Highlights
- Gracilis myocutaneous flap seems to be an effective and feasible method of perineal reconstruction after extended perineal resection for gynecological malignancies, including vulvar cancer.
Abstract
Performing radical surgery for locally advanced vulvar cancer is usually associated with the occurrence of large perineal defects. In order to provide a better healing process of the perineal wound, different reconstructive techniques have been proposed. We present the case of a 63-year-old female patient diagnosed with locally advanced vulvar cancer for which a left hemivulvectomy with bilateral inguinal lymph node dissection was performed. After completion of the resection phase, the reconstruction with gracilis myocutaneous flap was performed. The patient developed a non-union of the flap. However, it slowly healed without any surgical re-intervention. Gracilis myocutaneous flap seems to be an effective and feasible method of perineal reconstruction after extended perineal resection for gynecological malignancies, including vulvar cancer. The method appears effective even in pre-irradiated patients with larger perineal wounds resulting after total pelvic exenteration for locally advanced gynecological malignancies.
Highlights
- ✓
- Gracilis myocutaneous flap seems to be an effective and feasible method of perineal reconstruction after extended perineal resection for gynecological malignancies, including vulvar cancer.
Introduction
Vulvar cancer is a rare gynecological malignancy which, unfortunately, is usually diagnosed only after a long period of evolution. Most women diagnosed with this neoplastic lesion are elderly and they tend to ignore the occurrence of local symptoms such as bleeding, pruritus, or local development of a tumoral mass for a long period of time.
Therefore, in a significant number of cases, the diagnosis will be made in advanced stages of the disease, a good local control of the disease being achieved only after performing extensive perineal resections.
However, in these cases, although the oncological outcomes will generally be favorable, the patient will most often experience difficult healing of the perineal wound, wound dehiscence, infection, or, in cases associated with pelvic exenteration, even perineal herniation. As a consequence, attention was focused on limiting these debilitating postoperative complications by using myocutaneous flaps [1,2,3,4].
Case Report
The 63-year-old patient with no significant previous medical history self-referred to the gynecological service due to the occurrence of a tumoral lesion at the level of the left hemi-vulvar region. The biopsy of the lesion confirmed the presence of a moderately differentiated squamous cell vulvar carcinoma, and therefore, she was submitted to surgery with radical intent.
A left radical hemivulvectomy was performed, in association with inguinal and pelvic lymph node dissection. After completion of the resection phase, the patient was submitted to perineal reconstruction using a left myocutaneous flap originating in the left gracilis muscle. After dissecting the flap and pediculising it, the flap was rotated and fixed to the perineal wound in order to close the defect (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5 and Figure 6).

Figure 1.
The final aspect after left hemivulvectomy for locally advanced vulvar cancer.
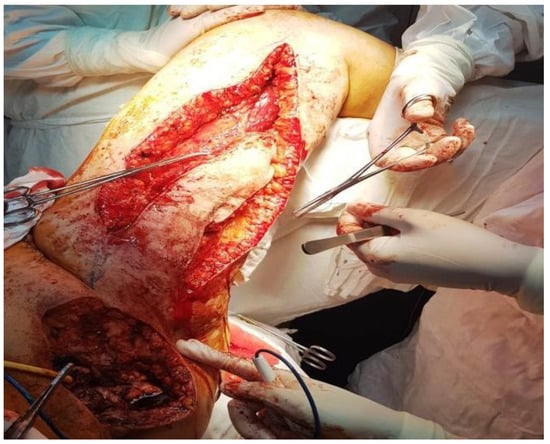
Figure 2.
Preparation of the the gracilis myocuta- neous flap.

Figure 3.
Pediculization of the flap by using the most proximal vascular pedicle.
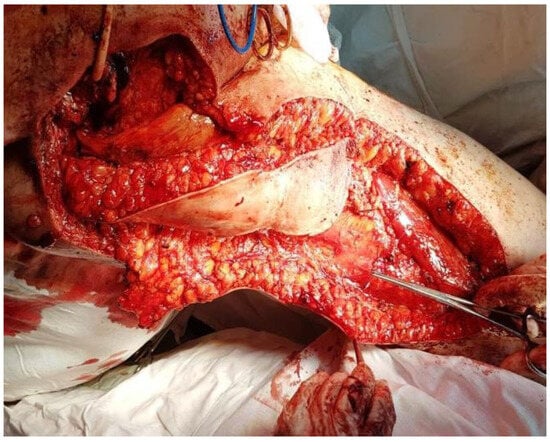
Figure 4.
The aspect after the complete dissection of the flap.

Figure 5.
Translation and suturing of the gracilis myocutaneous flap.
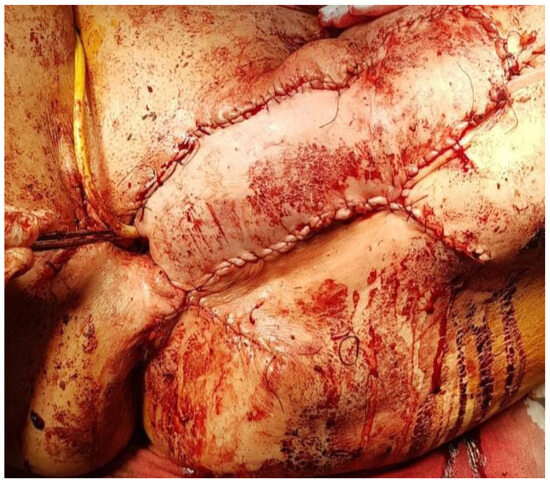
Figure 6.
The final aspect after suturing the flap.
The early postoperative evolution was marked by the occurrence of an early non-union of the distal part of the flap, which was successfully handled in a conservative manner.
Discussion
The gracilis muscle represents a minor adductor of the lower limb originating in the pubic bone and inserting on the medial tibial condyle, with vascularization originating in the medial circumflex branch of the profound femoral artery [5,6]. The transposition of the flap will usually result in functional disability of the lower limb; however, the degree of flap rotation can be significantly limited by the insertion of the vascular pedicle [6,7].
Myocutaneous flaps harvested from the gracilis, gluteus maximum or rectus abdominis muscles have been considered the gold standard in vulvar reconstruction for years. The choice between different flaps after vulvar resection seems to be strongly influenced by the location of the defect. Thus, in cases presenting anterior extended resections, vascularization from the medial circumflex femoral artery perforator should be used, a gracilis flap being performed. In cases presenting posterior extended vulvar resections, a deep femoral artery perforator flap should be selected [8].
Gluteal and gracilis flaps seem to be an appropriate reconstructive method for medium-sized defects (measuring between 20 and 60 cm3) resulting from anal- rectal, vaginal, or vulvar resections, addressed to locally advanced perineal malignancies [9]. Described for the first time by McCraw et al. in 1976 [10], gracilis myocutaneous flaps have rapidly become an attractive choice of vulvar reconstruction [10,11]. In order to assure an adequate vascularization of the flap, dissection of the branches of the medial circumflex femoral artery is recommended. After placing the patient in a lithotomy position, an incision on the medial side of the thigh is made in order to identify the distal part of the gracilis muscle. After dissecting the distal end of the gracilis muscle, it is mobilized to the proximal end, preserving the most proximal vascular pedicle. After completing the dissection, the resulting flap is tunneled subcutaneously in order to reach the perineal defect where it is fixed by using separate stitches. Once the reconstructive phase is completed, the defect from the thigh is closed in one layer [12].
In certain cases, placing the flap under the adductor muscle could provide additional length of the pedicle. An interesting study demonstrating the utility of placing the flap under the adductor muscles was conducted by Goldie et al., published in the Journal of Plastic, Reconstructive and Aesthetic Surgery in 2016 [13]. The study included three female cadaveric donors on whom bilateral myocutaneous gracilis was performed. The authors measured the length of the pedicle (from the branching point of the artery to the flap) and reported a mean length of reach of 3.26 cm when the flap was placed under the adductor muscles as compared to the situation in which no tunneling was performed [13].
One of the first studies demonstrating the utility of the procedure originates with Peled in 1990. That study included seven patients submitted to vulvar reconstruction with advanced gracilis myocutaneous flap; only two cases developed postoperative complications, and these were minimal [14].
Weikel et al. reported in 2005 that of 213 patients initially submitting to surgery for vulvar cancer at the Department of Obstetrics and Gynecology at the University of Mainz, myocutaneous flaps necessary to provide a better healing of the perineal defect were necessary in 19, and only one of these patients benefited from a gracilis myocutaneous flap [1].
Gracilis myocutaneous flap also seems to be a feasible alternative for perineal reconstructions after more extensive surgical procedures such as total pelvic exenteration. In the study conducted in Finland, Kaartinen et al. [15] included 12 patients submitting to total pelvic exenteration, two of them being submitted to exenteration for locally advanced vulvar cancer. In all cases, reconstruction using a transverse myocutaneous flap was performed. In six cases, unilateral reconstruction was needed, while in the remaining six, bilateral pedicle flap was performed. Of the eighteen myocutaneous flaps performed, only a single flap developed distal necrosis. Moreover, the flaps were used to reconstruct the vagina in five cases and no postoperative complications were reported. In conclusion, the authors demonstrated the utility of the method in providing better healing of the perineal wound after radical surgery for locally advanced gynecological malignancies, as well as the feasibility of the method in order to create a neo-vagina. Moreover, the authors reported no perineal herniation after this method, a single minimal flap related complication (consisting of a partial flap loss) being reported [15].
The method of pelvic reconstruction using a gracilis myocutenous flap seems to be especially important in cases with a previous history of irradiation. Beginning with the observation that a previous history of pelvic irradiation causes a 10-fold increase in the incidence of wound complications, certain authors have studied whether performing this type of perineal reconstruction could provide a decrease in the rate of postoperative complications. In the study by Vermaas et al. [7] that included 25 patients submitted to reconstruction for pelvic malignancies after irradiation, the authors reported three major complications, with a median time of healing of 17 days for the donor site and 190 days for the perineal defect. However, no necrosis of the gracilis myocutaneous flap was encountered. In conclusion, the authors demonstrated the efficacy of the method even in pre-irradiated gynecological malignancies, with low rates of perioperative complications and increased rates of complete healing of the perineal defects [7].
Conclusions
Gracilis myocutaneous flap appears to be an effective and feasible method for perineal reconstruction after extended perineal resection for gynecological malignancies, including vulvar cancer. Once the myocutaneous flap is dissected, it is tunneled subcutaneously or even under the adductor muscles in order to reach the perineal defect and provide an efficient coverage of the perineal wound.
This method seems to be effective even in pre- irradiated patients with larger perineal wounds resulting after total pelvic exenteration for locally advanced gynecological malignancies.
Institutional Review Board Statement
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Acknowledgments
This work was supported by the project entitled “Multidisciplinary Consortium for Supporting the Research Skills in Diagnosing, Treating and Identifying Predictive Factors of Malignant Gynecologic Disorders”, project number PN-III-P1-1.2-PCCDI2017-0833.
Conflicts of Interest
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
References
- Weikel, W.; Hofmann, M.; Steiner, E.; Knapstein, P.G.; Koelbl, H. Reconstructive surgery following resection of primary vulvar cancers. Gynecol Oncol. 2005, 99, 92–100. [Google Scholar] [CrossRef]
- Wheeless, C.R., Jr. Recent advances in surgical reconstruction of the gynecologic cancer patient. Curr Opin Obstet Gynecol. 1992, 4, 91–101. [Google Scholar]
- Burke, T.W. Changing surgical approaches to vulvar cancer. Curr Opin Obstet Gynecol. 1992, 4, 86–90. [Google Scholar] [PubMed]
- Reid, R. Local and distant skin flaps in the reconstruction of vulvar deformities. Am J Obstet Gynecol. 1997, 177, 1372–1383. [Google Scholar] [PubMed]
- Whetzel, T.P.; Lechtman, A.N. The gracilis myofasciocutaneous flap: Vascular anatomy and clinical application. Plast Reconstr Surg. 1997, 99, 1642–1652. [Google Scholar] [CrossRef]
- Friedman, J.; Dinh, T.; Potochny, J. Reconstruction of the perineum. Semin Surg Oncol. 2000, 19, 282–293. [Google Scholar] [CrossRef] [PubMed]
- Vermaas, M.; Ferenschild, F.T.; Hofer, S.O.; Verhoef, C.; Eggermont, A.M.; de Wilt, J.H. Primary and secondary reconstruction after surgery of the irradiated pelvis using a gracilis muscle flap transposition. Eur J Surg Oncol. 2005, 31, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.J.; Chang, N.J.; Chou, H.H.; Wu, C.W.; Abdelrahman, M.; Chen, H.Y.; Cheng, M.H. Pedicle perforator flaps for vulvar reconstruction--new generation of less invasive vulvar reconstruction with favorable results. Gynecol Oncol. 2015, 137, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Deutinger, M.; Kuzbari, R.; Paternostro-Sluga, T.; Quittan, M.; Zauner-Dungl, A.; Worseg, A.; Todoroff, B.; Holle, J. Donor-site morbidity of the gracilis flap. Plast Reconstr Surg. 1995, 95, 1240–1244. [Google Scholar] [CrossRef] [PubMed]
- McCraw, J.B.; Massey, F.M.; Shanklin, K.D.; Horton, C.E. Vaginal reconstruction with gracilis myocutaneous flaps. Plast Reconstr Surg. 1976, 58, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Ouar, N.; Mazouz-Dorval, S.; Revol, M.; Sorin, T. Perineal reconstruction: The use of a gracilis muscle flap for urethral fistula coverage, our point of view. Ann Chir Plast Esthet. 2017, 62, 163–166. [Google Scholar] [CrossRef] [PubMed]
- Borel, R.I.; Wiggers, T. Gracilis muscle flap in the treatment of persistent, infected pelvic necrosis. Eur J Surg. 1999, 165, 390–391. [Google Scholar] [CrossRef]
- Goldie, S.J.; Almasharqah, R.; Fogg, Q.A.; Anderson, W. Extending the use of the gracilis muscle flap in perineal reconstruction surgery. J Plast Reconstr Aesthet Surg. 2016, 69, 1097–1101. [Google Scholar] [CrossRef] [PubMed]
- Peled, I.J. Reconstruction of the vulva with V-Y advanced myocutaneous gracilis flap. Plast Reconstr Surg. 1990, 86, 1014–1016. [Google Scholar] [PubMed]
- Kaartinen, I.S.; Vuento, M.H.; Hyoty, M.K.; Kallio, J.; Kuokkanen, H.O. Reconstruction of the pelvic floor and the vagina after total pelvic exenteration using the transverse musculocutaneous gracilis flap. J Plast Reconstr Aesthet Surg. 2015, 68, 93–97. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the author. 2019 Nicolae Bacalbasa, Irina Balescu, Andreea Meruta, Alina Tanase, Adriana Ghelmene, Mihaela Vilcu, Iulian Brezean