Indicators of Psychological Distress and Body Image Disorders in Female Patients with Breast Cancer
Abstract
Introduction
Cancer-specific stress disorders in breast patients
Body image disorders in breast cancer patients
Materials and Methods
Participants
Materials
- Brief demographic questionnaire: a brief demographic questionnaire detailing the participant’s age, marital status, and medical history.
- The Beck Depression Inventory (BDI) [24]: This is a widely-used, 21-item multiple-choice inventory measuring attitudes and severity of depressive symptomatology. Pertinent to the present study are items relating to irritability, pessimism, feelings of guilt or being punished, self-dissatisfaction, and social withdrawal, in addition to physiological symptoms such as tiredness, weight loss, and loss of libido. This inventory evaluates depression in normal and psychiatric populations. Several items indicate the presence of hopelessness and suicidal ideation. Items are scored on a 4-point continuum, with the total score range being 0–63. High scores point to more severe level of depression.
- The Rosenberg Self-Esteem Scale [25]: This widely-used scale measures global self-esteem using a 10-item Likert-type scale. It comprises a scale of 0–30, with a score of less than 15 indicative of low self-esteem. Of the 10 items, five are positively worded statements and five are negatively worded. This scale measures global self-worth by means of measuring both positive and negative perceptions of the self. It is considered reliable and valid for the assessment of self-esteem
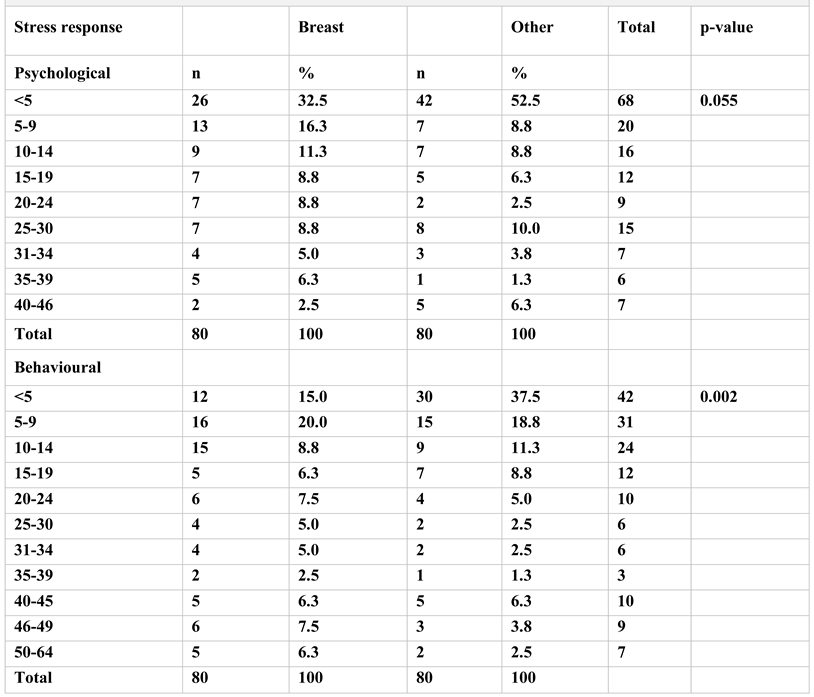
- The Stress Symptom Checklist (SSCL) [26]: This is an 87-item checklist relating to symptoms of unhealthy stress. The intensity or severity of stress is measured as reported by the patient’s reactions across 3 dimensions: physical (18 items), psychological (27 items), and behavioural (42 items). Each dimension is separately scored with a score of three or more indicative of elevated stress. High scores signify high levels of stress. The maximum score is 87. The checklist allows for further interpretation, with scores of 8 and below indicative of low stress, mild stress ranging from 9 to 15, moderate stress from 16 to 30, and the severe stress from 31 to 45. Profound stress is reflected in scores of 46 and above. Moreover, the SSCL offers an indication as to whether the respondent reflects stress reactions which are mainly physical or psychological and/or behavioural in nature. This scale is a useful clinical measure of stress.
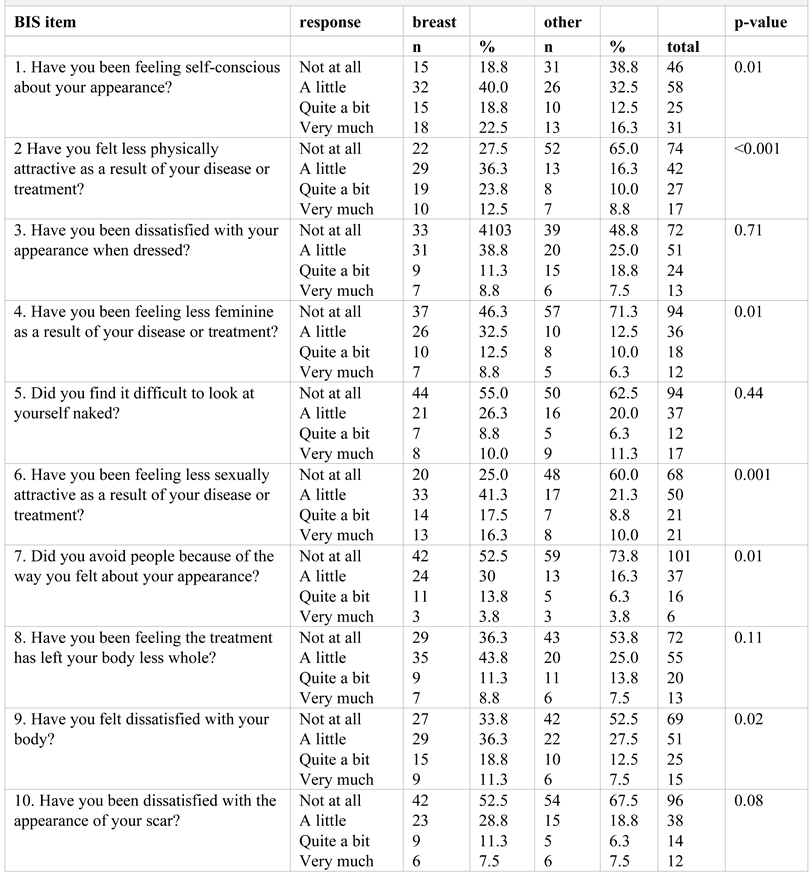
- Body Image Scale (BIS) [18]: The BIS is a 10-item, patient-reported outcome scale designed to briefly but comprehensively rate 3 dimensions of body image, for use exclusively with cancer patients: the affective (pertaining to feelings such as self-consciousness), behavioural (for example difficulties with looking at oneself naked) and cognitive (level of satisfaction with appearance). There is a 4-point response scale, the final score being the sum of all 10 items, with a range of 0-30. Low scores signify fewer symptoms and lower levels of body image distress while higher scores are associated with more symptoms and greater body image dysphoria.
Results
Discussions
Therapeutic interventions
Highlights
- ✓
- Breast cancer patients experience psychological distress differently as compared to patients with other sites of disease.
- ✓
- Specific body image disturbances and elevated stress are prominent sequelae of breast cancer.
- ✓
- The prevalence and severity of these comorbid symptoms warrant closer observation of patients to facilitate identification those at risk of distress.
Conclusions
Conflict of interest disclosure
Compliance with ethical standards
Acknowledgments
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018, 68, 394–424. [Google Scholar] [PubMed]
- World Heath Organization. Cancer. Available online: https://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/.
- Narod, S.A.; Iqbal, J.; Miller, A.B. Why have breast cancer mortality rates declined? J of Cancer Policy. 2015, 5, 8–17. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA A Cancer J Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef]
- Naughton, M.J.; Weaver, K.E. Physical and mental health among cancer survivors: Considerations for long-term care and quality of life. N C Med J. 2014, 75, 283–286. [Google Scholar] [CrossRef]
- Kang, D.H.; Park, N.J.; McArdle, T. Cancer-specific stress and mood disturbance: Implications for symptom perception, quality of life, and immune response in women shortly after diagnosis of breast cancer. ISRN Nurs. 2012, 2012, 608039. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.; Salmon, P.; Tudur-Smith, C.; Huntley, C.D.; Fisher, P.L. A systematic review of the quality of randomized controlled trials of psychological treatments for emotional distress in breast cancer. J of Psychosom Res. 2018, 108, 22–31. [Google Scholar]
- Taub, C.J.; Lippman, M.E.; Hudson, B.I.; Blomberg, B.B.; Diaz, A.; Fisher HM et, a.l. The effects of a randomized trial of brief forms of stress management on RAGE-associated S100A8/A9 in patients with breast cancer undergoing primary treatment. Cancer. 2019, 125, 1717–25. [Google Scholar] [CrossRef]
- Martinez, M.R.; Pasha, A. Prioritizing Mental Health Research in Cancer Patients and Survivors. AMA J Ethics. 2017, 19, 486–492. [Google Scholar] [CrossRef][Green Version]
- Sherman, K.A.; Przezdziecki, A.; Alcorso, J.; et al. Reducing Body Image-Related Distress in Women With Breast Cancer Using a Structured Online Writing Exercise: Results From the My Changed Body Randomized Controlled Trial. J Clin Oncol. 2018, 36, 1930–1940. [Google Scholar] [CrossRef]
- Van Oers, H. Body image and the psychological and behavioural indices of distress in female breast cancer patients. World Scientific News. 2020, 140, 172–184. [Google Scholar]
- Schoemaker, M.J.; Jones, M.E.; Wright, L.B.; et al. Psychological stress, adverse life events and breast cancer incidence: A cohort investigation in 106,000 women in the United Kingdom. Breast Cancer Res. 2016, 18, 72. [Google Scholar] [CrossRef] [PubMed]
- Schlebusch, L. Mind Shift: Stress management and your health; University of KwaZulu-Natal Press: Pietermaritzburg, South Africa, 2000; ISBN 13: 978-0869809563. [Google Scholar]
- Soung, N.K.; Kim, B.Y. Psychological stress and cancer. J Anal Sci Technol. 2015, 69300. [Google Scholar] [CrossRef]
- Barre, P.V.; Padmaja, G.; Rana, S.; Tiamongla. Stress and Quality of Life in Cancer Patients: Medical and Psychological Intervention. Indian J Psychol Med. 2018, 40, 232–238. [Google Scholar]
- Moreno-Smith, M.; Lutgendorf, S.K.; Sood, A.K. Impact of stress on cancer metastasis. Future Oncol. 2010, 6, 1863–1881. [Google Scholar] [CrossRef] [PubMed]
- Paterson, C.L.; Lengacher, C.A.; Donovan, K.A.; Kip, K.E.; Tofthagen, C.S. Body Image in Younger Breast Cancer Survivors: A Systematic Review. Cancer Nurs. 2016, 39, E39–E58. [Google Scholar] [CrossRef]
- Hopwood, P.; Fletcher, I.; Lee, A.; Al Ghazal, S. A body image scale for use with cancer patients. Eur J Cancer. 2001, 37, 189–197. [Google Scholar] [CrossRef]
- Falk Dahl, C.A.; Reinertsen, K.V.; Nesvold, I.L.; Fosså, S.D.; Dahl, A.A. A study of body image in long-term breast cancer survivors. Cancer. 2010, 116, 3549–3557. [Google Scholar] [CrossRef]
- Cash, T.F. Cash, T.F., Smolak, L., Eds.; Cognitive-behavioral perspectives on body image In Body image: A handbook of science, practice, and prevention; The Guilford Press: New York, NY, USA, 2011; pp. 39–47. [Google Scholar]
- Jones, D.P. Cultural views of the female breast. ABNF J. 2004, 15, 15–21. [Google Scholar]
- Kieszkowska-Grudny, A.; Rucinska, M.; Ciesak, R.; Wisniewska, M. Body image, self-esteem and quality of life during oncology treatment in breast cancer, cervical cancer, and prostate cancer in comparison to the healthy population. Journal of Clinical Oncology. 2017, 35 (Suppl. S15), e21550–e21550. [Google Scholar] [CrossRef]
- Fallbjörk, U.; Rasmussen, B.H.; Karlsson, S.; Salander, P. Aspects of body image after mastectomy due to breast cancer - a two-year follow-up study. Eur J Oncol Nurs. 2013, 17, 340–345. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961, 4, 561–571. [Google Scholar]
- Rosenberg, M. Society and the adolescent self-image; Princeton University Press: Princeton, NJ, USA, 1965; ISBN 9780691649443. [Google Scholar]
- Schlebusch, L. The development of a Stress Symptom Checklist. SA J Psychol. 2004, 34, 327–349. [Google Scholar]
- Ng, C.G.; Mohamed, S.; Kaur, K.; Sulaiman, A.H.; Zainal, N.Z.; Taib, N.A.; et al. Perceived distress and its association with depression and anxiety in breast cancer patients. PLoS ONE. 2017, 12, e0172975. [Google Scholar] [CrossRef]
- Tiezzi, M.F.B.; de Andrade, J.M.; Romão, A.P.M.; Tiezzi, D.G.; Lerri, M.R.; Carrara, H.A.H.; et al. Quality of life in women with breast cancer treated with or without chemotherapy. Cancer Nursing. 2017, 40, 108–116. [Google Scholar] [PubMed]
- Brandberg, Y.; Sandelin, K.; Erikson, S.; et al. Psychological reactions, quality of life, and body image after bilateral prophylactic mastectomy in women at high risk for breast cancer: A prospective 1-year follow-up study. J Clin Oncol. 2008, 26, 3943–3949. [Google Scholar] [CrossRef]
- Grogan Sarah, Taylor and Francis (2016). Body Image, ProQuest Ebook Central. Available online: https://ebookcentral. proquest.com/lib/nottingham/detail.action?docID=471 0093.
- Esplen, M.J.; Wong, J.; Warner, E.; Toner, B. Restoring Body Image After Cancer (ReBIC): Results of a Randomized Controlled Trial. J Clin Oncol. 2018, 36, 749–756. [Google Scholar] [CrossRef]
- Casellas-Grau, A.; Font, A.; Vives, J. Positive psychology interventions in breast cancer. A systematic review. Psychooncology. 2014, 23, 9–19. [Google Scholar] [CrossRef]
- Vachon, M. Psychosocial distress and coping after cancer treatment. How clinicians can assess distress and which interventions are appropriate--what we know and what we don't. Am J Nurs 2006, 106 (Suppl. S3), 26–31. [Google Scholar] [CrossRef]
- Daniels, S. Cognitive behavior therapy for patients with cancer. J Adv Pract Oncol. 2015, 6, 54–56. [Google Scholar]
- Jassim, G.A.; Whitford, D.L.; Hickey, A.; Carter, B. Psychological interventions for women with non-metastatic breast cancer. Cochrane Database Syst Rev. 2015, 5, CD008729. [Google Scholar] [CrossRef]
- Miovic, M.; Block, S. Psychiatric disorders in advanced cancer. Cancer. 2007, 110, 1665–1676. [Google Scholar] [PubMed]
- Ayub, N.; Kimong, P.J.; Ee, G.T. A distorted body image: Cognitive behavioral therapy for body dysmorphic disorder. [Online First]. IntchOpen 2018. [Google Scholar] [CrossRef]
- Lewer, M.; Kosfelder, J.; Michalak, J.; Schroeder, D.; Nasrawi, N.; Vocks, S. Effects of a cognitive-behavioral exposure-based body image therapy for overweight females with binge eating disorder: A pilot study. J Eat Disord. 2017, 5, 43. [Google Scholar] [CrossRef]
 |
 |
© 2020 by the author. 2020 Helena van Oers, Lourens Schlebusch
Share and Cite
van Oers, H.; Schlebusch, L. Indicators of Psychological Distress and Body Image Disorders in Female Patients with Breast Cancer. J. Mind Med. Sci. 2020, 7, 179-187. https://doi.org/10.22543/7674.72.P179187
van Oers H, Schlebusch L. Indicators of Psychological Distress and Body Image Disorders in Female Patients with Breast Cancer. Journal of Mind and Medical Sciences. 2020; 7(2):179-187. https://doi.org/10.22543/7674.72.P179187
Chicago/Turabian Stylevan Oers, Helena, and Lourens Schlebusch. 2020. "Indicators of Psychological Distress and Body Image Disorders in Female Patients with Breast Cancer" Journal of Mind and Medical Sciences 7, no. 2: 179-187. https://doi.org/10.22543/7674.72.P179187
APA Stylevan Oers, H., & Schlebusch, L. (2020). Indicators of Psychological Distress and Body Image Disorders in Female Patients with Breast Cancer. Journal of Mind and Medical Sciences, 7(2), 179-187. https://doi.org/10.22543/7674.72.P179187



