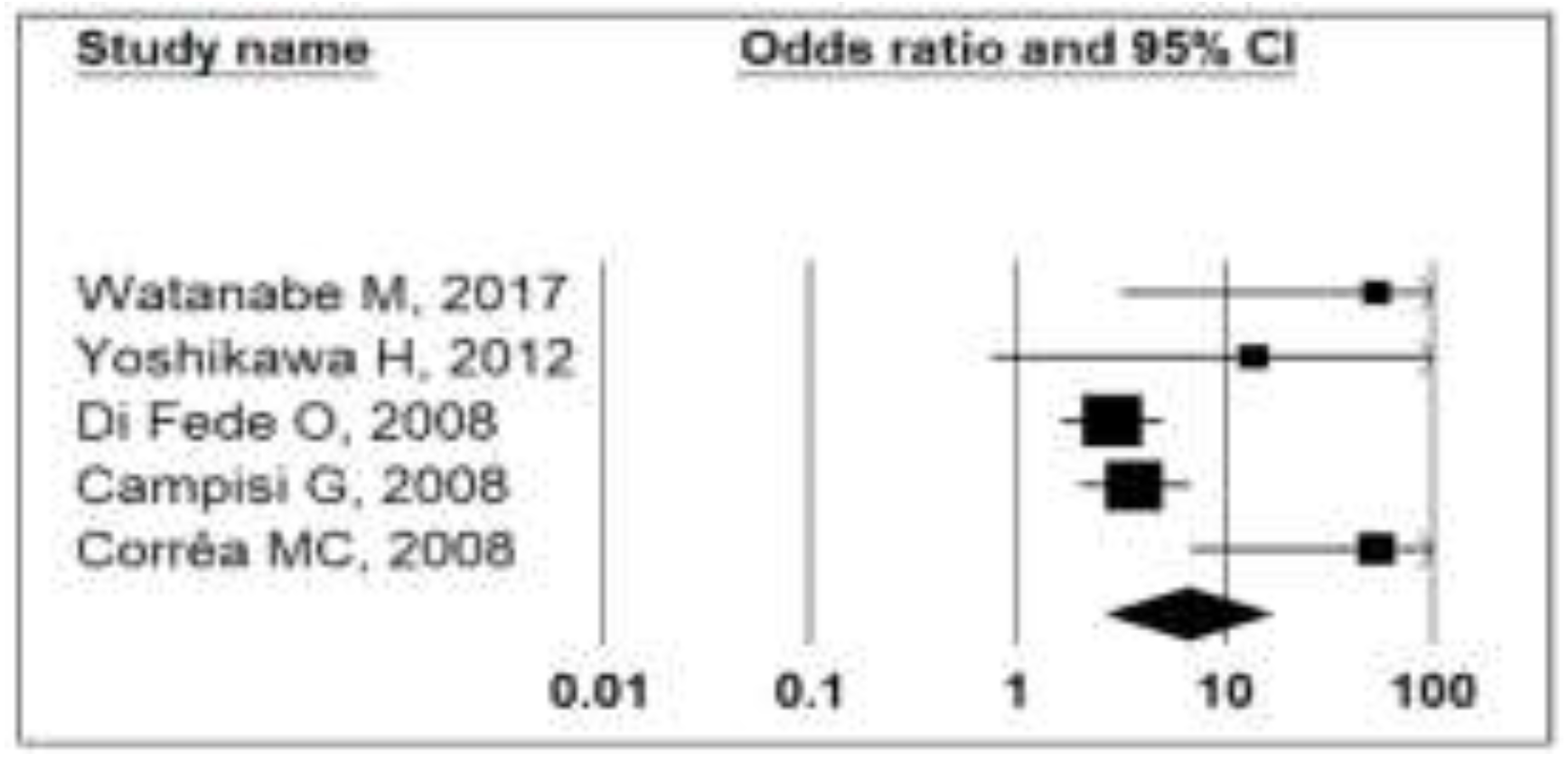
GERD- gastroesophageal reflux disease, CI- confidence interval
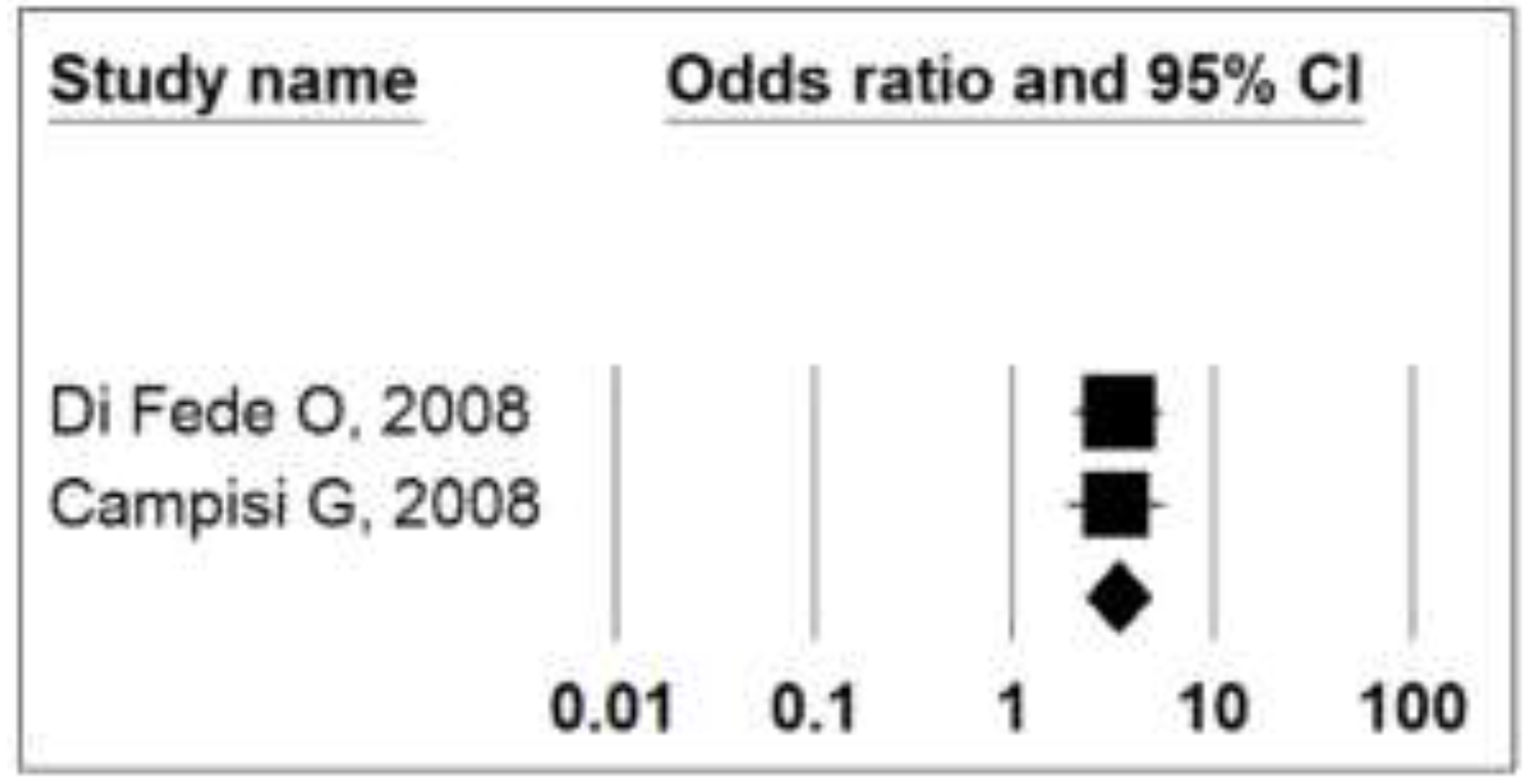
GERD- gastroesophageal reflux disease
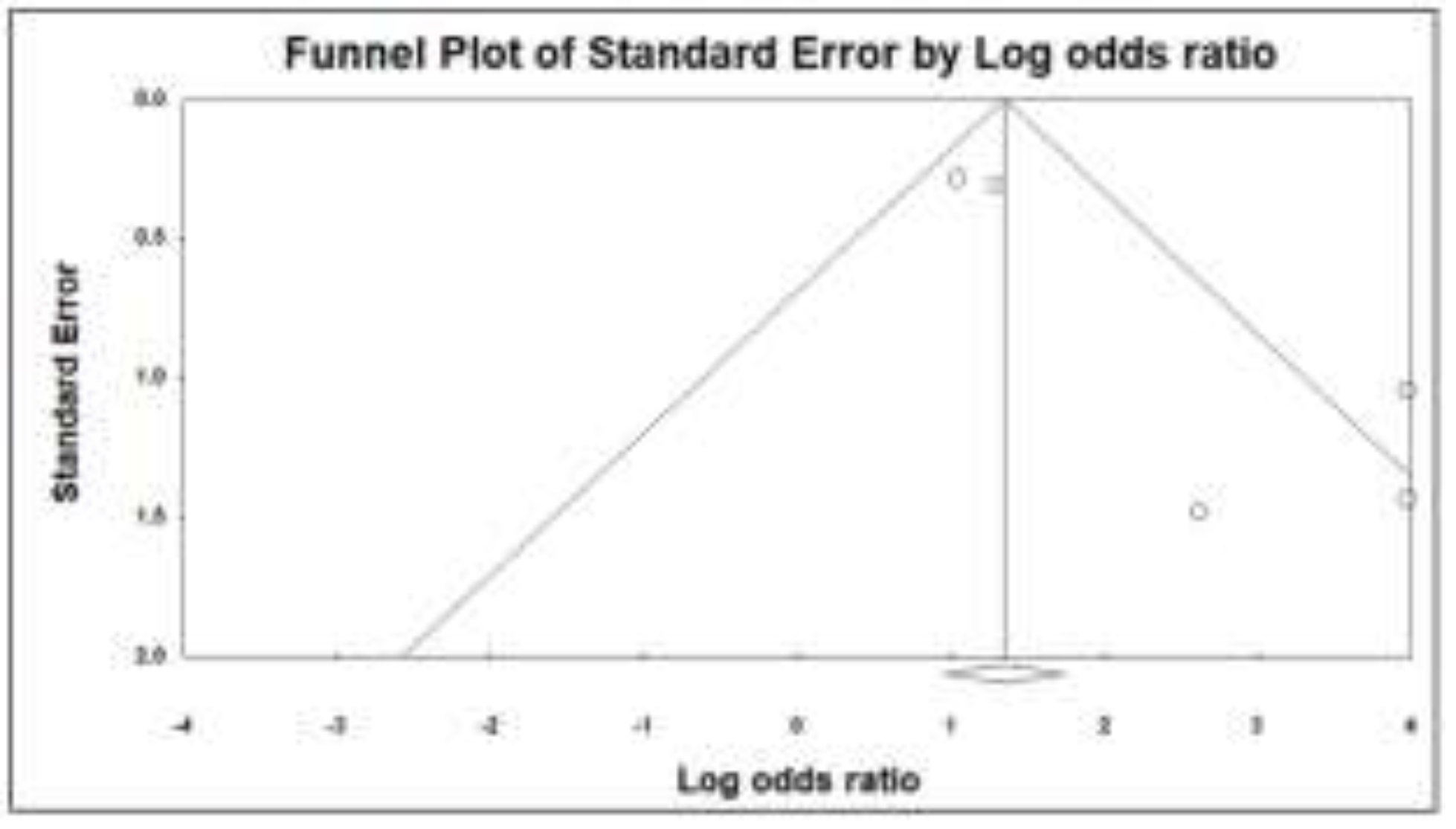
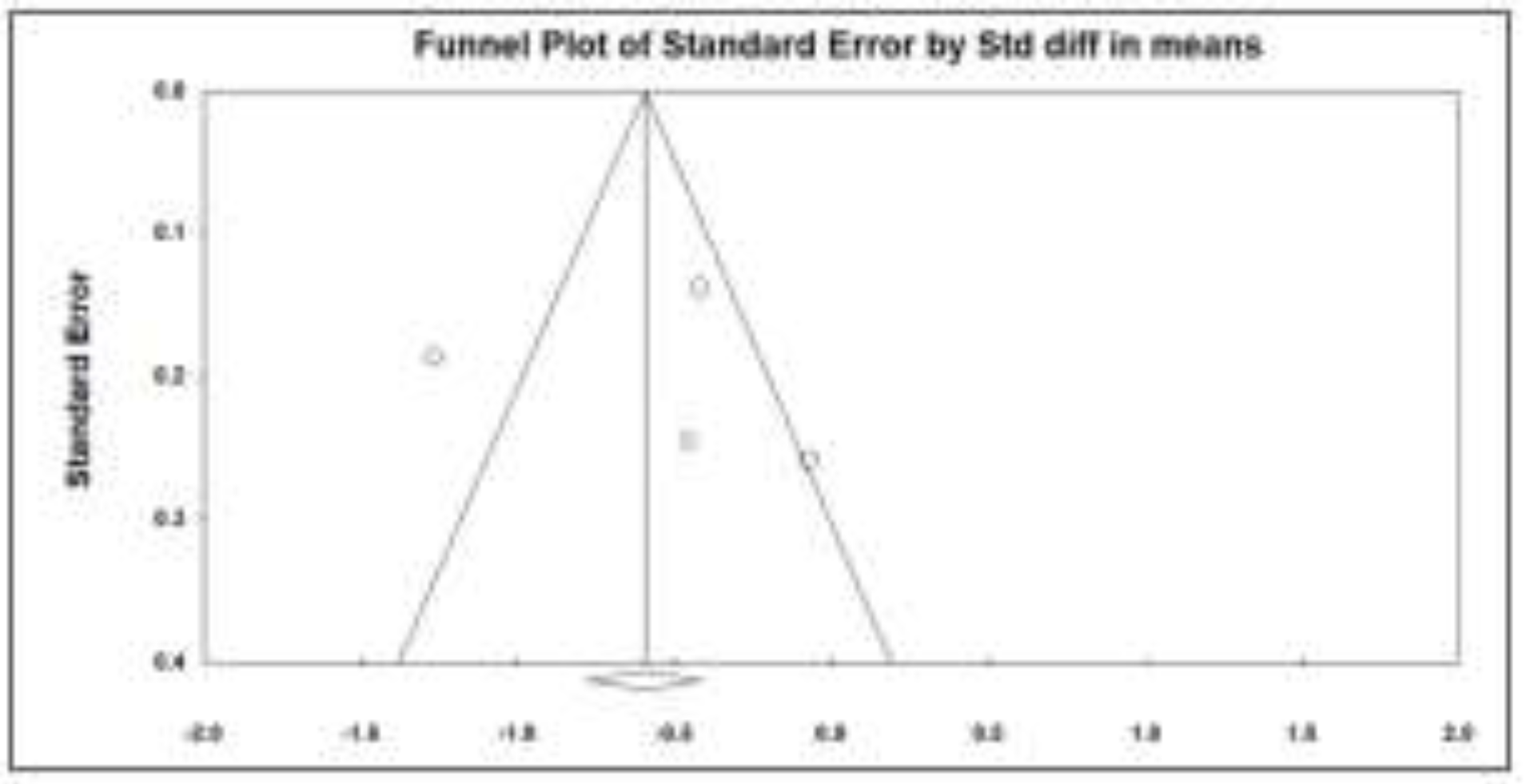
GERD- gastroesophageal reflux disease, CI- confidence interval
GERD- gastroesophageal reflux disease
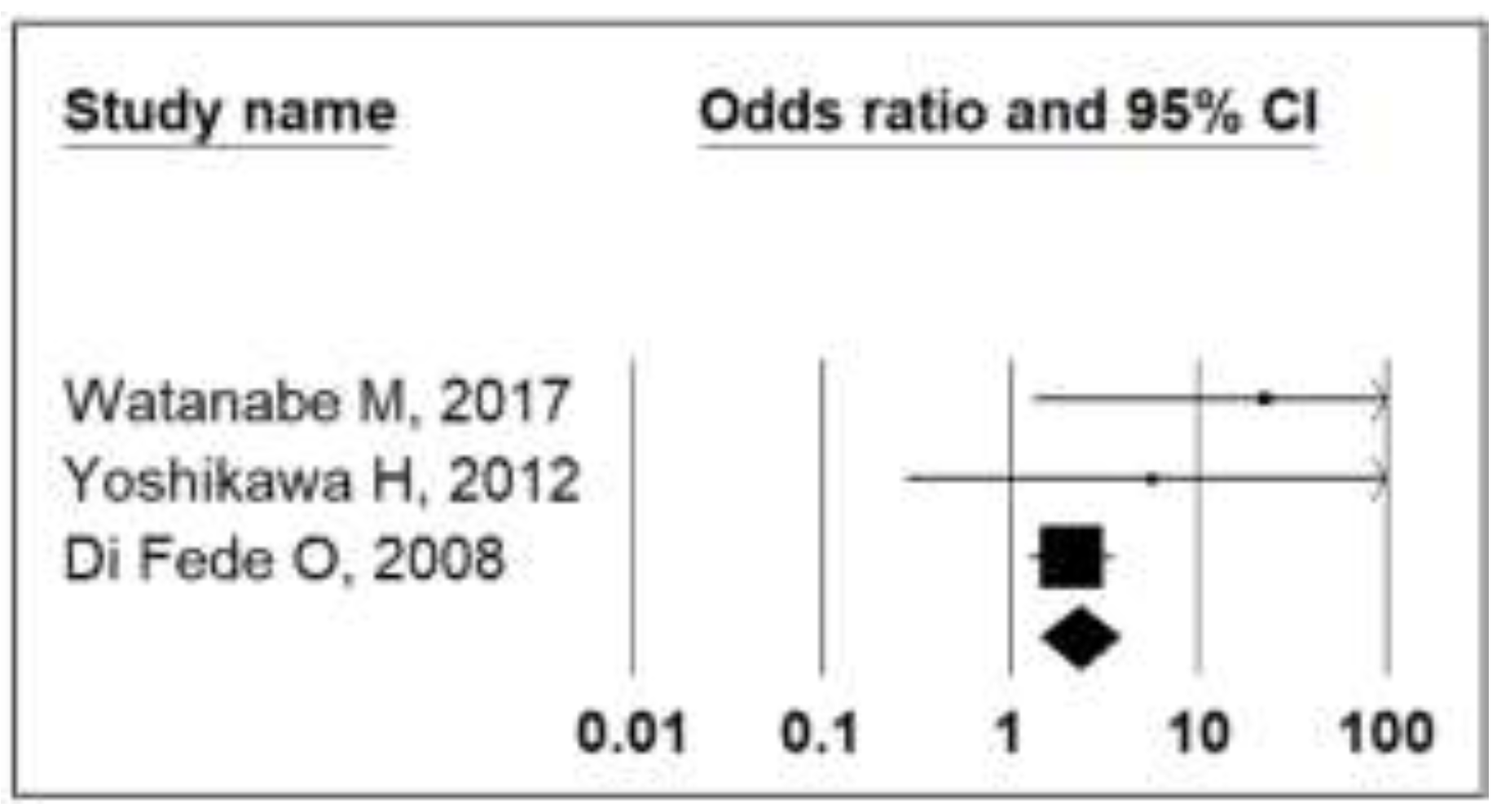
OABS- oral acid burning sensation, GERD- gastroesophageal reflux disease, CI- confidence interval
Highlights
- ✓
- Patients with GERD are at risk of developing oral acid burning sensation, subjective halitosis and xerostomia.
- ✓
- Non-dental oral cavity lesions such as angular cheilitis, candidiasis, gingivitis, glossitis, leucoplakia, palate erythema, periodontitis, oral submucous fibrosis and ulceration could represent extraesophageal manifestations of GERD.
Conclusions
Conflicts of Interest disclosure
Compliance with ethical standards
References
- Vakil, N.; van Zanten, S.V.; Kahrilas, P.; Dent, J.; Jones, R.; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: A global evidence-based consensus. Am J Gastroenterol. 2006, 101, 1900–1920. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.; Bolus, R.; Khanna, D.; Hays, R.D.; Chang, L.; Melmed, G.Y.; Khanna, P.; Spiegel, B. GERD symptoms in the general population: Prevalence and severity versus care-seeking patients. Dig Dis Sci. 2014, 59, 2488–2496. [Google Scholar] [CrossRef]
- Lundell, L.R.; Dent, J.; Bennett, J.R.; Blum, A.L.; Armstrong, D.; Galmiche, J.P.; Johnson, F.; Hongo, M.; Richter, J.E.; Spechler, S.J.; et al. Endoscopic assessment of oesophagitis: Clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999, 45, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Giannini, E.G.; Zentilin, P.; Dulbecco, P.; Vigneri, S.; Scarlata, P.; Savarino, V. Management strategy for patients with gastroesophageal reflux disease: A comparison between empirical treatment with esomeprazole and endoscopy-oriented treatment. Am J Gastroenterol. 2008, 103, 267–275. [Google Scholar] [CrossRef]
- Vinesh, E.; Masthan, K.; Kumar, M.S.; Jeyapriya, S.M.; Babu, A.; Thinakaran, M. A Clinicopathologic Study of Oral Changes in Gastroesophageal Reflux Disease, Gastritis, and Ulcerative Colitis. J Contemp Dent Pract. 2016, 17, 943–947. [Google Scholar] [CrossRef]
- Jajam, M.; Bozzolo, P.; Niklander, S. Oral manifestations of gastrointestinal disorders. J Clin Exp Dent. 2017, 9, e1242–e1248. [Google Scholar] [CrossRef] [PubMed]
- Haag, D.G.; Peres, K.G.; Balasubramanian, M.; Brennan, D.S. Oral Conditions and Health-Related Quality of Life: A Systematic Review. J Dent Res. 2017, 96, 864–874. [Google Scholar] [CrossRef]
- Ranjitkar, S.; Smales, R.J.; Kaidonis, J.A. Oral manifestations of gastroesophageal reflux disease. J Gastroenterol Hepatol. 2012, 27, 21–27. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009, 339, b2700. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ. 2015, 350, g7647. [Google Scholar] [CrossRef]
- Nakagawa, S.; Cuthill, I.C. Effect size, confidence interval and statistical significance: A practical guide for biologists. Biol Rev Camb Philos Soc. 2007, 82, 591–605. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, H.; Furuta, K.; Ueno, M.; Egawa, M.; Yoshino, A.; Kondo, S.; Nariai, Y.; Ishibashi, H.; Kinoshita, Y.; Sekine, J. Oral symptoms including dental erosion in gastroesophageal reflux disease are associated with decreased salivary flow volume and swallowing function. J Gastroenterol. 2012, 47, 412–420. [Google Scholar] [CrossRef]
- Watanabe, M.; Nakatani, E.; Yoshikawa, H.; Kanno, T.; Nariai, Y.; Yoshino, A.; Vieth, M.; Kinoshita, Y.; Sekine, J. Oral soft tissue disorders are associated with gastroesophageal reflux disease: Retrospective study. BMC Gastroenterol. 2017, 17, 92. [Google Scholar] [CrossRef] [PubMed]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [PubMed]
- Corrêa, M.C.; Lerco, M.M.; Cunha Mde, L.; Henry, M.A. Salivary parameters and teeth erosions in patients with gastroesophageal reflux disease. Arq Gastroenterol. 2012, 49, 214–218. [Google Scholar] [CrossRef]
- Campisi, G.; Lo Russo, L.; Di Liberto, C.; Di Nicola, F.; Butera, D.; Vigneri, S.; Compilato, D.; Lo Muzio, L.; Di Fede, O. Saliva variations in gastro-oesophageal reflux disease. J Dent. 2008, 36, 268–271. [Google Scholar] [CrossRef]
- Warsi, I.; Ahmed, J.; Younus, A.; Rasheed, A.; Akhtar, T.S.; Ain, Q.U.; Khurshid, Z. Risk factors associated with oral manifestations and oral health impact of gastro- oesophageal reflux disease: A multicentre, cross- sectional study in Pakistan. BMJ Open. 2019, 9, e021458. [Google Scholar] [CrossRef]
- Adachi, K.; Mishiro, T.; Tanaka, S.; Yoshikawa, H.; Kinoshita, Y. A Study on the Relationship between Reflux Esophagitis and Periodontitis. Intern Med. 2016, 55, 2523–2528. [Google Scholar] [CrossRef]
- Deppe, H.; Mücke, T.; Wagenpfeil, S.; Kesting, M.; Rozej, A.; Bajbouj, M.; Sculean, A. Erosive esophageal reflux vs. non erosive esophageal reflux: Oral findings in 71 patients. BMC Oral Health. 2015, 15, 84. [Google Scholar] [CrossRef]
- Orhan, U.; Aziz Serkan, S.; Selçuk, G.; Sinan, Ö.; Cem Batuhan, O.; Ayhan, Ö.; Erdal, P.; Mustafa, D. Evaluating the effect of tumor size on survival and its prognostic significance among gastric cancer patients. J Clin Invest Surg. 2020, 5, 76–82. [Google Scholar] [CrossRef]
- Corrêa, M.C.; Lerco, M.M.; Henry, M.A. Study in oral cavity alterations in patients with gastroesophageal reflux disease. Arq Gastroenterol. 2008, 45, 132–136. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Muñoz, J.V.; Herreros, B.; Sanchiz, V.; Amoros, C.; Hernandez, V.; Pascual, I.; Mora, F.; Minguez, M.; Bagan, J.V.; Benages, A. Dental and periodontal lesions in patients with gastro-oesophageal reflux disease. Dig Liver Dis. 2003, 35, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Liu, J.; Chen, S.; Wang, Y.; Zhang, Z. Prevalence of dental erosion among people with gastroesophageal reflux disease in China. J Prosthet Dent. 2017, 117, 48–54. [Google Scholar] [CrossRef]
- Pace, F.; Pallotta, S.; Tonini, M.; Vakil, N.; Bianchi Porro, G. Systematic review: Gastro-oesophageal reflux disease and dental lesions. Aliment Pharmacol Ther. 2008, 27, 1179–1186. [Google Scholar] [CrossRef] [PubMed]
- Jordão, H.W.T.; Coleman, H.G.; Kunzmann, A.T.; McKenna, G. The association between erosive toothwear and gastro-oesophageal reflux-related symptoms and disease: A systematic review and meta-analysis. J Dent. 2020, 95, 103284. [Google Scholar] [CrossRef]
- Picos, A.; Lasserre, J.F.; Chisnoiu, A.M.; Berar, A.M.; d’Incau, E.; Picos, A.M.; Chira, A.; des Varannes, S.B.; Dumitrascu, D.L. Factors associated with dental erosions in gastroesophageal reflux disease: A cross-sectional study in patients with heartburn. Med Pharm Rep. 2020, 93, 23–29. [Google Scholar] [CrossRef]
- Ganesh, M.; Hertzberg, A.; Nurko, S.; Needleman, H.; Rosen, R. Acid Rather Than Nonacid Reflux Burden Is a Predictor of Tooth Erosion. J Pediatr Gastroenterol Nutr. 2016, 62, 309–313. [Google Scholar] [CrossRef]
- Moazzez, R.; Anggiansah, A.; Bartlett, D.W. The association of acidic reflux above the upper oesophageal sphincter with palatal tooth wear. Caries Res. 2005, 39, 475–478. [Google Scholar] [CrossRef]
- Malfertheiner, P.; Hallerbäck, B. Clinical manifestations and complications of gastroesophageal reflux disease (GERD). Int J Clin Pract. 2005, 59, 346–355. [Google Scholar] [CrossRef]
- Smyth, E.C.; Lagergren, J.; Fitzgerald, R.C.; Lordick, F.; Shah, M.A.; Lagergren, P.; Cunningham, D. Oesophageal cancer. Nat Rev Dis Primers. 2017, 3, 17048. [Google Scholar] [CrossRef]
- Villanueva-Vilchis, M.D.; López-Ríos, P.; García, I.M.; Gaitán-Cepeda, L.A. Impact of oral mucosa lesions on the quality of life related to oral health. An etiopathogenic study. Med Oral Patol Oral Cir Bucal. 2016, 21, e178–e184. [Google Scholar] [CrossRef] [PubMed]
- DeVault, K.R.; Castell, D.O.; American College of Gastroenterology. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol. 2005, 100, 190–200. [Google Scholar] [CrossRef] [PubMed]

 |
  |
  |
 |
© 2021 by the author. 2021 Madalina-Gabriela Indre, Darius Sampelean, Vlad Taru, Angela Cozma, Dorel Sampelean, Mircea Vasile Milaciu, Olga Hilda Orasan
Share and Cite
Indre, M.-G.; Sampelean, D.; Taru, V.; Cozma, A.; Sampelean, D.; Milaciu, M.V.; Orasan, O.H. Non-Dental Oral Cavity Findings in Gastroesophageal Reflux Disease: A Systematic Review and Meta-Analysis. J. Mind Med. Sci. 2021, 8, 60-70. https://doi.org/10.22543/7674.81.P6070
Indre M-G, Sampelean D, Taru V, Cozma A, Sampelean D, Milaciu MV, Orasan OH. Non-Dental Oral Cavity Findings in Gastroesophageal Reflux Disease: A Systematic Review and Meta-Analysis. Journal of Mind and Medical Sciences. 2021; 8(1):60-70. https://doi.org/10.22543/7674.81.P6070
Chicago/Turabian StyleIndre, Madalina-Gabriela, Darius Sampelean, Vlad Taru, Angela Cozma, Dorel Sampelean, Mircea Vasile Milaciu, and Olga Hilda Orasan. 2021. "Non-Dental Oral Cavity Findings in Gastroesophageal Reflux Disease: A Systematic Review and Meta-Analysis" Journal of Mind and Medical Sciences 8, no. 1: 60-70. https://doi.org/10.22543/7674.81.P6070
APA StyleIndre, M.-G., Sampelean, D., Taru, V., Cozma, A., Sampelean, D., Milaciu, M. V., & Orasan, O. H. (2021). Non-Dental Oral Cavity Findings in Gastroesophageal Reflux Disease: A Systematic Review and Meta-Analysis. Journal of Mind and Medical Sciences, 8(1), 60-70. https://doi.org/10.22543/7674.81.P6070



