Highlights
- The tendency for recurrence, the local destructive ability and the risk of malignant transformation are the main problems posed by sinonasal inverted papillomata.
- The complete removal of the tumor and an aggressive follow-up are necessary for a good outcome for the patient.
Abstract
Sinonasal inverted papilloma is a rare benign epithelial tumor. Its three main clinical characteristics are the tendency of recurrence, the destructive ability of nearby structures and malignant transformation. The primary manifestations of this tumor include nasal obstruction, headaches, runny nose, hemorrhage and impaired sense of smell. The diagnosis is based on the clinical and endoscopic examination completed by CT or MRI scans and biopsy of the lesion. Allergies, chronic inflammation, nicotinism and viral infections such as HPV infection are considered possible causes of pathogenesis and potential risk factors for relapse and malignancy. The treatment for this condition is the complete removal of the tumor with disease-free margins. Postoperative follow-up is essential for the early detection of recurrence or malignant transformation. One of the most basic and important steps in managing these patients is to acknowledge the presence of the mentioned risk factors and avoid exposure. Due to the high risk of relapse, the follow-up must be aggressive and thorough and always include the endoscopic examination. In our article, we wish to highlight the importance of the proper surgical intervention, but also the difference in the overall outcome of the patient ensured by the correct management of the risk factors, allowing us to prevent recurrence and malignant transformation.
Highlights
The tendency for recurrence, the local destructive ability and the risk of malignant transformation are the main problems posed by sinonasal inverted papillomata.
The complete removal of the tumor and an aggressive follow-up are necessary for a good outcome for the patient.
Introduction
The sinonasal inverted papilloma is a rare benign epithelial tumor that derives from the Schneiderian membrane. The Schneiderian membrane is a ciliated columnar epithelium that originates in the ectodermis and forms a boundary between the sinus and nasal mucosa (1). This pathology is classified into three types: oncocytic, fungiform and inverted papilloma, which is the most common type. The inverted papilloma is more frequent in men than in women with the onset between the 4th and the 7th decade of life (1).
This tumor is usually unilateral, with its origin on the lateral wall of the nasal cavity in the middle meatal area. The growth of the inverted papilloma is inward in fingerlike projections. They are locally aggressive and are characterised by rapid growth with the destruction of nearby areas and bone erosion that can dramatically change the anatomical landmarks of the nasal cavity and sinuses. Other characteristics of the inverted papilloma are the invasion of the adjacent regions of the facial skeleton and anterior skull base, its tendency to recur and the risk of malignant transformation (2).
The pathogenesis of inverted papilloma is unclear. Allergies, chronic inflammation, nicotinism, viral infections such as HPV infection, diabetes, hypertension are considered possible causes (3, 4).
The primary manifestations of this tumor include nasal obstruction, headaches, runny nose, bleeding, impaired sense of smell. These symptoms can be accompanied by impaired vision and facial pain (5).
The majority of inverted papillomata are discovered during a physical ENT examination. For a better visualisation of the tumor, nasal endoscopy is performed. Their macroscopic appearance is a red-grey polypoid tumor, with an uneven surface that may bleed upon touching. Furthermore, the radiologic examination is needed to evaluate the extent of the tumor and the lesions of nearby structures. Because of its bone erosion characteristic, some surgeons consider CT scans the radiologic evaluation of choice, but CT scanning does not allow a proper differentiation between soft tissue and secretions. To avoid a wrong interpretation of the extent of the tumor, sometimes a complementary MRI is needed (6, 7).
The most frequent method used to evaluate the clinical preoperative severity is the Krouse classification, considering tumor location and malignancy:
- T1: tumor restricted to the nasal cavity only
- T2: tumor limited to ethmoid cells and/or the medial wall of the maxillary sinus
- T3: tumor extending to the lateral, inferior, superior, anterior, or posterior wall of the maxillary sinus or penetrating the sphenoid or frontal sinus
- T4: tumor extending beyond the sinonasal boundaries or any malignant tumor (8).
Discussions
Literature data
In order to assess the current practice regarding patients with inverted papillomata, we researched the available data and studies in the Medline database. For this purpose, a number of 5 studies and 23 articles on the topic and related data were reviewed, searching for a significant combination of terms that included: inverted papilloma recurrence, malignant transformation and risk factors. We only took into account the data relevant for the subject discussed. We researched both the method of choice for surgery according to the extension of the tumor and the protocol for the follow-up program.
In patients with inverted papilloma, the surgeon aims to remove an entire tumor. The surgical strategies varied over the years (9).
For a long time, lateral rhinotomy with medial maxillectomy and ethmoidectomy had been considered the treatment of choice, but with the development of endoscopy in the field of ENT, new and less invasive procedures have appeared (9).
Nowadays, endoscopic sinus surgery with the removal of the entire tumor represents “the gold standard” treatment for inverted papillomata. The advantages of endoscopic surgery are no external scars, good intraoperative visualisation of the lesion and adjacent structures, shorter healing periods and hospitalisation time (10).
However, in some cases, both endoscopic and external approaches are required to resect the entire lesion. The approach is chosen following the Krouse classification. According to this staging, patients with T1 and T2 tumors can undergo successful endoscopic surgery, and patients with stages T3 and T4 need a combined approach (11).
The elective investigations for inverted papillomata are computed tomography (CT) and magnetic resonance imaging (MRI). CT images are preferable because of the bony structure visualization, allowing to locate the papilloma attachment site, represented by a focal hyperostosis (12).
It was noted that endoscopic procedures performed by experienced surgeons present a lower risk of tumor recurrence than the external approach (13).
The surgical strategy is to reveal the insertion of the tumor and then to remove it entirely, if possible. After the removal of the tumor, the drilling of the insertion area is required to minimize the risk of recurrence. If the tumor extends to the orbital fossa or cerebral cranium, it is safer to segment the tumor and remove it piecemeally. At the end of surgery, the remaining cavity must be large enough to ensure optimal endoscopic follow-up procedures.
Complications such as hemorrhage from the sphenopalatine artery, internal maxillary artery or anterior ethmoidal artery, orbital complications or CSF leaks may occur due to the nearby important anatomical structures.
Postoperative follow-up is very important to detect relapse or malignant transformation in the early stages. In our clinic, the follow-up consists in an endoscopic examination of the patient every three months in the first two years and every six months in the next two years. If recurrence is suspected, a radiological evaluation is performed.
Results
The endoscopic approach is an overall method with excellent results, thus easier to accept by the patient. The advancements in the technological area have made the resection of large tumors in safe conditions possible. Also, the absence of any scars makes patients more prone to accept the intervention and present a higher adherence to the management protocol.
However, we must not rely on endoscopy alone. At any point of the intervention, the surgeon may be forced to switch to an open approach, or in cases of largely extensive tumors, this may be the method of choice from the beginning. That is why any surgeon approaching this pathology must be thoroughly prepared to perform an open approach as well.
Another subject that must be underlined is the advantage offered by a combined approach, with a lateral rhinotomy completed with the endoscopic control of the underlying areas. At any point, the magnified image offered by endoscopy will increase the degree of safety and will help expose areas that may be difficult to be only visually assessed, regardless of one’s experience. This is the preferable method for large extensive tumors, especially if located in the vicinity of vital structures. This may be the case due to the tendency of extension of inverted papillomata. This applies more often to cases with malignant degeneration, with late presentation to the doctor and delayed diagnosis.
The method of choice in treating patients with this pathology remains surgery. The tumor must be completely resected in order to avoid recurrence. We believe that the endoscopic approach can be considered the method of choice nowadays. It offers the possibility to completely resect the tumor in safe conditions, with minimal trauma for the patient and a faster recovery period. Also, the limited scarring and fibrosis increase the adherence to treatment and facilitate the follow-up. The process of regular appointments and endoscopic examinations has proven to be equally important to avoid postoperative complications and if any recurrence occurs, to provide a fast re-intervention.
Interpretations
Incomplete tumor resection or positive surgical margins represent the leading cause of recurrence of the inverted papilloma. Therefore, a proper selection of the surgical approach based on the preoperative nasal endoscopy and radiological examination is needed.
Pathological mucosal fragments left within the anfractuosities of the bone can also be a cause of recurrence; therefore, the resection of the bone should be considered after the excision of the tumor.
For a good outcome, the tumor needs to be resected along with the periosteum, paying extra attention to the origin site of the tumor shown on CT scans. A five- millimeter resection margin is recommended to obtain free surgical margins. Moreover, an intraoperative histopathological investigation can be done to prove negative resection margins. Even if surgery was well performed and free margins were insured, inverted papilloma recurrence may occur in distant locations from the primary site. The explanation for this type of recurrence is the multicenter origin of the inverted papilloma theory.
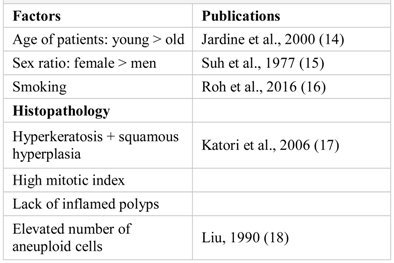
According to the relation between the stage of the tumor and the recurrence rate, it was noted that patients with T3-T4 stages (Krouse classification) present a higher risk of recurrence than patients with T1-T2 stages. However, the difference between the recurrence based on the different stages of the tumor is not significant enough to formulate a hypothesis (8, 11) (Table 1).

Table 1.
Risk factors for the recurrence of inverted papilloma.
The approach of the inverted papilloma can also be considered a risk factor for recurrence. Several studies have revealed better results with fewer recurrence rates for the endoscopic approach than the external one (19, 20).
The results of the studies regarding the relation between HPV and the onset of inverted papilloma are controversial. It is believed that the E6 and E7 viral oncoproteins play an important role in the genesis of the tumor and especially patients diagnosed with HPV-18 present a high risk of malignant transformation of the inverted papilloma (21, 22).
Another risk factor for recurrence and malignant transformation is smoking. It causes chronic inflammation of the sinonasal mucosa which leads to a higher relapse chance, but no conclusions were made regarding its relationship with malignant transformation (23, 24).
Several studies regarding the correlation between the recurrence risk and the location of the inverted papilloma were made. The results of the studies revealed that the inverted papilloma originating in the nasal cavity had reduced the recurrence risk compared with the ones that originate in the sinuses, especially in the frontal sinus. The reasons can be earlier diagnosis and a more accessible surgical approach (25).
Patients with systemic disease pose a greater therapeutic challenge. Out of all the comorbidities, coagulopathies are some of the most dangerous. These problems relate to both the general anesthesia that is necessary and the intervention itself, which can result in significant hemorrhages. Patients who associate other severe conditions, especially neurological, cardiologic or oncological, will associate a higher risk during the intervention and in the immediate period (26).
Studies show that 9% of inverted papillomata suffer malignant transformation, the most common tumor being squamous cell carcinoma (27). The malignant tumors usually develop from the primary mass of the inverted papilloma, but they can also appear after the surgical treatment. The prognosis for these tumors is poor, with a survival rate of 5 to 10 years in 39.6% of cases. An even lower survival rate is noted when the malignant tumor is diagnosed in an advanced stage with low differentiation. MRI is considered a very useful method for the early detection of malignant transformation of inverted papilloma. Radiotherapy should be considered if surgery is contraindicated or it should be done postoperatively if the inverted papilloma is associated with squamous cell carcinoma (23).
SCCA is the squamous cell carcinoma antigen released into blood circulation by the squamous cells. It became a nonspecific marker used in monitoring head and neck, ovarian, lung or hepatic carcinomata (24). Studies revealed increased levels of SCCA in patients with inverted papilloma even before a tumor can be observed macroscopically. Two subtypes of this protein were studied, SCCA1 and SCCA2. Further research is needed to establish if they might be useful in detecting squamous cell carcinoma in patients with inverted papilloma (28, 29).
Conclusions
Sinonasal inverted papilloma is a rare tumor that almost always develops unilaterally. Its three main clinical characteristics are the tendency of recurrence, the destructive ability of nearby structures and malignant transformation. The purpose of the surgical treatment is complete resection of the tumor with negative margins and drilling or removing the abnormal underlying bone. Regarding the surgical approach, the endoscopic treatment provides better results than the external approach. Postoperative follow-up is essential in the early detection of recurrence or malignant transformation. Usually, the follow-up consists of systematic flexible endoscopies and clinical examination. In case of doubt regarding its recurrence, MRI is performed. The MRI could be completed with biopsies for a positive diagnosis. Although literature describes possible risk factors for the recurrence and malignant transformation of the inverted papilloma, further research is needed to obtain accurate results.
We wish to highlight the importance of a correct and complete management protocol, which must always include a thorough preoperative evaluation, a correct surgical intervention with the complete removal of the tumor and an aggressive follow-up program. The primary purpose of the intervention is to achieve a disease-free status. If this may be accomplished using an endoscopic approach alone, this situation is preferable. However, if this is impossible, an open or combined approach must always be performed. The main reason for recurrence is considered to be the incomplete removal, but we still consider that further attention must be paid to the evaluation and management of risk factors.
Compliance with Ethical Standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Acknowledgments
All authors have contributed equally to this paper.
Conflicts of Interest
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
References
- Barnes, L. Schneiderian papillomas and nonsalivary glandular neoplasms of the head and neck. Modern Pathology. 2002, 15, 279–297. [Google Scholar] [CrossRef]
- Goyal, P. Advances in endoscopic resection of sinonasal neoplasms. Indian Journal of Otolaryngology and Head & Neck Surgery. 2010, 62, 277–284. [Google Scholar] [CrossRef]
- Myers, E.N.; Fernau, J.L.; Johnson, J.T.; Tabet, J.C.; Barnes, E.L. Management of inverted papilloma. The Laryngoscope. 1990, 100, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Moon, I.J.; Lee, D.Y.; Suh, M.W.; Han, D.H.; Kim, S.T.; Min, Y.G.; Lee, C.H.; Rhee, C.S. Cigarette smoking increases risk of recurrence for sinonasal inverted papilloma. Am J Rhinol Allergy. 2010, 24, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Ungari, C.; Riccardi, E.; Reale, G.; et al. Management and treatment of sinonasal inverted papilloma. Annali di Stomatologia. 2015, 6, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Wassef, S.N.; Batra, P.S.; Barnett, S. Skull base inverted papilloma: a comprehensive review. ISRN Surg. 2012, 2012, 175903. [Google Scholar] [CrossRef]
- Maroldi, R.; Farina, D.; Palvarini, L.; Lombardi, D.; Tomenzoli, D.; Nicolai, P. Magnetic resonance imaging findings of inverted papilloma: differential diagnosis with malignant sinonasal tumours. Am. J. Rhinol. Allergy 2004, 18, 305–310. [Google Scholar] [CrossRef]
- Krouse, J.H. Development of a staging system for inverted papilloma. The Laryngoscope. 2000, 110, 965–968. [Google Scholar] [CrossRef]
- Karkos, P.D.; Fyrmpas, G.; Carrie, S.C.; Swift, A.C. Endoscopic versus open surgical interventions for inverted nasal papilloma: a systematic review. Clin. Otolaryngol. 2006, 31, 499–503. [Google Scholar] [CrossRef]
- Weber, R.K.; Hosemann, W. Comprehensive review on endonasal endoscopic sinus surgery. GMS Curr. Top. Otorhinolaryngol. - Head Neck Surg. 2015, 14. [Google Scholar]
- Oikawa, K.; Furuta, Y.; Nakamaru, Y.; Oridate, N.; Fukuda, S. Preoperative staging and surgical approaches for sinonasal inverted papilloma. Ann. Otol. Rhinol. Laryngol. 2007, 116, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Bhalla, R.K.; Wright, E.D. Predicting the site of attachment of sinonasal inverted papilloma. Rhinology 2009, 47, 345–348. [Google Scholar] [CrossRef]
- Xiao-Ting, W.; Peng, L.; Xiu-Qing, W.; et al. Factors affecting recurrence of sinonasal inverted papilloma. Eur Arch Otorhinolaryngol. 2013, 270, 1349–1353. [Google Scholar] [CrossRef]
- Jardine, A.H.; Davies, G.R.; Birchall, M.A. Recurrence and malignant degeneration of 89 cases of inverted papilloma diagnosed in a non-tertiary referral population between 1975 and 1995: clinical predictors and p53 studies. Clin. Otolaryngol. Allied Sci. 2000, 25, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Suh, K.W.; Facer, G.W.; Devine, K.D.; Weiland, L.H.; Zujko, R.D. Inverting papilloma of the nose and paranasal sinuses. Laryngoscope 1977, 87, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Roh, H.J.; Mun, S.J.; Cho, K.S.; Hong, S.L. Smoking, not human papilloma virus infection, is a risk factor for recurrence of sinonasal inverted papilloma. Am. J. Rhinol. Allergy 2016, 30, 79–82. [Google Scholar] [CrossRef]
- Katori, H.; Nozawa, A.; Tsukuda, M. Histopathological parameters of recurrence and malignant transformation in sinonasal inverted papilloma. Acta Oto-Laryngol. 2006, 126, 214–218. [Google Scholar] [CrossRef]
- Liu, Z. Quantitative studies on nuclear DNA content and morphological features in inverted papillomas of the nasal cavities and paranasal sinuses. Chin. J. Otorhinolaryngol. Head Neck Surg. 1990, 25, 326–382. [Google Scholar]
- Busquets, J.M.; Hwang, P.H. Endoscopic resection of sinonasal inverted papilloma: a meta-analysis. Otolaryngol Head Neck Surg. 2006, 134, 476–482. [Google Scholar] [CrossRef]
- Jurado-Ramos, A.; Jodas, J.G.; Romero, F.R.; Linares, E.A.; Del Castillo, F.M.; Gomariz, E.M.; et al. Endoscopic medial maxillectomy as a procedure of choice to treat inverted papillomas. ACTA Otolaryngol 2009, 129, 1018–1025. [Google Scholar] [CrossRef]
- Pim, D.; Collins, M.; Banks, L. Human papillomavirus type 16 E5 gene stimulates the transforming activity of the epidermal growth factor receptor. Oncogene. 1992, 7, 27–32. [Google Scholar]
- Zhao, R.W.; Guo, Z.Q.; Zhang, R.X. Human papillomavirus infection and the malignant transformation of sinonasal inverted papilloma: A meta-analysis. J. Clin. Virol. 2016, 79, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Liang, Q.Z.; Li, D.Z.; Wang, X.L.; Huang, H.; Xu, Z.G.; Wu, Y.H. Survival outcome of squamous cell carcinoma arising from sinonasal inverted papilloma. Chinese Medical Journal. 2015, 128, 2457–2461. [Google Scholar] [CrossRef]
- Stanciu, A.E.; Zamfir-Chiru-Anton, A.; Stanciu, M.M.; Popescu, C.R.; Gheorghe, D.C. Serum Level of Matrix Metalloproteinase-9 in Patients with Head and Neck Squamous Cell Carcinoma. Clin Lab. 2016, 62, 1569–1574. [Google Scholar] [CrossRef]
- Kim, D.Y.; Hong, S.L.; Lee, C.H.; Jin, H.R.; Kang, J.M.; Lee, B.J.; et al. Inverted papilloma of the nasal cavity and paranasal sinuses: a Korean multicenter study. Laryngoscope. 2012, 122, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Paunica, M.; Manole, A.; Motofei, C.; Tanase, G.L. The Globalization in the actual Context of the European Union Economy. Proc. Int. Conf. Bus. Excell. 2018, 12, 739–750. [Google Scholar] [CrossRef]
- Ardeleanu, V.; Frincu, L.L.; Nechita, A.; Georgescu, C. Nuclear morphometry and proliferative activity evaluation in the gastrointestinal stromal tumors. Rom J Morphol Embryol. 2014, 55, 319–323. [Google Scholar]
- Popa, L.; Petrescu, S.; Panea, C.A. Treatment principles in the management of early coagulopathy following rtPA therapy – discussion based on a particular case report. Cerebrovasc. Dis. 2018, 45, 182–182. [Google Scholar]
- Yamashita, Y.; Uehara, T.; Hasegawa, M.; et al. Squamous cell carcinoma antigen as a diagnostic marker of nasal inverted papilloma. Am. J. Rhinol. Allergy 2016, 30, 122–127. [Google Scholar] [CrossRef]
authors 2019 Alexandru Meius, Teodora Ghindea, Catalina Pietrosanu, Irina Ionita, Daniel Timofte, Cornelia Nitipir, Laura Mazilu, Andreea Rusescu, Silviu Pituru, Razvan Hainarosie