Surgery of the Colon; The Impact of Colostomy and Postoperative Complications on Patients' Quality of Life
Abstract
Introduction
Materials and Methods
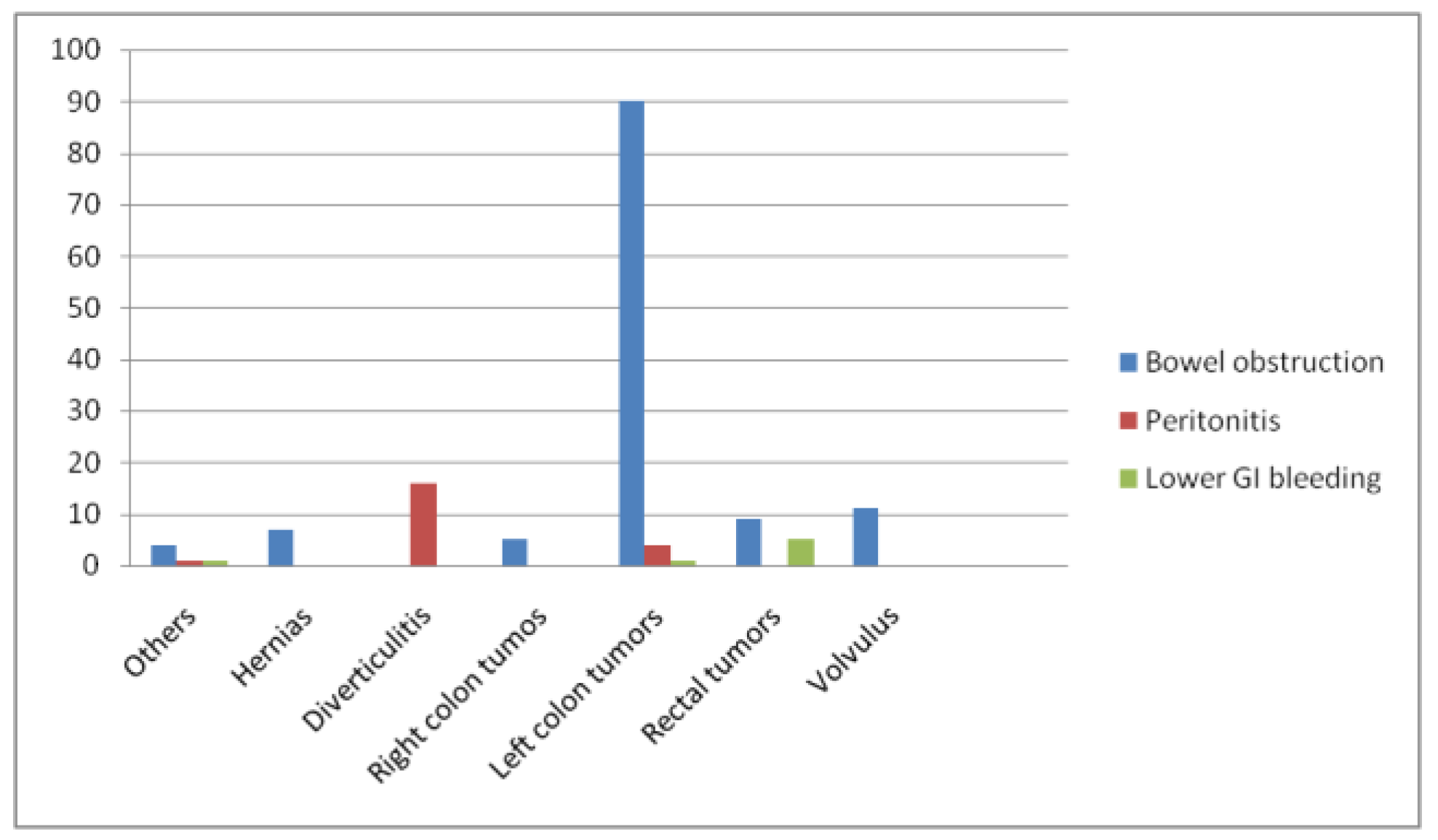
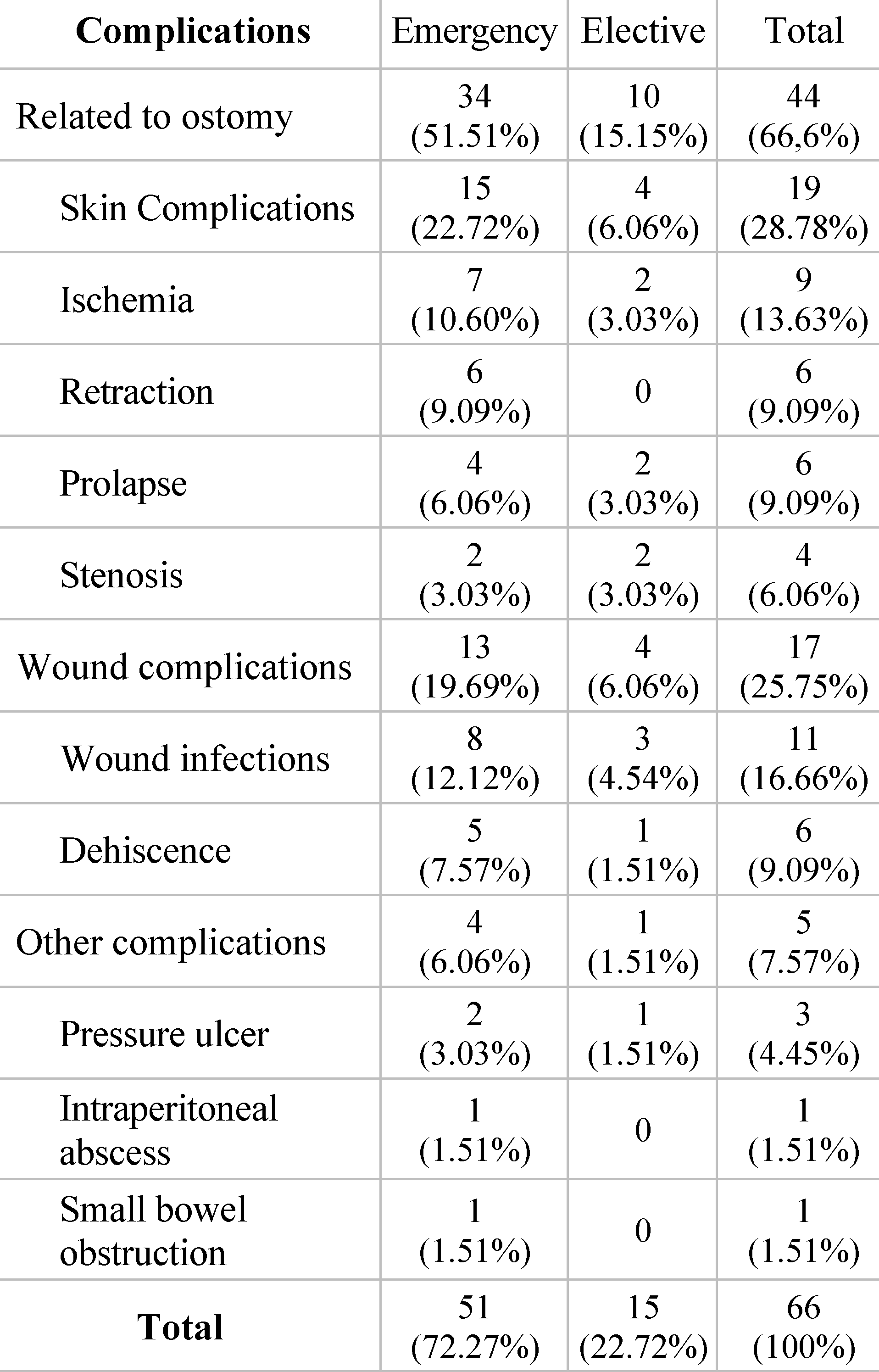
Results
Discussions
Conclusions
Informed Consent Statement
Conflicts of Interest
References
- Jin, D.-A.; Gu, F.-P.; Meng, T.-L.; Zhang, X.-X. Effect of low anterior resection syndrome on quality of life in colorectal cancer patients: A retrospective observational study. World J. Gastrointest. Surg. 2023, 15, 2123–2132. [Google Scholar] [CrossRef]
- Guerra-Londono, C.E.; Cata, J.P.; Nowak, K.; Gottumukkala, V. Prehabilitation in Adults Undergoing Cancer Surgery: A Comprehensive Review on Rationale, Methodology, and Measures of Effectiveness. Curr. Oncol. 2024, 31, 2185–2200. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Fang, Y.; Wei, Y.; Huang, F.; Zheng, J.; Xiao, H. The effects of a nurse-led discharge planning on the health outcomes of colorectal cancer patients with stomas: A randomized controlled trial. Int. J. Nurs. Stud. 2024, 155, 104769. [Google Scholar] [CrossRef]
- Ramamoorthy, L.; Davis, D.; Pottakkat, B. Impact of stoma on lifestyle and health-related quality of life in patients living with stoma: A cross-sectional study. J. Educ. Heal. Promot. 2020, 9, 328. [Google Scholar] [CrossRef] [PubMed]
- Krasnick, B.A.; Kalady, M.F. Management of Rectal Cancer in Lynch Syndrome: Balancing Risk Reduction and Quality of Life. Clin. Colon Rectal Surg. 2023, 37, 180–184. [Google Scholar] [CrossRef]
- Mohandas, K.M. Colorectal cancer in India: controversies, enigmas and primary prevention. Indian J. Gastroenterol. 2011, 30, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Braicu, V.; Stelian, P.; Fulger, L.; Verdes, G.; Brebu, D.; Duta, C.; Fizedean, C.; Ignuta, F.; Danila, A.I.; Cozma, G.V. Impact of Systemic Treatments on Outcomes and Quality of Life in Patients with RAS-Positive Stage IV Colorectal Cancer: A Systematic Review. Diseases 2024, 12, 79. [Google Scholar] [CrossRef]
- Tudosie, M.; Pauna, A.; Stefani, C.; Staicu, I. Diet and Food chemicals increasing the risk of colorectal cancer—Literature review. J. Mind Med Sci. 2022, 9, 118–124. [Google Scholar] [CrossRef]
- Post, M. Definitions of Quality of Life: What Has Happened and How to Move On. Top. Spinal Cord Inj. Rehabil. 2014, 20, 167–180. [Google Scholar] [CrossRef]
- Paszyńska, W.; Zborowska, K.; Czajkowska, M.; Skrzypulec-Plinta, V. Quality of Sex Life in Intestinal Stoma Patients—A Literature Review. Int. J. Environ. Res. Public Heal. 2023, 20, 2660. [Google Scholar] [CrossRef]
- Nitsch, K.E.; Ivatury, S.J. Patient reported outcome measures (PRO) in colorectal surgery. Surg. Open Sci. 2024, 19, 66–69. [Google Scholar] [CrossRef] [PubMed]
- Davidson, F. Quality of life, wellbeing and care needs of Irish ostomates. Br. J. Nurs. 2016, 25, S4–S12. [Google Scholar] [CrossRef]
- Pavlidis, E.T.; Galanis, I.N.; E Pavlidis, T. Management of obstructed colorectal carcinoma in an emergency setting: An update. World J. Gastrointest. Oncol. 2024, 16, 598–613. [Google Scholar] [CrossRef] [PubMed]
- Socea, B.; Silaghi, A.; Rebegea, L.F.; Balan, D.G.; Balalau, C.; Tenea-Cojan, T.Ș.; Mihai, D.A.; Paunica, I. Diabetes mellitus: Interdisciplinary medical, surgical and psychological therapeutic approach. J. Mind Med Sci. 2023, 10, 217–236. [Google Scholar] [CrossRef]
- Smith, J.A.; Spiers, J.; Simpson, P.; Nicholls, A.R. The psychological challenges of living with an ileostomy: An interpretative phenomenological analysis. Heal. Psychol. 2017, 36, 143–151. [Google Scholar] [CrossRef]
- Luo, X.; Xu, H.; Zhang, Y.; Liu, S.; Xu, S.; Xie, Y.; Xiao, J.; Hu, T.; Xiao, H. Identifying the unmet needs of post-treatment colorectal cancer survivors: A critical literature review. Eur. J. Oncol. Nurs. 2024, 70, 102570. [Google Scholar] [CrossRef]
- Skovsen, A.P.; Burcharth, J.; Gögenur, I.; Tolstrup, M.-B. Small bowel anastomosis in peritonitis compared to enterostomy formation: A systematic review. Eur. J. Trauma Emerg. Surg. 2022, 49, 2047–2055. [Google Scholar] [CrossRef]
- Faucheron, J.-L.; Vincent, D.; Barbut, M.; Jacquet-Perrin, I.; Sage, P.-Y.; Foote, A.; Bellier, A.; Quesada, J.-L.; Tidadini, F.; Trilling, B. Abdominal massage to prevent ileus after colorectal surgery. A single-center, prospective, randomized clinical trial: the MATRAC Trial. Tech. Coloproctology 2024, 28, 1–10. [Google Scholar] [CrossRef]
- Bisset, C.N.; Moug, S.J.; Oliphant, R.; Dames, N.; Parson, S.; Cleland, J. Influencing factors in surgical decision-making: A qualitative analysis of colorectal surgeons’ experiences of postoperative complications. Color. Dis. 2024, 26, 987–993. [Google Scholar] [CrossRef]
- Hoh, S.M.; Watters, D.A. The Best Stoma in an Emergency. World J. Surg. 2023, 47, 2865–2866. [Google Scholar] [CrossRef]
- van der Storm, S.L.; Bemelman, W.A.; van Dieren, S.; Schijven, M.P.; Stoma APPtimize Collaborative Study Group. A personalized app to improve quality of life of patients with a stoma: A protocol for a multicentre randomized controlled trial. Color. Dis. 2023, 25, 2071–2077. [Google Scholar] [CrossRef]
- Andersson, J.; Angenete, E.; Gellerstedt, M.; Haglind, E. Developing a multivariable prediction model of global health-related quality of life in patients treated for rectal cancer: A prospective study in five countries. Int. J. Color. Dis. 2024, 39, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Radulescu, D.; Baleanu, V.D.; Padureanu, V.; Radulescu, P.M.; Bordu, S.; Patrascu, S.; Socea, B.; Bacalbasa, N.; Surlin, M.V.; Georgescu, I.; et al. Neutrophil/Lymphocyte Ratio as Predictor of Anastomotic Leak after Gastric Cancer Surgery. Diagnostics 2020, 10, 799. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.P.; Talbott, V.A.; Leong, Q.Q.; Isenberg, G.A.; Goldstein, S.D. American Society of Anesthesiologists class and Charlson’s Comorbidity index as predictors of postoperative colorectal anastomotic leak: a single-institution experience. J. Surg. Res. 2013, 184, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Georgescu, S.R.; Tampa, M.; Paunica, S.; Balalau, C.; et al. Distribution of post-finasteride syndrome in men with androgenic alopecia. J. Investig. Dermatol. 2015, 135 (Suppl. 2). [Google Scholar]
- Hayden, D.M. Surgical approaches to locally advanced colon cancer: Best approach is a tough question to answer. Surgery 2021, 170, 1616–1617. [Google Scholar] [CrossRef]
- Constantin, V.D.; Silaghi, A.; Epistatu, D.; Dumitriu, A.S.; Paunica, S.; Bălan, D.G.; Socea, B. Diagnosis and management of colon cancer patients presenting in advanced stages of complications. J. Mind Med. Sci. 2023, 10, 51–65. [Google Scholar] [CrossRef]
- Razak, N.A.; Azhar, Z.I.; Baharuddin, I.H.; Ismail, Z.; Azman, Z.A.M.; Manap, S.A.A.; Ramli, N. Does Exercise Improve Health-Related Quality of Life of Colorectal Cancer Survivors? A Systematic Review and Meta-Analysis. Asian Pac. J. Cancer Prev. 2024, 25, 379–391. [Google Scholar] [CrossRef]
- MacDonald, S.; Wong, L.; John-Charles, R.; McKee, T.; Quasim, T.; Moug, S. The impact of intestinal stoma formation on patient quality of life after emergency surgery—A systematic review. Color. Dis. 2023, 25, 1349–1360. [Google Scholar] [CrossRef]
- Takayama, Y.; Tsukamoto, S.; Kudose, Y.; Takamizawa, Y.; Moritani, K.; Esaki, M.; Kanemitsu, Y.; Igarashi, A. Cost-effectiveness of surveillance intervals after curative resection of colorectal cancer. Ultrasound Med. Biol. 2024, 54, 637–646. [Google Scholar] [CrossRef]
- St-Louis, E.; Iqbal, S.; Feldman, L.S.; Sudarshan, M.; Deckelbaum, D.L.; Razek, T.S.; Khwaja, K.M. Using the age-adjusted Charlson comorbidity index to predict outcomes in emergency general surgery. J. Trauma Acute Care Surg. 2015, 78, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Feria, A.; Times, M. Effectiveness of Standard Treatment for Stage 4 Colorectal Cancer: Traditional Management with Surgery, Radiation, and Chemotherapy. Clin. Colon Rectal Surg. 2023, 37, 062–065. [Google Scholar] [CrossRef]
- Silaghi, A.; Constantin, V.; Socea, B.; Banu, P.; Sandu, V.; Andronache, L.; Dumitriu, A.; Paunica, S. Inflammatory bowel disease: pathogenesis, diagnosis and current therapeutic approach. J. Mind Med Sci. 2022, 9, 56–77. [Google Scholar] [CrossRef]
- Pirrera, B.; Vaccari, S.; Cuicchi, D.; Lecce, F.; De Raffele, E.; Via, B.D.; Di Laudo, M.; Tonini, V.; Cervellera, M.; Cola, B. Impact of octogenarians on surgical outcome in colorectal cancer. Int. J. Surg. 2016, 35, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Feizpour, C.A.; Turk, A.; Mohanty, S. Quality of Life Outcomes in Stage IV Colorectal Cancer. Clin. Colon Rectal Surg. 2023, 37, 102–107. [Google Scholar] [CrossRef]
- Cihan, E.; Vural, F. Effect of a telephone-based perioperative nurse-led counselling programme on unmet needs, quality of life and sexual function in colorectal cancer patients: A non-randomised quasi-experimental study. Eur. J. Oncol. Nurs. 2024, 68, 102504. [Google Scholar] [CrossRef]
- Krutsri, C.; Sumpritpradit, P.; Singhatas, P.; Thampongsa, T.; Phuwapraisirisan, S.; Gesprasert, G.; Jirasiritham, J.; Choikrua, P. Morbidity, mortality, and risk factors of emergency colorectal surgery among older patients in the Acute Care Surgery service: A retrospective study. Ann. Med. Surg. 2020, 62, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Koneru, S.; Builth-Snoad, L.; Rickard, M.J.F.X.; Keshava, A.; Chapuis, P.H.; Ng, K.-S. Major low anterior resection syndrome has equivalent health-related quality of life implications as having a permanent colostomy. Tech. Coloproctol. 2023, 28, 1–9. [Google Scholar] [CrossRef]
- Avsar, P.; Patton, D.; Ousey, K.; Blackburn, J.; O’Connor, T.; Moore, Z. The Impact of Surgical Site Infection on Health-related Quality of Life: A Systematic Review. Wound Manag. Prev. 2021, 67, 10–19. [Google Scholar] [CrossRef]
- Huynh, C.; Minkova, S.; Kim, D.; Stuart, H.; Hamilton, T.D. Laparoscopic versus open resection in patients with locally advanced colon cancer. Surgery 2021, 170, 1610–1615. [Google Scholar] [CrossRef]
- van der Storm, S.L.; Consten, E.C.J.; Govaert, M.J.P.M.; Tuynman, J.B.; Oosterling, S.J.; Grotenhuis, B.A.; Smits, A.B.; Marsman, H.A.; van Rossem, C.C.; van Duyn, E.B.; et al. Better stoma care using the Stoma App: does it help? A first randomized double-blind clinical trial on the effect of mobile healthcare on quality of life in stoma patients. Surg. Endosc. 2024, 38, 1442–1453. [Google Scholar] [CrossRef] [PubMed]

 |
© 2024 by the author. 2024 Vlad Denis Constantin, Adrian Silaghi, Dragos Epistatu, Daniela Gabriela Bălan, Florin Silviu Groseanu, Denisa Mihaela Nedelcu, Ioana Paunica
Share and Cite
Constantin, V.D.; Silaghi, A.; Epistatu, D.; Bălan, D.G.; Groseanu, F.S.; Nedelcu, D.M.; Paunica, I. Surgery of the Colon; The Impact of Colostomy and Postoperative Complications on Patients' Quality of Life. J. Mind Med. Sci. 2024, 11, 156-162. https://doi.org/10.22543/2392-7674.1493
Constantin VD, Silaghi A, Epistatu D, Bălan DG, Groseanu FS, Nedelcu DM, Paunica I. Surgery of the Colon; The Impact of Colostomy and Postoperative Complications on Patients' Quality of Life. Journal of Mind and Medical Sciences. 2024; 11(1):156-162. https://doi.org/10.22543/2392-7674.1493
Chicago/Turabian StyleConstantin, Vlad Denis, Adrian Silaghi, Dragos Epistatu, Daniela Gabriela Bălan, Florin Silviu Groseanu, Denisa Mihaela Nedelcu, and Ioana Paunica. 2024. "Surgery of the Colon; The Impact of Colostomy and Postoperative Complications on Patients' Quality of Life" Journal of Mind and Medical Sciences 11, no. 1: 156-162. https://doi.org/10.22543/2392-7674.1493
APA StyleConstantin, V. D., Silaghi, A., Epistatu, D., Bălan, D. G., Groseanu, F. S., Nedelcu, D. M., & Paunica, I. (2024). Surgery of the Colon; The Impact of Colostomy and Postoperative Complications on Patients' Quality of Life. Journal of Mind and Medical Sciences, 11(1), 156-162. https://doi.org/10.22543/2392-7674.1493



