Highlights
- Patients with type 2 diabetes mellitus have significantly higher scores in abandonment, failure, vulnerability, enmeshment, self-sacrifice, entitlement and insufficient self control schemas.
- Patients with type 2 diabetes mellitus have significantly higher scores in over-vigilance and inhibition schematic domains.
Highlights
- Patients with type 2 diabetes mellitus have significantly higher scores in abandonment, failure, vulnerability, enmeshment, self-sacrifice, entitlement and insufficient self control schemas.
- Patients with type 2 diabetes mellitus have significantly higher scores in over-vigilance and inhibition schematic domains.
Abstract
Objective. This study explored Early Maladjustment Schemas (EMSs) among individuals with and without type 2 diabetes mellitus and examined potential moderating roles for gender, level of education, and occupation. Methods. The sample included 371 adult participants (120 patients with diabetes and 251 individuals without diabetes), from Shiraz City, Fars province; Iran. The Young Schema Questionnaire-Short Form (YSQ-SF) was used to assess early maladjustment schemas. Results. Findings showed that patients with type 2 diabetes had significantly higher scores than controls on a number of EMSs, including abandonment, failure, vulnerability, enmeshment, self-sacrifice, entitlement, and insufficient self-control schemas as well as the over-vigilance and inhibition schematic domains. However, results did not support roles for gender, the level of education, and occupation on any of EMSs and schematic domains. Conclusions. Medical and health professionals may find these results helpful for assessment, treatment, and prevention goals in patients with type 2 diabetes.
Introduction
Diabetes mellitus is a major health problem, particularly in the Middle East [1]. The prevalence of diabetes has increased rapidly in Iran since the first national comprehensive survey in 1999 to the present [2]. For example, trend analyses show a 35% increase in the prevalence rate of diabetes among Iranian adults from 2005 to 2011 [3]. Moreover among all cases of diabetes, the proportion of type 2 diabetes mellitus (T2DM) was 85.5% in the country in 2015–2016 [4]. Studies have demonstrated a higher prevalence in females (12.86%) than males (9.90%). From a psychopathological perspective, research has shown that psychological distress, agitation, and mental preoccupation with disease are common in patients with diabetes mellitus [5]. Thus, diabetes-related distress is an indicator of health-related quality of life in patients with this disease, as it relates to how patients may handle their negative emotions toward the diagnosis and complications of diabetes, how to achieve good self-management, and how to access appropriate social support for an effective outcome [6,7].
Chronic distress can predispose diabetic patients for the development of various psychopathologcial and psychological disorders, with many studies demonstrating that anxiety disorders and depression are the most frequent psychiatric comorbid conditions in patients with type 2 diabetes [8,9,10,11]. In addition, investigations have affirmed that cognitive dysfunction as a form of psychopathology is frequent among patients with type 2 diabetes, and this dysfunction can influence self-care and general quality of life [12,13,14]. Munshi (2017) showed that cognitive dysfunctions in patients with type 2 diabetes can vary on a spectrum from a mild impairment (i.e., cognitive dysfunction without difficulty performing daily activities) to severe dysfunction (i.e., dementia).
In general, “schema” is an indicator of both functional and dysfunctional cognitive functioning. Schemas are considered the basis for perception, classification, viewing, differentiating, and encoding of different stimuli encountered by individuals during the course of their lifetime [15]. In the fields of cognitive psychology, cognitive development, self-psychology, and attachment theory, the concept of schema is used to understand and explain the developmental nature of psychopathology among patients with mental disorders or physical diseases [16]. Segal (1988) suggested that each schema shows some ingredients of past reactions and experiences, which shape a fairly cohesive entity of knowledge and directs the consecutive perception and appraisals in everyday life [17]. Young (1990) refers to schema as "templates for the processing of later experience". The development of early maladaptive schemas (EMSs) may lead to dysfunctional and self-preserving mechanisms throughout one’s life-time, which in turn lead an individual to perform and behave in maladaptive ways involving distorting reality, stress and pessimism.
Research has further demonstrated that dysfunctional cognitive schemas have influential roles on the development of psychosomatic disorders [18,19]. For instance, Dattilio (2010) conceptualized that generalized/ superordinate level of cognitive schemas are resistant to change and that they have a powerful influence over thoughts, affects, behaviors, and even physical and physiologic processes in patients with physical diseases. Since both the immune system and central nervous system have the capacity to learn and form memory, Dattilio (2010) suggested that a form of storage for cognitive schema is located not only in the brain but also in cells that are distributed throughout the entire body [15]. According to the mind theory as the function of brain-cell connection [15], it appears that cognitive schemas can influence the whole-body performance in patients with psychosomatic and chronic diseases. In line with the aforesaid conceptualizations, several studies have highlighted dysfunctional schema in patient with physical diseases. Ameri and colleagues (2014) indicated a significant difference between the mean scores of normal individuals and asthmatic patients on all major domains of EMSs, excepting other-directedness [20]. Gojani and colleagues (2017) showed that schema-based therapy can reduce defeated schema, dependence vs. incompetence schema, devotion schema, merit schema, stubbornly criteria schema, and restraint/inadequate self-discipline schema in patients with psoriasis [21].
However, there is still a lack of evidence about maladaptive schemas in patients with type 2 diabetes. Therefore, this study examined the Early Maladjustment Schemas (EMSs) among individuals with and without type 2 diabetes mellitus and investigated potential roles for gender, the level of education, and occupation variables.
The study design
Based on an integrative approach for behavioral and psychosocial interventions in diabetes [22], motivators, inhibitors/facilitators, intentions, and triggers are considered as four factors which influences the outcome of therapeutic interventions in patients. Motivators consist of needs and outcome expectances, and predispose patients to action and adherence to the treatment process. Inhibitors/facilitators represent either barriers or resources for accomplishment of the treatment process. Intentions are the external or inner cause for behavior change toward the therapy goals. Triggers are the factors that change a personal readiness into an action state [22]. The present study assumes that these four factors function in the maladaptive schemas in disease-stress conceptualizations and are important to an integrative approach for biopsychological interventions in diabetes [5,6,7,15,16,17,18,19,22]. This study further suggests that patients with diabetes commonly have a multifaceted set of repetitive thoughts and feelings about disease; worries about access to care; concerns about nutrition and diet, physical action, drugs and medications; psychological insulin confrontation; and not receiving adequate support from family members and others. Thus, the psychological distress response to diabetes may become a significant contributor to undesirable disease course, prognosis, and outcome, due to its relationship to both reduced metabolic control and impairment of the quality of life. Therefore, a careful assessment of cognitive schematic dysfunctions in patients with type 2 diabetes is essential for addressing psychological distress, and may assist in increasing treatment efficacy [23]. Finally, this study suggests that negative experiences and psychological distress due to type 2 diabetes as a chronic disease can provoke some EMSs, which could influence treatment management in these patients. The present study hypothesizes that individuals with and without type 2 diabetes will differ in EMSs, with possible moderating effects from gender, the level of education, and job variables.
Materials and Methods
Participants
The study sample consisted of 371 adult participants (females with diabetes =96, males with diabetes =24, females without diabetes=103, and males without diabetes=148), from Shiraz City, Fars province, Iran. Mean ages and standard deviation for individuals with and without diabetes were 51.4 (SD=6.05) and 48.4 (SD=5.14) respectively. The level of education ranged from less than diploma (N=100), to diploma (N=140), skill degree (N=43), bachelor degree (N=73), and master or doctorate (N=15). All participants were Muslim. Participants were enlisted using a non-random purposeful sampling strategy among over 30 year-old adults from outpatient clinics in Shiraz City. Inclusion criteria for patients with type 2 diabetes were: 1- over 30 years-old, 2- on diabetes care for more than six months, 3- meeting all clinical criteria for type 2 diabetes, 4- free of clinical psychological or psychiatric co-morbidities that might influence cognitive function, and 5- proficiency in the Persian language. Inclusion criteria for individuals in the control group were: 1- over 30 years-old, 2- free of serious health complications during the past year, 3-having no history of diabetes among his/her close relatives, 4- having no PPG, 5- free of cardiovascular disease, hypertension, or other chronic diseases, 6- having a BMI lower than 25, 7- being a non-smoker and free of drug abuse, 8- having no clinical psychological or psychiatric co-morbidities that might affect cognitive function, and 9- proficiency in the Persian language. Each participant was addressed individually and completed the study’s informed approval prior to contribution.
Materials
The Young Schema Questionnaire-Short Form (YSQ-SF; Young, 1998) was used to assess EMSs. The YSQ–SF is a 75-item self-rating questionnaire which measures the early maladjustment schemas. In this survey, participants respond to items on a Likert-type scale from 1 (completely untrue of me) to 6 (describes me perfectly). The YSQ–SF contains 15 subscales: Emotional Deprivation (e.g., In general, people have not been there to give me warmth, holding, and affection), Abandonment (e.g., I worry that people I feel close to will leave me or abandon me), Mistrust/Abuse (e.g., I feel that people will take advantage of me), Social Isolation (e.g., I don't belong; I'm a loner), Defectiveness (e.g.,. I feel that I'm not lovable), Failure (e.g., I'm not as talented as most people are at their work), Vulnerability (e.g., I worry about being attacked), Dependence (e.g., I lack common sense), Subjugation (e.g., In relationships, I let the other person have the upper hand), Enmeshment (e.g., I often feel that I do not have a separate identity from my parent(s) or partner), Emotional Inhibition (e.g., I find it hard to be warm and spontaneous), Self-Sacrifice (e.g., I am a good person because I think of others more than of myself), Entitlement (e.g., I hate to be constrained or kept from doing what I want), Unrelenting Standards (e.g., I must meet all my responsibilities), and Insufficient Self Control (e.g., I have rarely been able to stick to my resolutions) [24].
These 15 subscales fall into five domains including: (a) Disconnection and Rejection, (b) Impaired Autonomy and Performance, (c) Impaired Limits, (d) Other-Directedness, and (e) Entitlement and Insufficient Self-Control. The first domain represents lack of sufficient love and attention, supervision, and direction for the individual by his/her family during childhood. This domain assesses deterioration of the individual’s self-confidence and self-esteem by his/her parents in childhood. The second domain represents leniency, including a lack of regulations and boundaries in childhood. The third domain represents pathological or non-ordinary tendencies between children and families in childhood. The fourth domain is an indication of low power and poor self-control schemas. The fifth domain represents the role of non-sympathetic and insensitive parents who naturally valued self-control and self-denial in their children [18].
The validity and reliability of the YSQ-SF have been affirmed in clinical and non-clinical studies [24,25,26]. Research with the Persian language version of the YSQ-SF has demonstrated its validity and reliability in Iran [27]. Reliability analysis of the YSQ-SF using Cronbach’s alpha indicates internal consistency of the domains, Disconnection and Rejection (DR), Impaired Autonomy and Performance (IAP), Impaired Limits (IL), Other-Directedness (OD), and Over-Vigilance and Inhibition (OVI) domains, found to be .90, .88, .92, .90, .94 and .90 respectively.
Results
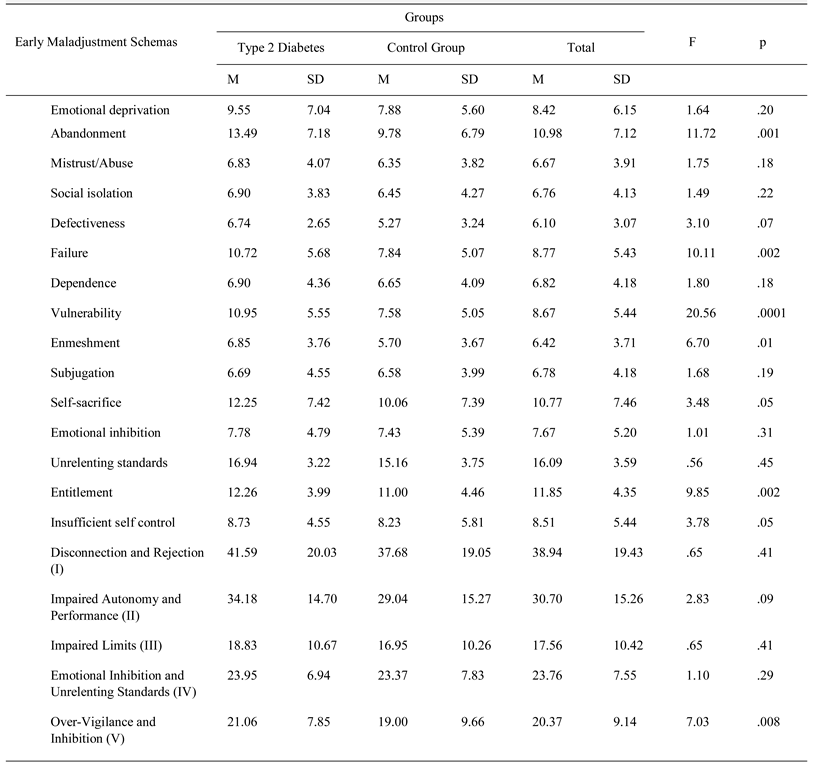
To evaluate differences in EMSs across diabetic and non-diabetic groups, a multivariate analysis of covariance (MANCOVA) was performed, with group status, gender, the level of education, and job type entered as fixed independent variables and maladjustment schemas (i.e. 15 schemas and 5 schematic domains) as dependent variables. This analysis showed differences based on group status, Wilks’k = .712; F(15, 352) = 9.47; p <.0001) regarding abandonment, failure, vulnerability, enmeshment, self-sacrifice, entitlement and insufficient self control schemas; and over-vigilance and inhibition schematic domains. Tests of between-subjects effects using LSD posthoc analysis showed that patients with type 2 diabetes had significantly higher scores in the aforementioned 7 maladjustment schemas as well as the over-vigilance and inhibition schematic domains than non-diabetic controls (Table 1). However, this analysis did not support moderating roles for gender, Wilks’k = .975; F(15, 352) = .601; p <.87; the level of education, Wilks’k = .968; F(15, 352) = .986; p <.889; and occupation, Wilks’k = .964; F(15, 352) = .887; p <.57.

Table 1.
Early Maladjustment Schemas in Individuals with and without Type 2 Diabetes Mellitus
Discussions
Significant group differences for a number of EMSs were found, specifically regarding abandonment, failure, vulnerability, enmeshment, self-sacrifice, entitlement, insufficient self control schemas, and over-vigilance and inhibition schematic domain were found in this sample. But no differences between clinical and control groups were found on the other subscales: emotional deprivation, mistrust/abuse, social isolation, defectiveness, dependence, subjugation, emotional inhibition, unrelenting standards, disconnection and rejection, impaired autonomy and performance, impaired limits, emotional inhibition and unrelenting standards schematic domains in this sample. In general, these results are consistent with predictions of a number of developmental psychopathology [15,16,17,18,19,28,29,30,31], as well as with the assumptions of the disease-stress model and the integrative approach for behavioral and psychosocial interventions in diabetes [5,6,7,15,16,17,18,19,22] which suggest schema differences associated with mental or physical disease states.
These results are also consistent with previous research which has supported the roles of maladaptive schemas, cognitive dysfunctions, and a role for schema therapy regarding the occurrence of or treatment for chronic diseases. For example, Gojani and colleagues reported that schema-based therapy can significantly reduce EMSs in patients with psoriasis [21]. Farrell and colleagues showed a positive relationship between cognitive distortions and perception of stress in children and adolescents who were diagnosed with Type I diabetes [32]. Smith and colleagues demonstrated a positive correlation between cognitive dysfunctions and disability scores in patient with chronic low back pain and further that pain-related and general cognitive dysfunctions significantly correlated with depressed mood in patients with rheumatoid arthritis [33,34,35]. Bums and colleagues recognized the influence of cognitive dysfunctions on the treatment of chronic pain [34]. Finally, Santos Ribas and colleagues reported a significant positive association between migraines and hypervigilance and inhibition, unrelenting standards, and self-punishment maladaptive schemas [36]. In line with previous research supporting roles for psychological distress, cognitive dysfunction, and maladaptive schemas on development and treatment of diabetes and other psychosomatic diseases [6,7,8,9,10,11,12,14,20,21,22,23], the present findings verify the influence of some EMS’s in patients with type 2 diabetes. The study further suggests that a similar predisposition to engage in maladaptive cognitive schemas may influence health-related behaviors in patients with type 2 diabetes. Therefore, these findings highlight how psychological vulnerability and poor self-management of negative emotions are associated with EMSs which may predispose an individual for the progression or maintenance of type 2 diabetes in his/her later life. Thus, EMSs may play an important role in the establishment and maintenance of psychological distress in patients with Type II diabetes. The underlying mechanism of EMSs is assumed to occur at an autonomous level, developed as a result of mental processing of childhood experiences, with individuals later engaging in distorted thought processes testing while attempting to establish a coherent image of the chronic health threat. Patients' mental representations of disease are therefore based on distinct maladaptive schemas which in turn may affect the way they cope with the disease, as seen in the over-vigilance and inhibition schematic domains of patients with type 2 diabetes.
Conclusions
This study builds upon current thinking within medical psychology by demonstrating higher levels of some EMSs in patients with type 2 diabetes mellitus; at the same time, no differences occurred due to gender, the level of education, or occupation of the patients. Medical and health professionals may utilize these findings to assist in developing an integrated biopsychosocial approach for the assessment, treatment, and prevention goals in patients with type 2 diabetes. Likewise, these results may be valuable for instructional and educational purposes by recognizing possible roles of maladjustment schemas in the rehabilitation of patients with diabetes.
The study is limited by the use of a single self-rating inventory in individuals with and without type 2 diabetes. Future investigation may benefit from both quantitative and qualitative procedures to explore how early psychological experiences and dysfunctional emotions-regulation may influence the nature and severity of EMSs in patients with type 2 diabetes.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
References
- Guariguata, L.; Whiting, D.R.; Hambleton, I.; Beagley, J.; Linnenkamp, U.; Shaw, J.E. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014, 103, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Noshad, S.; Afarideh, M.; Heidari, B.; Mechanick, J.I.; Esteghamati, A. Diabetes care in Iran: where We stand and where We Are headed. Ann Global Health. 2015, 81, 839–850. [Google Scholar] [CrossRef] [PubMed]
- Esteghamati, A.; Etemad, K.; Koohpayehzadeh, J.; Abbasi, M.; Meysamie, A.; Noshad, S.; Asgari, F.; Mousavizadeh, M.; Rafei, A.; Khajeh, E.; Neishaboury, M.; Sheikhbahaei, S.; Nakhjavani, M. Trends in the prevalence of diabetes and impaired fasting glucose in association with obesity in Iran: 2005–2011. Diabetes Res Clin Pract. 2014, 103, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Esteghamati, A.; Larijani, B.; Aghajani, M.H.; Ghaemi, F.; Kermanchi, J.; Shahrami, A.; Saadat, M.; Esfahani, E.N.; Ganji, M.; Noshad, S.; Khajeh, E.; Ghajar, A.; Heidari, B.; Afarideh, M.; Mechanick, J.; Ismail-Beigi, F. Diabetes in Iran: Prospective Analysis from First Nationwide Diabetes Report of National Program for Prevention and Control of Diabetes (NPPCD-2016). Sci Rep. 2017, 7, 13461. [Google Scholar] [CrossRef] [PubMed]
- Trovato, G.; Catalano, D.; Martines, G.; Spadaro, D.; Di Corrado, D.; Crispi, V.; Garufi, G.; Di Nuovo, S. Psychological stress measure in type 2 diabetes. Eur Rev Med Pharmacol Sci. 2006, 10, 69–74. [Google Scholar] [PubMed]
- Peyrot, M.; Rubin, R.; Lauritzen, T.; Snoek, F.; Matthews, D.; Skovlund, S. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005, 22, 1379–1385. [Google Scholar] [CrossRef] [PubMed]
- Skovlund, S.E.; Peyrot, M. The Diabetes Attitudes, Wishes, and Needs (DAWN) program: a new approach to improving outcomes of diabetes care. Diabetes Spectrum. 2005, 18, 136–142. [Google Scholar] [CrossRef]
- Almawi, W.; Tamim, H.; Al-Sayed, N.; Arekat, M.; Al-Khateeb, G.; Baqer, A.; Tutanji, H.; Kamel, C. Association of comorbid depression, anxiety, and stress disorders with Type 2 diabetes in Bahrain, a country with a very high prevalence of Type 2 diabetes. J Endocrinol Invest. 2008, 31, 1020–1024. [Google Scholar] [CrossRef] [PubMed]
- Das-Munshi, J.; Stewart, R.; Ismail, K.; Bebbington, P.E.; Jenkins, R.; Prince, M.J. Diabetes, common mental disorders, and disability: findings from the UK National Psychiatric Morbidity Survey. Psychosom Med. 2007, 69, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Barker, L.; Ford, E.; Zhang, X.; Strine, T.; Mokdad, A. Diabetes and anxiety in US adults: findings from the 2006 Behavioral Risk Factor Surveillance System. Diabet Med. 2008, 25, 878–881. [Google Scholar] [CrossRef] [PubMed]
- Perveen, S.; Otho, M.S.; Siddiqi, M.N.; Hatcher, J.; Rafique, G. Association of depression with newly diagnosed type 2 diabetes among adults aged between 25 to 60 years in Karachi, Pakistan. Diabetol Metab Syndr. 2010, 2, 17. [Google Scholar] [CrossRef] [PubMed]
- Chew, B.-H.; Shariff-Ghazali, S.; Fernandez, A. Psychological aspects of diabetes care: Effecting behavioral change in patients. World J Diabetes. 2014, 5, 796–808. [Google Scholar] [CrossRef] [PubMed]
- Koekkoek, P.S.; Kappelle, L.J.; van den Berg, E.; Rutten, G.E.; Biessels, G.J. Cognitive function in patients with diabetes mellitus: guidance for daily care. Lancet Neurol. 2015, 14, 329–340. [Google Scholar] [CrossRef] [PubMed]
- Munshi, M.N. Cognitive dysfunction in older adults with diabetes: what a clinician needs to know. Diabetes Care. 2017, 40, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Dattilio, F.M. Examining the Scope and Concept of Schema: Should We Look Beyond Cognitive Structures? Psihologijske Teme. 2010, 19, 221–234. [Google Scholar]
- Beck, A.T.; Rush, A.J.; Shaw, B.F.; Emery, G. Cognitive Therapy of Depression; Guilford Press: New York, NY, USA, 1987; ISBN 9780898629194. [Google Scholar]
- Segal, Z.V. Appraisal of the self-schema construct in cognitive models of depression. Psychol Bull. 1988, 103, 147–162. [Google Scholar] [CrossRef] [PubMed]
- Young, J.E.; Klosko, J.S.; Weishaar, M.E. Schema Therapy: A Practitioner's Guide; Guilford Press: New York, NY, USA, 2006; ISBN 9781593853723. [Google Scholar]
- Young, J.E. Cognitive Therapy for Personality Disorders: A Schema-Focused Approach; Professional Resource Press: Sarasota, FL, USA, 1999. [Google Scholar]
- Ameri, F.; Bayat, B.; Khosravi, Z. Comparison of early maladaptive schemas and defense styles in asthmatic, alexithymic and normal subjects. Journal of Practice in Clinical Psychology. 2014, 2, 51–57. [Google Scholar]
- Gojani, P.J.; Masjedi, M.; Khaleghipour, S.; Behzadi, E. Effects of the Schema Therapy and Mindfulness on the Maladaptive Schemas Hold by the Psoriasis Patients with the Psychopathology Symptoms. Adv Biomed Res. 2017, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Peyrot, M.; Rubin, R.R. Behavioral and psychosocial interventions in diabetes: a conceptual review. Diabetes Care. 2007, 30, 2433–2440. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, J.S.; Esbitt, S.A.; Schneider, H.E.; Osborne, P.J.; Kupperman, E.G. Psychological issues in adults with type 2 diabetes. Psychological Co-Morbidities of physical illness: Springer; 2011. p. 73-121. e-ISBN: 978-1-4419-0029-6. [CrossRef]
- Young, J.E.; Brown, G. Young Schema Questionnaire– Short form (YSQ-S)(On-Line); Cognitive Therapy Centre: New York, NY, USA, 1998. [Google Scholar]
- Trip, S. The Romanian version of Young Schema Questionnaire- Short Form 3. (YSQ-S3). Journal of Cognitive and Behavior Psychotherapies. 2006, 6, 173–181. [Google Scholar]
- Welburn, K.; Coristine, M.; Dagg, P.; Pontefract, A.; Jordan, S. The Schema Questionnaire—Short Form: Factor analysis and relationship between schemas and symptoms. Cognitive Therapy and Research. 2002, 26, 519–530. [Google Scholar] [CrossRef]
- Sadooghi, Z.; Aguilar-Vafaie, M.; Rasoulzadeh-Tabatabaie, S.; Esfehanian, K. Factor Analysis of the Young Schema Questionnaire-Short Form in a Nonclinical Iranian Sample. Iranian journal of psychaitry and clinical psychology. 2008, 14, 214–219. [Google Scholar]
- Bowlby, J. The making and breaking of affectional bonds. I. Aetiology and psychopathology in the light of attachment theory. An expanded version of the Fiftieth Maudsley Lecture, delivered before the Royal College of Psychiatrists, 19 November 1976. Br J Psychiatry. 1977, 130, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Timmerman, I.G.; Emmelkamp, P.M. The relationship between attachment styles and Cluster B personality disorders in prisoners and forensic inpatients. Int J Law Psychiatry. 2006, 29, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Windle, M. A multilevel developmental contextual approach to substance use and addiction. BioSocieties. 2010, 5, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Zubin, J.; Spring, B. Vulnerability: a new view of schizophrenia. Journal of Abnormal Psychology. 1977, 86, 103–126. [Google Scholar] [CrossRef]
- Farrell, S.P.; Haines, A.A.; Davies, W.H.; Smith, P.; Parton, E. The impact of cognitive distortions, stress, and adherence on metabolic control in youths with type 1 diabetes. Journal of Adolescent Health. 2004, 34, 461–467. [Google Scholar] [CrossRef]
- Smith, T.W.; Follick, M.J.; Ahern, D.K.; Adams, A. Cognitive distortion and disability in chronic low back pain. Cognitive Therapy and Research. 1986, 10, 201–210. [Google Scholar] [CrossRef]
- Bums, J.W.; Kubilus, A.; Bruehl, S.; Harden, R.N.; Lofland, K. Do changes in cognitive factors influence outcome following multidisciplinary treatment for chronic pain? A cross-lagged panel analysis. Journal of Counseling and Clinical Psychology. 2003, 7, 81–91. [Google Scholar]
- Smith, T.W.; Christensen, A.J.; Peck, J.R.; Ward, J.R. Cognitive distortion, helplessness, and depressed mood in rheumatoid arthritis: A four-year longitudinal analysis. Health Psychology. 1994, 13, 213–217. [Google Scholar] [CrossRef]
- Santos Ribas, K.H.; Ribas, V.R.; Mendes Barros, S.S.; Ribas, V.R.; Nogueira Filizola, M.C.; Guerra Ribas, R.M.; Silva, P.C.; Cardoso Kucera, C.A.; Lima Martins, H.A. The participation of Early Maladaptive Schemas (EMSs) in the perception of pain in patients with migraine. A psychological profile. Dement Neuropsychology. 2018, 12, 68–74. [Google Scholar] [CrossRef]
© 2019 by the author. 2019 Fazlolah Mirdrikvand, Mohammad Ali Sepahvandi, Siamak Khodarahimi, Simin Gholamrezaei, Mojtaba Rahmian Bougar, Pejman Shafikhani