Microleakage—The Main Culprit in Bracket Bond Failure?
Highlights
- In vitro microleakage value was higher in the gingival margin at the enamel-adhesive interfaces and in the occlusal margin at the adhesive-metal bracket interfaces.
- Bracket debonding remains the main concern during the orthodontic treatment, despite the new techniques that may improve the conventional orthodontic treatment.
Abstract
Highlights
- In vitro microleakage value was higher in the gingival margin at the enamel-adhesive interfaces and in the occlusal margin at the adhesive-metal bracket interfaces.
- Bracket debonding remains the main concern during the orthodontic treatment, despite the new techniques that may improve the conventional orthodontic treatment.
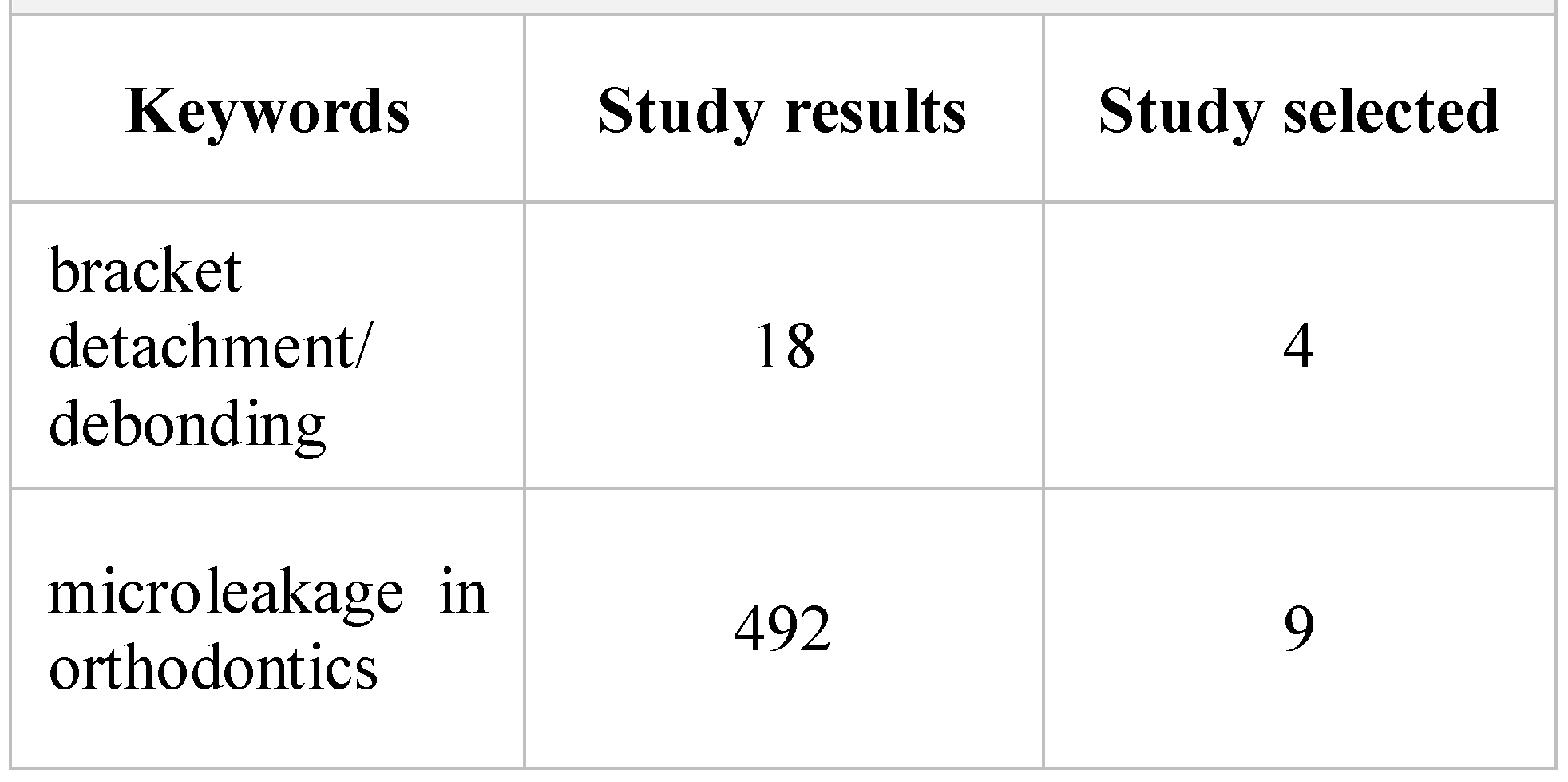
Introduction
Objective
Materials and Methods
Results and Discussions
Limitations
Conclusions and future directions
Compliance with Ethical Standards
Acknowledgments
Conflicts of Interest
References
- Isber, H.; Ambrosio, A.R.; Carvalho, P.E.; Valle-Corotti, K.M.; Siqueira, D.F. Comparative in vitro study of the shear bond strength of brackets bonded with restorative and orthodontic resins. Braz Oral Res. 2011, 25, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Elsaka, S.E.; Hammad, S.M.; Ibrahim, N.F. Evaluation of stresses developed in different bracket-cement-enamel systems using finite element analysis with in vitro bond strength tests. Prog Orthod. 2014, 15, 33. [Google Scholar] [CrossRef]
- Gioka, C.; Bourauel, C.; Zinelis, S.; Eliades, T.; Silikas, N.; Eliades, G. Titanium orthodontic brackets: structure, composition, hardness and ionic release. Dentl Mater. 2004, 20, 693–700. [Google Scholar] [CrossRef]
- Kusy, R.P.; O’grady, P.W. Evaluation of titanium brackets for orthodontic treatment: part II—the active configuration. Am J Orthod Dentofacial Orthop. 2000, 118, 675–684. [Google Scholar] [CrossRef] [PubMed]
- Klocke, A.; Kahl-Nieke, B. Influence of force location in orthodontic shear bond strength testing. Dent Mater. 2005, 21, 391–396. [Google Scholar] [CrossRef]
- Gama, A.C.; Moraes, A.G.; Yamasaki, L.C.; Loguercio, A.D.; Carvalho, C.N.; Bauer, J. Properties of composite materials used for bracket bonding. Braz Dent, J. 2013, 24, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Parrish, B.C.; Katona, T.R.; Isikbay, S.C.; Stewart, K.T.; Kula, K.S. The effects of application time of a self-etching primer and debonding methods on bracket bond strength. Angle Orthod. 2012, 82, 131–136. [Google Scholar] [CrossRef]
- Dall’Igna, C.M.; Marchioro, E.M.; Spohr, A.M.; Mota, E.G. Effect of curing time on the bond strength of a bracket-bonding system cured with a light-emitting diode or plasma arc light. Eur J Orthod. 2011, 33, 55–59. [Google Scholar] [CrossRef]
- Karandish, M. Relevance of Micro-leakage to Orthodontic Bonding- a Review. J Dent. Biomater. 2016, 3, 254–260. [Google Scholar]
- Youssef, M.N.; Youssef, F.A.; Souza-Zaroni, W.C.; Turbino, M.L.; Vieira, M.M. Effect of enamel preparation method on in vitro marginal microleakage of a flowable composite used as pit and fissure sealant. Int J Paediatr Dent. 2006, 16, 342–347. [Google Scholar] [CrossRef]
- Mahal, R.-D.S. A Standardized Approach to Determine the Effect of Thermocycling and Long Term Storage on the Shear Bond Strength of Orthodontic Brackets Cemented to bovine Enamel; National Library of Canada=Bibliothèque Nationale du: Ottawa, ON, Canada, 2000. [Google Scholar]
- Canbek, K.; Karbach, M.; Gottschalk, F.; Erbe, C.; Wehrbein, H. Evaluation of bovine and human teeth exposed to thermocycling for microleakage under bonded metal brackets. J Orofac Orthop. 2013, 74, 102–112. [Google Scholar] [CrossRef]
- Bishara, S.E.; Ostby, A.W.; Laffoon, J.F.; Warren, J. Shear bond strength comparison of two adhesive systems following thermocycling: a new self-etch primer and a resin-modified glass ionomer. Angle Orthod. 2007, 77, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Lamper, T.; Ilie, N.; Huth, K.C.; Rudzki, I.; Wichelhaus, A.; Paschos, E. Self-etch adhesives for the bonding of orthodontic brackets: faster, stronger, safer? Clin Oral Investig. 2014, 18, 313–319. [Google Scholar] [CrossRef]
- Almosa, N.; Zafar, H. Incidence of orthodontic brackets detachment during orthodontic treatment: A systematic review. Pak J Med Sci. 2018, 34, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Reddy, K.; Kishore MS, V.; Safeena, S. Shear bond strength of acidic primer, light-cure glass ionomer, light-cure and self-cure composite adhesive systems-an in vitro study. J Int Oral Health. 2013, 5, 73–78. [Google Scholar]
- Ahmed, T.; Rahman, N.A.; Alam, M.K. Assessment of in vivo bond strength studies of the orthodontic bracket- adhesive system: A systematic review. Eur J Dent. 2018, 12, 602–609. [Google Scholar] [CrossRef]
- Sha, H.N.; Choi, S.H.; Yu, H.S.; Hwang, C.J.; Cha, J.Y.; Kim, K.M. Debonding force and shear bond strength of an array of CAD/CAM-based customized orthodontic brackets, placed by indirect bonding—An in Vitro study. PLoS One. 2018, 13, e0202952. [Google Scholar] [CrossRef]
- Piccoli, L.; Migliau, G.; Besharat, L.K.; Di Carlo, S.; Pompa, G.; Di Giorgio, R. Comparison of two different debonding techniques in orthodontic treatment. Ann Stomatol (Roma). 2017, 8, 71–78. [Google Scholar] [CrossRef]
- Arash, V.; Naghipour, F.; Ravadgar, M.; Karkhah, A.; Barati, M.S. Shear bond strength of ceramic and metallic orthodontic brackets bonded with self-etching primer and conventional bonding adhesives. Electron Physician. 2017, 9, 3584–3591. [Google Scholar] [CrossRef]
- Kaneshima, E.N.; Berger, S.B.; Fernandes, T.M.F.; Navarro, M.F.L.; Oltramari, P.V.P. Using UV light for adhesive remnant removal after debonding of orthodontic accessories. Braz Oral Res. 2018, 32, e47. [Google Scholar] [CrossRef]
- Hedayati, Z.; Farjood, A. Evaluation of Microleakage under Orthodontic Brackets Bonded with Nanocomposites. Contemp Clin Dent. 2018, 9, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, F.; Ersöz, M.; Öztürk, S.A.; Hatunoğlu, E.; Malkoç Micro, C.T. Evaluation of microleakage under orthodontic ceramic brackets bonded with different bonding techniques and adhesives. Eur J Orthod. 2016, 38, 163–169. [Google Scholar] [CrossRef]
- Pakshir, H.; Ajami, S. Effect of Enamel Preparation and Light Curing Methods on Microleakage under Orthodontic Brackets. J Dent (Tehran). 2015, 12, 436–446. [Google Scholar]
- Kim, J.; Kanavakis, G.; Finkelman, M.D.; Lee, M. Microleakage under ceramic flash-free orthodontic brackets after thermal cycling. Angle Orthod. 2016, 86, 905–908. [Google Scholar] [CrossRef] [PubMed]
- Alkis, H.; Turkkahraman, H.; Adanir, N. Microleakage under orthodontic brackets bonded with different adhesive systems. Eur J Dent. 2015, 9, 117–121. [Google Scholar] [CrossRef]
- Tudehzaeim, M.H.; Yassaei, S.; Taherimoghadam, S. Comparison of Microleakage under Rebonded Stainless Steel Orthodontic Brackets Using Two Methods of Adhesive Removal: Sandblast and Laser. J Dent (Tehran). 2015, 12, 118–124. [Google Scholar] [PubMed]
- Toodehzaeim, M.H.; Rezaie, N. Effect of Saliva Contamination on Microleakage Beneath Bonded Brackets: A Comparison Between Two Moisture- Tolerant Bonding Systems. J Dent (Tehran). 2015, 12, 747–755. [Google Scholar]
- Toodehzaeim, M.H.; Yassaei, S.; Karandish, M.; Farzaneh, S. In vitro evaluation of microleakage around orthodontic brackets using laser etching and Acid etching methods. J Dent (Tehran). 2014, 11, 263–269. [Google Scholar]
- Shahabi, M.; Ahrari, F.; Mohamadipour, H.; Moosavi, H. Microleakage and shear bond strength of orthodontc brackets bonded to hypomineralized enamel following different surface preparations. J Clin Exp Dent. 2014, 6, e110–e115. [Google Scholar] [CrossRef]
- Dong, Q.; Chen, C.; Shan, L. A study on the relationship between the orthopedics of mandibular retrognathia and hypertension. Journal of Modern Stomatology. 2004, 1, 036. [Google Scholar]
- Rusu, A.; Todea, D.; Rosca, L.; Nita, C.; Bala, C. The development of a sleep apnea screening program in Romanian type 2 diabetic patients: a pilot study. Acta Diabetol. 2012, 49, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Bensch, L.; Braem, M.; Van Acker, K.; Willems, G. Orthodontic treatment considerations in patients with diabetes mellitus. Am J Orthod Dentofacial Orthop. 2003, 123, 74–78. [Google Scholar]
- Nita, R.A.; Todea, D.; Rosca, L.; Bala, C.; Hancu, N. Correlation of the daytime sleepiness with respiratory sleep parameters in patients with sleep apnea and type 2 diabetes. Acta Endo (Buc). 2011, 7, 163–171. [Google Scholar]
- Neeley WW 2nd Gonzales, D.A. Obesity in adolescence: implications in orthodontic treatment. Am J Orthod Dentofacial Orthop. 2007, 131, 581–588. [Google Scholar] [CrossRef]
- Alexescu, T.; Motocu, M.; Negrean, V.; Tarmure, S.; Lencu, M. Obezitatea si Sindromul metabolic. Epidemiologie si Etiopatogenie. Clujul Medical. 2009, 82, 353–359. [Google Scholar]
- Vremaroiu-Coman, A.; Alexescu, T.G.; Negrean, V.; Milaciu, M.V.; Buzoianu, A.D.; Ciumarnean, L.; Todea, A.D. Ethical aspects of smoking cessation among the population from Transylvania. Balneo Research Journal. 2018, 9, 254–259. [Google Scholar]
- Burden, D.; Mullally, B.; Sandler, J. Orthodontic treatment of patients with medical disorders. Eur J Orthod. 2001, 23, 363–372. [Google Scholar] [PubMed]
- Ionescu, R.; Bertesteanu, S.V.; Popescu, R.C.; Balalau, C.; Scaunasu, R.V.; Popescu, B. Standard or individualized quality of life for larynx cancer patients? J Clin Invest Surg. 2018, 3, 62–65. [Google Scholar] [CrossRef]
- Lucas, V.S.; Omar, J.; Vieira, A.; Roberts, G.J. The relationship between odontogenic bacteraemia and orthodontic treatment procedures. Eur J Orthod. 2002, 24, 293–301. [Google Scholar]
- Radescu, D.O.; et al. Results in the Treatment with Twin Block Polymeric Appliance of the Retrognathic Mandible in Sleep Apnea Patients. Materiale Plastice 2017, 54, 473–476. [Google Scholar]
- Banabilh, S.M. Orthodontic view in the diagnoses of obstructive sleep apnea. J Orthod Sci. 2017, 6, 81–85. [Google Scholar] [CrossRef]
- Coman, A.C.; et al. Multilateral characterization of masks and tubes surfaces in contact with respiratory system through ventilation. Journal of Optoelectronics and Advanced Materials 2015, 17, 1563–1571. [Google Scholar]
- Daley, T.D.; Armstrong, J.E. Oral manifestations of gastrointestinal diseases. Can J Gastroenterol. 2007, 21, 241–244. [Google Scholar] [PubMed]
- Todea, D.; Cadar, O.; Simedru, D.; Roman, C.; Tanaselia, C.; Suatean, I.; Naghiu, A. Determination of Major-to- Trace Minerals and Polyphenols in Different Apple Cultivars. Not Bot Horti Agrobo. 2014, 42, 523–529. [Google Scholar]
- Gomes, M.N.; Dutra, H.; Morais, A.; Sgura, R.; Devito-Moraes, A.G. In-Office Bleaching During Orthodontic Treatment. J Esthet Restor Dent. 2017, 29, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Bordea, I.R.; et al. The influence of chromophore presence in an experimental bleaching gel on laser assisted tooth whitening efficiency. Studia Universitatis Babes-Bolyai. Chemia 2016, 61, 215–224. [Google Scholar]
- Yadav, D.; et al. Effect of tooth bleaching on orthodontic stainless steel bracket bond strength. J Orthod Sci. 2015, 4, 72–76. [Google Scholar] [CrossRef]
- Andreea, S.; et al. Correlations Between pH Values of Oral Fluid and Dental Caries Epidemiologic Indicators in Children Aged within 6-12 Years. Revista de Chimie 2018, 69, 484–487. [Google Scholar]

 |
authors Ioana Roxana Bordea, Adina Sîrbu, Ondine Lucaciu, Aranka Ilea, Radu Septimiu Câmpian, Doina Adina Todea, Teodora Gabriela Alexescu, Maria Aluaș, Corina Budin and Andreea Simona Pop
Share and Cite
Bordea, I.R.; Sîrbu, A.; Lucaciu, O.; Ilea, A.; Câmpian, R.S.; Todea, D.A.; Alexescu, T.G.; Aluaș, M.; Budin, C.; Pop, A.S. Microleakage—The Main Culprit in Bracket Bond Failure? J. Mind Med. Sci. 2019, 6, 86-94. https://doi.org/10.22543/7674.61.P8694
Bordea IR, Sîrbu A, Lucaciu O, Ilea A, Câmpian RS, Todea DA, Alexescu TG, Aluaș M, Budin C, Pop AS. Microleakage—The Main Culprit in Bracket Bond Failure? Journal of Mind and Medical Sciences. 2019; 6(1):86-94. https://doi.org/10.22543/7674.61.P8694
Chicago/Turabian StyleBordea, Ioana Roxana, Adina Sîrbu, Ondine Lucaciu, Aranka Ilea, Radu Septimiu Câmpian, Doina Adina Todea, Teodora Gabriela Alexescu, Maria Aluaș, Corina Budin, and Andreea Simona Pop. 2019. "Microleakage—The Main Culprit in Bracket Bond Failure?" Journal of Mind and Medical Sciences 6, no. 1: 86-94. https://doi.org/10.22543/7674.61.P8694
APA StyleBordea, I. R., Sîrbu, A., Lucaciu, O., Ilea, A., Câmpian, R. S., Todea, D. A., Alexescu, T. G., Aluaș, M., Budin, C., & Pop, A. S. (2019). Microleakage—The Main Culprit in Bracket Bond Failure? Journal of Mind and Medical Sciences, 6(1), 86-94. https://doi.org/10.22543/7674.61.P8694



