Support for Family Members Who Are Caregivers to Relatives with Acquired Brain Injury
Abstract
:Introduction
Materials and Methods
Study design
Ethical considerations
Data analyses
Results
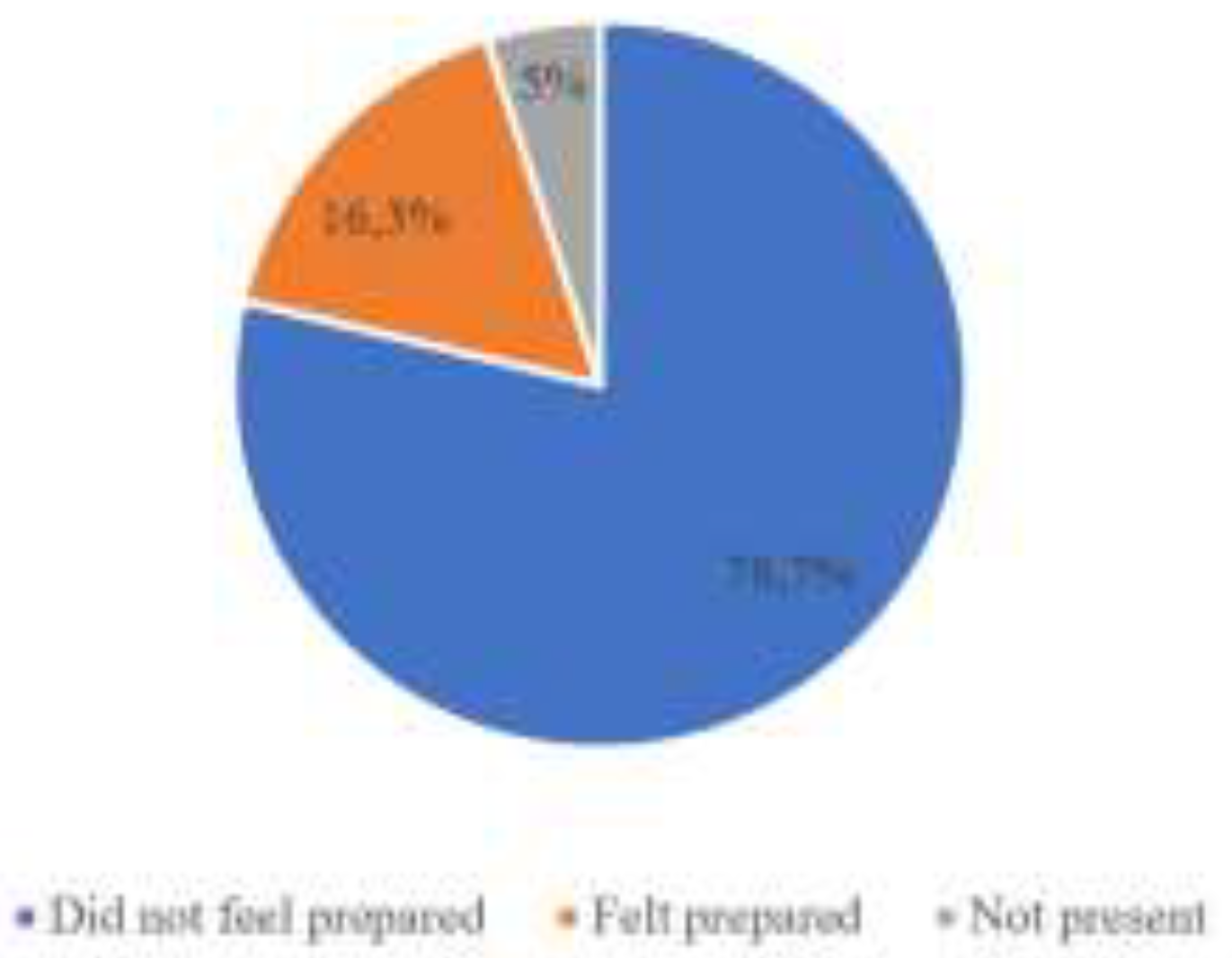
During your family member’s treatment in the hospital, did you feel adequately prepared by the healthcare professionals for the changes in your family member’s psychological status, behavior, cognition, and personality? Circle Yes or No: Please elaborate.
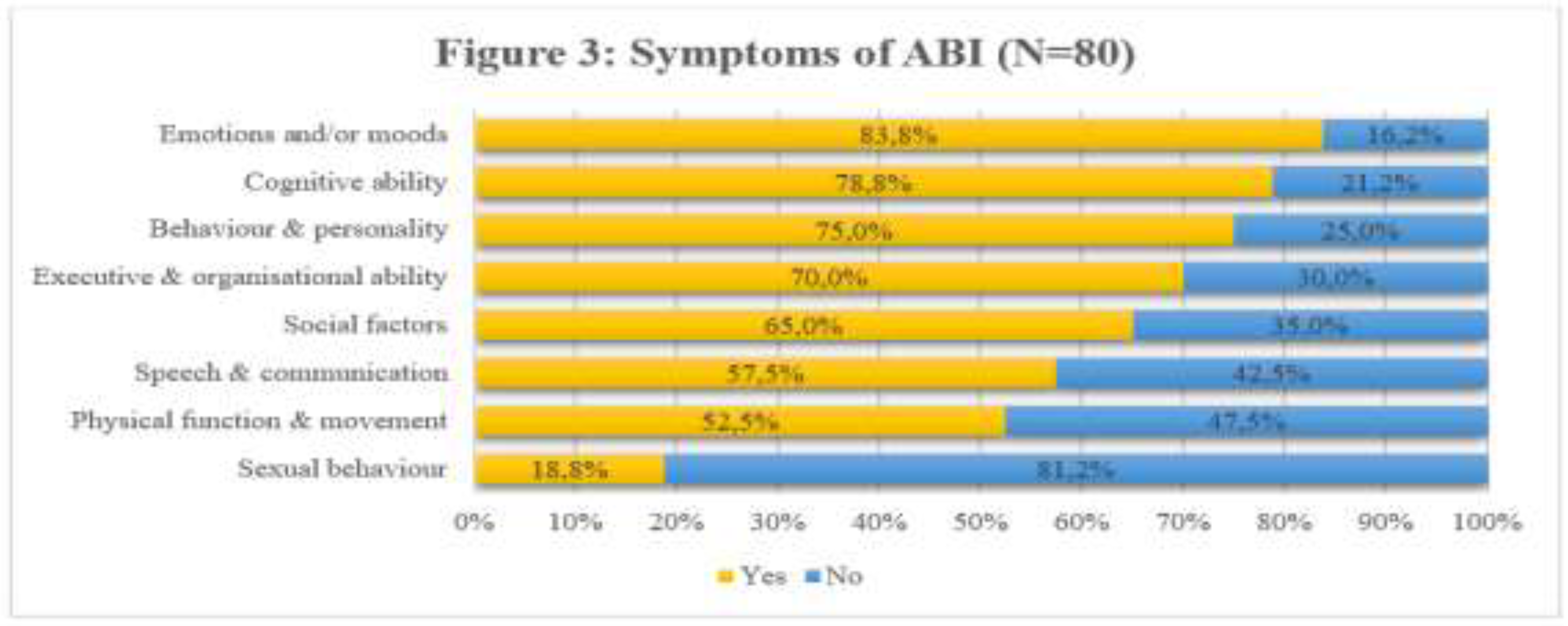
Which changes in your family member with ABI cause you most stress? Using the rating scale provided, please rate the categories listed in the box below according to the level of stress each one causes.
- Theme 1: Lack of availability of the healthcare professionals during the acute phase of the hospital treatment.
Feedback 1: The doctors were generally unavailable. When we did get to see them, there was a lack of clear communication. Little information was available, and the doctors seemed to make sure their rounds took place when you were not there. The nurses also avoided providing any explanation. We felt isolated and incredibly stressed all the time.
Feedback 2: There was no information about the severity of our daughter’s ABI, there was limited assistance and feedback on the long-term treatment and prognosis. We were told to expect some changes, but we never thought that she would be so aggressive with extreme moods. We were never told what to expect, except that shewould be physically disabled. Everything I know about brain injury I got from the internet, Headway Gauteng and reading books as the medical staff treats you as if you were standing in their way.
- Theme 2: Lack of psychological referral, support and follow-up.
Feedback 1: It took 36 months to find out that my husband has a traumatic brain injury and what this means. Headway Gauteng is where I am getting counselling and understanding. We feel let down by the doctors and the hospital. Why did no one explain the potential difficulties caused by ABI?
Feedback 2: We as a family had no idea how to cope with the problem and we did not know that an organization such as Headway Gauteng even existed. Follow-up from the hospital was non-existent. We are all traumatized because we feel that we have made so many mistakes in terms of our relative’s health and care. We feel that we have failed him. We were not given any real support. When we did end up in a sub-acute rehabilitation facility, they helped a lot with information and advice. It made all the difference.
- Theme 3: Lack of education and preparation for home-based care.
Feedback 1: We were not informed of the extent of the injury and how severely it would impact our lives once he was back home. We were given some information about his physical disability. We were only told that he would not function normally, and any improvement would only occur in the first 2 years. I feel that we should have been informed or educated about the severe impact of ABI on his personality and how to handle this. They have never contacted me to provide the family with trauma support. No one told me what to expect. The main problem was that he was sent home extremely aggressive and he physically abused both myself and my daughters. It was extremely traumatic as he had not been an aggressive person before the brain injury.
Feedback 2: When my wife was discharged from the hospital, we were told that she was stable and ready to go home. We thought everything would be fine and that she would go back to work and live a normal life. We discovered that she had lost her memory and she would never be able to work again. The whole family wishes that we had been warned. We all went through a lot of pain and difficulty before figuring out what was going on with her. The children were confused by her erratic behavior. For a long time, they were angry with her and they did not want to have anything to do with their mother. I feel that this could have been avoided if we had had a better understanding of the brain injury.
- Theme 4: Lack of education and information regarding ABI and its varied effects in the patient, such as extreme moods and aggression.
Feedback 1: There was no indication that my husband might be different. He has lost his fantastic sense of humor, lost his sharp intellect, lost his good sense of direction. I feel as if I were married to someone else, who is now in my husband’s body.
Feedback 2: We were never informed about his injury and as a result, a lot of time was wasted. He had lived with the injury for a couple of years before he could be treated. A lot of healthcare professionals do not know about brain injury. Advocacy is needed around brain injury from healthcare professionals. Also, counselling family is essential. My husband can run and move around just as easily as he used to, but he has a lack of emotions, such as love and kindness. He is impatient, needs instant gratification and is excessively selfish and sometimes very aggressive. At the Headway Friendship Circle, I have met other wives with similar experiences, which has helped me a lot. I feel less alone.
- Theme 5: Lack of treatment and education regarding the effects of stress on the psychological and physiological health in the family caregivers.
Feedback 1: Caring for my wife since she had a brain injury has been my priority. It is a lonely job, but I do it willingly. Before her injury, she had cared for me for many years. Unfortunately, I smoke and drink more than I ever have before. It is hard not to be able to have a proper conversation with my wife. Lately, I have been feeling low. I have also had a mini-stroke (trans ischemic attack) and I have been told that my heart is not as good as it should be. I have been neglecting my health and I am now suffering the consequences. I can see that the stress of being my wife’s primary carer has gotten on top of me. At Headway Gauteng, they have explained that I need to start taking care of myself too and I am going to start doing that. I do not want my wife to end up alone. My wife will be attending the group support programme two days per week. I am looking forward to the time out.
Discussion
Study limitations
Conclusions
Conflicts of Interest disclosure
Compliance with ethical standards
Acknowledgments
References
- Lezak, M.D.; Howieson, D.B.; Bigler, E.D.; Tranel, D. Neuropsychological Assessment, 5th ed.; Oxford University Press: New York, NY, USA, 2012; ISBN 9780195395525. [Google Scholar]
- Camplair, P.S.; Butler, R.W.; Lezak, M.D. Prigatano, G.P., Pliskin, N.H., Eds.; Providing psychological services to families of brain injured adults and children in the present health-care environment. In Clinical neuropsychology and cost outcome research: A beginning; Psychology Press: New York, NY, USA, 2003; pp. 83–107. [Google Scholar]
- Schlebusch, L.; Walker, J. The relationship between stress and suicidal ideation in family members caring for a patient with acquired brain injury. World Sci. News 2020, 140, 156–171. [Google Scholar]
- Walker, J.; Schlebusch, L.; Gaede, B. The impact of stress on depression, ill health and coping in family members caring for patients with acquired brain injury. S Afr Fam Pract (2004). 2020, 62, e1–e6. [Google Scholar] [CrossRef]
- Vitaliano, P.P.; Young, H.M.; Zhang, J. Is caregiving a risk factor for illness? Curr. Dir. Psychol. Sci. 2004, 13, 13–16. [Google Scholar] [CrossRef]
- Vitaliano, P.P.; Scanlan, J.M.; Zhang, J.; Savage, M.V.; Hirsch, I.B.; Siegler, I.C. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom Med. 2002, 64, 418–435. [Google Scholar] [CrossRef] [PubMed]
- Formica, C.; La Face, A.; Lo Buono, V.; Di Cara, M.; Micchìa, K.; Bonanno, L.; Logiudice, A.L.; Todaro, A.; Palmeri, R.; Bramanti, P.; Marino, S.; Corallo, F. Factors related to cognitive reserve among caregivers of severe acquired brain injury. J Clin Neurosci. 2020, 77, 94–97. [Google Scholar] [CrossRef]
- Zachariae, R. Psychoneuroimmunology: A bio-psycho-social approach to health and disease. Scand J Psychol. 2009, 50, 645–651. [Google Scholar] [CrossRef]
- Howard, L.; Wibberley, C.; Crowe, L.; Body, R. How events in emergency medicine impact doctors’ psychological well-being. Emerg Med J. 2018, 35, 595–599. [Google Scholar] [CrossRef]
- Kraemer, K.M.; Luberto, C.M.; O’Bryan, E.M.; Mysinger, E.; Cotton, S. Mind-Body Skills Training to Improve Distress Tolerance in Medical Students: A Pilot Study. Teach Learn Med. 2016, 28, 219–228. [Google Scholar] [CrossRef]
- Logan, J.G.; Barksdale, D.J. Allostasis and allostatic load: Expanding the discourse on stress and cardiovascular disease. J Clin Nurs. 2008, 17, 201–208. [Google Scholar] [CrossRef]
- McEwen, B.S. Neurobiological and Systemic Effects of Chronic Stress. Chronic Stress (Thousand Oaks) 2017, 1, 2470547017692328. [Google Scholar] [CrossRef]
- Levy-Gigi, E.; Donner, R.; Bonanno, G.A. Free Your Mind: Emotional Expressive Flexibility Moderates the Effect of Stress on Post-Traumatic Stress Disorder Symptoms. Int J Mol Sci. 2020, 21, 5355. [Google Scholar] [CrossRef]
- Ashman, T.A.; Gordon, W.A.; Cantor, J.B.; Hibbard, M.R. Neurobehavioral consequences of traumatic brain injury. Mt Sinai J Med. 2006, 73, 999–1005. [Google Scholar]
- Anderson, M.I.; Parmenter, T.R.; Mok, M. The relationship between neurobehavioural problems of severe traumatic brain injury (TBI), family functioning and the psychological well-being of the spouse/caregiver: Path model analysis. Brain Inj. 2002, 16, 743–757. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.; Linn, R.T.; Gutierrez, H.; Willer, B.S. Family burden following traumatic brain injury. Rehabil. Psychol. 1994, 39, 29–48. [Google Scholar] [CrossRef]
- Manskow, U.S.; Friborg, O.; Røe, C.; Braine, M.; Damsgard, E.; Anke, A. Patterns of change and stability in caregiver burden and life satisfaction from 1 to 2 years after severe traumatic brain injury: A Norwegian longitudinal study. NeuroRehabilitation 2017, 40, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Mathers, C.D. History of global burden of disease assessment at the World Health Organization. Arch Public Health 2020, 78, 77. [Google Scholar] [CrossRef] [PubMed]
- Engel, G.L. The clinical application of the biopsychosocial model. Am J Psychiatry 1980, 137, 535–544. [Google Scholar] [CrossRef]
- Schlebusch, L. Health Psychology in South Africa: An Introduction. South Afr. J. Psychol. 1996, 26, 1–3. [Google Scholar] [CrossRef]
- Mo, Q.; Ma, Z.; Wang, G.; Jia, C.; Niu, L.; Zhou, L. The pattern of stressful life events prior to suicide among the older adults in rural China: A national case-control psychological autopsy study. BMC Geriatr. 2020, 20, 473. [Google Scholar] [CrossRef]
- Schlebusch, L. The development of a stress symptom checklist. South Afr. J. Psychology 2004, 34, 327–349. [Google Scholar] [CrossRef]
- Lo Castro, A.M.; Schlebusch, L. The measurement of stress in breast cancer patients. South Afr. J. Psychol. 2006, 36, 762–779. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Schlebusch, L. Andriessen, K., Krysinska, K., Grad, O.T., Eds.; South Africa—Experiences of suicide survivors support. In Postvention in action: The international handbook of suicide bereavement support; Hogrefe: Göttingen, Germany, 2017; pp. 377–382. [Google Scholar]
- Schlebusch, L. Postvention in suicide survivor support: Some ethical considerations. Ment. Health Matters 2020, 7, 12–13. [Google Scholar]
- Auxéméry, Y.; Gayraud, F. Post-concussion syndrome: Still forgotten? From the disappearance of the DSM-5 to a multidisciplinary consultation. Encephale 2020, S0013-7006(20)30206-2. [Google Scholar] [CrossRef] [PubMed]
- de Vries, P.J.; Wilde, L.; de Vries, M.C.; Moavero, R.; Pearson, D.A.; Curatolo, P. A clinical update on tuberous sclerosis complex-associated neuropsychiatric disorders (TAND). Am J Med Genet C Semin Med Genet. 2018, 178, 309–320. [Google Scholar] [CrossRef] [PubMed]
- Khondowe, O.; Rhoda, A.; Mpofu, R. Perceived needs of caregivers of stroke patients’ receiving out-patient physiotherapy treatment in Lusaka, Zambia. South Afr. J. Physiother. 2007, 63, 14–17. [Google Scholar] [CrossRef]
- Hux, K.; Schram, C.D.; Goeken, T. Misconceptions about brain injury: A survey replication study. Brain Inj. 2006, 20, 547–553. [Google Scholar] [CrossRef]
- Maunsell, H.; Tyerman, A.; Barton, S.; Bramley, M. Ongoing support needs after brain injury, as reported by a long-term relatives’ group. Neuropsychol. 2015, 22–24. [Google Scholar] [CrossRef]
- Diaz, A.P.; Schwarzbold, M.L.; Thais, M.E.; Hohl, A.; Bertotti, M.M.; Schmoeller, R.; Nunes, J.C.; Prediger, R.; Linhares, M.N.; Guarnieri, R.; Walz, R. Psychiatric disorders and health-related quality of life after severe traumatic brain injury: A prospective study. J Neurotrauma. 2012, 29, 1029–1037. [Google Scholar] [CrossRef]
- Grossman, P.; Niemann, L.; Schmidt, S.; Walach, H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004, 57, 35–43. [Google Scholar] [CrossRef]
- van der Klink, J.J.; Blonk, R.W.; Schene, A.H.; van Dijk, F.J. The benefits of interventions for work-related stress. Am J Public Health. 2001, 91, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Southwick, S.M.; Bonanno, G.A.; Masten, A.S.; Panter-Brick, C.; Yehuda, R. Resilience definitions, theory, and challenges: Interdisciplinary perspectives. Eur J Psychotraumatol. 2014, 5. [Google Scholar] [CrossRef] [PubMed]
- Ungar, M.; Theron, L.; Murphy, K.; Jefferies, P. Researching Multisystemic Resilience: A Sample Methodology. Front Psychol. 2021, 11, 607994. [Google Scholar] [CrossRef] [PubMed]
- Theron, L.C.; Theron, A.M.; Malindi, M.J. Toward an African definition of resilience: A rural South African community’s view of resilient Basotho youth. J. Black Psychol. 2013, 39, 63–87. [Google Scholar] [CrossRef]
- Thoits, P.A. Stress and health: Major findings and policy implications. J Health Soc Behav. 2010, 51 (Suppl. S41–S53). [Google Scholar] [CrossRef]
- Smith, L.M.; Godfrey, H.P.D. Family support programs and rehabilitation: A cognitive-behavioural approach to traumatic brain injury; Plenum Press: New York, NY, USA, 1995. [Google Scholar]

 |
© 2021 by the author. 2021 Janet Walker, Lourens Schlebusch, Bernhard Gaede
Share and Cite
Walker, J.; Schlebusch, L.; Gaede, B. Support for Family Members Who Are Caregivers to Relatives with Acquired Brain Injury. J. Mind Med. Sci. 2021, 8, 76-85. https://doi.org/10.22543/7674.81.P7685
Walker J, Schlebusch L, Gaede B. Support for Family Members Who Are Caregivers to Relatives with Acquired Brain Injury. Journal of Mind and Medical Sciences. 2021; 8(1):76-85. https://doi.org/10.22543/7674.81.P7685
Chicago/Turabian StyleWalker, Janet, Lourens Schlebusch, and Bernhard Gaede. 2021. "Support for Family Members Who Are Caregivers to Relatives with Acquired Brain Injury" Journal of Mind and Medical Sciences 8, no. 1: 76-85. https://doi.org/10.22543/7674.81.P7685
APA StyleWalker, J., Schlebusch, L., & Gaede, B. (2021). Support for Family Members Who Are Caregivers to Relatives with Acquired Brain Injury. Journal of Mind and Medical Sciences, 8(1), 76-85. https://doi.org/10.22543/7674.81.P7685



