Alexithymia and Physical Outcomes in Psychosomatic Subjects: A Cross-Sectional Study
Abstract
Introduction
Study hypotheses
Materials and Methods
Participants
Instruments and procedure
Statistical analysis
Results
Hypothesis 1
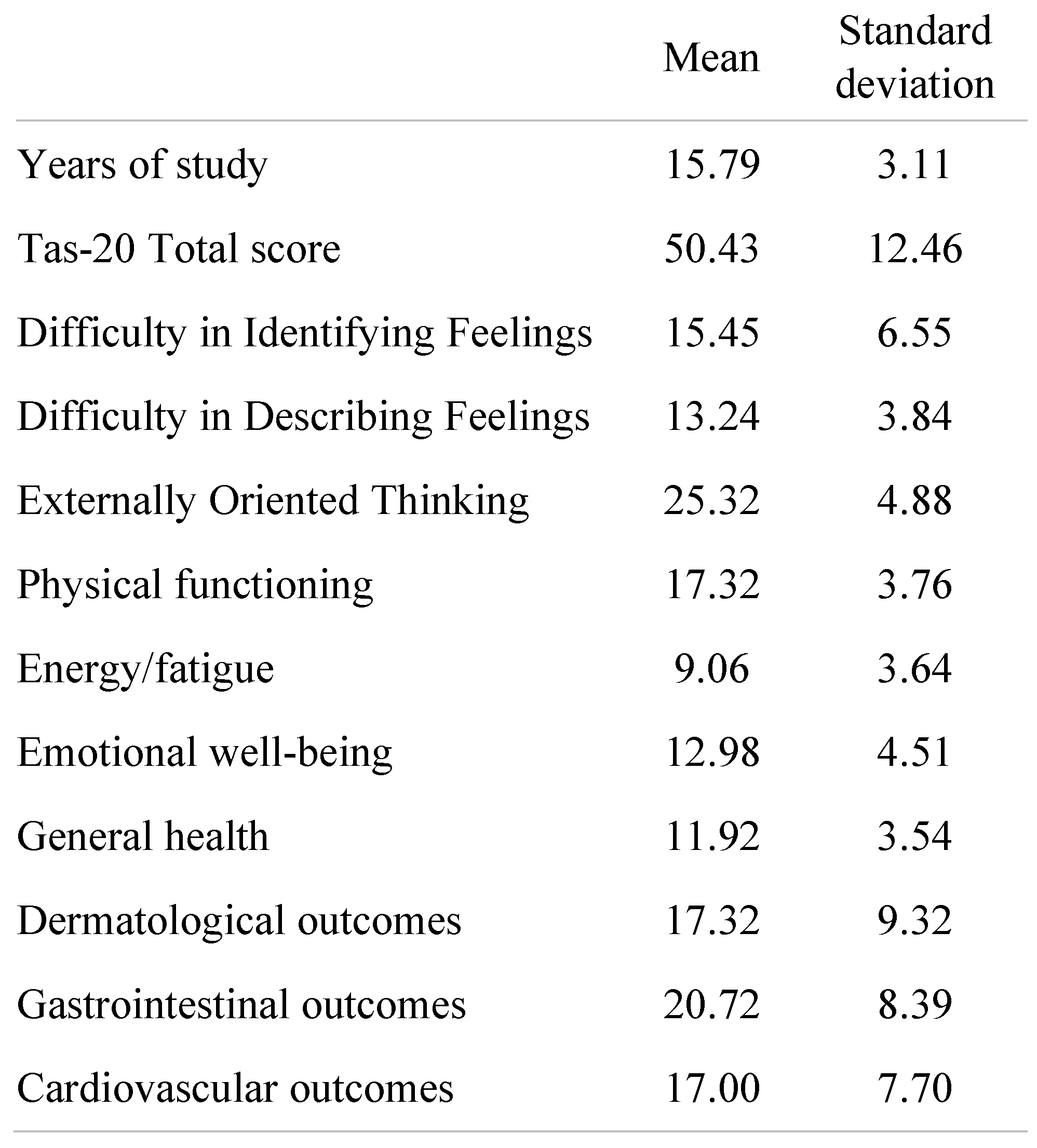 |
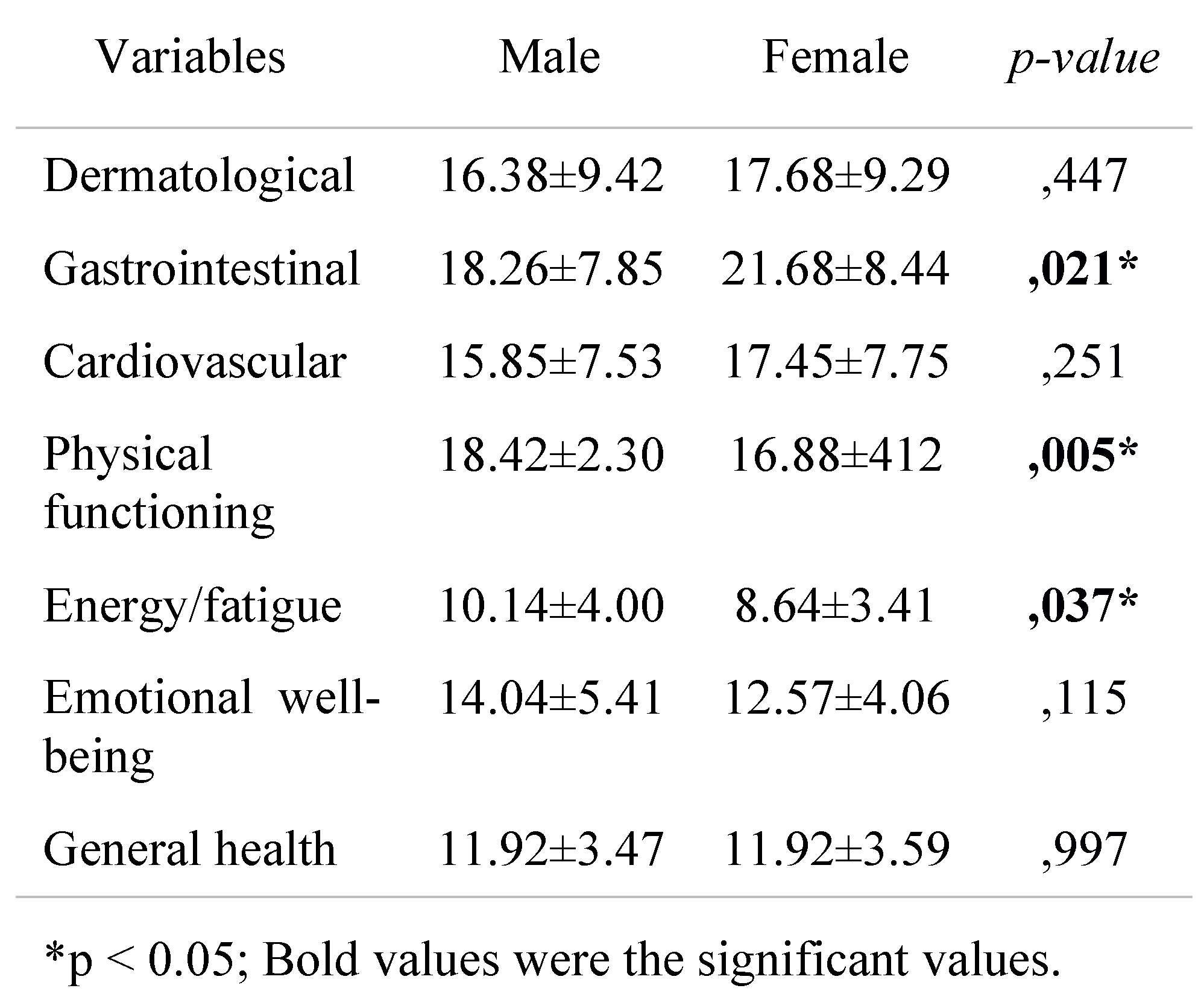
Hypothesis 2
Hypothesis 3
Discussions
Conclusions
Conflicts of Interest disclosure
Compliance with ethical standards
References
- Gregory, R.J.; Berry, S.L. Measuring counterdependency in patients with chronic pain. Psychosom Med. 1999, 61, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Sifneos, P.E. The prevalence of ‘alexithymic’ characteristics in psychosomatic patients. Psychother Psychosom. 1973, 22, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Šago, D.; Babić, G. Roots of Alexithymia. Arch. Psychiatry Res. Int. J. Psychiatry Relat. Sci. 2019, 55, 71–84. [Google Scholar] [CrossRef]
- Taylor, G.J. Recent developments in alexithymia theory and research. Can J Psychiatry. 2000, 45, 134–142. [Google Scholar] [CrossRef]
- Widge, A.S.; Dougherty, D.D.; Moritz, C.T. Affective Brain-Computer Interfaces As Enabling Technology for Responsive Psychiatric Stimulation. Brain Comput Interfaces (Abingdon). 2014, 1, 126–136. [Google Scholar] [CrossRef]
- Porcelli, P.; Taylor, G. Alexithymia and Physical Illness: A Psychosomatic Approach. In Alexithymia: Advances in Research, Theory, and Clinical Practice; Luminet, O., Bagby, R., Taylor, G., Eds.; Cambridge University Press: Cambridge, UK, 2018; pp. 105–126. [Google Scholar] [CrossRef]
- Terock, J.; Klinger-König, J.; Janowitz, D.; Nauck, M.; Völzke, H.; Grabe, H.J. Alexithymia is associated with increased all-cause mortality risk in men, but not in women: A 10-year follow-up study. J Psychosom Res. 2021, 143, 110372. [Google Scholar] [CrossRef]
- Torrado, M.; Eusébio, S.; Ouakinin, S. Alexithymia and illness: Towards a psychosomatic perspective of emotion regulation deficits. In Perspectives on Cognitive Psychology. Current developments in alexithymia: A cognitive and affective deficit; Teixeira, R.J., Bermond, B., Moormann, P.P., Eds.; Nova Science Publishers: Hauppauge, NY, USA, 2018; pp. 173–194. [Google Scholar]
- Conversano, C. Common Psychological Factors in Chronic Diseases. Front Psychol. 2019, 10, 2727. [Google Scholar] [CrossRef]
- Conversano, C.; Di Giuseppe, M. Psychological Factors as Determinants of Chronic Conditions: Clinical and Psychodynamic Advances. Front Psychol. 2021, 12, 635708. [Google Scholar] [CrossRef]
- Hyphantis, T.; Goulia, P.; Carvalho, A.F. Personality traits, defense mechanisms and hostility features associated with somatic symptom severity in both health and disease. J Psychosom Res. 2013, 75, 362–369. [Google Scholar] [CrossRef]
- Di Giuseppe, M.; Ciacchini, R.; Micheloni, T.; Bertolucci, I.; Marchi, L.; Conversano, C. Defense mechanisms in cancer patients: A systematic review. J Psychosom Res. 2018, 115, 76–86. [Google Scholar] [CrossRef]
- Martino, G.; Langher, V.; Cazzato, V.; Vicario, C.M. Editorial: Psychological Factors as Determinants of Medical Conditions. Front Psychol. 2019, 10, 2502. [Google Scholar] [CrossRef] [PubMed]
- Kramer, G.P.; Bernstein, D.A.; Phares, V. Introduction to clinical psychology; Cambridge University Press: Cambridge, UK, 2019; ISBN-10: 1108705146. [Google Scholar]
- Hunsley, J.; Lee, C.M. Introduction to clinical psychology; John Wiley & Sons: Hoboken, NJ, USA, 2017; ISBN 978-1-119-30151-6. [Google Scholar]
- Merlo, E.M. Opinion Article: The role of psychological features in chronic diseases, advancements and perspectives. Mediterr. J. Clin. Psychol. 2019, 7. [Google Scholar] [CrossRef]
- Settineri, S.; Frisone, F.; Alibrandi, A.; Merlo, E.M. Emotional Suppression and Oneiric Expression in Psychosomatic Disorders: Early Manifestations in Emerging Adulthood and Young Patients. Front Psychol. 2019, 10, 1897. [Google Scholar] [CrossRef]
- Picardi, A.; Abeni, D.; Melchi, C.F.; Puddu, P.; Pasquini, P. Psychiatric morbidity in dermatological outpatients: An issue to be recognized. Br J Dermatol. 2000, 143, 983–991. [Google Scholar] [CrossRef] [PubMed]
- Grandi, S.; Fabbri, S.; Tossani, E.; Mangelli, L.; Branzi, A.; Magelli, C. Psychological Evaluation after Cardiac Transplantation: The Integration of Different Criteria. Psychother Psychosom. 2001, 70, 176–183. [Google Scholar] [CrossRef]
- Vadini, F.; Sozio, F.; Madeddu, G.; De Socio, G.; Maggi, P.; Nunnari, G.; Vichi, F.; Di Stefano, P.; Tracanna, E.; Polilli, E.; Sciacca, A.; Zizi, B.; Lai, V.; Bartolozzi, C.; Flacco, M.E.; Bonfanti, P.; Santilli, F.; Manzoli, L.; Parruti, G. Alexithymia Predicts Carotid Atherosclerosis, Vascular Events, and All-Cause Mortality in Human Immunodeficiency Virus-Infected Patients: An Italian Multisite Prospective Cohort Study. Open Forum Infect Dis. 2019, 6, ofz331. [Google Scholar] [CrossRef] [PubMed]
- Porcelli, P.; Taylor, G.J.; Bagby, R.M.; De Carne, M. Alexithymia and functional gastrointestinal disorders. A comparison with inflammatory bowel disease. Psychother Psychosom. 1999, 68, 263–269. [Google Scholar] [CrossRef]
- Kano, M.; Muratsubaki, T.; Yagihashi, M.; Morishita, J.; Mugikura, S.; Dupont, P.; Takase, K.; Kanazawa, M.; Van Oudenhove, L.; Fukudo, S. Insula Activity to Visceral Stimulation and Endocrine Stress Responses as Associated With Alexithymia in Patients With Irritable Bowel Syndrome. Psychosom Med. 2020, 82, 29–38. [Google Scholar] [CrossRef]
- Kano, M.; Endo, Y.; Fukudo, S. Association Between Alexithymia and Functional Gastrointestinal Disorders. Front Psychol. 2018, 9, 599. [Google Scholar] [CrossRef]
- Baysak, S.; Kılıç, F.A.; Karagün, E.; Baysak, E. Relationship of Alexithymia, Rumination and Coping Style with Psoriasis and Their Effects on The Clinical Features. Turk Psikiyatri Derg. 2020, 31, 252–258. [Google Scholar]
- Craparo, G.; Magnano, P.; Zapparrata, M.V.; Gori, A.; Costanzo, G.; Pace, U.; Pellerone, M. Coping, attachment style and resilience: The mediating role of alexithymia. Mediterr. J. Clin. Psychol. 2018, 6. [Google Scholar] [CrossRef]
- Hemming, L.; Haddock, G.; Shaw, J.; Pratt, D. Alexithymia and Its Associations With Depression, Suicidality, and Aggression: An Overview of the Literature. Front Psychiatry 2019, 10, 203. [Google Scholar] [CrossRef] [PubMed]
- Talamonti, M.; Galluzzo, M.; Servoli, S.; D’Adamio, S.; Bianchi, L. Alexithymia and Plaque Psoriasis: Preliminary Investigation in a Clinical Sample of 250 Patients. Dermatology 2016, 232, 648–654. [Google Scholar] [CrossRef]
- Willemsen, R.; Roseeuw, D.; Vanderlinden, J. Alexithymia and dermatology: The state of the art. Int J Dermatol. 2008, 47, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Carney, R.M.; Rich, M.W.; Freedland, K.E.; Saini, J.; teVelde, A.; Simeone, C.; Clark, K. Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med. 1988, 50, 627–633. [Google Scholar] [CrossRef]
- Craparo, G.; Gagliano, O.; Costanzo, G.; La Rosa, V.L.; Gori, A.; Mendolicchio, L. Boredom, alexithymia, and desire thinking in eating disorders: A cross-sectional study. Mediterr. J. Clin. Psychol. 2020, 8. [Google Scholar] [CrossRef]
- Frasure-Smith, N.; Lespérance, F.; Talajic, M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993, 270, 1819–1825. [Google Scholar] [CrossRef]
- Kojima, M.; Frasure-Smith, N.; Lespérance, F. Alexithymia following myocardial infarction: Psychometric properties and correlates of the Toronto Alexithymia Scale. J Psychosom Res. 2001, 51, 487–495. [Google Scholar] [CrossRef]
- Martino, G.; Caputo, A.; Schwarz, P.; Bellone, F.; Fries, W.; Quattropani, M.C.; Vicario, C.M. Alexithymia and Inflammatory Bowel Disease: A Systematic Review. Front Psychol. 2020, 11, 1763. [Google Scholar] [CrossRef]
- Mazaheri, M.; Afshar, H.; Weinland, S.; Mohammadi, N.; Adibi, P. Alexithymia and functional gastrointestinal disorders (FGID). Med Arh. 2012, 66, 28–32. [Google Scholar] [CrossRef]
- Porcelli, P.; Leoci, C.; Guerra, V.; Taylor, G.J.; Bagby, R.M. A longitudinal study of alexithymia and psychological distress in inflammatory bowel disease. J Psychosom Res. 1996, 41, 569–573. [Google Scholar] [CrossRef]
- Martino, G.; Caputo, A.; Vicario, C.M.; Catalano, A.; Schwarz, P.; Quattropani, M.C. The Relationship Between Alexithymia and Type 2 Diabetes: A Systematic Review. Front Psychol. 2020, 11, 2026. [Google Scholar] [CrossRef]
- Özsoy, F.; Taşcı, İ. Defense mechanisms, dissociation, alexithymia and childhood traumas in chronic migraine patients. Journal of Rational-Emotive & Cognitive- Behavior Therapy 2021, 39, 1–13. [Google Scholar] [CrossRef]
- Pappalardo, S.M. Vlad-Virtual Reality Application for Treatment of Psychosomatic Conditions: A report at final stage of software validation process. Mediterr. J. Clin. Psychol. 2020, 8. [Google Scholar] [CrossRef]
- De Vries, A.M.M.; Gholamrezaee, M.M.; Verdonck-de Leeuw, I.M.; de Roten, Y.; Despland, J.N.; Stiefel, F.; Passchier, J. Physicians’ emotion regulation during communication with advanced cancer patients. Psychooncology 2018, 27, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Merlo, E.M.; McNabney, S.M.; Frisone, F.; Sicari, F.; Paunica, M.; Motofei, C.; Settineri, S. Compassion and suppression in caregivers: Twin masks of tragedy and joy of caring. J Mind Med Sci. 2020, 7, 61–68. [Google Scholar] [CrossRef]
- Merlo, E.M.; Stoian, A.P.; Motofei, I.G.; Settineri, S. Clinical Psychological Figures in Healthcare Professionals: Resilience and Maladjustment as the "Cost of Care". Front Psychol. 2020, 11, 607783. [Google Scholar] [CrossRef]
- Fava, G.A.; Freyberger, H.J.; Bech, P.; Christodoulou, G.; Sensky, T.; Theorell, T.; Wise, T.N. Diagnostic criteria for use in psychosomatic research. Psychother Psychosom. 1995, 63, 1–8. [Google Scholar] [CrossRef]
- Porcelli, P.; Sonino, N. Psychological Factors Affecting Medical Conditions: A New Classification for DSM-V; Karger Medical and Scientific Publishers: Basel, Switzerland, 2007; Volume 28. [Google Scholar] [CrossRef]
- Galeazzi, G.M.; Ferrari, S.; Mackinnon, A.; Rigatelli, M. Interrater reliability, prevalence, and relation to ICD-10 diagnoses of the Diagnostic Criteria for Psychosomatic Research in consultation-liaison psychiatry patients. Psychosomatics 2004, 45, 386–393. [Google Scholar] [CrossRef]
- Ware, J.E.; Snow, K.K.; Kosinski, M.; Gandek, B. SF-36 health survey. Manual and interpretation guide; The Health Institute, New England Medical Center: Boston, MA, USA, 1997; p. 10-6. [Google Scholar]
- Apolone, G.; Mosconi, P. The Italian SF-36 Health Survey: Translation, validation and norming. J Clin Epidemiol. 1998, 51, 1025–1036. [Google Scholar] [CrossRef]
- Hays, R.D.; Sherbourne, C.D.; Mazel, R.M. The RAND 36-Item Health Survey 1.0. Health Econ. 1993, 2, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Bagby, R.M.; Parker, J.D.; Taylor, G.J. The twenty-item Toronto Alexithymia Scale--I. Item selection and cross-validation of the factor structure. J Psychosom Res. 1994, 38, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Gritti, P.; Lombardi, S.; Nobile, B.; Trappoliere, P.; Gambardella, A.; Di Caprio, E.L.; Resicato, G. Alexithymia and cancer-related fatigue: A controlled cross-sectional study. Tumori. 2010, 96, 131–137. [Google Scholar]
- Theisen, M.E.; MacNeill, S.E.; Lumley, M.A.; Ketterer, M.W.; Goldberg, A.D.; Borzak, S. Psychosocial factors related to unrecognized acute myocardial infarction. Am J Cardiol. 1995, 75, 1211–1213. [Google Scholar] [CrossRef]
- Craparo, G.; Faraci, P.; Gori, A. Psychometric Properties of the 20-Item Toronto Alexithymia Scale in a Group of Italian Younger Adolescents. Psychiatry Investig. 2015, 12, 500–507. [Google Scholar] [CrossRef]
- Kauhanen, J.; Kaplan, G.A.; Julkunen, J.; Wilson, T.W.; Salonen, J.T. Social factors in alexithymia. Compr Psychiatry. 1993, 34, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Kirmayer, L.J.; Robbins, J.M. Cognitive and social correlates of the Toronto Alexithymia Scale. Psychosomatics. 1993, 34, 41–52. [Google Scholar] [CrossRef]
- Marty, P. L’ordre psychosomatique (PAYOT) (French) Paperback–September 17 1998; ISBN-10: 2228891819.
- Motofei, I.G. The etiology of premature ejaculation starting from a bihormonal model of normal sexual stimulation. Int J Impot Res. 2001, 13, 49–50. [Google Scholar] [CrossRef]
- Taylor, G.J.; Bagby, R.M. Examining Proposed Changes to the Conceptualization of the Alexithymia Construct: The Way Forward Tilts to the Past. Psychother Psychosom. 2020, 7, 1–11. [Google Scholar] [CrossRef]
- Goerlich, K.S. The Multifaceted Nature of Alexithymia- A Neuroscientific Perspective. Front Psychol. 2018, 9, 1614. [Google Scholar] [CrossRef]
- Cupertino, F.; Niemeyer-Corbellini, J.P.; Ramos-E-Silva, M. Psychosomatic aspects of vitiligo. Clin Dermatol. 2017, 35, 292–297. [Google Scholar] [CrossRef]
- Gieler, U.; Gieler, T.; Peters, E.M.J.; Linder, D. Skin and Psychosomatics—Psychodermatology today. J Dtsch Dermatol Ges. 2020, 18, 1280–1298. [Google Scholar] [CrossRef] [PubMed]
- Mulinari-Brenner, F. Psychosomatic aspects of alopecia areata. Clin Dermatol. 2018, 36, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Zięciak, T.; Rzepa, T.; Król, J.; Żaba, R. Stigmatization feelings and depression symptoms in psoriasis patients. Psychiatr Pol. 2017, 51, 1153–1163. [Google Scholar] [CrossRef] [PubMed]
- Aluja, A.; Malas, O.; Urieta, P.; Worner, F.; Balada, F. Biological correlates of the Toronto Alexithymia Scale (TAS-20) in cardiovascular disease and healthy community subjects. Physiol Behav. 2020, 227, 113151. [Google Scholar] [CrossRef]
- Karukivi, M.; Jula, A.; Pulkki-Råback, L.; Hutri-Kähönen, N.; Laitinen, T.T.; Viikari, J.; Juonala, M.; Raitakari, O. Ideal cardiovascular health in adolescents and young adults is associated with alexithymia over two decades later: Findings from the cardiovascular risk in Young Finns Study: Department: Research Centre of Applied and Preventive Cardiovascular Medicine, University of Turku, Turku, Finland. Psychiatry Res. 2020, 289, 112976. [Google Scholar] [CrossRef]
- Motofei, I.G. A dual physiological character for cerebral mechanisms of sexuality and cognition: Common somatic peripheral afferents. BJU Int. 2011, 108, 1634–1639. [Google Scholar] [CrossRef]
- Xiong, N.N.; Wei, J.; Ke, M.Y.; Hong, X.; Li, T.; Zhu, L.M.; Sha, Y.; Jiang, J.; Fischer, F. Illness Perception of Patients with Functional Gastrointestinal Disorders. Front Psychiatry. 2018, 9, 122. [Google Scholar] [CrossRef]
- Wiernik, E.; Lemogne, C.; Fezeu, L.; Arnault, N.; Hercberg, S.; Kesse-Guyot, E.; Galan, P. Association Between Alexithymia and Risk of Incident Cardiovascular Diseases in the SUpplémentation en VItamines et Minéraux AntioXydants (SU.VI.MAX) Cohort. Psychosom Med. 2018, 80, 460–467. [Google Scholar] [CrossRef]
- Adeyemo, M.A.; Spiegel, B.M.; Chang, L. Meta-analysis: Do irritable bowel syndrome symptoms vary between men and women? Aliment Pharmacol Ther. 2010, 32, 738–755. [Google Scholar] [CrossRef]
- Kanazawa, M.; Endo, Y.; Whitehead, W.E.; Kano, M.; Hongo, M.; Fukudo, S. Patients and nonconsulters with irritable bowel syndrome reporting a parental history of bowel problems have more impaired psychological distress. Dig Dis Sci. 2004, 49, 1046–1053. [Google Scholar] [CrossRef]
- Kosako, M.; Akiho, H.; Miwa, H.; Kanazawa, M.; Fukudo, S. Impact of symptoms by gender and age in Japanese subjects with irritable bowel syndrome with constipation (IBS-C): A large population-based internet survey. Biopsychosoc Med. 2018, 12, 12. [Google Scholar] [CrossRef]
- Löwe, B.; Lohse, A.; Andresen, V.; Vettorazzi, E.; Rose, M.; Broicher, W. The Development of Irritable Bowel Syndrome: A Prospective Community-Based Cohort Study. Am J Gastroenterol. 2016, 111, 1320–1329. [Google Scholar] [CrossRef]
- Demers, L.A.; Schreiner, M.W.; Hunt, R.H.; Mueller, B.A.; Klimes-Dougan, B.; Thomas, K.M.; Cullen, K.R. Alexithymia is associated with neural reactivity to masked emotional faces in adolescents who self-harm. J Affect Disord. 2019, 249, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Donges, U.S.; Suslow, T. Alexithymia and automatic processing of emotional stimuli: A systematic review. Rev Neurosci. 2017, 28, 247–264. [Google Scholar] [CrossRef] [PubMed]
- Lane, R.D. Is it possible to bridge the Biopsychosocial and Biomedical models? Biopsychosoc Med. 2014, 8, 3. [Google Scholar] [CrossRef][Green Version]
- Meza-Concha, N.; Arancibia, M.; Salas, F.; Behar, R.; Salas, G.; Silva, H.; Escobar, R. Towards a neurobiological understanding of alexithymia. Medwave. 20 1729, 17, e6960. [Google Scholar] [CrossRef]
- Patrikelis, P.; Lucci, G.; Alexoudi, A.; Korfias, S.; Messinis, L.; Nasios, G.; Papasilekas, T.; Sakas, D.; Gatzonis, S. Addressing Evidence Linking Secondary Alexithymia to Aberrant Humor Processing. Behav Neurol. 2019, 2019, 1803624. [Google Scholar] [CrossRef]
- Damasio, A.R. Descartes’ error and the future of human life. Sci Am. 1994, 271, 144. [Google Scholar] [CrossRef]
- Damasio, A.R. Descartes’ error revisited. J Hist Neurosci. 2001, 10, 192–194. [Google Scholar] [CrossRef]
- Kastrup, B. An ontological solution to the mind-body problem. Philosophies. 2017, 2, 10. [Google Scholar] [CrossRef]
- Motofei, I.G.; Rowland, D.L. Solving the mind-body problem through two distinct concepts: Internal-mental existence and internal mental reality. J Mind Med Sci. 2015, 2, 128–141. [Google Scholar]
- Motofei, I.G.; Rowland, D.L. The mind-body problem; three equations and one solution represented by immaterial-material data. J Mind Med Sci. 2018, 5, 59–69. [Google Scholar] [CrossRef]
 |
 |
 |
© 2008 by the author. 2008 Liam Alexander MacKenzie Myles, Emanuele Maria Merlo
Share and Cite
Myles, L.A.M.; Merlo, E.M. Alexithymia and Physical Outcomes in Psychosomatic Subjects: A Cross-Sectional Study. J. Mind Med. Sci. 2021, 8, 86-93. https://doi.org/10.22543/7674.81.P8693
Myles LAM, Merlo EM. Alexithymia and Physical Outcomes in Psychosomatic Subjects: A Cross-Sectional Study. Journal of Mind and Medical Sciences. 2021; 8(1):86-93. https://doi.org/10.22543/7674.81.P8693
Chicago/Turabian StyleMyles, Liam Alexander MacKenzie, and Emanuele Maria Merlo. 2021. "Alexithymia and Physical Outcomes in Psychosomatic Subjects: A Cross-Sectional Study" Journal of Mind and Medical Sciences 8, no. 1: 86-93. https://doi.org/10.22543/7674.81.P8693
APA StyleMyles, L. A. M., & Merlo, E. M. (2021). Alexithymia and Physical Outcomes in Psychosomatic Subjects: A Cross-Sectional Study. Journal of Mind and Medical Sciences, 8(1), 86-93. https://doi.org/10.22543/7674.81.P8693



