The Psychosocial Impact of Vaginal Delivery and Cesarean Section in Primiparous Women
Highlights
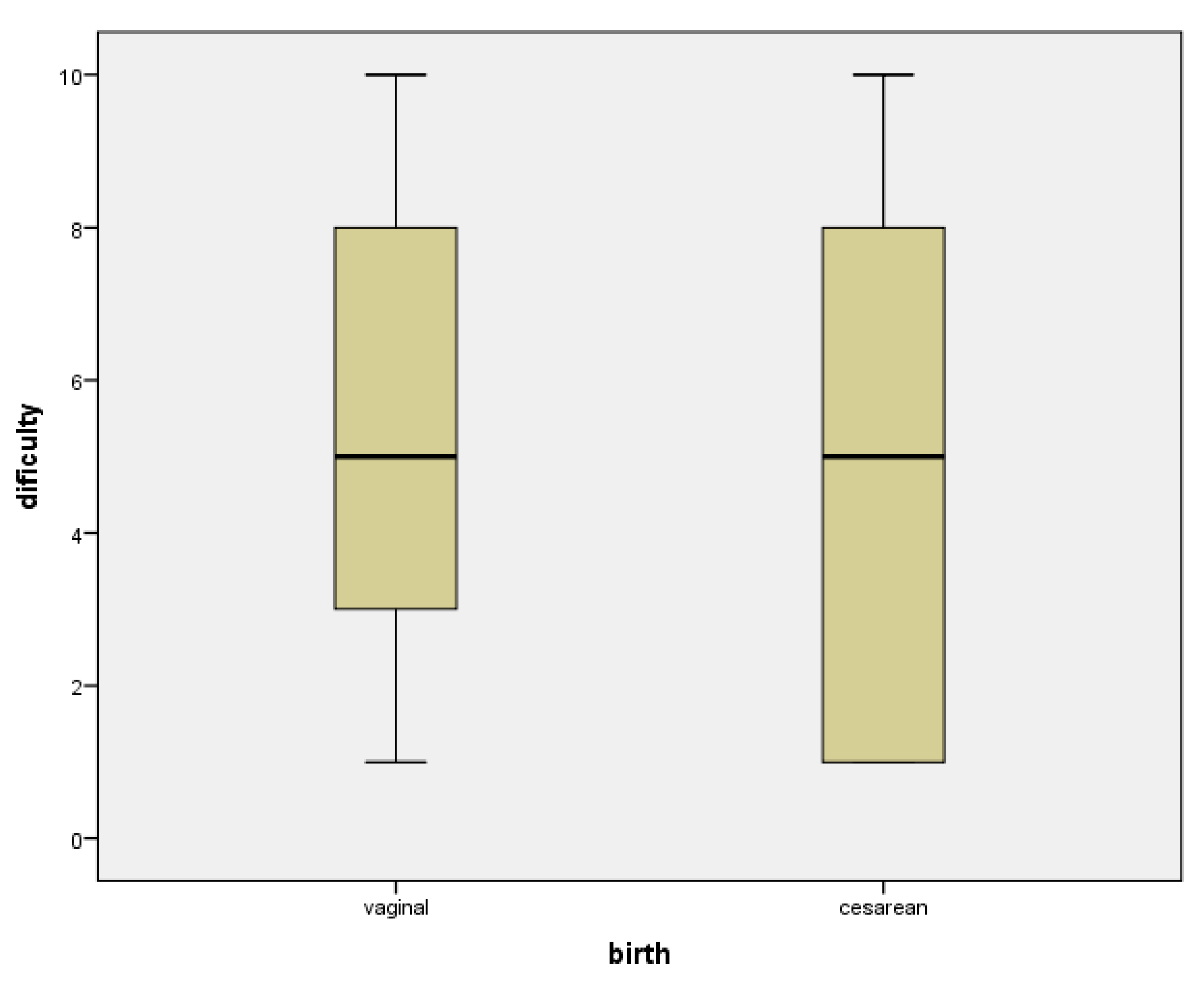
- Majority of the patients didn’t find the birth experience difficult, irrespective of the method of delivery.
- Lactation and taking care of the baby are also not impacted by the method of delivery.
Abstract
:Highlights
- ✓
- Majority of the patients didn’t find the birth experience difficult, irrespective of the method of delivery.
- ✓
- Lactation and taking care of the baby are also not impacted by the method of delivery.
Abstract
Introduction
Materials and Methods
Results
| Group characteristics | All patients | Vaginal birth | Cesarean section |
|---|---|---|---|
| Maternal age (years) | 27.69 (min 17, max 42, std dev 5.145) | 25.84 (min 17, max 36, std dev 5.212) | 25.84 (min 17, max 42, std dev 414.58) |
| Gestational age at delivery (weeks) | 38.36(min 34, max 41, std dev 1.508) | 38.42(min 34, max 41, std dev 1.810) | 38.35(min 35, max 41, std dev 1.397) |
| Fetal birth weight | 3036.08 (min 1850, max 3980, std dev 424.88) | 2912.11 (min 1980, max 3400, std dev 414.580) | 3078.91 (min 1850, max 3980, std dev 421.799) |
Discussions
Conclusions
References
- Nystedt, A.; Hildingsson, I. Women’s and men’s negative experience of child birth-A cross-sectional survey. Women Birth 2017, S1871-5192(17)30056-2. [Google Scholar] [CrossRef] [PubMed]
- Kingsbury, A.M.; Plotnikova, M.; Najman, J.M. Commonly occurring adverse birth outcomes and maternal depression: a longitudinal study. Public Health 2018, 155, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Nagl, M.; Linde, K.; Stepan, H.; Kersting, A. Obesity and anxiety during pregnancy and postpartum: A systematic review. J Affect Disord 2015, 186, 293–305. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.; Paranjothy, S.; James, D. National cross- sectional survey to determine whether the decision to delivery interval is critical in emergency caesarean section. BMJ. 2004, 328, 665. [Google Scholar] [CrossRef] [PubMed]
- Sénat, M.V.; Sentilhes, L.; Battut, A.; Benhamou, D.; Bydlowski, S.; Chantry, A.; Deffieux, X.; Diers, F.; Doret, M.; Ducroux-Schouwey, C.; Fuchs, F.; Gascoin, G.; Lebot, C.; Marcellin, L.; Plu-Bureau, G.; Raccah-Tebeka, B.; Simon, E.; Bréart, G.; Marpeau, L. Postpartum practice: guidelines for clinical practice from the French College of Gynaecologists and Obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol. 2016, 202, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, S.J.; Boyce, P.M.; Hickey, A.R.; Morris- Yatees, A.D.; Harris, M.G. Obstetric risk factors for postnatal depression in urban and rural community samples. Aust N Z J Psychiatry. 2001, 35, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Glazener, C.M.; Abdalla, M.; Stroud, P.; Naji, S.; Templeton, A.; Russell, I.T. Postnatal maternal morbidity: extent, causes, prevention and treatment. Br J Obstet Gynaecol. 1995, 102, 282–7. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.; Astbury, J.; Smith, A. Adverse psychological impact of operative obstetric interventions: a prospective longitudinal study. Aust N Z J Psychiatry. 1997, 31, 728–38. [Google Scholar] [CrossRef] [PubMed]
- Boyce, P.M.; Todd, A.L. Increased risk of postnatal depression after emergency caesarean section. Med J Aust. 1992, 157, 172–4. [Google Scholar] [CrossRef] [PubMed]
- Culp, R.E.; Osofsky, H.J. Effects of cesarean delivery on parental depression, marital adjustment, and mother- infant interaction. Birth. 1989, 16, 53–7. [Google Scholar] [CrossRef] [PubMed]
- Saisto, T.; Salmela-Aro, K.; Nurmi, J.E.; Halmesmaki, E. Psychosocial predictors of disappointment with delivery and puerperal depression. A longitudinal study. Acta Obstet Gynecol Scand. 2001, 80, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Boero, G.; Biggio, F.; Pisu, M.G.; Locci, V.; Porcu, P.; Serra, M. Combined effect of gestational stress and postpartum stress on maternal care in rats. Physiol Behav 2018, 184, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Skinner, E.M.; Barnett, B.; Dietz, H.P. Psychological consequences of pelvic floor trauma following vaginal birth: a qualitative study from two Australian tertiary maternity units. Arch Womens Ment Health. 2017. [CrossRef] [PubMed]
- Pereira, T.R.C.; Souza, F.G.; Beleza, A.C.S. Implications of pain in functional activities in immediate postpartum period according to the mode of delivery and parity: an observational study. Braz J Phys Ther 2017, 21, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Bălălău, D.O.; Sima, R.M.; Bacalbașa, N.; Pleș, L.; Stănescu, A.D. Emergency peripartum hysterectomy, physical and mental consequences: a 6-year study. J Mind Med Sci. 2016, 3, 65–70. [Google Scholar] [CrossRef]
- Holden, L.; Hockey, R.; Ware, R.S.; Lee, C. Mental health-related quality of life and the timing of motherhood: a 16-year longitudinal study of a national cohort of young Australian women. Qual Life Res. 2018. [CrossRef] [PubMed]
- Triviño-Juárez, J.M.; Romero-Ayuso, D.; Nieto-Pereda, B.; Forjaz, M.J.; Criado-Álvarez, J.J.; Arruti-Sevilla, B.; Avilés-Gamez, B.; Oliver-Barrecheguren, C.; Mellizo-Díaz, S.; Soto-Lucía, C.; Plá-Mestre, R. Health related quality of life of women at the sixth week and sixth month postpartum by mode of birth. Women Birth. 2017, 30, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Karlström, A. Women’s self-reported experience of unplanned caesarean section: Results of a Swedish study. Midwifery 2017, 50, 253–8. [Google Scholar] [CrossRef] [PubMed]
- Bălălău, D.O.; Sima, R.M.; Bacalbașa, N.; Banu, P.; Bălălău, C.; Pleș, L.; Stănescu, A.D. High-grade cervical dysplasia in pregnancy–psychological and medical challenges. J Mind Med Sci. 2017, 4, 24–30. [Google Scholar] [CrossRef]
- Amorim, M.; Silva, S.; Kelly-Irving, M.; Alves, E. Quality of life among parents of preterm infants: a scoping review. Qual Life Res. 2017. [CrossRef] [PubMed]
- Ionescu, C.A.; Ples, L.; Banacu, M.; Poenaru, E.; Panaitescu, E.; Traian Dimitriu, M.C. Present tendencies of elective caesarean delivery in Romania: Geographic, social and economic factors. J Pak Med Assoc. 2017, 67, 1248–53. [Google Scholar] [PubMed]
© 2018 by the author. 2018 Liana Pleș, Romina M. Sima, Delia Carp, Camelia Alexăndroaia, Denisa O. Bălălău, Anca D. Stănescu, Octavian G. Olaru
Share and Cite
Pleș, L.; Sima, R.M.; Carp, D.; Alexăndroaia, C.; Bălălău, D.O.; Stănescu, A.D.; Olaru, O.G. The Psychosocial Impact of Vaginal Delivery and Cesarean Section in Primiparous Women. J. Mind Med. Sci. 2018, 5, 70-74. https://doi.org/10.22543/7674.51.P7074
Pleș L, Sima RM, Carp D, Alexăndroaia C, Bălălău DO, Stănescu AD, Olaru OG. The Psychosocial Impact of Vaginal Delivery and Cesarean Section in Primiparous Women. Journal of Mind and Medical Sciences. 2018; 5(1):70-74. https://doi.org/10.22543/7674.51.P7074
Chicago/Turabian StylePleș, Liana, Romina M. Sima, Delia Carp, Camelia Alexăndroaia, Denisa O. Bălălău, Anca D. Stănescu, and Octavian G. Olaru. 2018. "The Psychosocial Impact of Vaginal Delivery and Cesarean Section in Primiparous Women" Journal of Mind and Medical Sciences 5, no. 1: 70-74. https://doi.org/10.22543/7674.51.P7074
APA StylePleș, L., Sima, R. M., Carp, D., Alexăndroaia, C., Bălălău, D. O., Stănescu, A. D., & Olaru, O. G. (2018). The Psychosocial Impact of Vaginal Delivery and Cesarean Section in Primiparous Women. Journal of Mind and Medical Sciences, 5(1), 70-74. https://doi.org/10.22543/7674.51.P7074



