Vulnerability and Physical Well-Being of Caregivers: What Relationship?
Highlights
- The experience of contact with pathologies can produce different existential outcomes in caregivers, manifested through different phenomenologies. The research proposes an analysis of the relationships existing among the different components involved.
- The knowledge about links among dimensions such as fatigue and burnout with mood, the conflict of role, the burdens and the emotional state, could be useful for the necessary interventions aimed to reduce possible suffering of caregivers.
- The fatigue and the burnout, would represent one of the possibilities due to the continuos contact with different pathologies, but not the only one.
Abstract
:- The experience of contact with pathologies can produce different existential outcomes in caregivers, manifested through different phenomenologies. The research proposes an analysis of the relationships existing among the different components involved.
- The knowledge about links among dimensions such as fatigue and burnout with mood, the conflict of role, the burdens and the emotional state, could be useful for the necessary interventions aimed to reduce possible suffering of caregivers.
- The fatigue and the burnout, would represent one of the possibilities due to the continuos contact with different pathologies, but not the only one.
Introduction
Materials and Methods
Participants
Research Method
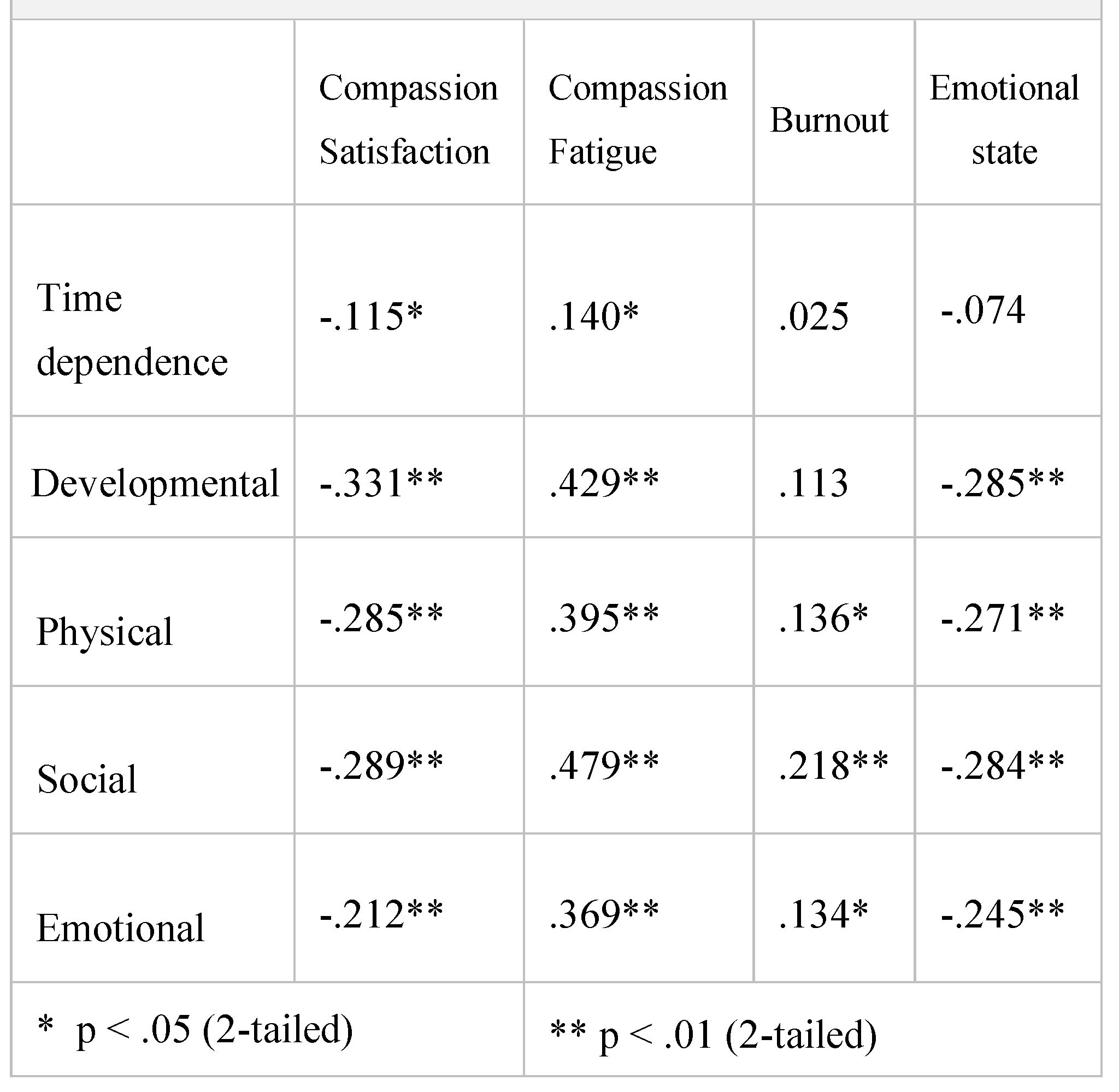
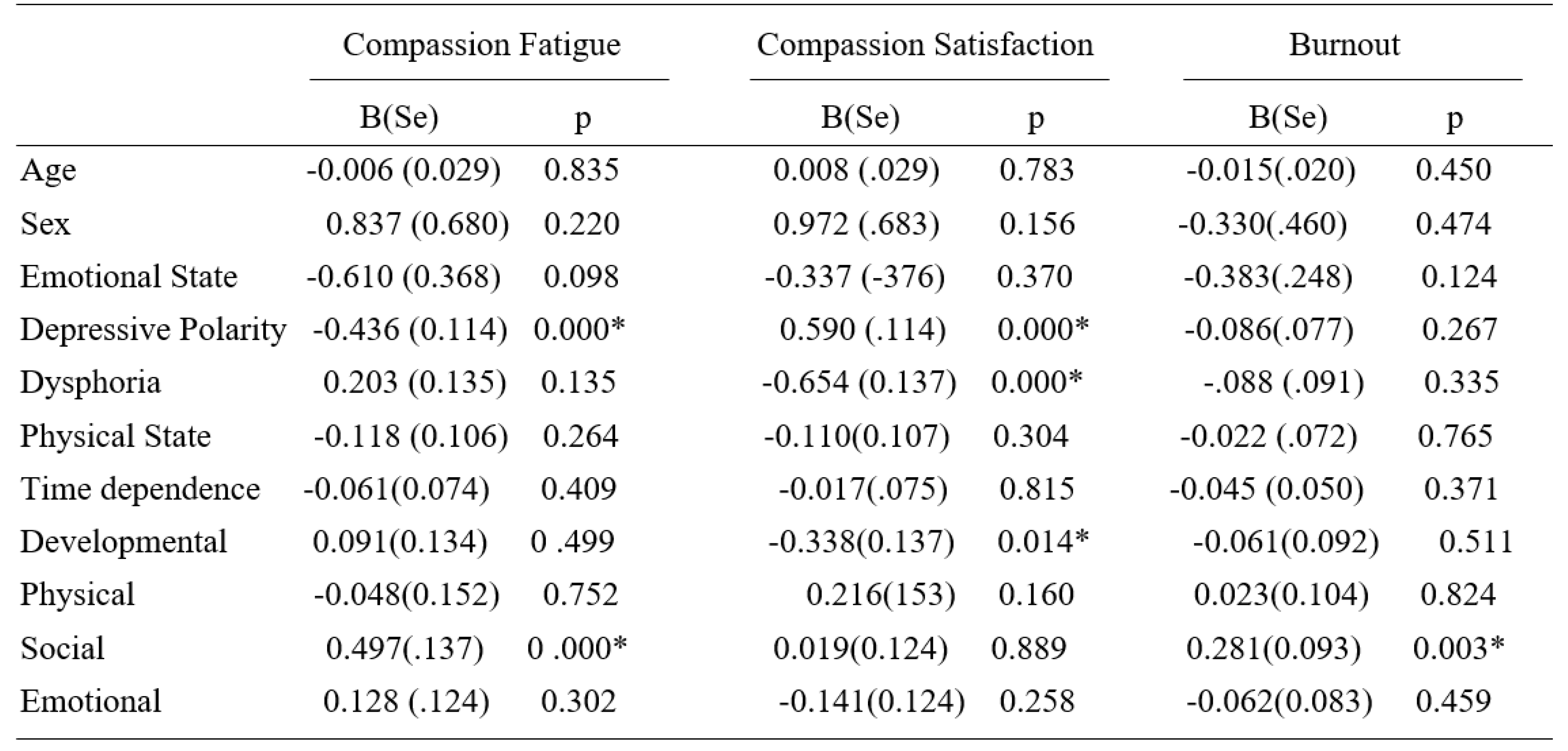
- The Italian version of the Caregiver Burden Inventory CBI [2], a 24-items multi-dimensional questionnaire that measures the caregiver’s burdens along 5 dimensions: Time Dependence, Developmental, Physical, Social, Emotional, with each evaluated using a 5-point Likert scale from 0 (not at all disruptive) to 4 (very disruptive);
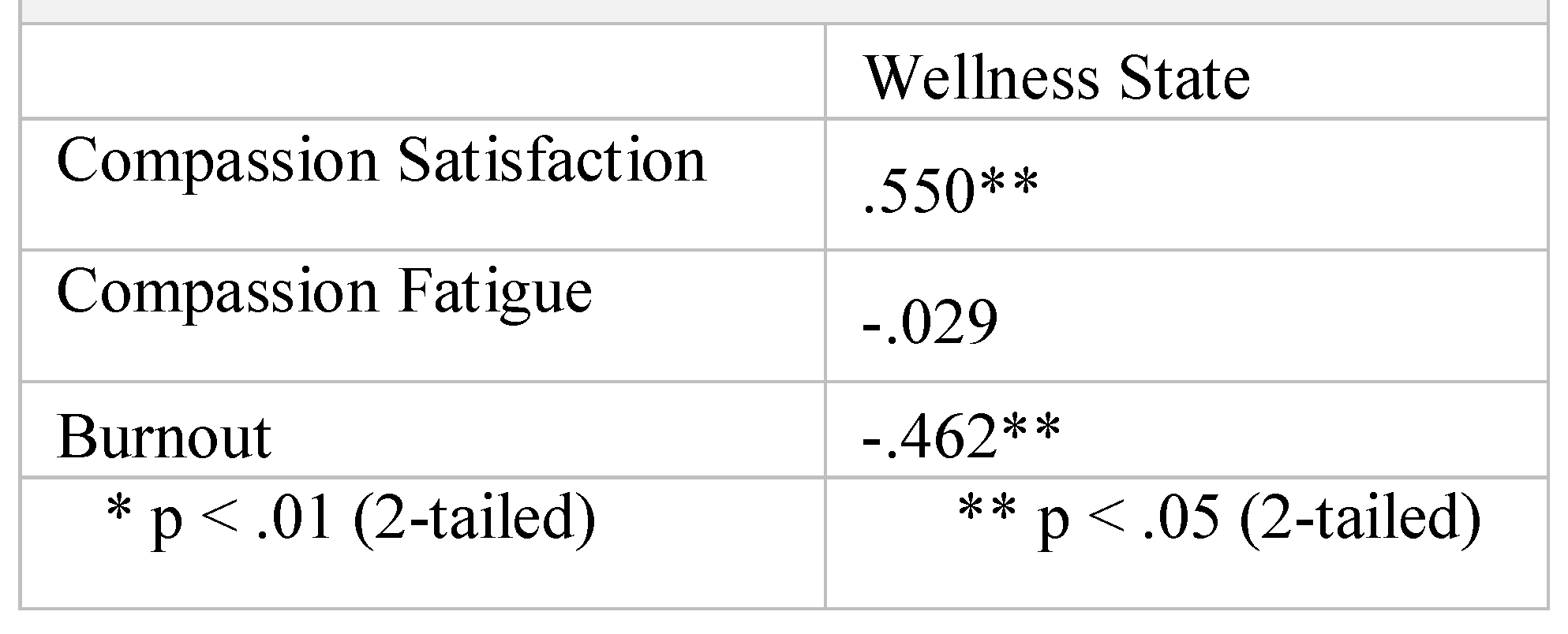
- WHO (Five) Well-Being Index (WHO-5, 1998), composed of 5 items assessing well-being, evaluated using a 6-point Likert scale from 5 (always) to 0 (never).
Statistical Analysis
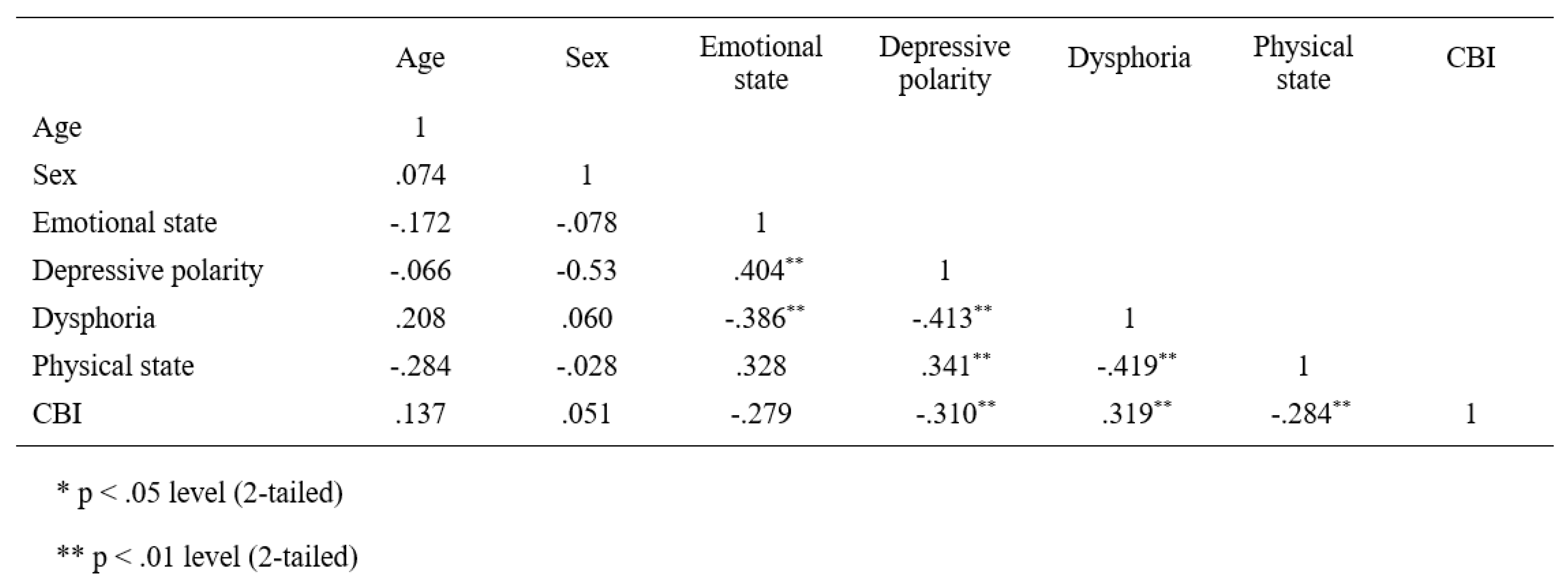
Results
Discussions
Conclusions
Compliance with Ethical Standards
Conflicts of Interest
References
- Schulz, R.; Beach, S.R. Caregiving as a risk factor for mortality. JAMA: The journal of the American Medical Association. 1999, 282, 22152219. [Google Scholar] [CrossRef] [PubMed]
- Novak, M.; Guest, C. Application of a multidimensional caregiver burden inventory. The gerontologist. 1989, 29, 798–803. [Google Scholar] [CrossRef]
- Settineri, S.; Rizzo, A.; Liotta, M.; Mento, C. Caregiver’s burden and quality of life: Caring for physical and mental illness. International Journal of Psychological Research. 2014, 7, 30–39. [Google Scholar] [CrossRef]
- Provencher, H.L. Objective burden among primary caregivers of persons with chronic schizophrenia. Journal of psychiatric and mental health nursing. 1996, 3, 181–187. [Google Scholar] [CrossRef]
- Greenberg, J.S.; Greenley, J.R.; Brown, R. Do mental health services reduce distress in families of people with serious mental illness? Psychiatric Rehabilitation Journal. 1997, 21, 40–50. [Google Scholar] [CrossRef]
- Nikmanesh, Z.; Shahinfar, M. The Role of Caregiver Burden in Quality of Life and Perception of Patients with Chronic Kidney Failure on Hemodialysis. Annals of Military and Health Sciences Research 2016, 14, e11465. [Google Scholar] [CrossRef]
- Shdaifat, E.A.; Manaf, M.R.A. Quality of life of caregivers and patients undergoing haemodialysis at ministry of health, Jordan. Int J Appl. 2012, 2, 78–85. [Google Scholar]
- Grant, M.; Sun, V.; Fujinami, R.; Sidhu, R.; Otis-Green, S.; Juarez, G.; et al. Family caregiver burden, skills preparedness, and quality of life in non-small cell lung cancer. Oncol Nurs Forum. 2013, 40, 337–346. [Google Scholar] [CrossRef]
- Maslach, C. The Cost of Caring; Practice Hall Inc.: Hoboken, NJ, USA, 1982. [Google Scholar]
- Medland, J.; Howard-Ruben, J.; Whitaker, E. Fostering psychosocial wellness in oncology nurses: Addressing burnout and social support in the workplace. Oncology Nursing Forum. 2004, 31, 47–54. [Google Scholar] [CrossRef]
- Elwood, L.S.; Mott, J.; Lohr, J.M.; Galovski, T.E. Secondary trauma symptoms in clinicians: A critical review of the construct, specificity, and implications for trauma- focused treatment. Clinical psychology review. 2011, 31, 25–36. [Google Scholar] [CrossRef]
- Franza, F.; Del Buono, G.; Pellegrino, F. Psychiatriccaregiver stress: Clinicalimplications of compassionfatigue. Psychiatr Danub. 2015, 27 (Suppl. S1), S321–S327. [Google Scholar]
- Figley, C.R. Compassion fatigue: Toward a new understanding of the costs of caring. In Secondary Traumatic Stress: Self-Care Issues for Clinicians, Researchers, and Educators; Stamm, B.H., Ed.; Sidran Press: Lutherville, MD, USA, 1995. [Google Scholar]
- Figley, C.R. Compassion fatigue: Psychotherapists’ chronic lack of self-care. Journal of clinical psychology. 2002, 58, 1433–1441. [Google Scholar] [PubMed]
- Lynch, S.H. Looking at Compassion Fatigue Differently: Application to Family Caregivers. American Journal of Health Education. 2018, 49, 9–11. [Google Scholar]
- Coetzee, S.K.; Laschinger, H.K. Toward a comprehensive, theoretical model of compassion fatigue: An integrative literature review. Nurs Health Sci. 2018, 20, 4–15. [Google Scholar]
- Cocker, F.; Joss, N. Compassion fatigue among healthcare, emergency and community service workers: A systematic review. International journal of environmental research and public health. 2016, 13, 618. [Google Scholar]
- Nolte, A.G.; Downing, C.; Temane, A.; Hastings-Tolsma, M. Compassion fatigue in nurses: A metasynthesis. Journal of clinical nursing. 2017, 26, 4364–4378. [Google Scholar] [PubMed]
- Rossi, A.; Cetrano, G.; Pertile, R.; Rabbi, L.; Donisi, V.; Grigoletti, L.; et al. Burnout, compassion fatigue, and compassion satisfaction among staff in community- based mental health services. Psychiatry Research. 2012, 200, 933–938. [Google Scholar]
- Labra, C.; Millán-Calenti, J.C.; Buján, A.; Núñez-Naveira, L.; Jensen, A.M.; Peersen, M.C.; et al. Predictors of caregiving satisfaction in informal caregivers of people with dementia. Archives of gerontology and geriatrics. 2015, 60, 380–388. [Google Scholar]
- Lawton, M.P.; Kleban, M.H.; Moss, M.; Rovine, M.; Glicksman, A. Measuring caregiving appraisal. Journal of Gerontology. 1989, 44, P61–P71. [Google Scholar]
- Stamm, B.H. Measuring compassion satisfaction as well as fatigue: Developmental history of the Compassion Satisfaction and Fatigue Test. In Treating Compassion Fatigue; Figley, C.R., Ed.; Brunner-Routledge: New York, NY, USA, 2002; pp. 107–119. [Google Scholar]
- Ware, J.E. SF-36 Health Survey: Manual and Interpretation Guide; Health Institute: Tijuana, Mexico, 1993. [Google Scholar]
- Apolone, G.; Mosconi, P. The Italian SF-36 Health Survey: Translation, validation and norming. Journal of clinical epidemiology. 1998, 51, 1025–1036. [Google Scholar]
- Stamm, B.H. Theprofessional Quality of Life Scale: Compassion Satisfaction, Burnout, and Compassion Fatigue/Secondary Trauma Scales; Sidran Press: Latherville, MD, USA, 2005. [Google Scholar]
- Palestini, L.; Prati, G.; Pietrantoni, L.; Cicognani, E. La qualità della vita professionale nel lavoro di soccorso: Un contributo alla validazione italiana della Professional Quality of Life Scale (ProQOL). Psicoterapia Cognitiva e Comportamentale. 2009, 15, 205–227. [Google Scholar]
- Day, J.R.; Anderson, R.A. Compassion fatigue: An application of the concept to informal caregivers of family members with dementia. Nursing Research and Practice. 2011. [Google Scholar] [CrossRef]
- Sinclair, S.; Raffin-Bouchal, S.; Venturato, L.; Mijovic- Kondejewski, J.; Smith-MacDonald, L. Compassion fatigue: A meta-narrative review of the healthcare literature. International journal of nursing studies. 2017, 69, 9–24. [Google Scholar] [PubMed]
- Fernando, A.T.; Consedine, N.S. Beyond compassion fatigue: The transactional model of physician compassion. Journal of pain and symptom management. 2014, 48, 289–298. [Google Scholar] [PubMed]
- Ledoux, K. Understanding compassion fatigue: Understanding compassion. Journal of advanced nursing. 2015, 71, 2041–2050. [Google Scholar]
- Roeser, R.W., Colaianne. Compassion and human development: Current approaches and future directions. Research in Human Development. 2018, 15, 238–251. [Google Scholar]
- Seppala, E.M.; Simon-Thomas, E.; Brown, S.L.; Worline, M.C.; Cameron, C.D.; Doty, J.R. (Eds.) The Oxford Handbook of Compassion Science; Oxford University Press: New York, NY, USA, 2017. [Google Scholar]
- Lavelle, B.D. Compassion in context: Tracing the Buddhist roots of secular, compassion- based contemplative programs. In The Oxford Handbook of Compassion Science; Seppala, E.M., Thomas, E.S., Brown, S.L., Worline, M.C., Cameron, C.D., Doty, J.R., Eds.; Oxford University Press: New York, NY, USA, 2017; pp. 17–25. [Google Scholar]
- De Fazio, P.; Ciambrone, P.; Cerminara, G.; Barbuto, E.; Bruni, A.; Gentile, P.; et al. Depressive symptoms in caregivers of patients with dementia: Demographic variables and burden. Clinical Interventions in Aging. 2015, 10, 1085–1090. [Google Scholar]
- Kim, S.K.; Park, M.; Lee, Y.; Choi, S.H.; Moon, S.Y.; Seo, S.W.; et al. Influence of personality on depression, burden, and health-related quality of life in family caregivers of persons with dementia. International psychogeriatrics. 2017, 29, 227–237. [Google Scholar]
- Mathieu, F. The Compassion Fatigue Workbook; Routledge: New York, NY, USA, 2008. [Google Scholar]
- Huggard, P. Caring for the carers: Compassion fatigue and disenfranchised grief. Science with feeling: Animals and people. In Australia and Royal Society of New Zealand Anzccart Conference Proceedings; 2016; Volume 28. [Google Scholar]
- Ferrara, M.; Langiano, E.; Di Brango, T.; De Vito, E.; Di Cioccio, L.; Bauco, C. Prevalence of stress, anxiety and depression in with Alzheimer caregivers. Health and Quality of Life Outcomes. 2008, 6, 93. [Google Scholar] [CrossRef]
- Brodaty, H.; Donkin, M. Family caregivers of people with dementia. Dialogues in Clinical Neuroscience. 2009, 11, 217–228. [Google Scholar]
- Lown, BA. Mission Critical: Nursing Leadership Support for Compassion to Sustain Staff Well- being. Nursing administration quarterly. 2018, 42, 217–222. [Google Scholar]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry. 2016, 15, 103–111. [Google Scholar] [PubMed]
- Sollenberger, J. Looking inside ourselves: A culture of kindness. J Med Libr Assoc. 2018, 106, 283. [Google Scholar] [CrossRef]
- Andreychik, M.R. Feeling your joy helps me to bear feeling your pain: Examining associations between empathy for others’ positive versus negative emotions and burnout. Personality and Individual Differences. 2019, 137, 147–156. [Google Scholar]
- Lloyd, J.; Muers, J.; Patterson, T.G.; Marczak, M. Self- Compassion, Coping Strategies, and Caregiver Burden in Caregivers of People with Dementia. Clin Gerontol. 2019, 42, 47–59. [Google Scholar]
- Adelman, R.D.; Tmanova, L.L.; Delgado, D.; Dion, S.; Lachs, M.S. Caregiver burden: A clinical review. Jama. 2014, 311, 1052–1060. [Google Scholar] [PubMed]
- Silliman, R.A. Caring for the frail older patient: The doctor-patient-family caregiver relationship. Journal of General Internal Medicine. 1989, 4, 237–241. [Google Scholar]
- Shoenmakers, B.; Buntinx, F.; Delepeleire, J. What is the role of the general practitioner torwards the family caregiver of a community-dwelling demented relative? A systematic literature review. Scandinavian Journal of Primary Health Care. 2009, 27, 31–40. [Google Scholar]
 |
 |
 |
 |
 |
authors 2019 Salvatore Settineri1, Fabio Frisone, Angela Alibrandi, Emanuele Maria Merlo
Share and Cite
Settineri, S.; Frisone, F.; Alibrandi, A.; Merlo, E.M. Vulnerability and Physical Well-Being of Caregivers: What Relationship? J. Mind Med. Sci. 2019, 6, 95-102. https://doi.org/10.22543/7674.61.P95102
Settineri S, Frisone F, Alibrandi A, Merlo EM. Vulnerability and Physical Well-Being of Caregivers: What Relationship? Journal of Mind and Medical Sciences. 2019; 6(1):95-102. https://doi.org/10.22543/7674.61.P95102
Chicago/Turabian StyleSettineri, Salvatore, Fabio Frisone, Angela Alibrandi, and Emanuele Maria Merlo. 2019. "Vulnerability and Physical Well-Being of Caregivers: What Relationship?" Journal of Mind and Medical Sciences 6, no. 1: 95-102. https://doi.org/10.22543/7674.61.P95102
APA StyleSettineri, S., Frisone, F., Alibrandi, A., & Merlo, E. M. (2019). Vulnerability and Physical Well-Being of Caregivers: What Relationship? Journal of Mind and Medical Sciences, 6(1), 95-102. https://doi.org/10.22543/7674.61.P95102



