A Comprehensive Analysis of Postpartum Depression and Delivery Characteristics: A Cross-Sectional Study
Abstract
:Introduction
Materials and Methods
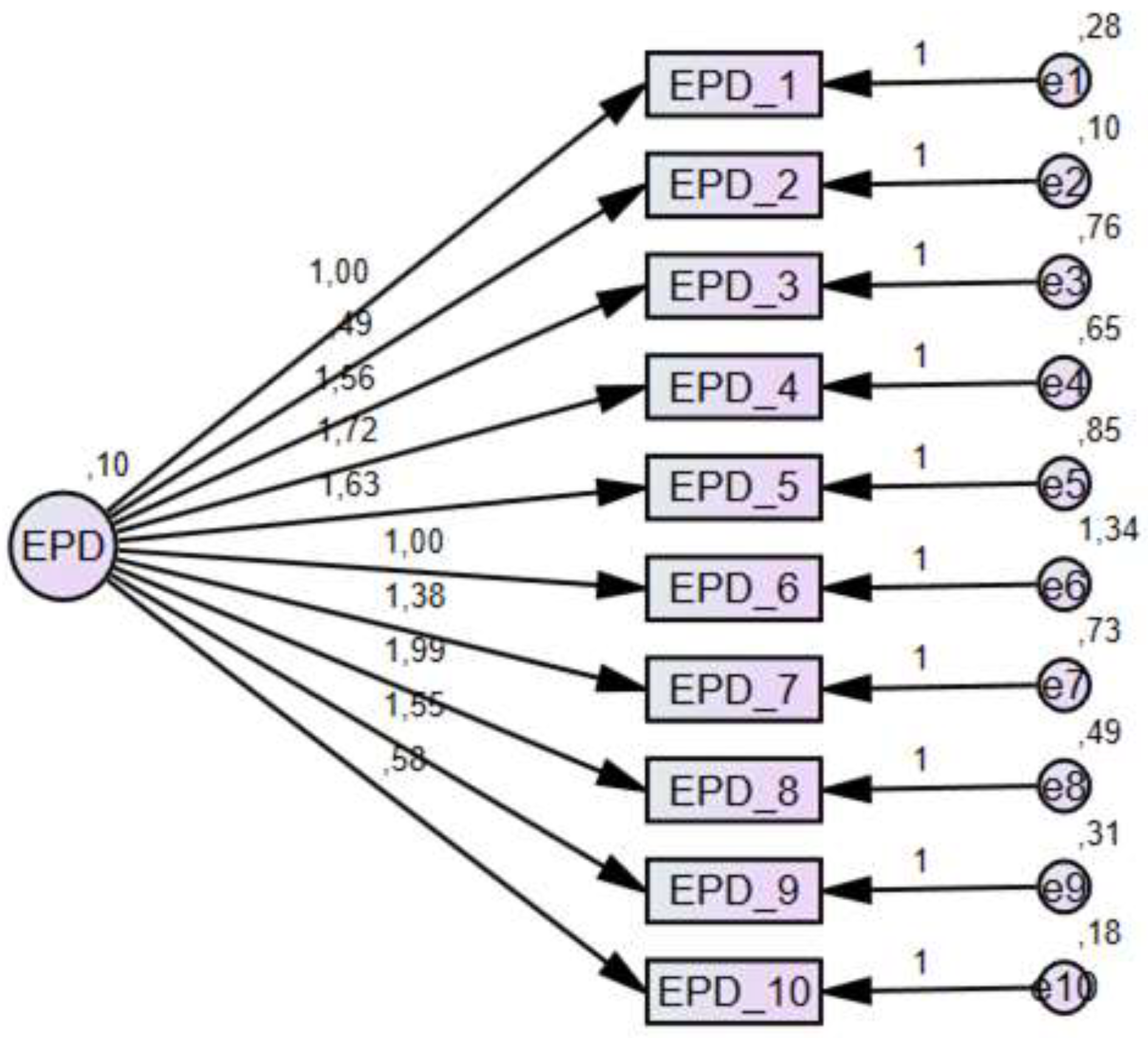
Data Collection Tools
Statistical Methods
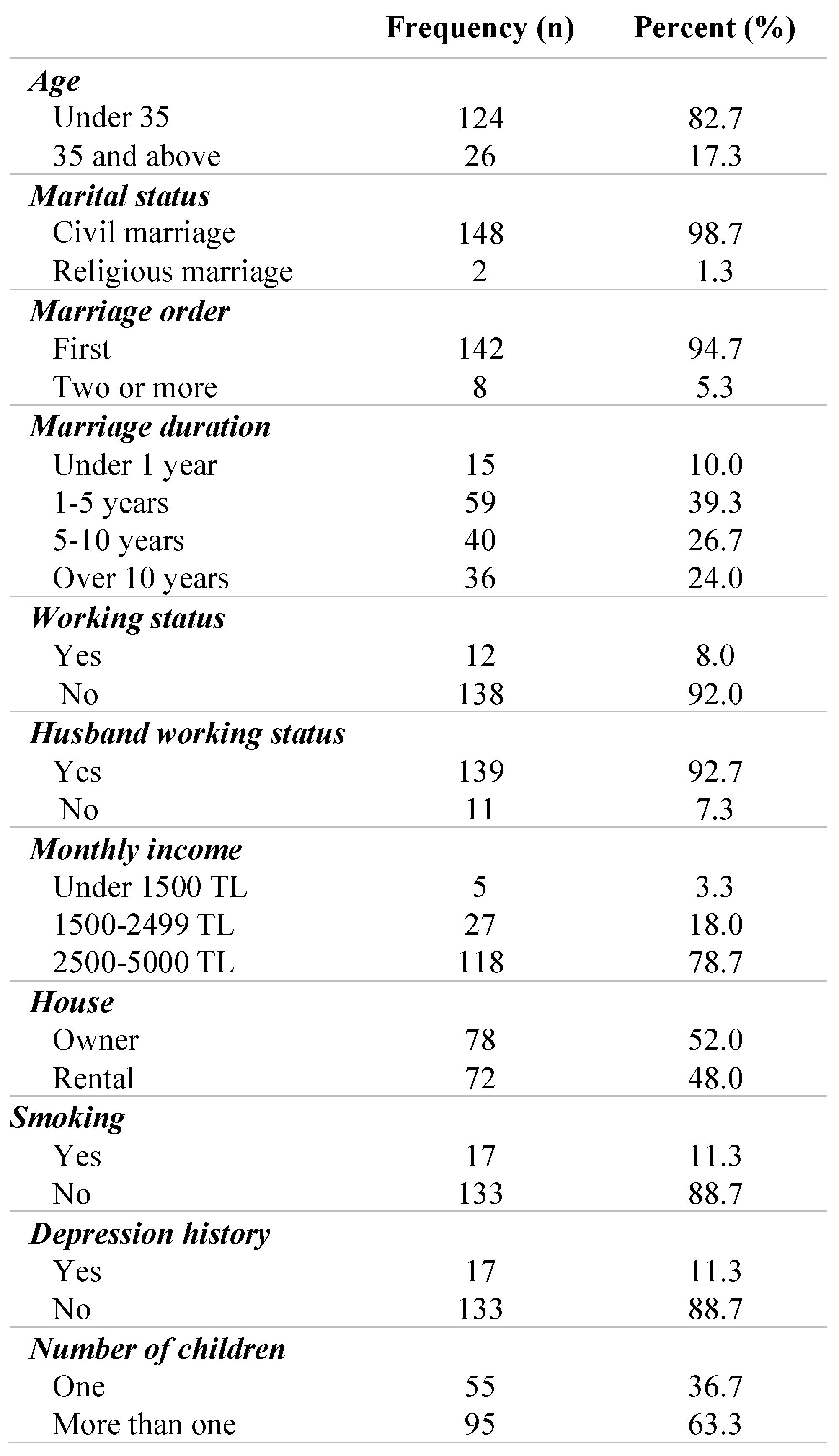
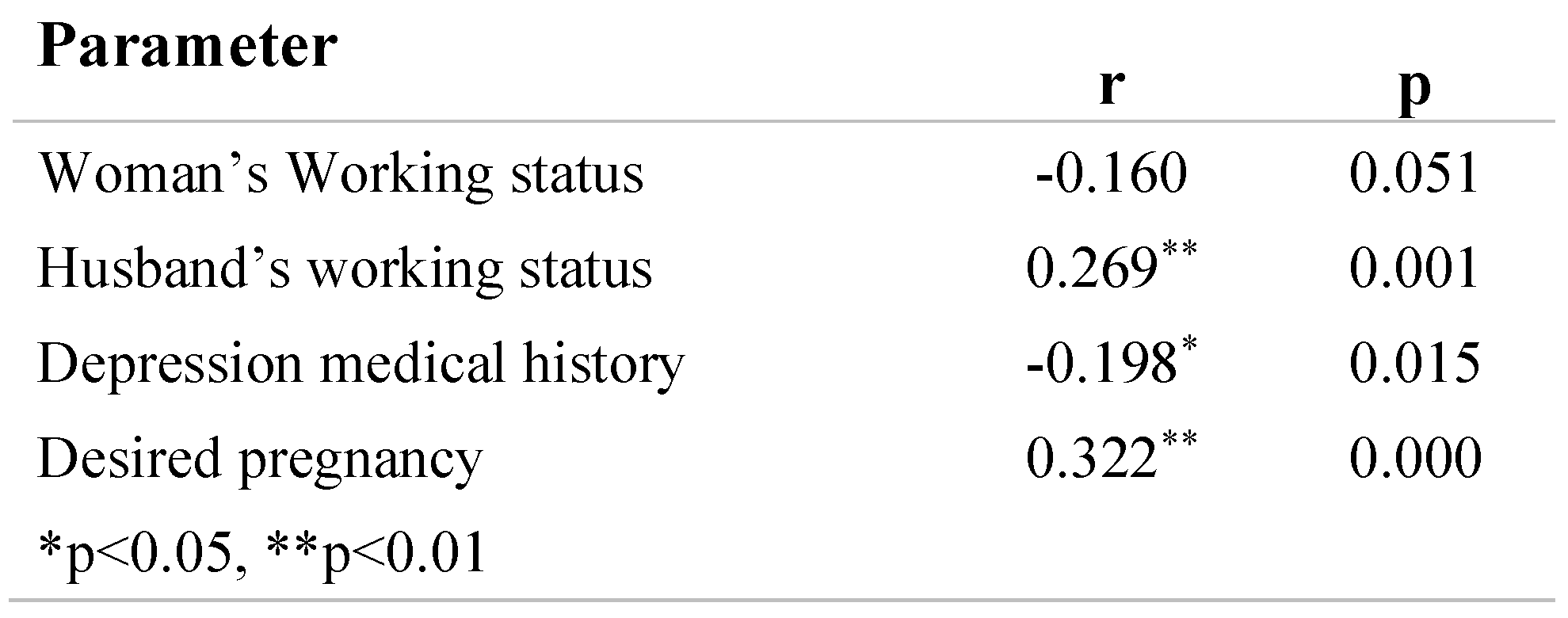
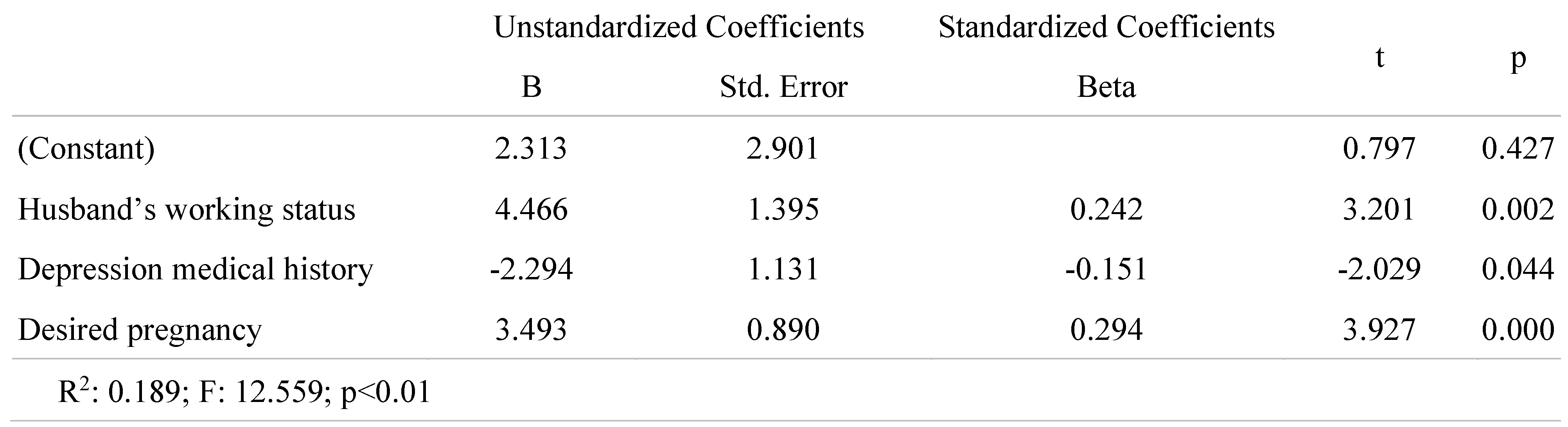
Results
Discussions
Conclusions
Conflict of interest disclosure
Compliance with ethical standards
References
- Wszołek, K.; Żurawska, J.; Łuczak-Wawrzyniak, J.; Kopaszewska-Bachorz, B.; Głowińska, A.; Pięta, B. Postpartum depression—A medical or a social problem? J Matern Fetal Neonatal Med. 2020, 33, 2556–2560. [Google Scholar] [CrossRef]
- Pluym, I.D.; Holliman, K.; Afshar, Y.; Lee, C.C.; Richards, M.C.; Han, C.S.; Krakow, D.; Rao, R. Emergency department use among postpartum women with mental health disorders. Am J Obstet Gynecol MFM. 2021, 3, 100269. [Google Scholar] [CrossRef] [PubMed]
- van der Zee-van den Berg, A.I.; Boere-Boonekamp, M.M.; Groothuis-Oudshoorn, C.G.M.; Reijneveld, S.A. Postpartum depression and anxiety: A community- based study on risk factors before, during and after pregnancy. J Affect Disord. 2021, 286, 158–165. [Google Scholar] [CrossRef]
- O’hara, M.W.; Swain, A.M. Rates and risk of postpartum depression—A meta-analysis. Int Rev Psychiatry. 1996, 8, 37–54. [Google Scholar] [CrossRef]
- Stewart, D.E.; Vigod, S. Postpartum Depression. N Engl J Med. 2016, 375, 2177–2186. [Google Scholar] [CrossRef]
- Xiao, M.; Zhang, J. Research progress in prediction of postpartum depression. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2020, 45, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Perry, A.; Gordon-Smith, K.; Jones, L.; Jones, I. Phenomenology, Epidemiology and Aetiology of Postpartum Psychosis: A Review. Brain Sci. 2021, 11, 47. [Google Scholar] [CrossRef]
- Lebel, C.; MacKinnon, A.; Bagshawe, M.; Tomfohr- Madsen, L.; Giesbrecht, G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020, 277, 5–13. [Google Scholar] [CrossRef]
- Karaçam, Z.; Kitiş, Y. The Postpartum Depression Screening Scale: Its reliability and validity for the Turkish population. Turk Psikiyatri Derg. 2008, 19, 187–196. [Google Scholar]
- Alp Yilmaz, F.; Avci, D.; Arzu Aba, Y.; Ozdilek, R.; Dutucu, N. Sexual Dysfunction in Postpartum Turkish Women: It’s Relationship with Depression and Some Risk Factors. Afr J Reprod Health. 2018, 22, 54–63. [Google Scholar] [CrossRef]
- Cadorin, L.; Grassetti, L.; Paoletti, E.; Cara, A.; Truccolo, I.; Palese, A. Evaluating self-directed learning abilities as a prerequisite of health literacy among older people: Findings from a validation and a cross-sectional study. Int J Older People Nurs. 2020, 15, e12282. [Google Scholar] [CrossRef]
- Cangur, S.; Ercan, I. Comparison of model fit indices used in structural equation modeling under multivariate normality. Journal of Modern Applied Statistical Methods. 2015, 14, 152–167. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M. Structural Equation Modelling: Guidelines for Determining Model Fit. Electronic Journal of Business Research Methods. 2008, 6, 53–60. [Google Scholar]
- Beck Aaron, T.; Steer Robert, A.; Carbin Margery, G. Psychometric properties of the Beck depression inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Bekmezci, H.; Hamlacı, Y.; Ozerdogan, N. Postpartum specific assessment scales in Turkey. HEAD 2016, 13, 122–128. [Google Scholar] [CrossRef]
- Silva, R.S.; Junior, R.A.; Sampaio, V.S.; Rodrigues, K.O.; Fronza, M. Postpartum depression: A case-control study. J Matern Fetal Neonatal Med. 2019, 3, 1–6. [Google Scholar] [CrossRef]
- Durukan, E.; İlhan, N.M.; Bumin, A.M.; Aycan, S. Postpartum Depression Frequency and Quality of Life Among a Group of Mothers Having a Child Aged 2 Weeks-18 Months. Balkan Med J. 2011, 28, 385–393. [Google Scholar] [CrossRef]
- Chalise, A.; Bhandari, T.R. Postpartum Depression and its Associated Factors: A Community-based Study in Nepal. J Nepal Health Res Counc. 2019, 17, 200–205. [Google Scholar] [CrossRef]
- Haque, S.; Malebranche, M. Impact of culture on refugee women’s conceptualization and experience of postpartum depression in high-income countries of resettlement: A scoping review. PLoS ONE. 2020, 15, e0238109. [Google Scholar] [CrossRef]
- Opie, R.S.; Uldrich, A.C.; Ball, K. Maternal Postpartum Diet and Postpartum Depression: A Systematic Review. Matern Child Health J. 2020, 24, 966–978. [Google Scholar] [CrossRef]
- Mischoulon, D.; Freeman, M.P. Omega-3 fatty acids in psychiatry. Psychiatr Clin North Am. 2013, 36, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.; Skouteris, H.; Wertheim, E.H.; Paxton, S.J.; Milgrom, J. The relationship between depression and body dissatisfaction across pregnancy and the postpartum: A prospective study. J Health Psychol. 2009, 14, 27–35. [Google Scholar] [CrossRef]
- Frokjaer, V.G.; Pinborg, A.; Holst, K.K.; Overgaard, A.; Henningsson, S.; Heede, M.; Larsen, E.C.; Jensen, P.S.; Agn, M.; Nielsen, A.P.; Stenbæk, D.S.; da Cunha-Bang, S.; Lehel, S.; Siebner, H.R.; Mikkelsen, J.D.; Svarer, C.; Knudsen, G.M. Role of Serotonin Transporter Changes in Depressive Responses to Sex-Steroid Hormone Manipulation: A Positron Emission Tomography Study. Biol Psychiatry. 2015, 78, 534–543. [Google Scholar] [CrossRef] [PubMed]
- Ghaedrahmati, M.; Kazemi, A.; Kheirabadi, G.; Ebrahimi, A.; Bahrami, M. Postpartum depression risk factors: A narrative review. J Educ Health Promot. 2017, 6, 60. [Google Scholar] [CrossRef]
- Kheirabadi, G.R.; Maracy, M.R.; Barekatain, M.; Salehi, M.; Sadri, G.H.; Kelishadi, M.; Cassy, P. Risk factors of postpartum depression in rural areas of Isfahan Province, Iran. Arch Iran Med. 2009, 12, 461–467. [Google Scholar] [PubMed]
- Mayberry, L.J.; Horowitz, J.A.; Declercq, E. Depression symptom prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. J Obstet Gynecol Neonatal Nurs. 2007, 36, 542–549. [Google Scholar] [CrossRef]
- Horibe, M.; Hane, Y.; Abe, J.; Matsui, T.; Kato, Y.; Ueda, N.; Sasaoka, S.; Motooka, Y.; Hatahira, H.; Hasegawa, S.; Kinosada, Y.; Hara, H.; Nakamura, M. Contraceptives as possible risk factors for postpartum depression: A retrospective study of the food and drug administration adverse event reporting system, 2004-2015. Nurs Open. 2018, 5, 131–138. [Google Scholar] [CrossRef]
- Dias, C.C.; Figueiredo, B. Breastfeeding and depression: A systematic review of the literature. J Affect Disord. 2015, 171, 142–154. [Google Scholar] [CrossRef]
- Leung, B.M.; Kaplan, B.J. Perinatal depression: Prevalence, risks, and the nutrition link--a review of the literature. J Am Diet Assoc. 2009, 109, 1566–1575. [Google Scholar] [CrossRef]
- Forty, L.; Jones, L.; Macgregor, S.; Caesar, S.; Cooper, C.; Hough, A.; Dean, L.; Dave, S.; Farmer, A.; McGuffin, P.; Brewster, S.; Craddock, N.; Jones, I. Familiality of postpartum depression in unipolar disorder: Results of a family study. Am J Psychiatry. 2006, 163, 1549–1553. [Google Scholar] [CrossRef]
- Murphy-Eberenz, K.; Zandi, P.P.; March, D.; Crowe, R.R.; Scheftner, W.A.; Alexander, M.; McInnis, M.G.; Coryell, W.; Adams, P.; DePaulo JRJr Miller, E.B.; Marta, D.H.; Potash, J.B.; Payne, J.; Levinson, D.F. Is perinatal depression familial? J Affect Disord. 2006, 90, 49–55. [Google Scholar] [CrossRef]
- Wisner, K.L.; Sit, D.K.; McShea, M.C.; Rizzo, D.M.; Zoretich, R.A.; Hughes, C.L.; Eng, H.F.; Luther, J.F.; Wisniewski, S.R.; Costantino, M.L.; Confer, A.L.; Moses-Kolko, E.L.; Famy, C.S.; Hanusa, B.H. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen- positive depression findings. JAMA Psychiatry. 2013, 70, 490–498. [Google Scholar] [CrossRef]
- Guo, Y.J.; Shan, Y.M.; Wang, Z.J.; Shen, Z.F. Efficacy of transcranial magnetic stimulation and fluoxetine in the treatment of postpartum depression: A protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020, 99, e20170. [Google Scholar] [CrossRef]
- Powell, J.G.; Garland, S.; Preston, K.; Piszczatoski, C. Brexanolone (Zulresso): Finally, an FDA-Approved Treatment for Postpartum Depression. Ann Pharmacother. 2020, 54, 157–163. [Google Scholar] [CrossRef]
- Shabbir, O.; Khan, K.S.; Jawaid, H. Brexanolone Therapy for Postpartum Depression. J Pak Med Assoc. 2020, 70, 565–566. [Google Scholar] [CrossRef]
 |
 |
 |
 |
© 2008 by the author. 2008 Navdar Dogus Uzun, Mustafa Tekin, Fulya Uzun
Share and Cite
Uzun, N.D.; Tekin, M.; Uzun, F. A Comprehensive Analysis of Postpartum Depression and Delivery Characteristics: A Cross-Sectional Study. J. Mind Med. Sci. 2021, 8, 94-99. https://doi.org/10.22543/7674.81.P9499
Uzun ND, Tekin M, Uzun F. A Comprehensive Analysis of Postpartum Depression and Delivery Characteristics: A Cross-Sectional Study. Journal of Mind and Medical Sciences. 2021; 8(1):94-99. https://doi.org/10.22543/7674.81.P9499
Chicago/Turabian StyleUzun, Navdar Dogus, Mustafa Tekin, and Fulya Uzun. 2021. "A Comprehensive Analysis of Postpartum Depression and Delivery Characteristics: A Cross-Sectional Study" Journal of Mind and Medical Sciences 8, no. 1: 94-99. https://doi.org/10.22543/7674.81.P9499
APA StyleUzun, N. D., Tekin, M., & Uzun, F. (2021). A Comprehensive Analysis of Postpartum Depression and Delivery Characteristics: A Cross-Sectional Study. Journal of Mind and Medical Sciences, 8(1), 94-99. https://doi.org/10.22543/7674.81.P9499



