1. Introduction
In-hospital cardiac arrest (IHCA) refers to an event in which a patient has spontaneous circulation at the time of admission but subsequently suffers cardiac arrest during hospitalization. According to the internationally recognized Utstein criteria for standardized reporting of cardiac arrest, IHCA is clearly defined as a patient with spontaneous circulation or measurable vital signs at the time of admission, who experiences a cardiac arrest during the subsequent hospitalization [
1]. More than 290,000 adults in the United States suffer in-hospital cardiac arrest each year. According to the American Heart Association (AHA) Get With The Guidelines-Resuscitation (GWTG-R), the incidence of IHCA from 2008 to 2017 was 9–10 events per thousand people [
2]. In 2015, the AHA published an expert consensus that strengthened hospitals’ attention to unexpected in-hospital cardiac arrest and proposed the concept of the IHCA survival chain [
3]. In 2019, the AHA further emphasized the early identification of IHCA risks, and that prevention is the key; it is recommended that hospitalized adults can use the early warning scoring system to identify risk factors, which can effectively prevent the deterioration of cardiac arrest. A study by Hodgetts et al. [
4] showed that 1/3 to 2/3 of IHCAs are avoidable. Many scholars have also found that signs of deterioration in physiological indicators can be traced several hours before IHCA occurs [
5,
6,
7], indicating that there are signs to be found before IHCA occurs. However, only about a quarter of the cases can be detected in advance clinically; if high-risk patients can be identified early and given appropriate treatment in a timely manner, the occurrence of death or serious adverse events caused by IHCA can be reduced or avoided [
8,
9].
Emergency IHCA refers to a patient who enters the emergency department for triage and has measured vital signs, but suffers unexpected cardiac arrest during his or her stay in the emergency department and requires immediate emergency treatment to save his or her life. TPR (2019) statistics show that the incidence of IHCA in the emergency department is approximately 6.4%. The emergency department is the first line of defense for the hospital to deal with critically ill patients. It is responsible for responding to the rapid changes in the condition of the patients. The sources of emergency patients are extremely diverse, ranging from mild discomfort to acute and critical illness. It is worth noting that those patients with potential cardiovascular disease or respiratory problems are at a greater risk of developing IHCA during hospitalization [
10]. This variable and unpredictable condition poses a huge challenge to medical personnel in responding to emergencies, further emphasizing the importance of early diagnosis and treatment. However, most of the current domestic and international literature on IHCA patient analysis data focuses on wards or intensive care units, and rarely explores the monitoring of unexpected cardiac arrest in the emergency room. The emergency department has a large patient flow, a high turnover rate, and patients of varying severity, usually with urgent conditions. Therefore, emergency medical personnel need to quickly assess, understand, and treat the patients in a short period of time, and are subject to high judgment pressure and decision-making risks. When judgment or decision-making is biased, once an unexpected cardiac arrest occurs, in addition to facing changes in the patient’s condition, prognosis, and family members’ accountability, there is a blow to the morale of team members and satisfaction with the quality of hospital care, and even subsequent medical treatment disputes and other pressures. Investigations in Taiwan [
1] and South Korea [
11] have found that emergency department congestion is associated with IHCA. It is even more important to identify high-risk factors that can predict IHCA, so that busy emergency medical personnel on the front line can grasp and identify IHCA early and efficiently. For high-risk patients, immediate intervention should be initiated to reduce the incidence of IHCA [
12,
13,
14,
15,
16,
17].
In the past, some hospitals have analyzed the causes of IHCA through statistics, as reviewed below. Tan and Leong [
18] used the Utstein survey to investigate emergency IHCA in Singapore and found that 43.4% of IHCAs were related to heart problems. If defibrillation and effective CPR were given to treat arrhythmias as soon as possible, the survival rate would be 70.8%. Topjian et al. [
19] pointed out that if fatal arrhythmias can be identified early and treated promptly and correctly, the risk of IHCA can be reduced. Wang et al. [
20] counted the causes of IHCA in 21 hospitals of different levels in Taiwan and found that 35.7% were due to fatal arrhythmia, 21.3% were due to myocardial infarction/ischemia, and 14.9% were due to respiratory failure. Thorén et al. [
21] found that early detection of the type of electrocardiographic changes that can be corrected can predict 30-day survival based on a statistical analysis of the Swedish Registry for Cardiopulmonary Resuscitation (SRCR) from 2008 to 2017. In [
22,
23], many innovative and effective prevention methods for IHCA are collated and analyzed in detail.
In recent years, artificial intelligence has been widely used in auxiliary diagnosis and prediction in the medical field [
24,
25,
26]. To develop a predictive model for identifying patients at high risk of IHCA in the emergency department, this study used Power BI and decision tree to analyze the clinical data of emergency patients and evaluate the key influencing factors of IHCA. The research data was collected from Taipei United Hospital in Taiwan. Medical records of IHCA cases that occurred in the emergency department were collected. The data sources included the Hospital Information System (HIS), the Nursing Information System (NIS), and the unexpected in-hospital cardiac arrest abnormal event reporting form. At the same time, patients who were admitted to the intensive care unit after the emergency but did not develop IHCA were collected as a control group for comparative analysis. The data we used were unexpected cardiac arrest events reported in the emergency department from 1 January 2019 to 31 December 2020. A total of 140 IHCA cases and 100 patients transferred to the intensive care unit (ICU) from the emergency department were initially included in the medical records. After excluding duplicate records and cases with missing or incomplete data, 130 IHCA cases and 96 patients transferred to the ICU from the emergency department were included for analysis. In addition, the research subjects must meet the following conditions: have measurable vital signs when entering the emergency room and have received emergency treatment during the emergency room; the final emergency outcome of the research group (IHCA group) is death, and the final emergency outcome of the control group is admission to the intensive care unit; the research subjects must be 20 years old or older. This study excluded OHCA cases, trauma patients, patients with terminal cancer or non-cancer diseases confirmed by medical records who chose palliative care and signed the Do Not Resuscitation (DNR) form, and pregnant women. Finally, we used the Power BI visual analysis platform and binary decision tree model to construct a data-driven risk prediction tool. Power BI analysis successfully presented the dynamic ranking of influencing factors, and the decision tree prediction model showed excellent performance, with an accuracy of 91%, a recall rate of 89%, an F1-score of 89%, and an overall accuracy of 100%.
The rest of this study is as follows.
Section 2 introduces materials.
Section 3 shows the proposed mehod.
Section 4 gives experimental results and discussion. The conclusion is in
Section 5.
2. Materials
This study collected data from patients who had experienced IHCA in the emergency department of Taipei City United Hospital (Peace, Ren’ai, Zhongxiao, Zhongxing, and Yangming branches) across five campuses. Data sources included the Hospital Information System (HIS), the Nursing Information System (NIS), and the Unexpected In-Hospital Cardiac Arrest Event Report Form. A control group was also collected with data collected on patients who had their last emergency department visit to the intensive care unit. All patient data are approved by the Ethics Committee of Taipei City Hospital (protocol code TCHIRB-11011003-E and date of approval: 6 December 2021).
We originally included 140 IHCA medical records and 100 emergency patients transferred to the ICU as the control group, but after removing duplicates and missing or incomplete data, 130 IHCA and 96 emergency patients transferred to the ICU were finally included. These data types include numerical and fractional types:
1. Numeric type: variables can be integers or floating point numbers. For example, age, breathing rate, heart rate, etc., are all integer types; height, weight, systolic blood pressure, diastolic blood pressure, etc., are all floating-point numbers.
2. Category type: you can only choose variables from a limited number of options, such as gender, whether you have a chronic disease like heart disease, etc.
Personal characteristic variables include age, gender, smoking, drinking, and body mass index (BMI). Physiological measurements include temperature, pulse rates, respiratory rates, systolic pressure, and other physiological parameters.
3. Proposed Method
The purpose of this study was to identify risk factors associated with the prediction of IHCA. After literature review and analysis, possible risk factors were selected to collect data. The data of patients who were not IHCA and whose final outcome was transfer from the emergency department to the intensive care unit were used as the control group for data registration. The associated modules compiled from the collected data include personal variables, NEWS scores, test indicators, Charlson comorbidity index scale, and possible causes of IHCA for decision analysis.
3.1. Power BI Method
When using Power BI to analyze the key influencing factors of IHCA in hospitalized patients, the analysis process starts with the data import and organization stage. This study used Power Query to integrate various clinical data, including patients’ personal characteristic variables, NEWS categories, and CCI comorbidity categories. After the data was imported, it was first cleaned, missing values and abnormal values were screened and processed, and data in different formats were converted to ensure the integrity and consistency of data quality. This process is crucial for subsequent analysis because high-quality data can provide a solid foundation for research. After completing the data cleaning, we further used Power Pivot to build a data model, that is, using the patient ID as the primary key, linking data tables from different sources to each other, and building a unified data structure to establish a model.
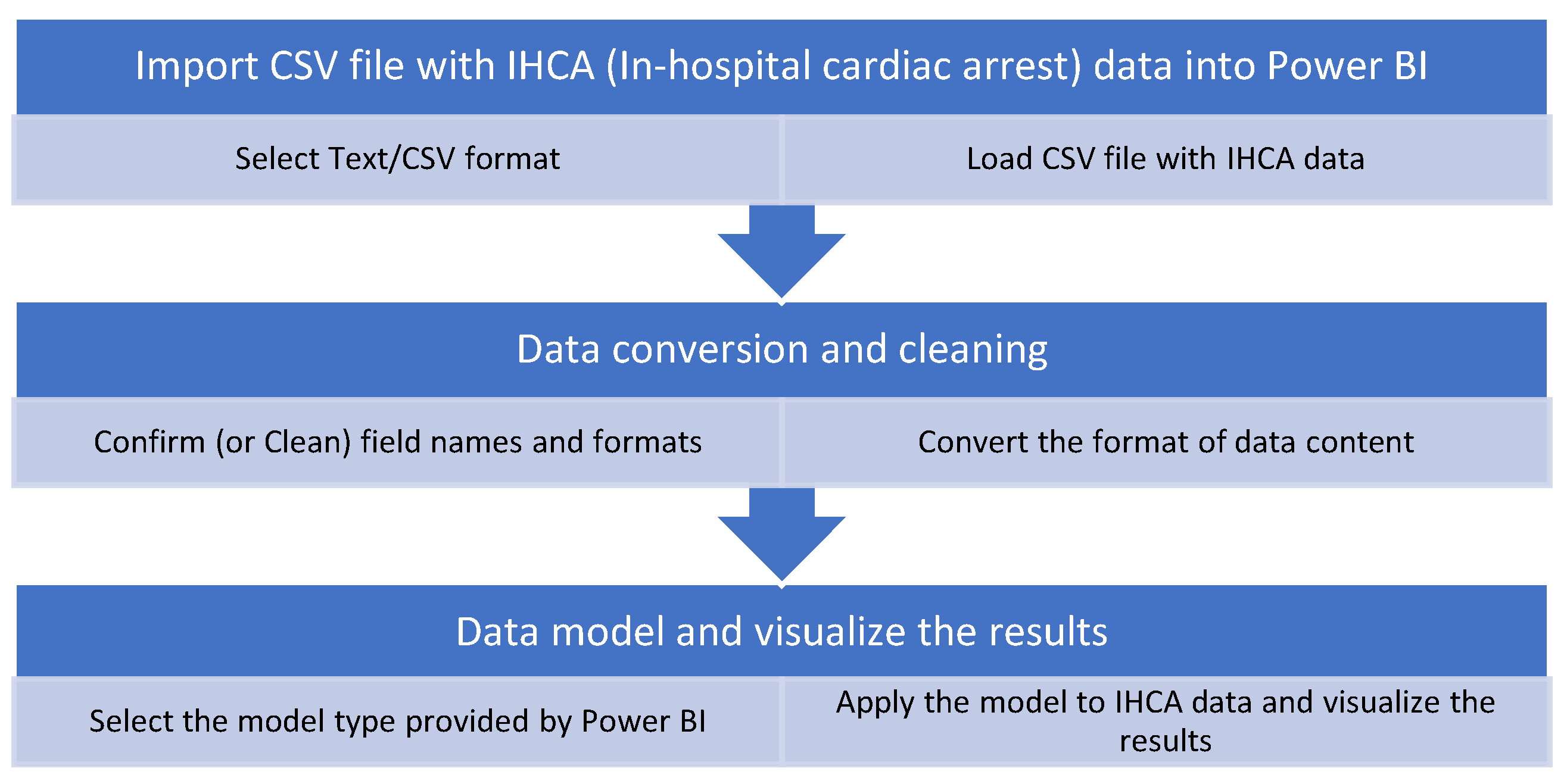
After entering the visual analysis stage, the study used Power View to create multi-dimensional analysis charts to achieve intuitive presentation of data. When analyzing key influencing factors, a variety of correlation analysis charts were produced to focus on identifying variables that have a significant impact on the occurrence of IHCA. In this process, we paid special attention to the correlation strength between the predicted variables and the occurrence of IHCA, and by exploring the interactive relationship between the variables, we further analyzed the significant correlation variable combinations that led to the occurrence of IHCA. The research flowchart using Power BI is shown in
Figure 1.
3.2. Decision Tree Method
CART (Classification and Regression Trees) is an important algorithm. Compared with other decision tree algorithms, CART is unique in that it can handle both classification and regression problems. In classification problems, CART uses the Gini coefficient as the criterion for node splitting; in regression problems, it uses the mean square error as the evaluation criterion. This flexibility enables CART to adapt to various types of data analysis tasks. The CART algorithm works in three main stages: tree generation, pruning, and tree selection. During the generation stage, the algorithm constructs a decision tree using a recursive binary partitioning method. Each split selects the features and split points that best reduce impurity. The Gini coefficient is an important metric for measuring node impurity; a lower Gini coefficient indicates better class purity. To prevent overfitting, the CART algorithm employs cost complexity pruning. Research has shown that pruning is achieved by minimizing the objective function Cα(T) = C(T) + α|T|, where C(T) is the error of tree T, |T| is the number of terminal nodes in the tree, and α is the complexity parameter [
22]. This method achieves a good balance between model complexity and predictive accuracy. The steps of the CART decision tree algorithm are as follows:
Step 1: Calculate the Gini coefficient;
Step 2: Select the optimal split point;
Step 3: Create nodes and split the data;
Step 4: Recursively build the tree;
Step 5: Determine the decision rule;
Step 6: Prune the decision tree.
Decision trees can establish concise and efficient classification prediction models through training data, and can be flexibly applied to the prediction of new data. Their special feature is that they can process multiple data types at the same time, showing excellent adaptability. Podgorelec et al. [
22] stated that CART has become an important tool for medical diagnosis and prediction because of its excellent interpretability, accuracy, and easy-to-understand features, which enable doctors to better understand and trust the algorithm’s diagnostic recommendations.
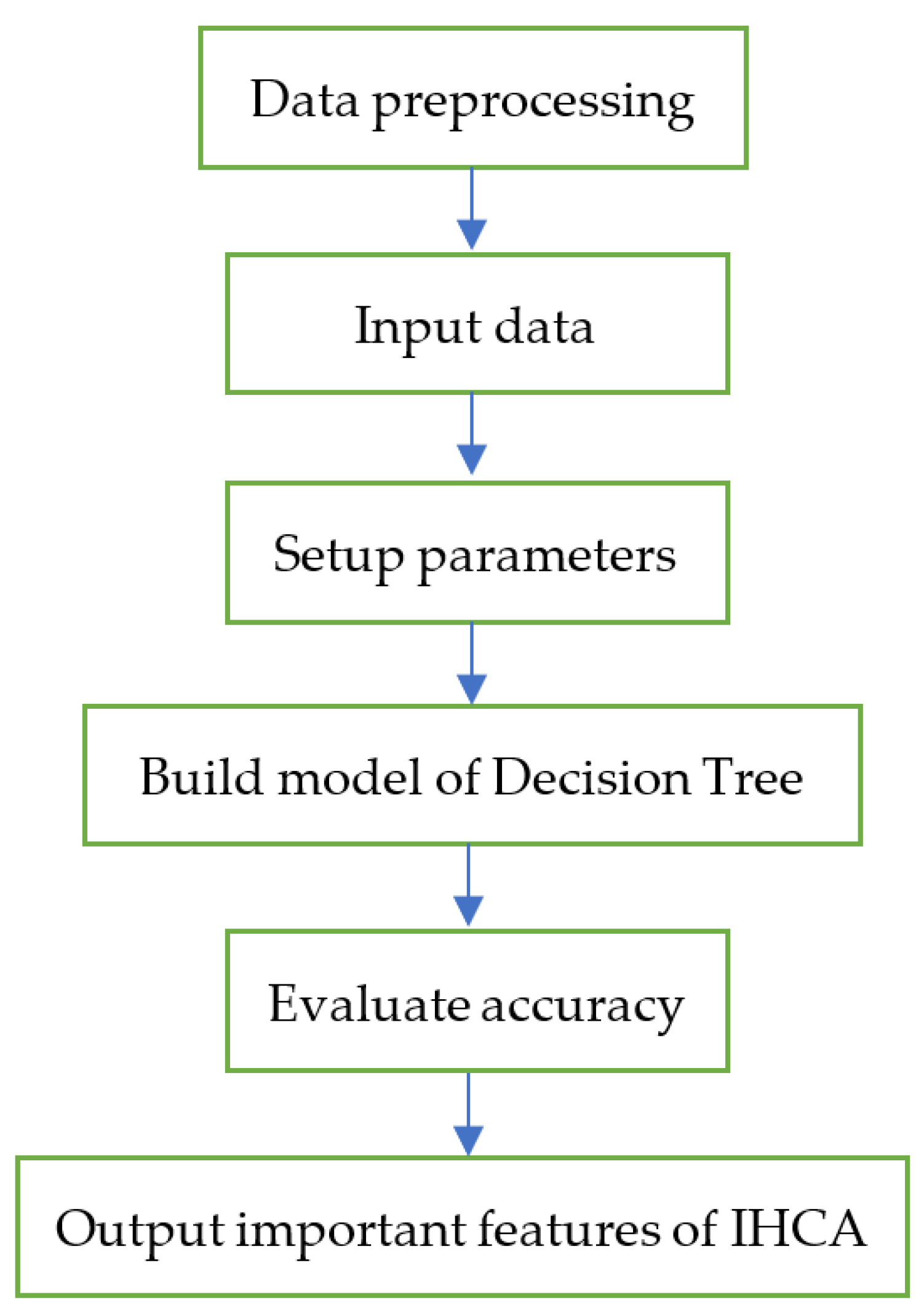
As shown in
Figure 2, the construction steps of the decision tree and the research flowchart of this study are as follows:
Step 1. The dataset of this study contains two main data types: one is numerical variables, including integer indicators such as age, respiratory rate, and heart rate, as well as precise measurements that need to be expressed in floating-point numbers, such as height, weight, and blood pressure data (including systolic and diastolic blood pressure); the other is categorical variables, which have clear classification characteristics and their values can only be selected from preset options, such as gender distinction and indicators for determining whether or not a person suffers from chronic diseases such as heart disease. Therefore, this stage mainly converts the patient’s original clinical data into a standard format that can be processed by the decision tree algorithm, including the standardization of numerical data such as physiological indicators, and the coding conversion of categorical data such as gender and disease status, to ensure that all data can be correctly identified and used by the algorithm.
Step 2. Treat each transformed variable as a potential decision node. These nodes may be various physiological indicators, laboratory test values, medical history data, or demographic characteristics, etc. Each node may become a key point for future decision tree branching.
Step 3. The system will comprehensively traverse all possible segmentation methods for each decision node. During this process, the algorithm will calculate the information gain or Gini coefficient of each potential segmentation point to evaluate the effects of different segmentation methods and ultimately select the optimal segmentation point that can maximize the classification effect.
Step 4. Divide the dataset into two subsets according to this split point, that is, generate a left subtree and a right subtree. The goal of this split process is to make each subset have a higher category purity, thereby improving the overall prediction accuracy.
Step 5. The system will repeat the aforementioned split evaluation process for each newly generated subtree. This recursive tree-building process will continue until a specific stopping condition is reached, such as the node reaching the preset purity requirement, the number of samples being less than the minimum limit, or the depth of the tree reaching the preset value. The whole process is carried out through continuous binary segmentation, and finally a hierarchical decision-making structure that can effectively predict the risk of IHCA is established.
4. Experimental Results and Discussion
The original data collection schedule for this study was to start in January 2018, but the medical records were not yet digitized and locked in that year and could not be obtained; therefore, the collection time was changed to cases of unexpected cardiac arrest reported in the emergency department from 1 January 2019 to 31 December 2020. A total of 140 IHCA medical records and 100 emergency department patients transferred to the intensive care unit were included. Duplicates, missing data, and incomplete data were removed, and finally 130 IHCAs and 96 patients transferred from the emergency department to the ICU were included for analysis. Power BI Desktop 2.138.782.0 and decision tree Python C5.0 were used.
4.1. Results of Power BI Method
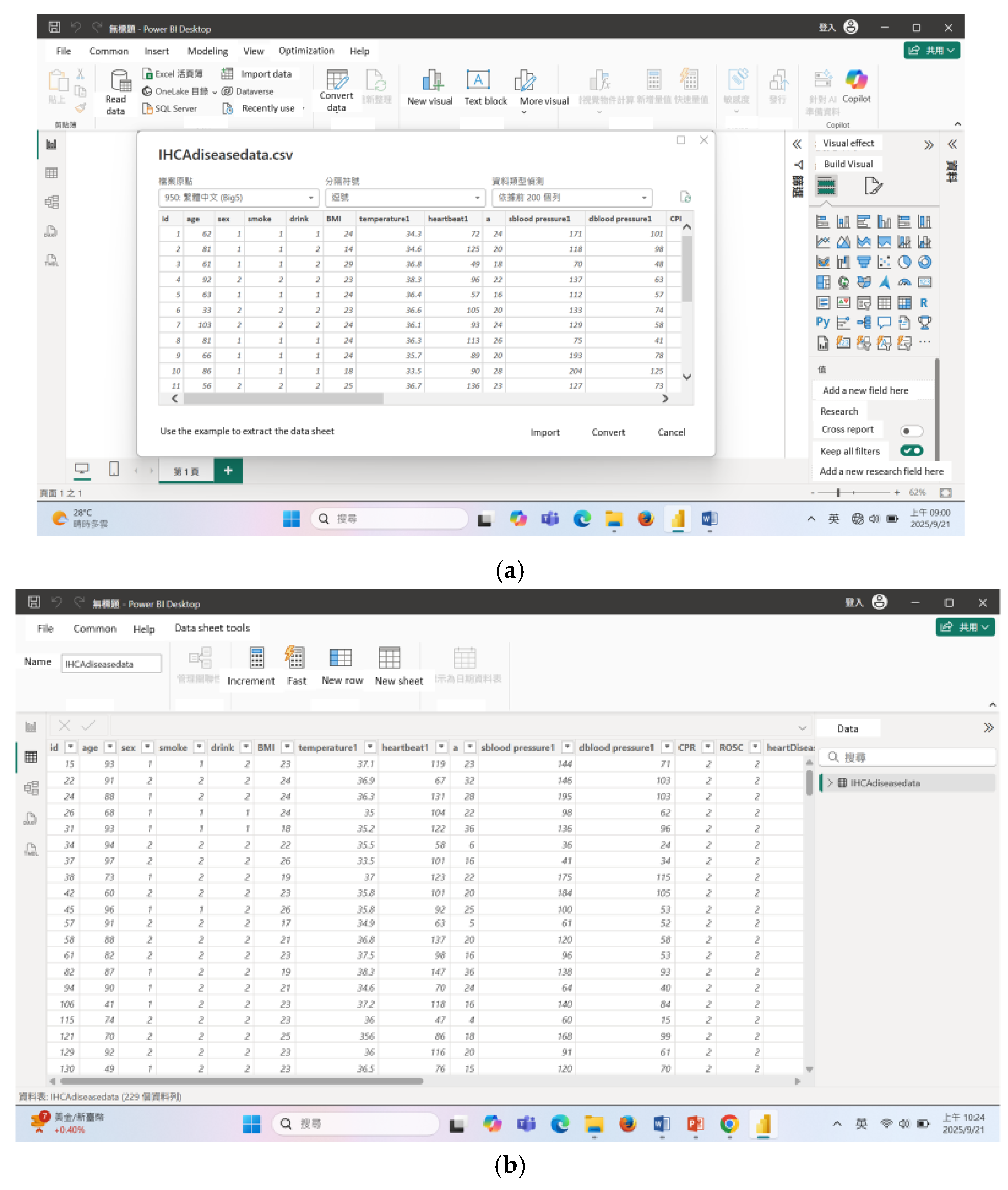
To obtain the results of using the Power BI method in
Section 3.1, we first imported IHCA data and used Power Query to integrate various clinical data, including patients’ personal characteristic variables, NEWS categories, and CCI comorbidity categories. After the data was imported, missing values and abnormal values were screened and processed. Moreover, data in different formats were converted to ensure the integrity and consistency of data quality as shown in
Figure 3. Then, we used Power Pivot to build a data model, that is, using the patient ID as the primary key, linking data tables from different sources to each other, and building a unified data structure to establish a model.
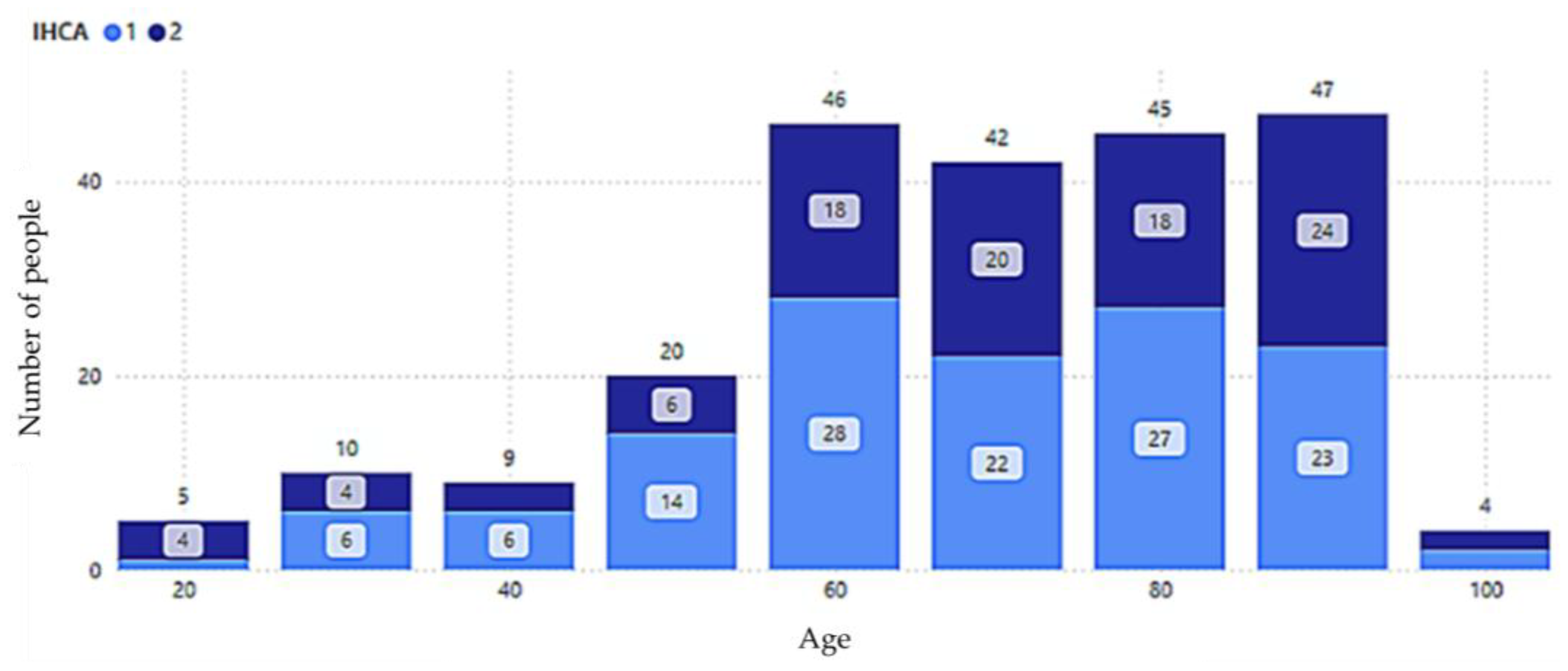
Power BI analysis found that age and BMI were key influencing factors closely related to the occurrence of IHCA among personal variables. With aging, the natural deterioration of cardiovascular system function, the accumulation of underlying diseases (such as hypertension, diabetes, or chronic heart disease), and the decreased tolerance to acute stress events may increase the risk of IHCA. The results in
Figure 4 show that there is a certain positive correlation between age increase and the incidence of IHCA, especially in the elderly population, where this effect is particularly evident. As shown in
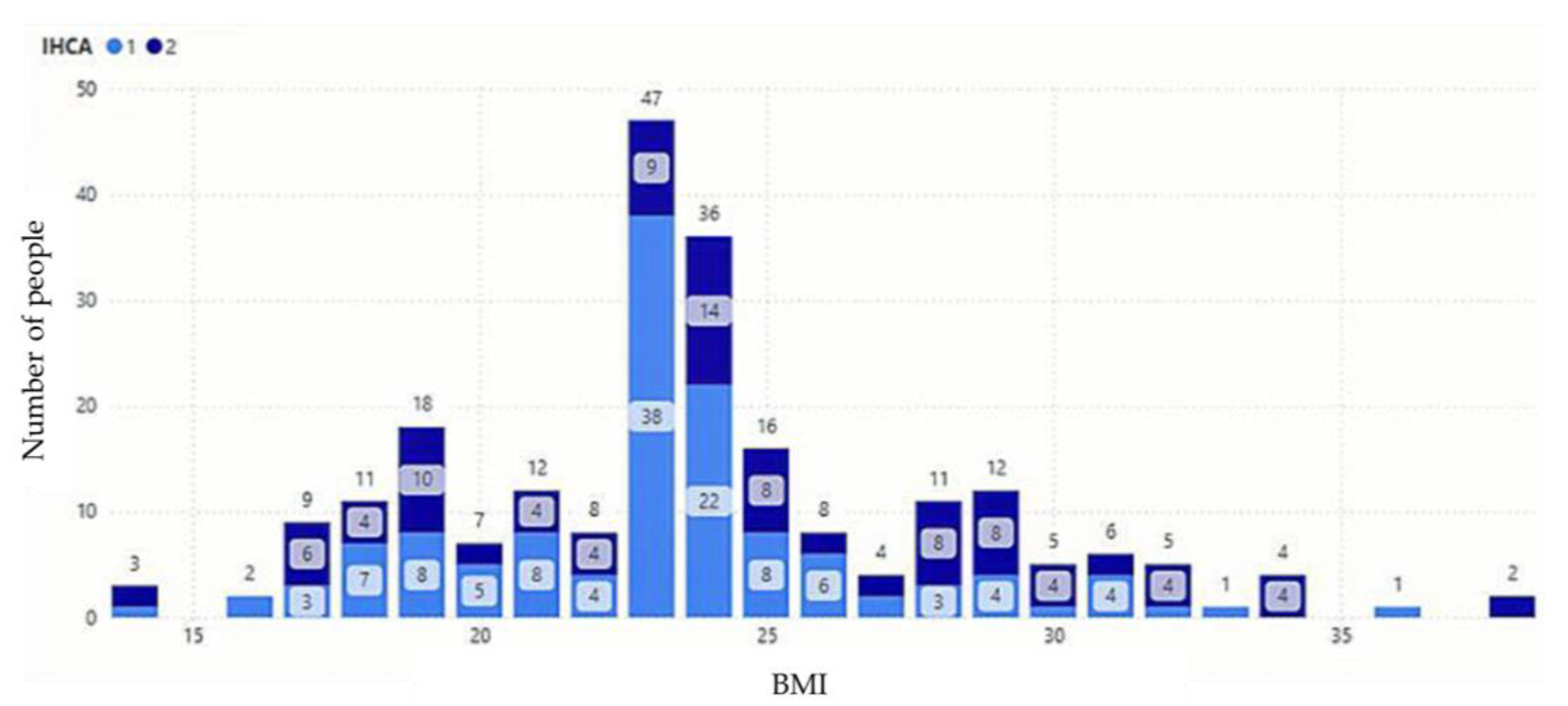
Figure 5, it was found that differences in BMI may indeed affect the prognosis of the emergency treatment process by analyzing the relationship between BMI value and IHCA.
Physiological test indicators, Charlson comorbidity index scale, and possible causes of IHCA were found to be the key factors affecting the occurrence of IHCA, namely the execution of CPR, the state of ROSC spontaneous circulation, and chronic obstructive pulmonary disease.
The impact of CPR and IHCA: First, timely and high-quality CPR can maintain the patient’s basic circulation and oxygen supply, which is crucial to improving survival rate; secondly, the quality of CPR will directly affect whether ROSC can be successfully achieved, including compression depth. Factors such as rate and complete rebound will affect the effect of resuscitation; in addition, continuous CPR can reduce ischemic damage to important organs, especially the protection of the brain and heart. In addition, the implementation of CPR may cause complications. Symptoms such as rib fractures or internal organ damage may affect the patient’s recovery process; finally, the quality of teamwork and communication during CPR, as well as whether the cause of cardiac arrest can be accurately identified and treated, will affect the overall effectiveness of resuscitation (Kagawa et al., 2010 [
27]); therefore, high-quality CPR can not only increase the survival chance of IHCA patients, but also improve their prognosis quality.
Figure 6 analyzes the impact of CPR intervention on the survival rate of IHCA patients. The data show that 81 patients died among those who did not receive CPR, which highlights the importance of timely cardiopulmonary resuscitation. In contrast, 81 patients died among those who received CPR. Although 48 people still died, 99 people survived successfully, indicating that CPR can indeed effectively improve the survival rate of IHCA patients. Such results also suggest the complexity of factors affecting the prognosis of IHCA. In addition to the implementation of CPR, factors such as the severity of the disease, emergency response time, and the accessibility of medical resources may be important variables affecting the patient’s final prognosis.
ROSC has a significant impact on IHCA patients. First, the time to achieve ROSC is directly related to the patient’s chance of survival. The earlier the spontaneous circulation is restored, the higher the survival rate. Second, the length of ROSC will affect the patient’s neurological prognosis. The earlier the ROSC is achieved, the better the patient’s chance of survival. ROSC can reduce brain damage caused by hypoxia. Furthermore, even if ROSC is achieved, the patient’s organs may still be damaged to varying degrees due to previous ischemia and reperfusion, and need to be closely monitored. Finally, the patient’s condition after ROSC will determine the subsequent survival. In terms of treatment direction, the medical team needs to immediately evaluate the cause of cardiac arrest and adjust the treatment strategy based on the patient’s vital signs, including considering whether to perform special treatments such as target temperature management. Therefore, ROSC is not only a key indicator of IHCA survival, but also an important factor affecting prognosis and treatment decisions. As shown in
Figure 7, when ROSC did not occur, 46 patients with in-hospital cardiac arrest died, and when ROSC occurred, 83 patients with in-hospital cardiac arrest died and 99 patients survived. This suggests that the occurrence of spontaneous circulation restoration has a significant impact on patient survival, but even if spontaneous circulation is successfully restored, a considerable number of patients may still die.
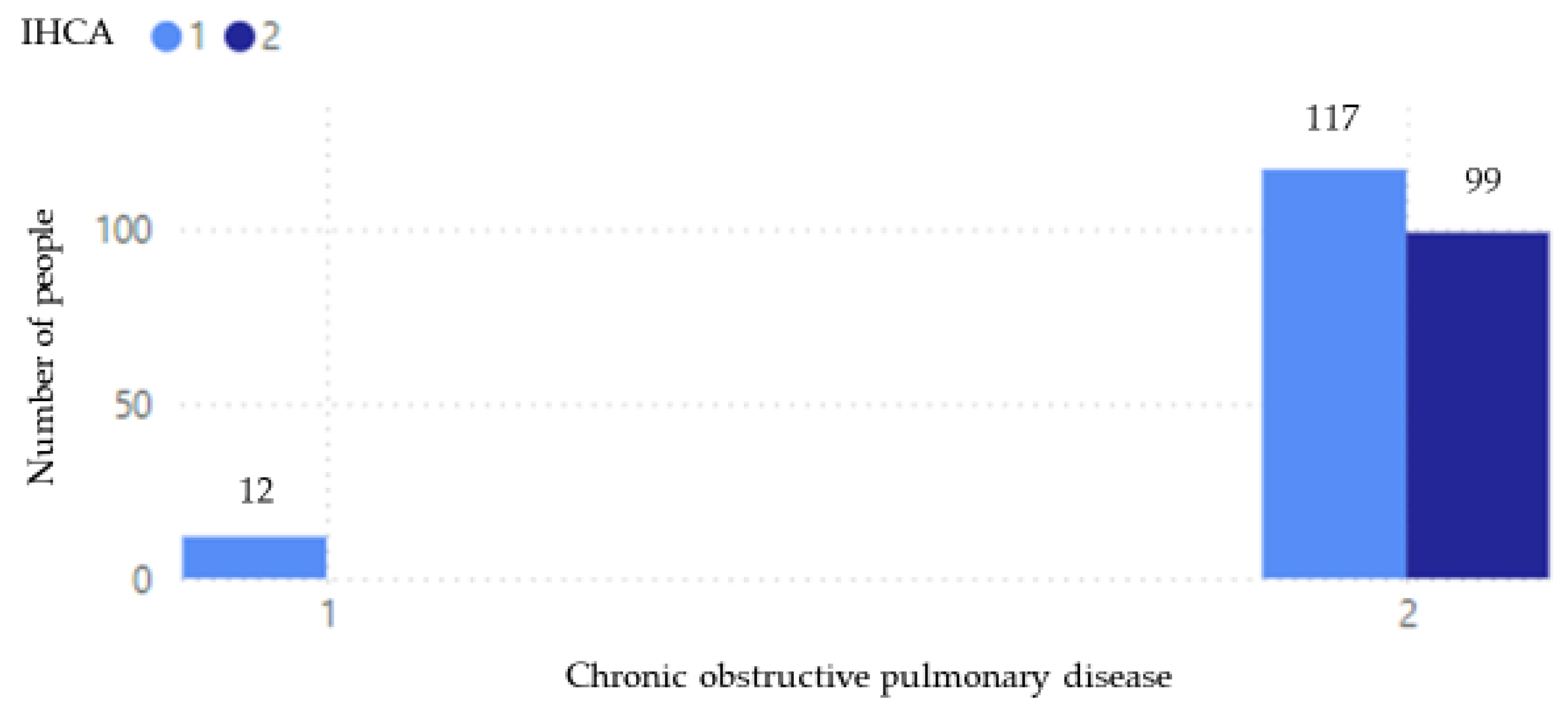
Figure 8 shows the relationship between COPD and IHCA mortality. The data show that among patients without COPD, 12 died after IHCA. In contrast, among patients with COPD, there were 117 deaths and 99 survivals after IHCA. From these data, we can observe that patients with COPD are not only more likely to develop IHCA, but their overall number of cases is also significantly higher than that of patients without COPD. This may be because the respiratory defense function of patients with COPD is weaker. Poor lung function makes it easier to develop infections such as pneumonia, and coupled with poor lung function, it is more likely to cause severe respiratory failure. However, among patients with COPD, the survival rate after IHCA is relatively high, which may be due to the higher awareness of medical staff for these high-risk patients and the fact that these patients have more complete care plans.
4.2. Results of Decision Tree Method
In order to establish a prediction model, this study applied the decision tree method in
Section 3.2 to our IHCA data. Again, we consider patients’ personal characteristic variables, NEWS categories, and CCI comorbidity categories and the IHCA features include age, gender, smoking, drinking, BMI, body temperature, pulse, respiration, systolic blood pressure, diastolic blood pressure, CPR, ROSC, heart disease, diabetes, hypertension, chronic obstructive pulmonary disease, kidney disease, stroke, dementia, polyarthritis, gastric ulcer, cancer, and asthma. These variables will be used as classification features (splitting attributes) of the decision tree model, and IHCA will be used as the target variable (target attribute). When conducting machine learning analysis, these variables will be used to build a classification model that aims to predict whether a person will develop IHCA based on these features. In order to adapt these variables to the decision tree model, some categorical variables need to be encoded and converted in data preprocessing. For example, gender includes two categories: male and female, and smoking and drinking may have options of “yes” or “no”. In these cases, numerical encoding (such as 1 and 2) is usually used to convert them into numerical data (
Table 1) so that they can be processed in the decision tree algorithm. In addition to processing the encoding conversion of categorical variables, some continuous variables also need to be standardized or normalized. For example, continuous variables such as age, BMI, body temperature, pulse, systolic blood pressure, and diastolic blood pressure may need to be scaled to have the same numerical range, thereby improving the training efficiency and prediction accuracy of the model.
When evaluating the model, we first examine the hyperparameters of decision tree model such as
Test size: 1/2, 1/3, 1/4;
Measures of impurity: Gini, entropy;
The maximum depth of the tree: 2–20;
Random state: 0~42.
As you can see, there are many hyperparameter combinations to test. This study examines the performance of the model based on the confusion matrix (
Table 2). TP (True Positive) is true and the prediction is true, that is, the prediction is correct; TN (True Negative) is false and the prediction is false, that is, the prediction is correct; FP (False Positive) is false but the prediction is correct, that is, the prediction is wrong; FN (False Negative) is correct but the prediction is false, that is, the prediction is wrong. The indicators used in this study include accuracy, precision, recall, and F1-score.
Table 3 shows the results in different test sizes under max_depth = 12, measures of impurity = Gini, and random state = 42. The best combination is found to be test size = 1/3, max_depth = 12, measures of impurity = Gini, and random state = 42. Since we have less data and the test set data is even smaller after cutting, the accuracy is relatively high, even up to 100%.
In addition,
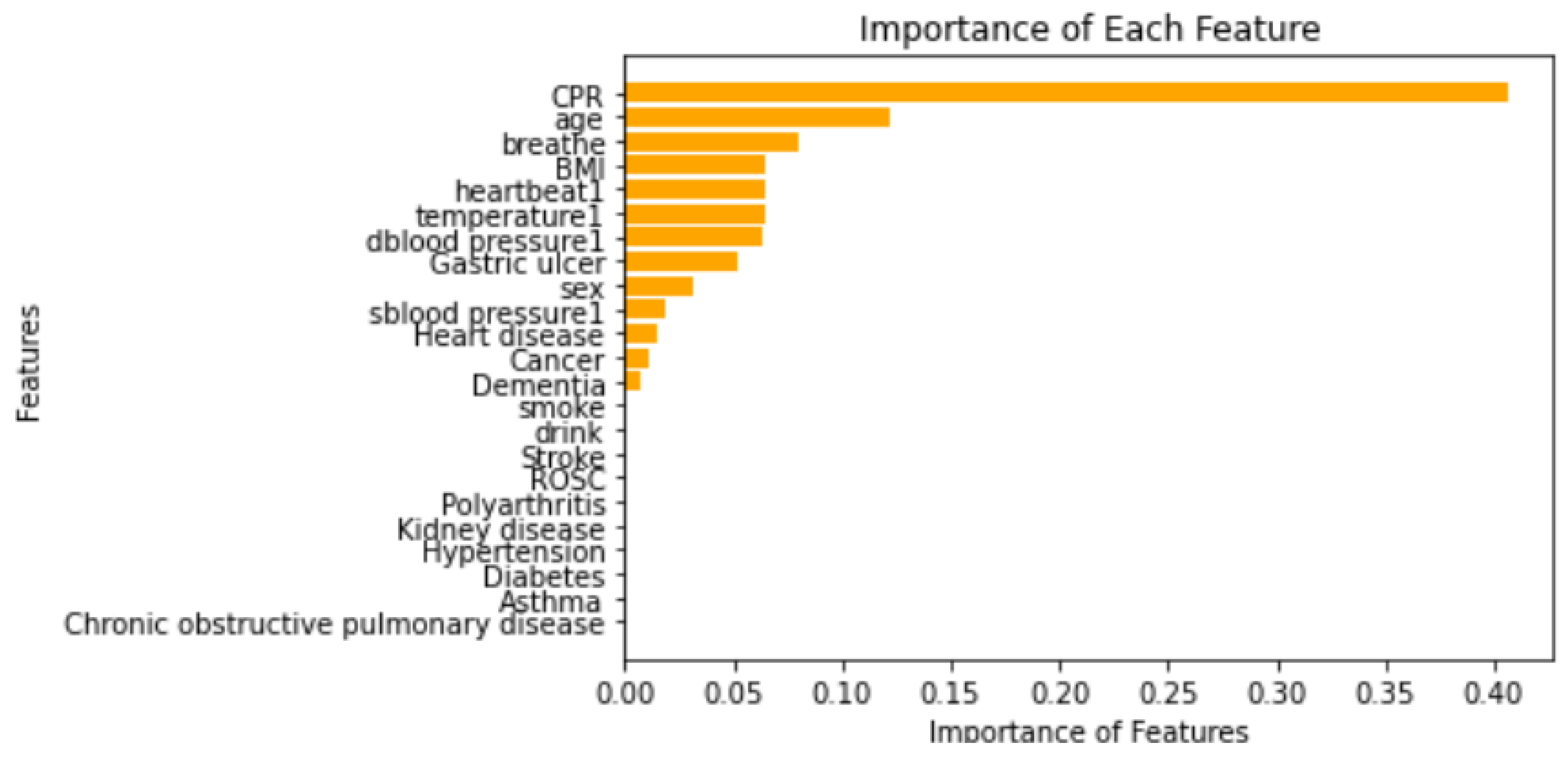
Figure 9 shows the importance of each feature in the decision tree model, sorted from high to low. It can be clearly seen from the figure that CPR is the most critical feature, and its weight far exceeds that of other features. Whether CPR is performed or not often plays a decisive role in the handling of acute events; the second most important factor is age, which is second only to CPR, indicating that age has a significant impact on the assessment of cardiac arrest risk; this is followed by respiratory rate, whose characteristic importance shows the key role of respiratory function in the risk of cardiac arrest. Problems such as dyspnea and abnormal breathing are often important precursors to acute cardiac arrest, especially in patients with heart failure, hypoxic shock, or complications of lung disease. Timely detection of abnormal breathing can provide early warning signals. BMI and body temperature are also considered important features by the model. BMI is an indicator of the patient’s body shape and nutritional status. Abnormal body temperature may be a manifestation of systemic disease or shock, which are usually potentially related to cardiac arrest. Therefore, BMI and body temperature occupy a certain position in the model, which also shows the warning value of these characteristics for acute risks; blood pressure is another important set of physiological indicators. The blood pressure value can directly reflect the patient’s cardiovascular function. In emergency situations, the real-time monitoring and analysis of blood pressure are of great significance for the prediction and prevention of cardiac arrest. The importance of gastric ulcer in the model is at a medium to low level. Although gastric ulcer is not a disease directly related to cardiac arrest, it may indirectly affect cardiovascular function through other mechanisms, thereby causing a low perfusion state and posing a potential threat to cardiac function. Gender also has a certain impact on the incidence of cardiac arrest. In emergency treatment, the impact of gender is often not the most direct decisive factor. This may be one of the reasons why the gender characteristics in the model are less important. From then on, although the contribution of characteristics with lower importance (such as chronic obstructive pulmonary disease, asthma, dementia, etc.) to the model is relatively small, they still have supplementary value in specific situations.
4.3. Discussion and Limitation
This study comprehensively explored the main factors for predicting IHCA through data analysis and model construction. Power BI key impact analysis and decision tree model were used for in-depth research. Both methods consistently pointed out that CPR, BMI, and heart disease are key influencing factors for predicting in-hospital cardiac arrest in emergency patients. These factors are not only of great clinical significance, but the consistency of the results of the two analysis methods further confirms the stability and reliability of these characteristics in model prediction.
(i) The importance of CPR is particularly evident in acute events of IHCA, which is consistent with the results of Kagawa et al. [
27] that immediate implementation of CPR can significantly improve ROSC and discharge survival rate.
(ii) BMI is an important indicator of cardiovascular health. Too high or too low BMI may be associated with the occurrence of cardiac arrest. Obese patients are usually accompanied by risk factors such as hypertension, diabetes, and metabolic syndrome, which are closely related to IHCA; low BMI may indicate the potential impact of malnutrition or chronic diseases, further increasing the risk of IHCA.
In addition, this study has the following limitations:
(i) Limited sample size
The sample size of this study is relatively limited and may not fully represent all patient groups in emergency settings. A larger dataset may provide a more robust and generalizable prediction model. Future studies should expand the scope of data collection to cover different regions and medical institutions to improve the applicability and external validity of the model.
(ii) Balance between clinical interpretation and decision support
Although the binary decision tree model constructed in this study has good interpretability, the key risk factors identified by the model may differ from clinical experience in some situations.
(iii) The main limitations of Power BI
1. It slows down when processing large datasets, especially when processing over a million records, where it can easily run out of memory or encounter memory allocation errors.
2. Power BI’s visualization tools and CSV import/export are generally limited to approximately 30,000 rows.
(iv) The main limitations of decision trees (CART)
1. Unrestricted tree depth may overfit the training data, resulting in poor generalization.
2. When certain classes are overrepresented, CART tends to favor those classes unless data balancing or weighting strategies are used to adjust for this.
3. While it can handle missing values directly, this automatic approach may introduce bias.
4.4. Importance of This Study for IHCA
In the context of unexpected in-hospital cardiac arrest (IHCA), mortality rates are high, and there is a high rate of permanent neurological impairment among survivors. This means that every incident prevention, prompt identification, and rapid intervention directly impacts the patient’s quality of life and length of life. When comparing with related references [
20,
21], our visual analytics of Power BI with the predictive capabilities of AI decision trees is particularly important for the following reasons:
1. Immediately understand risks and key indicators
IHCA often occurs within a short period of time, when a patient’s condition deteriorates. Traditional medical records and reports are often retrospective, failing to alert the medical team within prime time. This study addresses this issue as follows:
Power BI can instantly integrate data from multiple sources, including electronic medical records, monitoring device data, and laboratory tests, into dynamic dashboards.
AI decision trees can quickly identify high-risk combinations (such as specific vital sign changes, medication combinations, and abnormal test patterns) from a large number of historical cases and instantly assign risk scores.
2. Identifying early warning patterns from complex data
The precursors of IHCA may be scattered across various systemic data (respiratory rate, blood pressure trends, decreased urine output, etc.), making it easy for manual analysis to miss subtle but potentially fatal patterns. This study addresses this issue as follows:
Decision tree models automatically summarize the interactions among multiple variables, identifying often-overlooked risk combinations. For example, the model might indicate the following:
Low blood pressure + high lactate + increased respiratory rate → high risk;
Decreased heart rate variability + increased oxygen demand → need for enhanced monitoring.
These results are then visualized using Power BI, enabling medical staff to quickly understand them.
3. Helping medical teams develop more precise prevention strategies
Hospital resources are limited, making it impossible to provide the highest level of monitoring for all patients. This study addresses this issue as follows:
AI predictions can help accurately identify high-risk patients, prioritizing intensive care resources or proactive evaluation.
4. Continuously improving healthcare quality and reducing IHCA sequelae
IHCA survivors suffer a high rate of permanent neurological damage (such as anoxic encephalopathy), leaving limited room for improvement. This study addresses this issue as follows:
An AI decision tree analyzes data from the 24–48 h prior to IHCA to identify the appropriate time window for intervention and the most influential risk factors.
Power BI trend analysis tracks the correlation between interventions and outcomes, verifying which interventions reduce mortality and neurological injury rates.
Accordingly, we show the comparison of the proposed work to the existing works [
20,
21] in
Table 4.