Introduction
Endoscopic Retrograde Cholangiopancreatography (ERCP) is the gold standard technique for biliary tree exploration in benign or malignant pathologies of the common bile duct. Stone extraction or stent deployment are common mainstays in tertiary centers worldwide [
1,
2]. ERCP in congenital or post-surgery modified anatomy is a difficult task even in the hands of an expert endoscopist [
3]. Its efficacy, however, may be potentially challenged in anatomically complex scenarios such as situs inversus, a congenital condition characterized by a mirrored transposition of the abdominal/ thoracic organs. The mirrored anatomy not only necessitates a nuanced understanding, but also the mastery of modified techniques to ensure the safety and effectiveness of the ERCP procedure. This article presents particularities of stone extraction ERCP techniques tailored for situs inversus patients, including the procedural adaptations, technological support, and the multidisciplinary approach able to ensure optimal outcomes.
Situs inversus totalis (SIT) is a rare congenital condition characterized by the complete inversion and mirroring of the normal human anatomy. The incidence of SIT in the general population is estimated to be between 1 in 8,000 to 1 in 25,000 live births. This condition is inherited in an autosomal recessive pattern and has been linked to multiple gene mutations. Additionally, SIT is often associated with primary ciliary dyskinesia [
1]. Another study reported the incidence of SIT to be approximately 1 in 10,000, with a female-to-male ratio of 1:1.5, and no racial predilection. Clinically, SIT is usually asymptomatic in the absence of diseases. However, when associated with other conditions, such as cholecystitis or appendicitis, the diagnosis can be challenging due to the reversed anatomical location of symptoms [
4,
5].
In the following article, the case of a 33-year-old woman with known situs inversus is presented and discussed, with special emphasis on the main diagnostic and therapeutic difficulties that may be encountered during the medical management. The debate also includes the interdisciplinary approach between endoscopists, radiologists and surgeons, which is essential in addressing the complex anatomical landscape of patients with situs inversus undergoing ERCP calculus extraction, thus contributing to a better understanding and further refinement of these specialized techniques.
Case presentation
It is presented the case of a 33-year-old female, without any significant medical history outside of known SIT, cholecystectomy and obesity grade I, that presented to our hospital for abdominal pain and fever which started 7 days prior to admission.
Clinical examination showed a hemodynamically stable patient, with no jaundice, but mild tenderness in the epigastrium. Laboratory tests revealed mild leukocytosis and hepatocytolisis, increased serum direct bilirubin (0.80 mg/dL) and fibrinogen (499mg/dL).
An abdominal contrast-enhanced MRI combined with MR cholangiopancreatography (MRCP) revealed a normal common bile duct and right intrahepatic branches dilated with a section resembling an intrahepatic biliary lake with lithiasis inside.
ERCP was performed with difficulty due to the patient's anatomical particularities, but initially the patient was placed in supine position, with the endoscopist turned with his right side toward the patient and then prone position was adopted when advancing the scope into the duodenum. A stable position in front of a macroscopically normal papilla was gained and facile biliary access quickly followed, with contrast injection showing a common bile duct (CBD) of 6 mm with filiform morphology of the distal CBD and no lacunary image along the duct. Extraction ballon was then used to control the CBD, but during this procedure, an intrahepatic biliary lake with lacunary image resembling stone conglomerate emerged the right lobe due to the pressure put up by the balloon inflation.
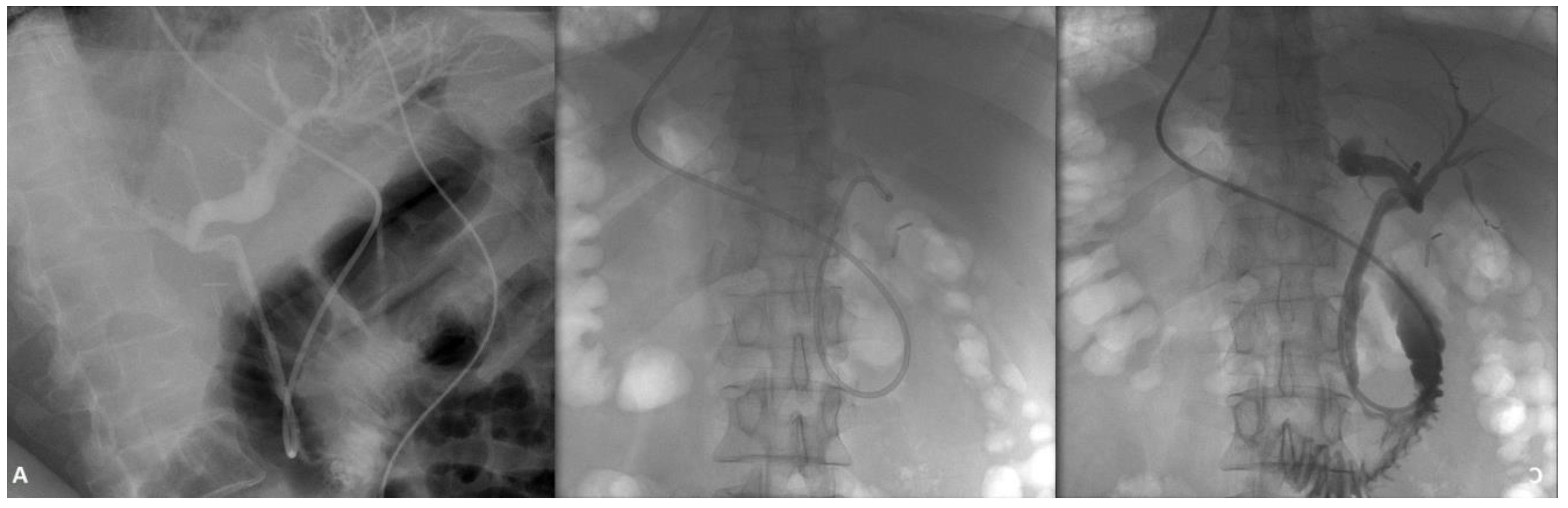
Figure 1.
Normal common bile duct (A), with biliary lake emerging in the right intrahepatic ducts (B and C).
Figure 1.
Normal common bile duct (A), with biliary lake emerging in the right intrahepatic ducts (B and C).
A guidewire was directed towards this anomaly and due to its twisted and narrow connection to the CBD, the decision was made to place a naso-biliary drainage tube (NBDT). Over the next 7 days the drainage was used to pour saline into the intrahepatic biliary abnormal dilation, at a rate of circa 1000-1500 ml per day.
Figure 2.
Naso-biliary drainage placement into the biliary lake (A), efficient downstream drainage (B) and clearance of the biliary stone conglomerate (C).
Figure 2.
Naso-biliary drainage placement into the biliary lake (A), efficient downstream drainage (B) and clearance of the biliary stone conglomerate (C).
Radiology studies showed by this time significant reduction in the biliary stone conglomerate, so ERCP was attempted two days later and the NBDT was extracted with insertion of 3 biliary plastic stents of 7 French each with their proximal part inside the biliary lake.
Figure 3.
Plastic stent placement after the NBDT was extracted.
Figure 3.
Plastic stent placement after the NBDT was extracted.
Through the days, the patient received antibiotic therapy of quinolone class and ursodeoxycholic acid (UDCA) was introduced at a dosage of 1500 mg per day in three portions following the first ERCP. Both the patient’s clinical and biochemical statuses improved and she was discharged two days after the second ERCP. Over the following 3 months the patient maintained only a UDCA therapy at the same doses as previously mentioned and no other symptoms were observed apart from a single diarrheal episode. At 3 months, the patient was once again admitted and ERCP evaluation, showing a normal CBD with the 3 biliary stents inside and almost normal intrahepatic ducts. Contrast injection showed complete bile clearance from within the intrahepatic ducts, so all the stents were removed. Repeated extraction balloon and basket passes of the CBD were performed with mere sludge extraction, mainly due to the lithogenic property of biliary stents. Patient was closely monitored over the next two days and then discharged with no other symptomatology for the following 6 months of surveillance.
Discussions
Situs inversus totalis is a very rare anatomical condition with a reported incidence of 1:5000 to 1:20000 that can initially lead the clinician to an incorrect or a delayed diagnosis. It is very important to note that a patient with clinical manifestations of cholangitis, but with left upper quadrant pain can be a patient with SIT. A thorough physical and biochemical examination as well as radiological investigations (abdominal ultrasound, CT scan or MRI) can guide the clinician into establishing a positive diagnosis of biliary lithiasis and SIT in a patient with left quadrant pain and with clinical signs of cholangitis [
6]. The literature has several reports of patients with SIT and bile duct lithiasis for which ERCP was performed. There is a debate about the best patient position and whether or not it is necessary to change the patient's position during the procedure to achieve better cannulation of the papilla. Currently, there is no guiding consensus as to whether left or right lateral, prone or supine positions are indicated in such cases, so for now physician experience contributes significantly to the patient management. [
7]. The first published ERCP case of a patient with SIT dates back to 1985, the subject being moved into different positions during the procedure to successfully cannulate the papilla [
8]. In 1988, in Finland, another ERCP with successful cannulation of the major papilla was performed to a SIT patient, with the patient lying on her right side and then in prone position and the endoscopist turned with his right side towards the patient. Another decade spanning study, which gathered 14 patients with SIT who underwent ERCP between 2011 and 2021, compared papilla cannulation rates and complication rates for patients placed in different positions. The study found that patients sitting in the prone position had less successful cannulation and more complications. The key to successful cannulation, according to this study, is changing the patients' position when the papilla cannot be cannulated on the first attempt, but more studies with larger numbers of patients are needed to identify the best approach [
9]. Another case of choledocholithiasis in a SIT patient who underwent both ERCP and laparoscopy is reported in the literature. The endoscopic approach was with the patient in left lateral decubitus and the duodenoscope rotated to 180 degrees into the second duodenum to identify the papilla. The patient experienced no complications or adverse events after the procedure, the case report drawing the conclusion that the patient can be placed in the usual position, but the endoscopist must carefully adapt to the altered anatomy in the patient [
9].
Patients with SIT and other congenital, gained or post-surgical alterations in the digestive or biliary tracts may pose difficult therapeutic challenges during ERCP. Although the literature most often refers to lithiasis developing in an SIT patient, there are also reports of malignancies in such patients. For example, an 85-year-old patient with jaundice due to adenocarcinoma of the head of the pancreas, duodenal infiltration and liver metastases is presented, in whom, despite multiple endoscopic maneuvers, the papilla could not be cannulated [
10]. Significant knowledge may be brought from more complex cases, like obtaining tissue biopsy and doing immunohistochemical studies for identification of tumoral types [
11]. Placing a plastic or metallic stent may impede or help in the process [
12]. Another research area may prove to be the radiofrequency ablation in cholangiocarcinoma [
13]. More questions on these patients may be answered by elaborately evaluating the duodenal wall for detection of duodenal primary tumors, like either the paragangliomas and GISTs, with possible global consequences, or lipomas and leiomyomas with benign evolution [
14,
15].
ERCP is a pivotal diagnostic and therapeutic procedure for pancreatico-biliary diseases. Its application can be technically challenging in patients with anatomical variations, such as situs inversus, a rare genetic condition where the organs are transposed to the opposite side of the body. This condition not only presents with an atypical clinical picture, but also necessitates modifications in standard surgical and endoscopic techniques. Moyon et al. highlighted a case of a 55-year-old male diagnosed with acute cholecystitis and situs inversus. Following a modified laparoscopic cholecystectomy, the patient had residual choledocholithiasis, which was addressed with ERCP [
16]. Inoue et al. described a woman in her 50s with situs inversus who underwent ERCP for biliary drainage using double-balloon enteroscopy without any modification in patient or endoscopist positioning [
17]. Sharma et al. discussed a 40-year-old male with situs inversus who was diagnosed with traumatic pancreatic injury. The resulting external pancreatic fistula was successfully managed with ERCP and stenting [
18]. Lastly, Téllez-Ávila et al. presented a case of a 65-year-old man with situs inversus totalis who had giant biliary stones. The ERCP procedure combined with intraductal cholangioscopy and laser lithotripsy was successfully performed without any modifications to the conventional technique [
19].
Recent studies have delved into the challenges and techniques associated with performing ERCP in patients with SIT. One study explored the intricacies of ERCP and Endoscopic Ultrasound (EUS) techniques in SIT, emphasizing the need for adaptability when confronted with the anatomical mirror image presented by these patients [
20]. Another comprehensive multicenter case series reinforced the efficacy and safety of ERCP in SIT patients, providing valuable insights from an extensive literature review [
21]. The unique challenges posed by SIT during ERCP were further highlighted, emphasizing the importance of understanding this rare anatomical condition [
22]. A novel approach to facilitate ERCP in SIT patients was also proposed, suggesting the use of a rotatable papillotome in conjunction with adjusting the monitor's position, underscoring the need for innovative techniques in such unique cases [
23,
24].
Our case report presents a combination of two statistically very rare pathology features: the congenital predisposition for developing intrahepatic biliary stasis and SIT. Along with presenting the distinct medical case of our patient, the study also sheds light on the feasibility of complex interventional endoscopy when dealing with this kind of patient.
One other peculiarity was the biliary dilations’ volume at which the localized biliary stasis produced symptoms of pain, fever and leukocytosis, being estimated to be around 30/15mm.
Regarding treatment, placing a NBDT was of utmost help, the UDCA probably having a minor role. Still, we recommend using it when isolate conglomerate stones are found intrahepatic. In this case, antibiotic was primarily used because the patient presented with fever, but it still played an additional role of removing bile and dissolving stones. NBDT can easily be used to monitor the clearance of stone mass by injecting it with contrast. Consequently, the decision to remove the tube and place the stents resulted from the observation of the reduction in the diameter of the bile lakes but with the small microlithiasis remaining in this place, as well as from the need to discharge the patient. Keeping the patient for another two days was made for precluding further cholangitic event. Almost 100 days after diagnosis, the appearance of the biliary tree resembled normal architecture, so the stentless solution was chosen at this time, but with careful clinical and biochemical monitoring that showed it to be a correct option.
Endoscopic retrograde cholangiopancreatography in patients with situs inversus is a particularly rare and technically challenging procedure. Given the infrequency of this condition, there is a paucity of references and case studies available in the specialized literature. This limited availability of references underscores the need for more comprehensive research and documentation on the subject. The existing literature primarily focuses on the technical modifications and approaches required to successfully perform ERCP in these patients. However, the scarcity of such references highlights the importance of accumulating and sharing experiences from different medical centers to enhance our understanding and management of ERCP in situs inversus patients.