Case presentation
We present the case of a 47-year-old patient who was followed since 2018 for several lesions (discoidal, erythematous, asymptomatic papules and plaques) on the chest, upper body, face, and scalp. Systemic corticosteroid therapy and anti-H1 antihistamines were administered with partial/ temporary clinical improvement. In 2020, the skin lesions expanded and became intensely itchy. Skin biopsies were immediately performed and confirmed the diagnosis of chronic eczema, disapproving the suspicion of mycosis fungoides. In March 2021, another episode of exacerbation was recorded and systemic corticosteroids were administered, with favorable evolution to high doses. Subsequently, dose reductions resulted in recurrence of the lesions. Given the lack of response and severe local and systemic manifestations, the treatment with dupilumab was administered from May to October 2021. However, lesional progression occurred with the appearance of tumor formations on the scalp and face, some of which became ulcerated.
Consequently, additional histopathological examination and immunohistochemistry tests were performed in February 2022, which confirmed the diagnosis of mycosis fungoides in the tumoral stage. Therefore, treatment with methotrexate (15 mg/week) and UVA phototherapy were initiated. In March 2022, the patient presented to dermatology with severe eruptions, consisting of well delineated, infiltrated, exudative, erythematous plaques, some of them with an erythematous halo, associated with itching and local pain, disseminated on the trunk, upper limbs and cephalic extremity. For these manifestations systemic antibiotherapy and corticotherapy were initiated. The weekly administration of methotrexate 15 mg and folic acid continued and also the topic treatment of the lesions with benzalkonium chloride solution and application of betamethasone ointment. This management was followed by a partial improvement of skin lesions and resumption of UVA therapy.
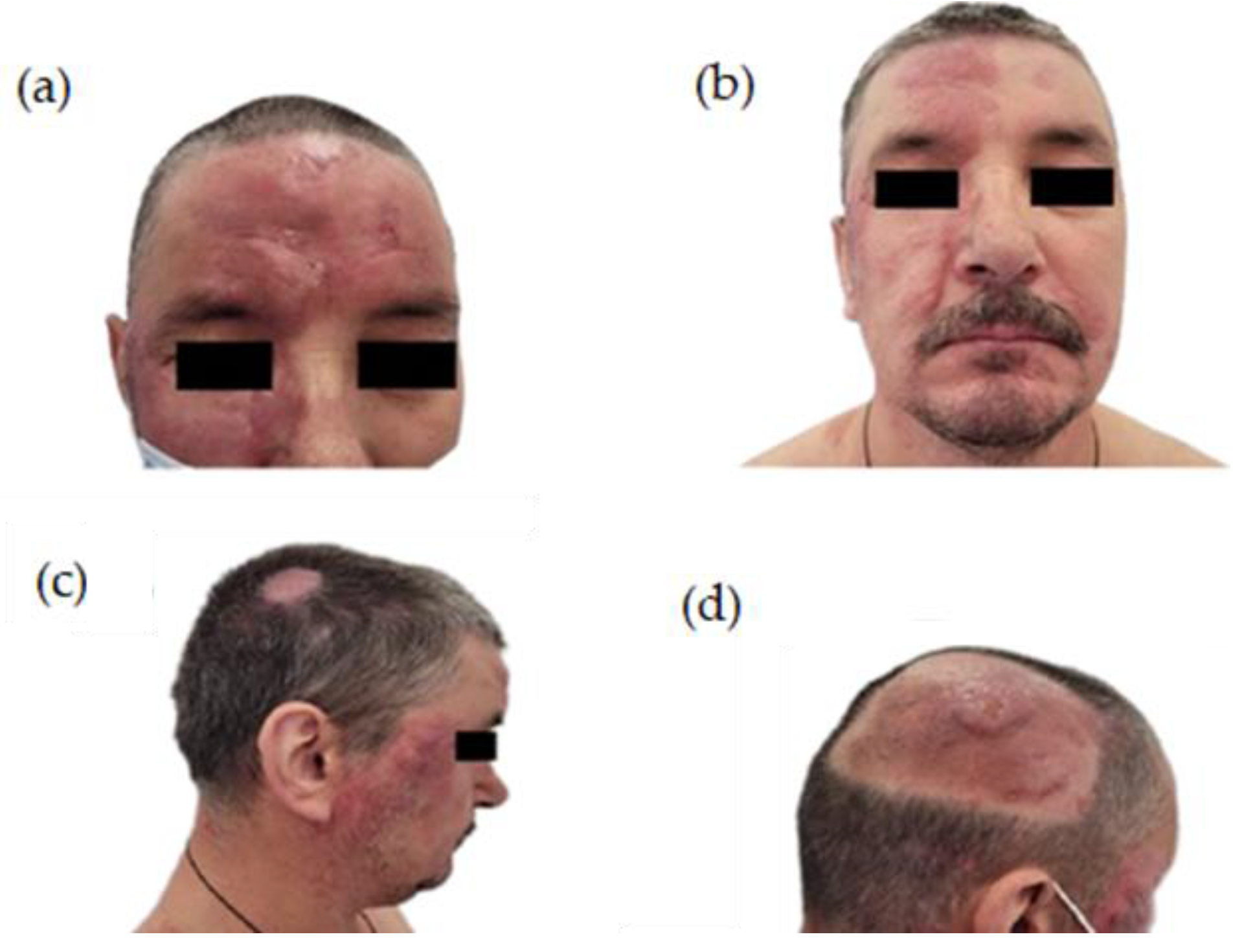
In May 2022, the oncology board at our radiation therapy center examined the patient and decided to enroll him in a palliative radiation therapy program for the treatment of localized lesions on the face and scalp (
Figure 1), using LINAC ELEKTA 6 MV with 3DCRT technique on the following PTVs: PTV right frontal (TD=30 Gy/15 fractions, D/fr=200 cGy), PTV right parietal (TD=30 Gy/15 fractions, D/fr=200 cGy), PTV left oral commissure (TD=30 Gy/15 fractions, D/fr=200 cGy) (
Figure 2).
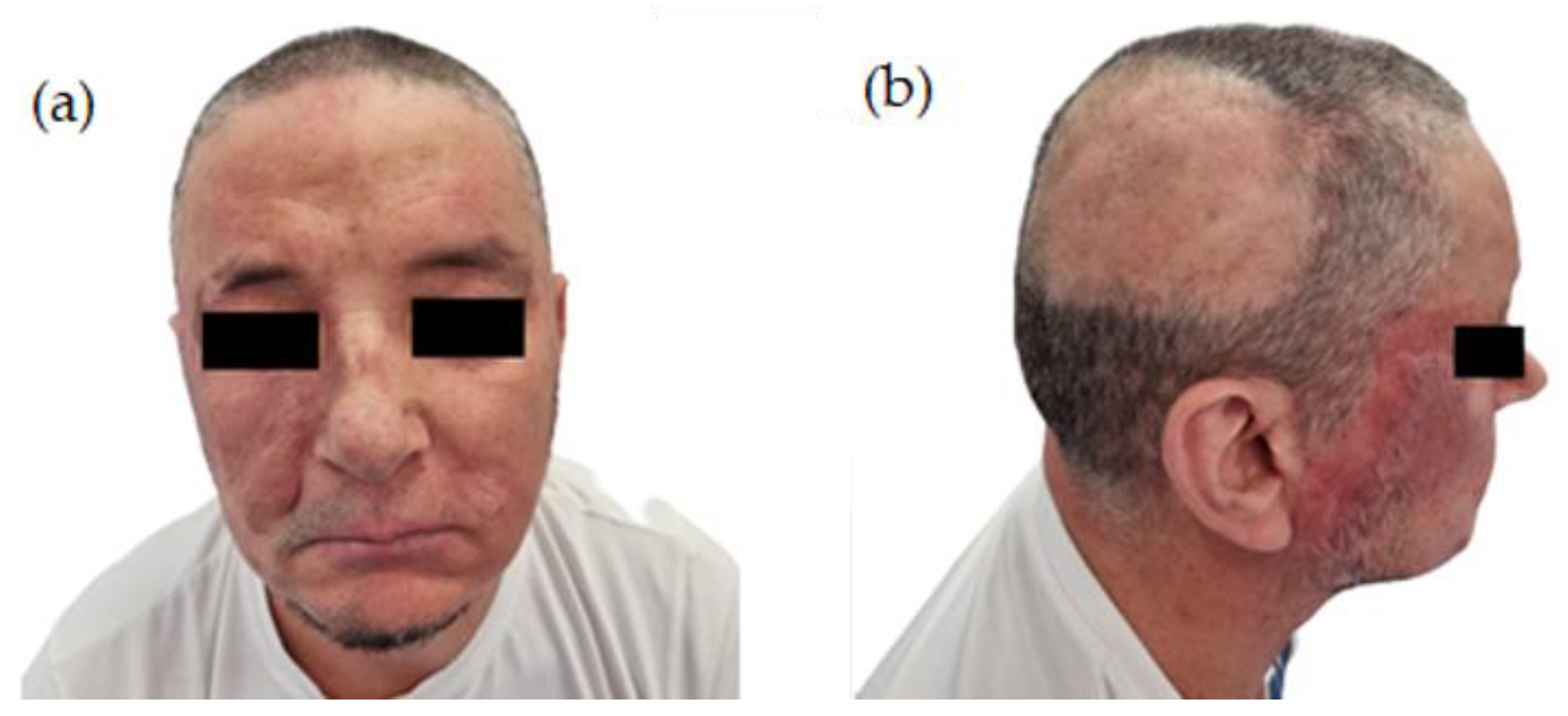
During RTE, the patient developed mucositis and second grade radiodermatitis; the ECOG performance status remained the same (ECOG=1) with a stationary weighting curve. At the end of the treatment, remission until the disappearance of the irradiated skin lesions were observed (
Figure 3).
Discussions
Rarely, mycosis fungoides present as a single lesion or as a small number of clustered lesions, with definitive radiotherapy having a role in long-term disease control. Generally, patients with MF refer to a specialist with diffuse lesions. In this type of presentation, the management is based on the symptom relief and local control of the disease. In the case of other therapeutic models that are not effective or if a quick response is desired, local RT may be necessary, especially for facial disfiguring tumors, thick plaques (RT can treat in depth), painful or pruritic lesions [
6]. Local radiation response is a positive prognosis factor in comparison with same-age control subjects without response for Stage IA patients (affecting 10% of the body surface, no large bleeding regions, and no severe nodal or visceral involvement) [
7,
8]. Three (2%) of the 121 patients registered in a retrospective study with clinical stage IA disease died as a result of the disease's progression during the study period. The median survival rate was not reached until 32 years of follow-up. With only local RT, long-term remission or even an apparent "cure" has been seen [
7,
8]. Wilson et al. assessed 21 patients with minimal disease, treated with only local RT, and found the following results: complete response rate was obtained in (CR) =97%, disease free survival (DFS) after 5 and 10 years was 75% and 64%, respectively, improved DFS at 10 years in patients with a single lesion (85%) and in those receiving doses of at least 20 Gy (91%) [
9].
Micaily et al. reported the results obtained by the treatment of 18 patients with unilesional stage IA of MF, in which TD (total dose) was 30.6 Gy, CR was 100%, relapse-free survival (RFS) and overall survival after 10 years were 86% and 100%, respectively [
10].
Finally, Piccinno et al. evaluated 15 patients with MF stage IA who received an average dose was 22 Gy, the obtained remission rates of treated lesions being 95%. 5% of lesions presented a partial remission, while after 5-10 years the total rate without recurrence was 51% [
11].
In summary, the literature data shows that less than 5% of patients present with stage IA of MF, and this singular subgroup can only be effectively managed with local RT. Additionally, the best results for disease-free survival appear to be when doses of 20 to 30 Gy are used [
7].
Local RT is an effective palliative therapy for patients in all stages of MF with symptomatic skin lesions and is often used to treat lesions refractory to other local and systemic therapies. Various retrospective studies have shown very high CR rates (>95%) for individual MF lesions with fractional RT courses, and the fact that higher doses are associated with higher CR rates and local control [
9,
10,
11].
Cotter et al. registered 111 MF lesions (53% plates, 47% tumors) and recorded the effect of the radiation therapy and the impact of dose used on local control, demonstrating a CR when all lesions received doses >20Gy. Local in-field recurrence rates ranged from 42% for doses less than 10 Gy to 32% for doses between 10 and 20 Gy to 21% for doses between 20 and 30 Gy to 0 for doses greater than 30 Gy. There was no difference in response rates between plaques and tumors and it has been suggested that tumor doses equivalent to 30 Gy with 2 Gy per fraction were necessary for proper control of MF lesions [
12].
Palliation of individual skin lesions with very short courses of RT is more convenient for patients and also more cost-effective compared to hyperfraction [
13]. Thomas and colleagues evaluated the treatment of 270 CTCL lesions (primarily MF) using only a single fraction of local RT reaching the following conclusions: 97% of patients were treated with a single dose≥ 7 Gy, CR was observed in 94% of cases, the rate of relapse in the irradiation field was 1% with a median follow-up of 41.8 months [
14].
Neelis and colleagues reported a CR of 92% with DT=8 Gy in two fractions; local relapse occurred in 8% of the lesions treated. Only 30% of the lesions treated with 4 Gy in two fractions had a CR. Patients who did not have CR were retreated with 20 Gy in eight fractions without complications [
15]. None of these studies reported acute or chronic adverse reactions. As a conclusion of these studies, the palliation of MF skin lesions is very effective using only local RT. Moreover, short courses of one to two fractions (7–8 Gy) have led to favorable results and can be used for patients who require fast palliation and for patients who have a difficult time coming for a conventional regimen. In general, smaller lesions are eligible for a single treatment fraction, while larger lesions are often better managed with a more prolonged fractional approach [
16]. Jensen and collab. reported on the effectiveness of radiation therapy in the management of central nervous system involvement by MF. Their retrospective study included five patients with MF and CNS involvement who underwent cranial or craniospinal radiation therapy [
17]. From the five patients who had neurologic deficits at the initiation of radiation therapy, four of them experienced at least a partial improvement. After completing radiation therapy, these four patients were evaluated by MRI and three of them had complete resolution of CNS disease within the irradiated field. From their diagnosis of CNS involvement, the median time until death was 7.4 months and 1.2 months (ranging 0.4–7.1 months) from the end of radiation therapy treatment. Even though at the time of the last follow-up, all patients had succumbed to their disease, this condition having an infaust prognosis, the conclusion of this study suggests that radiotherapy can play a valuable palliative part for patients with MF and central nervous system involvement [
17].
Geller and colleagues reported on three cases of MF involving the female genitalia. The implication of female genitalia is uncommon; therefore, the diagnosis and the therapeutic decision represent real challenges. All three patients had a long history of MF before the appearance of a vulvar MF tumor. The first patient was a 30-year-old female with a 10-year background of MF stage IIA, under multiple therapeutic approaches such as phototherapy, corticotherapy, interferon and local radiation, a partial response was obtained and the aggravating of the disease on her skin, including the appearance of a vulvar MF tumor that was rapidly registered. Subsequently, after the biopsy confirmed the tumoral stage MF, treatment was initiated, but with partial response. Consequently, palliative RT to the labia with a total dose of 14 Gy in 7 fractions 2 fractions weekly were administered and followed by TSEB to the rest of the skin with a complete response. The second patient, an 85-year-old female, with a 5-year background of MF stage IIB, was in almost complete remission after TSEBT and local RT to the genital area and maintenance therapy (bexarotene). However, as in the first case, the patient developed a rapidly growing labial tumor. Local RT with a total dose of 25 Gy in 10 fractions was given every other day with a nearly complete response and notable attenuation of symptomatology. The third patient was a 52-year-old, which followed the same management plan as the first two cases; thereby, electron beam radiotherapy with a total dose of 20 Gy in 10 fractions, every other day, was administered to the genitalia and intergluteal fold with important improvement. Eventually, the skin disease progressed, but not in the genital area. As a conclusion of this study, despite the systemic progression, exceptional local control can be reached with low dose radiation therapy of the genital area [
18].
Katano reported on the case of a sixty-year-old man with a 5-year history of tumor stage MF of the scalp who showed excellent response after only one fraction of palliative radiation therapy. The pillar treatment for tumor stage MF is systemic therapy together with skin directed local therapy. During retinoid therapy, the patient complained about itching and oozing. He had received multiple treatments, such as UVB phototherapy, corticotherapy, and oral bexarotene administration. The tumor was over 10 cm in diameter with partial necrosis, located in the occipital region. Palliative skin directed electron radiation therapy was performed for the occipital tumor with a total dose of 8 Gy in only one fraction; the electron energy used was 6 MeV with a 5 mm bolus onto the tumor. After the treatment, the tumor regressed remarkably without any side effects related to radiation therapy [
19].
Radiotherapy together with immunotherapy, a combination that has a synergistic effect on cancer cells, has been shown to produce positive results in patients with non-small cell lung cancer and malignant melanoma [
20,
21]. In advanced MF, the use of immunotherapy is still experimental. However, the monoclonal PD-1 antibody pembrolizumab has recently been shown to be effective in treating advanced refractory MF [
22]. Pembrolizumab inhibits the PD-1/PD-L1 axis, which prevents immune cells from recognizing malignant cells. PD-1 is expressed by depleted T cells, and the T cell response is blunted by neoplastic cells expressing PD-L1. The potential risks of PD-1 inhibitors in malignant T cells have been the subject of much scientific work, as malignant T cells in MF and Sezary syndrome have also been shown to express PD-1 [
23]. Furthermore, the positive effect of combining immunotherapy and radiotherapy is thought to result from a "vaccine-like" effect resulting from increased antigen release from irradiated neoplastic cells and subsequent enhanced antitumor immunity by immunotherapeutic agents. This application perspective has not yet been published as a treatment scheme for advanced MF, and this small case series could be the basis for further studies. Interestingly, the first patient from their study did not respond to nivolumab in the past, but did respond to pembrolizumab and whole-skin electron irradiation. This may be due to the higher response rates of pembrolizumab compared to nivolumab in refractory MF. In addition, the benefit of PD-1 inhibitors plus radiotherapy over radiotherapy alone was demonstrated in the past, but remains to be investigated in MF, particularly with pembrolizumab and whole skin electron beam irradiation [
24].
The only late toxicity that occurred in the patients was hypothyroidism, and apart from that, the treatment was very well tolerated. In summary, pembrolizumab in combination with radiotherapy resulted in durable remission in 2 cases of refractory advanced stage cancer MF that had recurred after AHSCT. Pembrolizumab in combination with radiotherapy could be a valuable treatment option for patients with refractory MF who do not benefit from the graft-versus-lymphoma effect [
25].
Even though the majority of patients will never experience symptomatic nodal or visceral illness, local RT can be applied in this situation to relieve symptoms. Patients with advanced-stage MF may have swelling, discomfort, or other local symptoms as a result of bulky lymphadenopathy. Generally speaking, common doses are between 20 and 30 Gy with 2 to 3 Gy portions [
7].
Egal et al. reported on the psychological aspect of using palliative radiation therapy for the treatment of disfiguring mycosis fungoides lesions as a way to reduce psychological and social impact. The patient presented with multiple lesions on the skin including a mutilating nasal lesion, lesions whose extension gave a palliative intent to the treatment. After multiple lines of systemic therapy and immunotherapy, the results were poor. Following, the patient received localized radiotherapy, the lesions vanishing entirely after a few weeks. As a result, the patient reported a psychological alleviation. It is highlighted that radiation therapy can be performed with a palliative intent in such a way that it can improve esthetic aspects and reduce psychological and social impact. The total dose used was 36 Gy, 2 Gy per fraction, 5 fractions a week with low adverse events and great efficacy. The inclusion of psychologists, social workers, radiation oncologists and palliative care workers in the multidisciplinary boards is important in the complete patient care of the advanced stage of MF [
26].
Acute and chronic toxicities
Local RT for skin lesions has low rates regarding acute and long-term adverse effects. Within the treatment area, patients may have erythema and, rarely, dry or moist desquamation. Immediately following the start of RT, ulcerated lesions can occasionally seem more threatening. In general, the tegument heals quickly following a radiation treatment [
27]. In most cases, treatment doesn't require anything more than local symptom management. Patients may experience alopecia and changes in pigmentation in the treated areas over time. Although there are few examples of this in the literature, there is a potential possibility of secondary cutaneous cancers [
7].
Total Skin Electron Beam Therapy (TSEBT)
Total Skin Electron Beam Therapy (TSEBT) is a particular technique that allows uniform irradiation of the entire tegument. The dose that is typically used for treatment is 36 Gy, administered as one to two Gy per session for five to nine weeks [
28]. Complete remission rates are high; nonetheless, recurrences are frequent, a dose of 12 Gy with one Gy per fraction for twenty-one days, can be used for low-dose TSEBT [
29]. Current guidelines regarding the use of TSEBT in MF have postulated that the tumor location and the radiation dose are elements that influence treatment-related toxicity. Side effects include erythema, alopecia, temporary nail growth arrest, hand and foot swelling, minor epistaxis, blisters on the fingers and toes, diaphoresis, mild parotid gland swelling, gynecomastia in men, keratitis due to the use of internal eye shields, permanent nail dystrophy, xerosis, dysesthesia in the fingers [
30]. Even though the response rates are lower, low-dose TSEBT is better tolerated and adverse effects are temporary and milder when compared to the standard dose [
2].
Total skin electron beam therapy can be utilized at any stage of MF, especially when the disease has spread to the entire surface of the skin. It has a high success rate for remission and typically requires an 8–10 weeks treatment period with a total dose of 30-36 Gy [
6]. TSEBT is a technically challenging method that delivers radiation to the entire tegument's surface and is linked to more toxicities than local RT (erythema, desquamation, hyperpigmentation, pain) [
7].
One retrospective study from January 2013 until December 2020 focuses on the evaluation of the clinical response rate and disease-free interval (DFI) for three patients with MF after TSEBT. Two of the three patients had clinical complete remission (cCR) with clinical stages IB and IIB, while a clinical partial response was observed in one patient with clinical stage IIB. The disease-free interval persisted for 30 months for the first patient with stage IB (T2N0M0); however, the second patient died due to sepsis after five months of ending the treatment. These three patients who were previously treated with other methods of treatment had a lower DFI with radiation, compared with other literature data [
31]. Another literature study revealed the advantage of TSEBT for patients with MF with an initial complete clinical response of 75% and 47% for T2 and T3 disease, respectively [
32]. The extent of the disease is another important element that can influence the DFI and local control, Quirós et al. reported the major effect of extensive T3 skin involvement on cCR and DFI [
28].
Grandi et al. reported on the efficacy of low-dose and standard-dose total skin electron beam therapy in the management of MF, both in the early and in the advanced stages. This analysis revealed that low-dose TSEBT is associated with lower complete response rates but with high overall response rates. In addition, standard dose TSEBT was associated with high complete response rates, mainly in the early stages, and very high overall response rates. The majority of patients experienced not less than one adverse event during or briefly after the end of the treatment. However, multiple concurrent adverse events are experienced by patients treated with standard-dose TSEBT. Severe adverse effects were uncommon in both types of TSEBT. The chances of obtaining a complete response are not affected by the stage of the disease and seem not to be remarkably impacted, or to have a significant clinical response to low-dose TSEBT. Patients with advanced stage MF might have a decreased chance of achieving a complete response, unlike early stages when treated with standard-dose TSEBT [
33]. The MF’s treatment is multimodal, and his management requires a multidisciplinary team, with a difference regarding the primary tumor location and staging of the tumor [
34].
Because it affects mainly the skin and due to the fact that it is a life-long disease, MF generates high levels of distress and it has many associated psychiatric disorders, such as anxiety and depression [
35]. Research is and should remain focused on MF treatment by developing methods of improving the risk to benefit ratio which characterize this class of drugs, by enhancing the efficacy of drug transportation to the exact sites of action and by developing newer, innovative targeted therapies.