Postpartum Depression and Thyroid Dysfunction–Should Pregnant Women be Screened for Thyroid Disorders?
Highlights
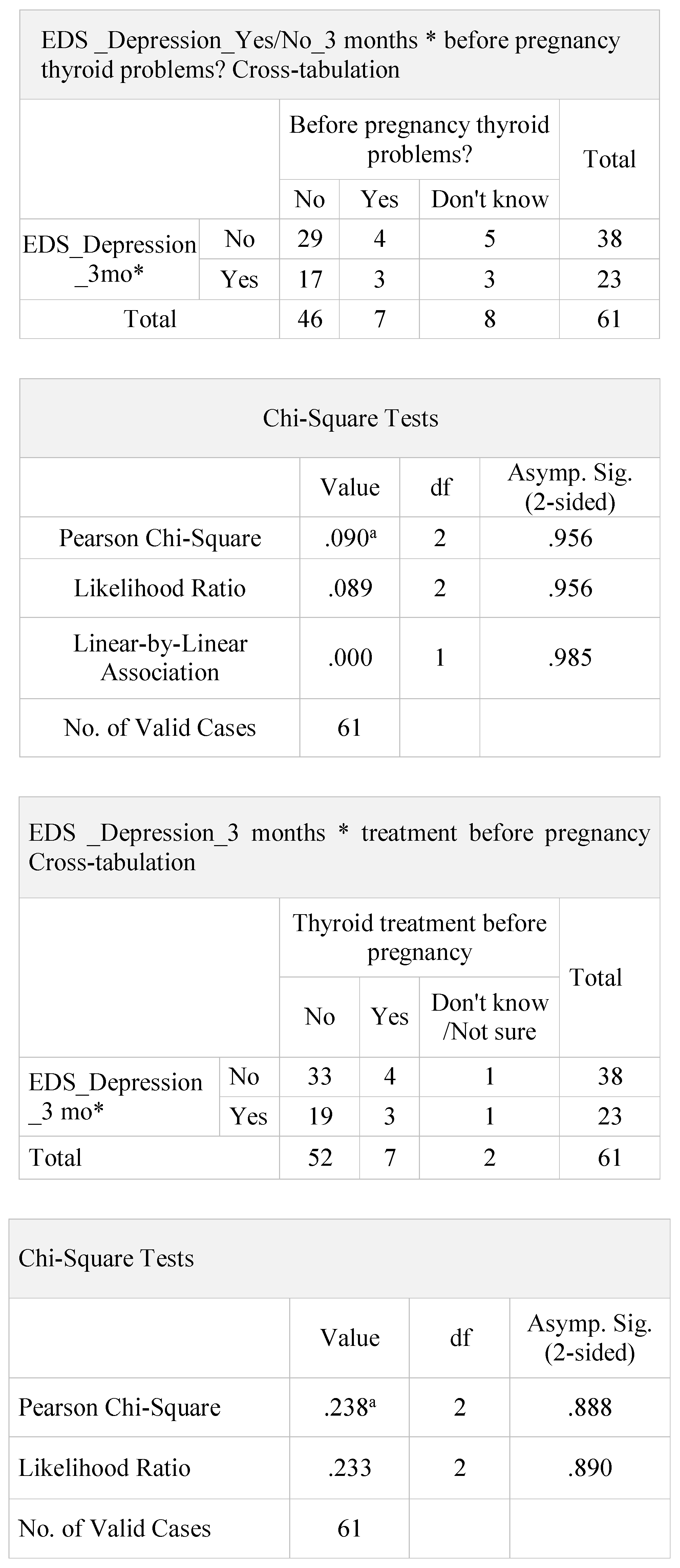
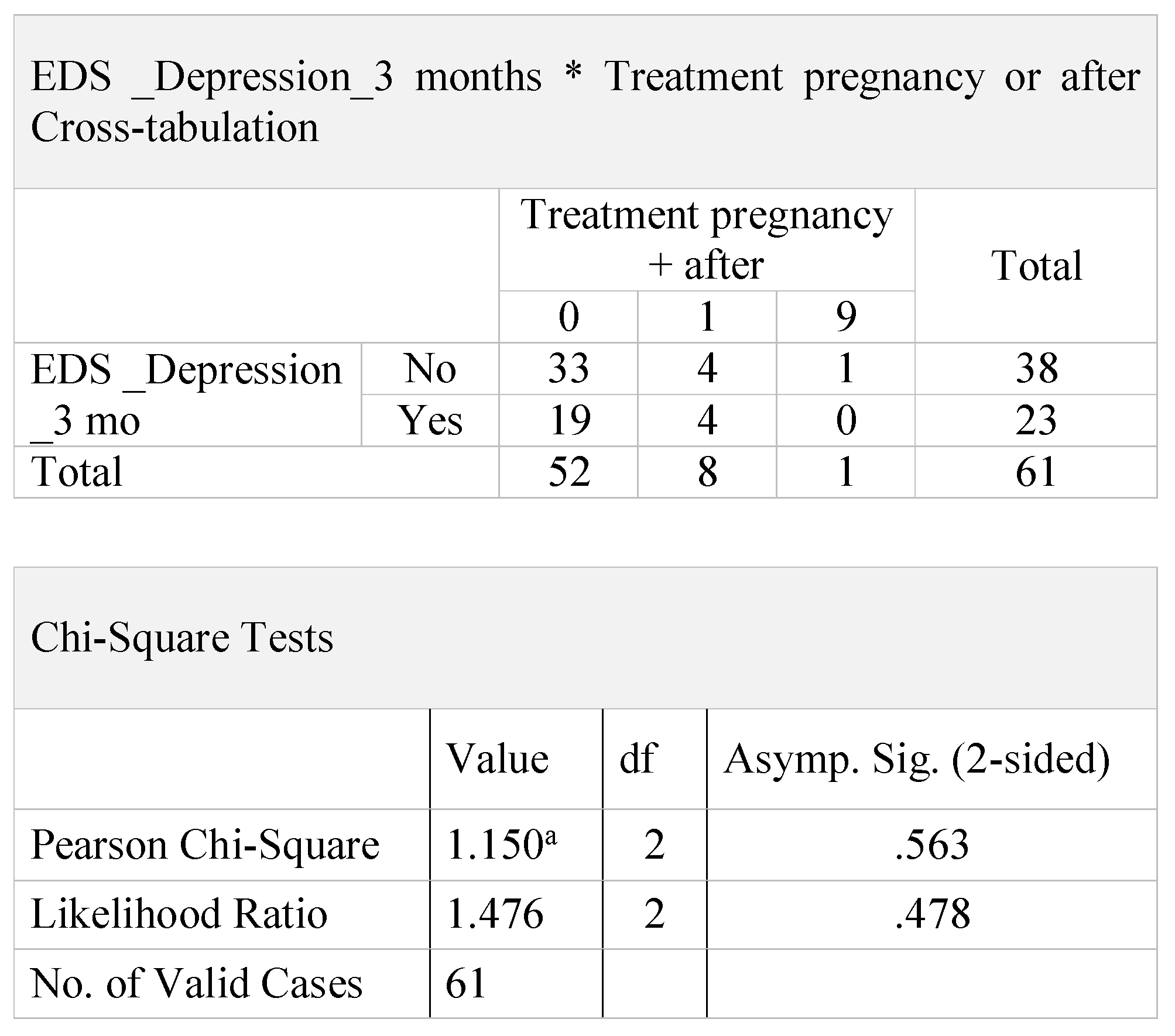
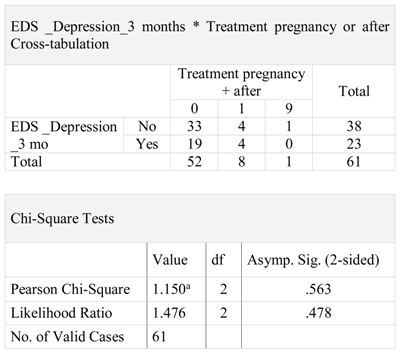
- This study found no difference in postpartumdepression for women with thyroid dysfunction compared to women without thyroid dysfunction.
- The study pinpoints the need for appropriate and constant assessment of postpartum depression in Romania and the creation of an appropriate medical structure to identify and mitigate the risks of postpartum depression.
Abstract
Highlights
- This study found no difference in postpartumdepression for women with thyroid dysfunction compared to women without thyroid dysfunction.
- The study pinpoints the need for appropriate and constant assessment of postpartum depression in Romania and the creation of an appropriate medical structure to identify and mitigate the risks of postpartum depression.
Introduction
Materials and Methods
- Variable 1—a variable showing if the patient had or did not have thyroid issues before pregnancy;
- Variable 2—a variable showing if the patient underwent or did not undergo treatment for the thyroid before pregnancy;
- Variable 3—a variable showing if the patient underwent or did not undergo treatment for the thyroid during pregnancy or immediately after (in the first year after giving birth).
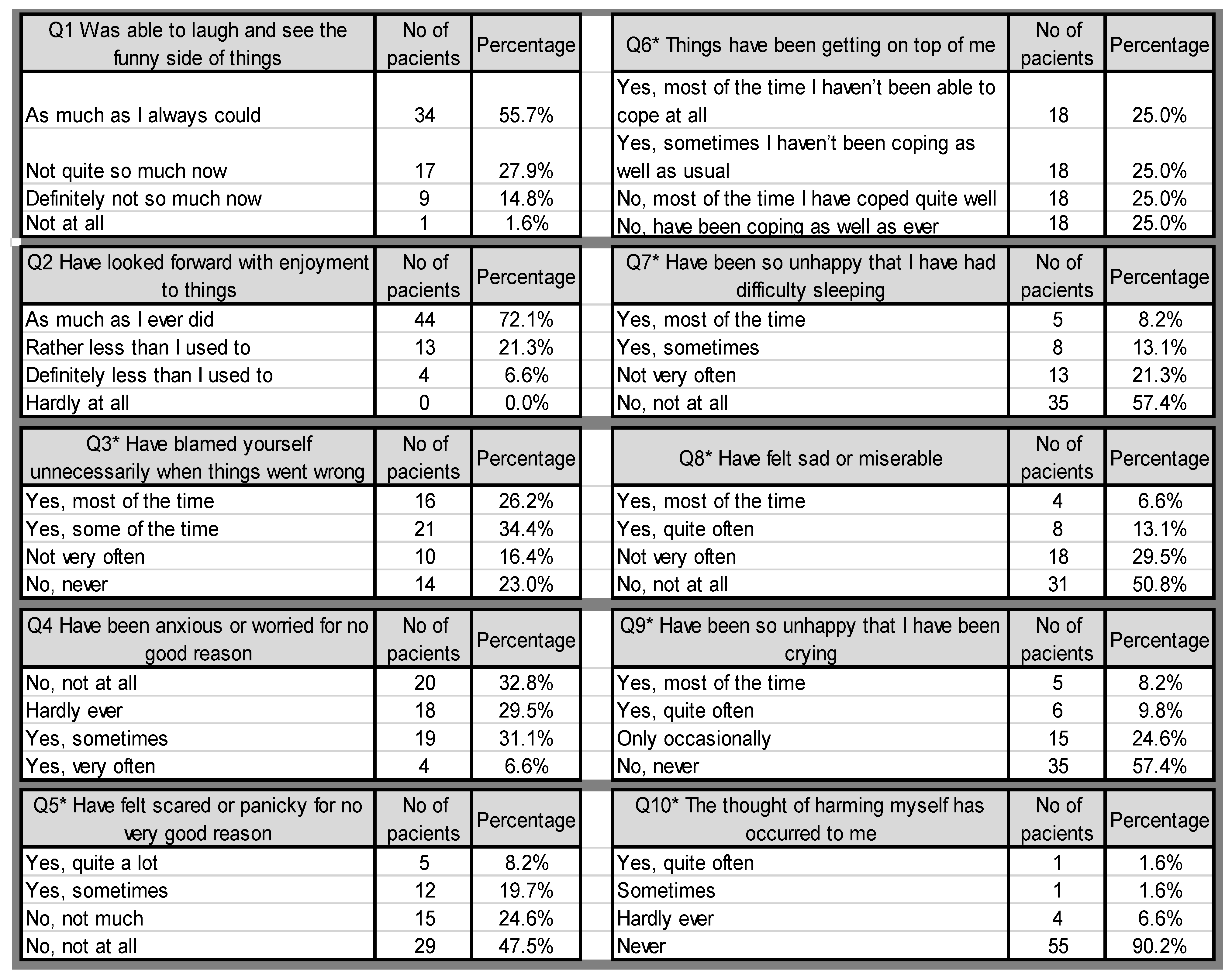
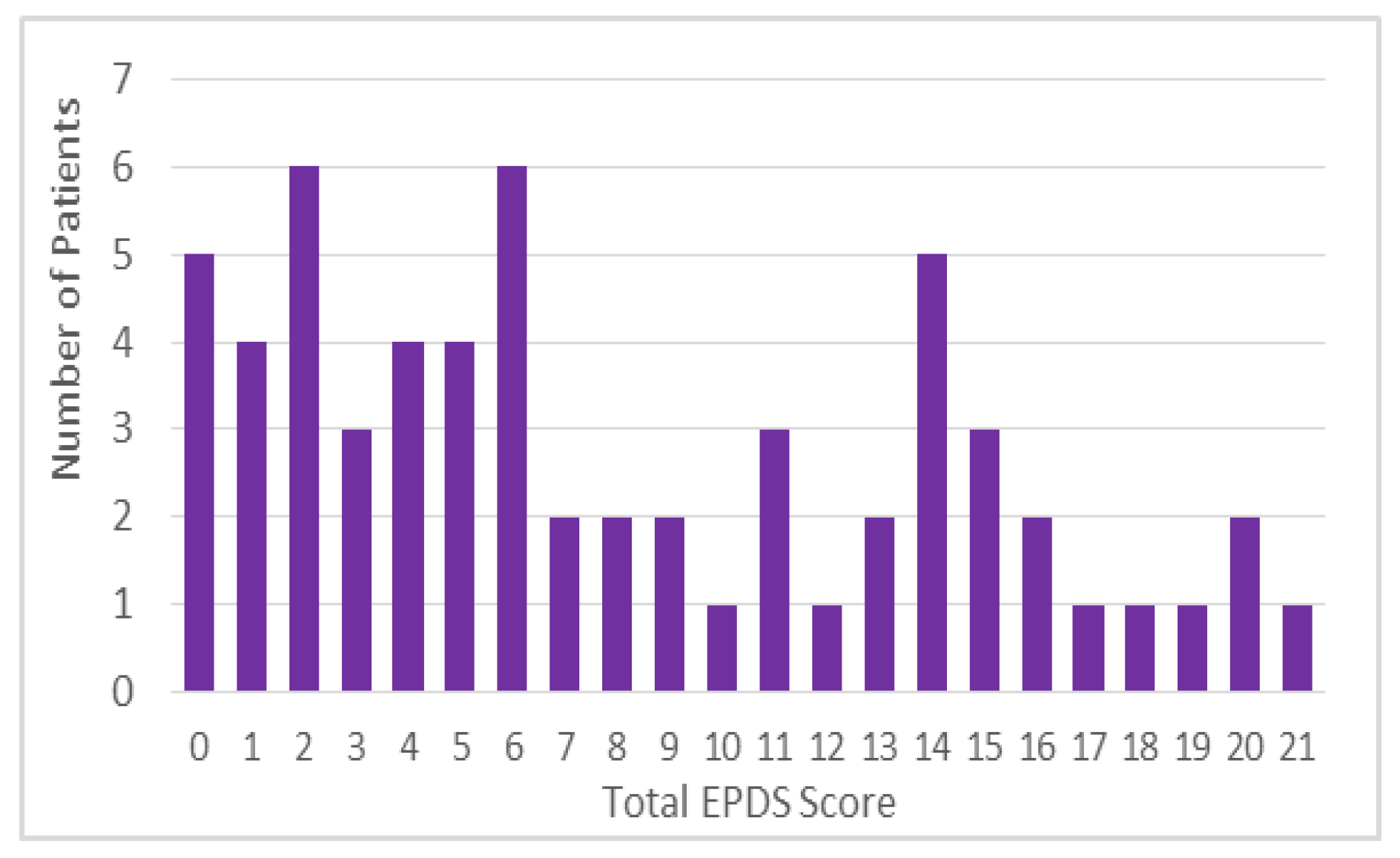
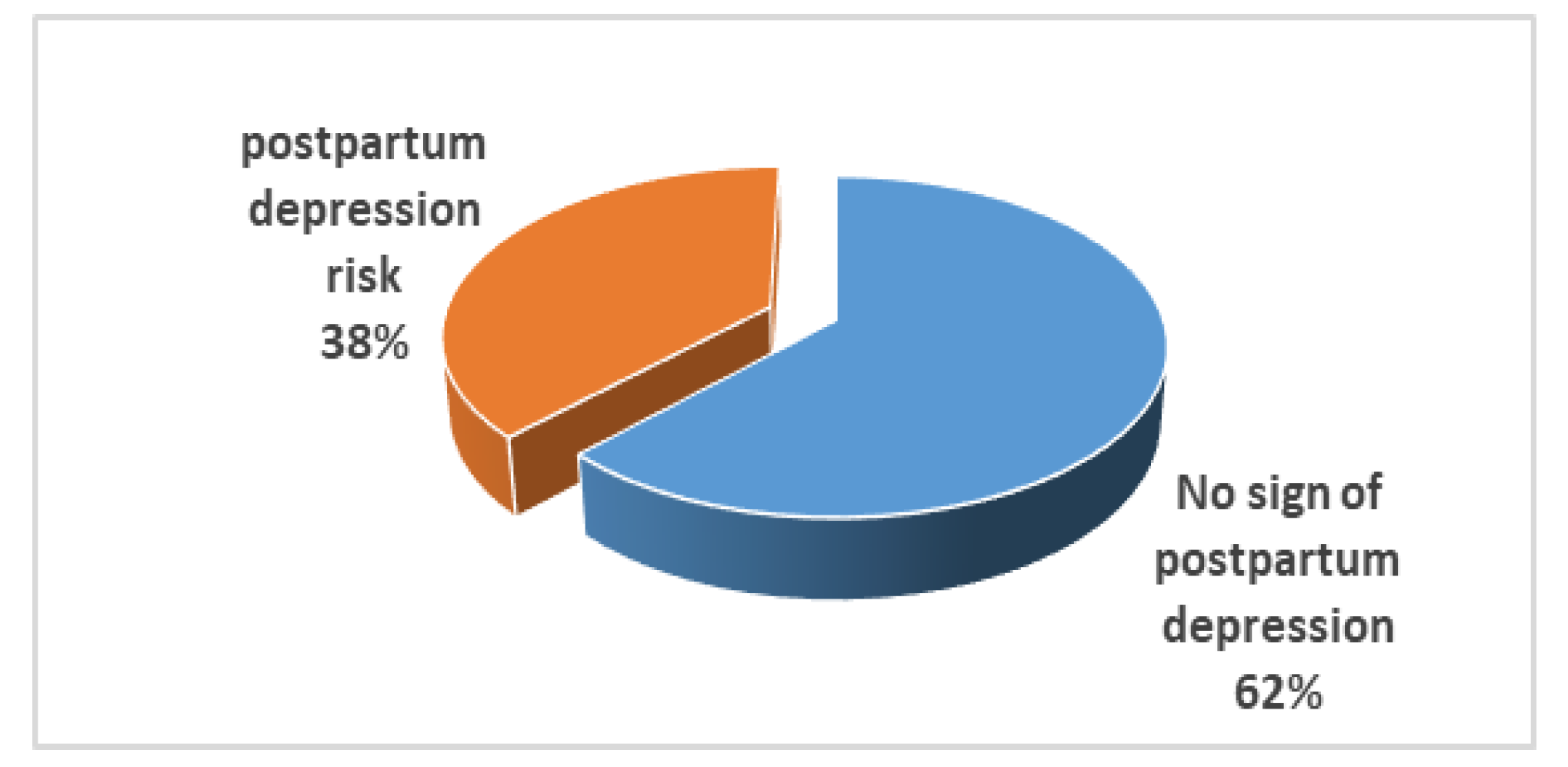
Results
Discussion
Conclusions
Compliance with Ethical Standards
Conflicts of Interest
References
- Rasmussen, M.H.; Strøm, M.; Wohlfahrt, J.; Videbech, P.; Melbye, M. Risk, treatment duration, and recurrence risk of postpartum affective disorder in women with no prior psychiatric history: A population-based cohort study. PLoS Med. 2017, 14, e1002392. [Google Scholar] [CrossRef]
- Patel, M.; Bailey, R.K.; Jabeen, S.; Ali, S.; Barker, N.C.; Osiezagha, K. Postpartum Depression: A Review. J Health Care Poor Underserved. 2012, 23, 534–542. [Google Scholar] [CrossRef] [PubMed]
- Gaynes, B.N.; Gavin, N.; Meltzer-Brody, S.; Lohr, K.N.; Swinson, T.; Gartlehner, G.; Brody, S.; Miller, W.C. Perinatal depression: Prevalence, screening accuracy, and screening outcomes. Evid Rep Technol Assess (Summ). 2005, 119, 1–8. [Google Scholar]
- Murray, L.; Sinclair, D.; Cooper, P.; Ducournau, P.; Turner, P.; Stein, A. The socioemotional development of 5- year-old children of postnatally depressed mothers. J Child Psychol Psychiatry. 1999, 40, 1259–1271. [Google Scholar] [PubMed]
- Hendrick, V. Treatment of postnatal depression. BMJ. 2003, 327, 1003–1004. [Google Scholar] [PubMed]
- Roti, E.; Uberti, E.d. Postpartum thyroiditis- a clinical update. Eur J Endocrinol. 2002, 146, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Hage, M.P. 1.; Azar, S.T. The link between thyroid function and depression. J Thyroid Res. 2012, 2012, 590648. [Google Scholar] [CrossRef] [PubMed]
- Alexander, E.K.; Pearce, E.N.; Brent, G.A.; Brown, R.S.; Chen, H.; Dosiou, C.; Grobman, W.A.; Laurberg, P.; Lazarus, J.H.; Mandel, S.J.; Peeters, R.P.; Sullivan, S. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017, 27, 315–389. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.; Brown, R.S.; Daumerie, C.; Hubalewska- Dydejczyk, A.; Negro, R.; Vaidya, B. European thyroid association guidelines for the management of subclinical hypothyroidism in pregnancy and in children. Eur Thyroid J. 2014, 3, 76–94. [Google Scholar] [CrossRef] [PubMed]
- Ardeleanu, I.; Nanu, M.; Moldovanu, F.; Nanu, A. Neonatal screening for hypothyroidism. Endocrine Abstracts 2015, 37, EP106. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987, 150, 782–786. [Google Scholar] [PubMed]
- Lambrinoudaki, I.; Rizos, D.; Armeni, E.; Pliatsika, P.; Leonardou, A.; Sygelou, A.; Argeitis, J.; Spentzou, G.; Hasiakos, D.; Zervas, I.; Papadias, C. Thyroid function and postpartum mood disturbances in Greek women. J Affect Disord. 2010, 121, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Iseme, R.A.; McEvoy, M.; Kelly, B.; Agnew, L.; Attia, J.; Walker, F.R.; Oldmeadow, C.; Boyle, M. Autoantibodies are not predictive markers for the development of depressive symptoms in a population-based cohort of older adults. Eur Psychiatry. 2015, 30, 694–700. [Google Scholar] [CrossRef] [PubMed]
- Harris, B.; Oretti, R.; Lazarus, J.; Parkes, A.; John, R.; Richards, C.; Newcombe, R.; Hall, R. Randomised trial of thyroxine to prevent postnatal depression in thyroid-antibody-positive women. Br J Psychiatry. 2002, 180, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Keshavarzi, F.; Yazdchi, K.; Rahimi, M.; Rezaei, M.; Farnia, V.; Davarinejad, O.; Abdoli, N.; Jalili, M. Post Partum Depression and Thyroid Function. Iran J Psychiatry. 2011, 6, 117–120. [Google Scholar] [PubMed]
- Josefsson, A.; Angelsiöö, L.; Berg, G.; Ekström, C.M.; Gunnervik, C.; Nordin, C.; Sydsjö, G. Obstetric, somatic, and demographic risk factors for postpartum depressive symptoms. Obstet Gynecol. 2002, 99, 223–228. [Google Scholar] [PubMed]
- Leung, S.S.; Leung, C.; Lam, T.H.; Hung, S.F.; Chan, R.; Yeung, T.; Miao, M.; Cheng, S.; Leung, S.H.; Lau, A.; Lee, D.T. Outcome of a postnatal depression screening programme using the Edinburgh Postnatal Depression Scale: A randomized controlled trial. J Public Health (Oxf). 2011, 33, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Paulden, M.; Palmer, S.; Hewitt, C.; Gilbody, S. Screening for postnatal depression in primary care: Cost effectiveness analysis. BMJ. 2009, 339, b5203. [Google Scholar] [CrossRef] [PubMed]
- Basraon, S.; Costantine, M.M. Mood disorders in pregnant women with thyroid dysfunction. Clin Obstet Gynecol. 2011, 54, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Wisner, K.L.; Parry, B.L.; Piontek, C.M. Postpartum Depression. N Engl J Med. 2002, 347, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Wolkowitz, O.M.; Rothschild, A.J. (Eds.) Psychoneuroendocrinology: The Scientific Basis of Clinical Practice; American Psychiatric Press: Washington, DC, USA, 2003; ISBN 0880488573. ISSN 9780880488570. [Google Scholar]
 |
authors 2019 Anca A. Simionescu, Erika Marin
Share and Cite
Simionescu, A.A.; Marin, E. Postpartum Depression and Thyroid Dysfunction–Should Pregnant Women be Screened for Thyroid Disorders? J. Mind Med. Sci. 2019, 6, 103-109. https://doi.org/10.22543/7674.61.P103109
Simionescu AA, Marin E. Postpartum Depression and Thyroid Dysfunction–Should Pregnant Women be Screened for Thyroid Disorders? Journal of Mind and Medical Sciences. 2019; 6(1):103-109. https://doi.org/10.22543/7674.61.P103109
Chicago/Turabian StyleSimionescu, Anca A., and Erika Marin. 2019. "Postpartum Depression and Thyroid Dysfunction–Should Pregnant Women be Screened for Thyroid Disorders?" Journal of Mind and Medical Sciences 6, no. 1: 103-109. https://doi.org/10.22543/7674.61.P103109
APA StyleSimionescu, A. A., & Marin, E. (2019). Postpartum Depression and Thyroid Dysfunction–Should Pregnant Women be Screened for Thyroid Disorders? Journal of Mind and Medical Sciences, 6(1), 103-109. https://doi.org/10.22543/7674.61.P103109



