Abstract
Background. Coronavirus Disease 2019 (COVID-19, also known as 2019-nCoV), a cluster of acute respiratory illness with unknown causes, has occurred in India since January 2020. Over the past several months, the entire world is struggling to cope with and contain the virus spread. Several studies showed that mental health problems could occur in both healthcare workers and SARS survivors during the SARS epidemic. Considering the geographical variation, dense population, multi-strata health care structure, and rising COVID cases in South India, we have a reason to speculate that the burden on the frontline doctors is high and their psychological condition may also be affected during COVID-19 outbreak. Aims. The aim of the study is to estimate the anxiety and depression among front line doctors during COVID 19 duty in south India and also the impact of the various strata of health care on the depression and anxiety scores. Methods. An online form was created which included personal details of COVID 19 duty, Beck’s anxiety and depression questionnaire. Results. Severity of anxiety and depression scores was significantly higher among front line doctors working in primary health centers when compared to medical college and private hospital doctors (p < 0.002). Conclusion. Our study verified the results from previous reports that anxiety and depression are high among doctors posted in COVID duties, but also that they remain largely unaddressed. We provide new findings regarding the nature of work place and the mental health issues.
Introduction
Coronavirus Disease 2019 (COVID-19, also known as 2019-nCoV), a cluster of acute respiratory illness with unknown causes, has occurred in India since January 2020. Over the past several months, the entire world is struggling to cope with and contain the virus spread [1]. In view of the urgency of this outbreak, the international community is mobilizing to find ways to significantly accelerate the development of intervention, having declared the pandemic a Public Health Emergency of International Concern [2].
Evidence has indicated that COVID-19 is a distinct clad from the beta corona viruses related to human severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) [3]. The severity of the disease has both immediate and long-term physical health implications [2], but in addition it is also having a potentially serious impact on the mental health of the public. Large scale disasters of any type are almost always accompanied by increase in depression, and it appears that the COVID-19 pandemic will be no exception [4].
COVID and healthcare workers
Several studies have shown that mental health problems occurred in both healthcare workers and SARS survivors during the SARS epidemic [5,6]. Post-traumatic stress disorder (PTSD) and depressive disorders were the most prevalent long-term psychological effects [7,8]. Health care professionals are often working round the clock, traveling substantial distances, and separating from family in order to assist people in need. In addition, the long hours of work may result in insufficient rest and sleep time. Doctors and health care workers reportedly show a high prevalence of mental health care issues, but the topic needs further study [9]. Furthermore, health care workers face the likelihood of burnout due to prolonged periods of overtime, an overburdened health care system, and shortages of appropriate resources. A previous study, for example, conducted during the outbreak of Middle East Respiratory Syndrome, reported a 26.6% prevalence of depression among doctors [10]. The high number of confirmed and suspected cases, excessive workload, lack of personal protective equipment, exhaustive media coverage, and lack of target medications can all contribute to the mental burden of the health professional [5,11,12].
The uncertainty posed by the coronavirus has placed an extra burden on health professionals who may have suffered from anxiety and OCD in the past [13]. A study by conducted by Seshadri Sekar Chatterjee et al in West Bengal (North India) showed 34.9% of the doctors were depressed and 39.5% reported anxiety [14]. Considering the geographical variation, dense population, multi-strata health care structure, and rising COVID cases in South India, we have a reason to speculate that the burden on the frontline doctors is high and that their psychological condition may also be affected during COVID-19 outbreak. Only a limited number of studies have addressed mental health issues related to COVID 19, and none have assessed the mental health of frontline doctors in South India.
Materials and Methods
This study was a cross-sectional survey using convenience sampling. Participants were doctors in South India aged 24-45 years of age who were posted in COVID 19 duties and willing to participate in the study. Study duration was two months. An online questionnaire was generated and circulated among doctors posted in COVID duties through e-mail. Participants completed and mailed the questionnaire independently and anonymously, and a gift card was mailed to express gratitude for their participation. This study was approved by the research ethics committees of the medical college hospital. All information collected through this survey was strictly confidential.
MEASURES
The online questionnaire gathered personal and demographic information, including age, gender, sex, specialization, marital status, workplace location, number of days spent on COVID duty, specialization, nature of COVID duty ranging from screening to ICU duties, and work setting, such as Primary Health Centre, General Hospital, or Medical college, which represent all strata of the current health care structure in South India.
SCALES
- 1.
- Becks depression inventory
The Beck Depression Inventory (BDI) is a 21-item, self-report rating inventory that measures characteristic attitudes and symptoms of depression. The 21 symptoms and attitudes contained in the BDI reflect the intensity of the depression; items receive a rating of 0-3 to reflect their intensity and are summed linearly to create a score ranging from 0 to 63. It has high internal consistency and reliability among both psychiatric and non-psychiatric populations. The Pearson r between the odd and even categories yielded a reliability coefficient of 0.86 and with a Spearman-Brown correction, the coefficient rose to 0.93 [15].
- 2.
- Becks anxiety inventory
Beck Anxiety Inventory (BAI) is a 21-item scale with high internal consistency (α r.75. The scale discriminates anxious diagnostic groups (Panic disorder, generalized anxiety disorder) from no anxious diagnostic groups (Major depression, Dysthymic disorder). The scale is moderately correlated with the revised Hamilton Anxiety Rating Scale, = (81) r.51, and mildly correlated with the revised Hamilton Depression Rating Scale, = (150) r.25 = (153) [16].
SAMPLE SIZE CALCULATION
Based on the review of literature by Samara in 2020, the prevalence of depression and anxiety was 51%, with the limit of accuracy as 10% of the anticipated prevalence, the Z alpha value of 1.96, the sample size was calculated as (n=96) [17].
STATISTICAL ANALYSIS
Perception parameters were represented as percentages. Comparison test of significance for frequencies used the Chi square test. Association between the study variables was evaluated using odds ratio. Comparison between the groups was done using ANOVA. SPSS Licensed Statistical software version 16 was used for data analysis.
Results
CHARACTERISTICS OF THE STUDY POPULATION
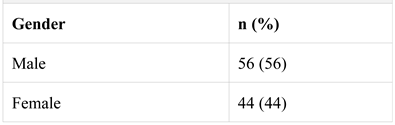
The age group range for study participants was 20-51 years, with 56 men and 44 women. Among study participants, 62 were married and 38 were unmarried. 65% of participants completed post-graduation (Table 1).

Table 1.
Distribution of male and female participants.
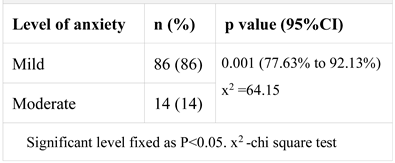
ANXIETY SCORES
86% of the sample showed low anxiety and 14% moderate anxiety, as per Beck anxiety score (p<0.001, x2 =64.15) (Table 2).

Table 2.
Distribution of anxiety among study participants.
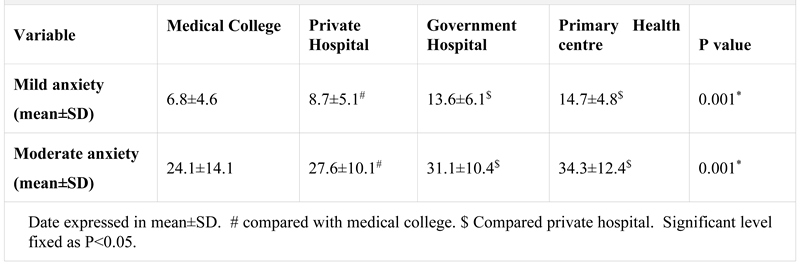
Anxiety was more predominant in males when compared to females. The odds of developing anxiety among males was 6 times higher compared to females (OR 6.02, 95%CI 2.6029 to 13.8306, p <0.0001). Severity of anxiety was significantly higher among front line doctors working in primary health center when compared to doctors in medical college and private hospital settings (P<0.001) (Table 3). However, there was no significant result in anxiety score with respect to nature of duty (screening, corona suspect ward, corona positive ward, corona ICU).

Table 3.
Comparison of anxiety with different work locations.
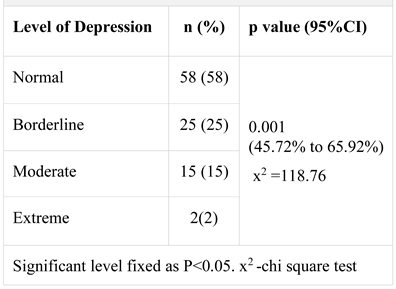
DEPRESSION SCORES
With respect to depression, 58% of the sample was in the normal range, 25% showed borderline depression, 15% showed moderate depression, and 2 % severe depression (p<0.001, x2 =118.76) (Table 4). Similar to anxiety, depression was also more predominant in males compared to females. The odds of developing depression among males was 6 times higher compared to females (OR 8.33, 95%CI 3.3068 to 21.0005, p <0.0001).

Table 4.
Distribution of depression among study participants.
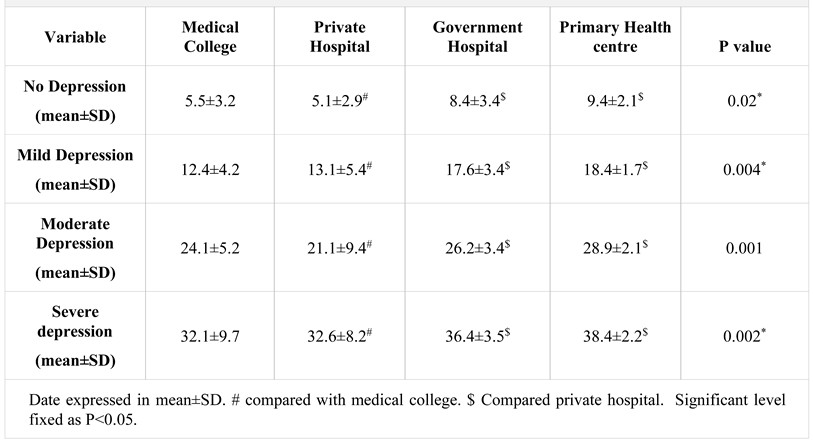
Severity of depression scores was significantly higher among frontline doctors working in primary health centers compared to medical college and private hospital settings (P=0.002) (Table 5). However, there was no significant variation in depression score with respect to nature of duty (screening, corona suspect ward, corona positive ward, corona ICU).

Table 5.
Comparison of depression with different work locations.
Discussions
MAIN FINDINGS
Majority of the study sample had low anxiety (86%), and 40% had either low or moderate depression. The percentage showing severe depression was low. No participants were taking medications such as antidepressants, anxiolytics, or benzodiazepines, which generally ruled out pre-existing anxiety or depressive disorder. With respect to work locations, significant p value was found in doctors working in Primary Health Centers compared with other work places like medical college or a private hospital setting.
COMPARISON WITH PREVIOUS STUDIES
A recent analysis by Jianbo Lai et al. on 1257 health care workers in China reported depression in 50.4% of the sample, and anxiety in 44.6% [12]. Women health care workers and health care workers in Wuhan reported higher incidence of anxiety, depression, and distress. Our study sample depicted similar values for depression, but lower levels of anxiety. In contrast with Jianbo Lai et al., in our study men had higher odds of developing anxiety and depression. This difference might be due to predominance of female nursing staff in the Wuhan study.
Regarding the work place, frontline doctors posted in Primary Health Care Centers were higher in both anxiety and depression compared to those in medical colleges and private hospitals, perhaps due to the blinded exposure to probable COVID patients, these staff serve as gatekeepers to the health system. They may be exposed to positive patients (without knowing beforehand) and thus must refer them to a higher medical facility, whereas in other health care facilities like medical colleges and hospitals, frontline doctors deal with already diagnosed COVID patients with full protection like PPEs. A study in North India showed results of 35% of depressive symptoms and 33% of anxiety symptoms in doctors posted in COVID duty, findings that were similar to ours [14]. A study Um DH et al. in South Korea during the MERS outbreak showed a 26% rate of depression, but the sample size at 64 was quite small [10].
RELEVANCE IN HEALTH CARE POLICY
The results of this study suggest two public health directions. One is the need to address the psychological burden on the gatekeepers of the health care system, those on the frontline at Primary Health Care Centers. This can be achieved by providing appropriate Personal Protective Equipment, ensuring they take adequate protective measures, and requiring them to consider every patient with COVID symptoms as a positive patient unless found otherwise—measures that might mitigate psychological tension, depression, and anxiety. The second is to provide hot line numbers to all doctors working in COVID duties. Trained psychologists and psychiatrists at these hot line numbers could provide critical psychological support, as suggested by Geoffroy et al. [18].
STRENGTH AND LIMITATIONS
Ours is the first study to estimate the anxiety and depression exclusively in doctors posted in COVID, as previous studies have included all health care professionals such as doctors, nurses, lab workers, and other paramedics. Ours is the first such study conducted in southern India. None of the previous studies had analyzed different characteristics of the health care system, such as working hours and nature of the work. Limitations include the cross-sectional nature of the study. Data regarding frontline doctors in higher care centers like ICU or tertiary care centers may be underrepresented in our study, as data were collected during April and May, 2020, which was early in the COVID pandemic in India. Asymptomatic and mildly symptomatic cases were high at that time, and need for referral to higher centers was low.
Conclusions
Our study verified results from previous reports that anxiety and depression can be high among doctors posted in COVID duties. The results stress the need for providing mental health support for frontline health care staff.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
References
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef] [PubMed]
- COVID 19 Public Health Emergency of International Concern (PHEIC) (2020). Global research and innovation forum: towards a research roadmap. WHO. Available online: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum.
- Zhu, N.; Zhang, D.; Wang, W.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Galea, S.; Merchant, R.M.; Lurie, N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern Med. 2020, 180, 817–818. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.M.; Wong, J.G.; McAlonan, G.M.; et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007, 52, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.C.; Shu, B.C.; Chang, Y.Y.; Lung, F.W. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychother Psychosom. 2006, 75, 370–375. [Google Scholar] [CrossRef] [PubMed]
- McAlonan, G.M.; Lee, A.M.; Cheung, V.; et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007, 52, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Tracy, M.; Norris, F.H.; Galea, S. Differences in the determinants of posttraumatic stress disorder and depression after a mass traumatic event. Depress Anxiety. 2011, 28, 666–675. [Google Scholar] [CrossRef] [PubMed]
- Misra, A. Doctors and healthcare workers at frontline of COVID 19 epidemic: Admiration, a pat on the back, and need for extreme caution. Diabetes Metab Syndr. 2020, 14, 255–256. [Google Scholar] [CrossRef] [PubMed]
- Um, D.H.; Kim, J.S.; Lee, H.W.; Lee, S.H. Psychological effects on medical doctors from the Middle East Respiratory Syndrome (MERS) outbreak: A comparison of whether they worked at the MERS occurred hospital or not, and whether they participated in MERS diagnosis and treatment. J Korean Neuropsychiat Assoc. 2017, 56, 28–34. [Google Scholar]
- The State Council of China, 2020. A notification to set up nationwide psychological assistance hotlines against the 2019-nCoV outbreak. Available online: http://www.gov.cn/xinwen/2020-02/02/content_5473937.htm.
- Lai, J.; Ma, S.; Wang, Y.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Neto, M.L.R.; Almeida, H.G.; Esmeraldo, J.D.; et al. When health professionals look death in the eye: the mental health of professionals who deal daily with the 2019 coronavirus outbreak. Psychiatry Res. 2020, 288, 112972. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.S.; Bhattacharyya, R.; Bhattacharyya, S.; Gupta, S.; Das, S.; Banerjee, B.B. Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian J Psychiatry. 2020, 62, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch Gen Psychiatry. 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, S. COVID-19 Affects Mental Health of Nurses, Frontline Workers More Than Others. HCP Live. 2020. Available online: https://www.hcplive.com/view/covid-19-affects-mental-health-nurses-frontline-more.
- Geoffroy, P.A.; Le Goanvic, V.; Sabbagh, O.; et al. Psychological Support System for Hospital Workers During the Covid-19 Outbreak: Rapid Design and Implementation of the Covid-Psy Hotline. Front Psychiatry. 2020, 11, 511. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the author. 2020 Vishnupriya Veeraraghavan, Krishnan Srinivasan