Management of Macrovascular Diabetic Complications: A Single-Center Case Series Analysis of Consecutively Attending Patients in Primary Care
Abstract
Introduction
Materials and Methods
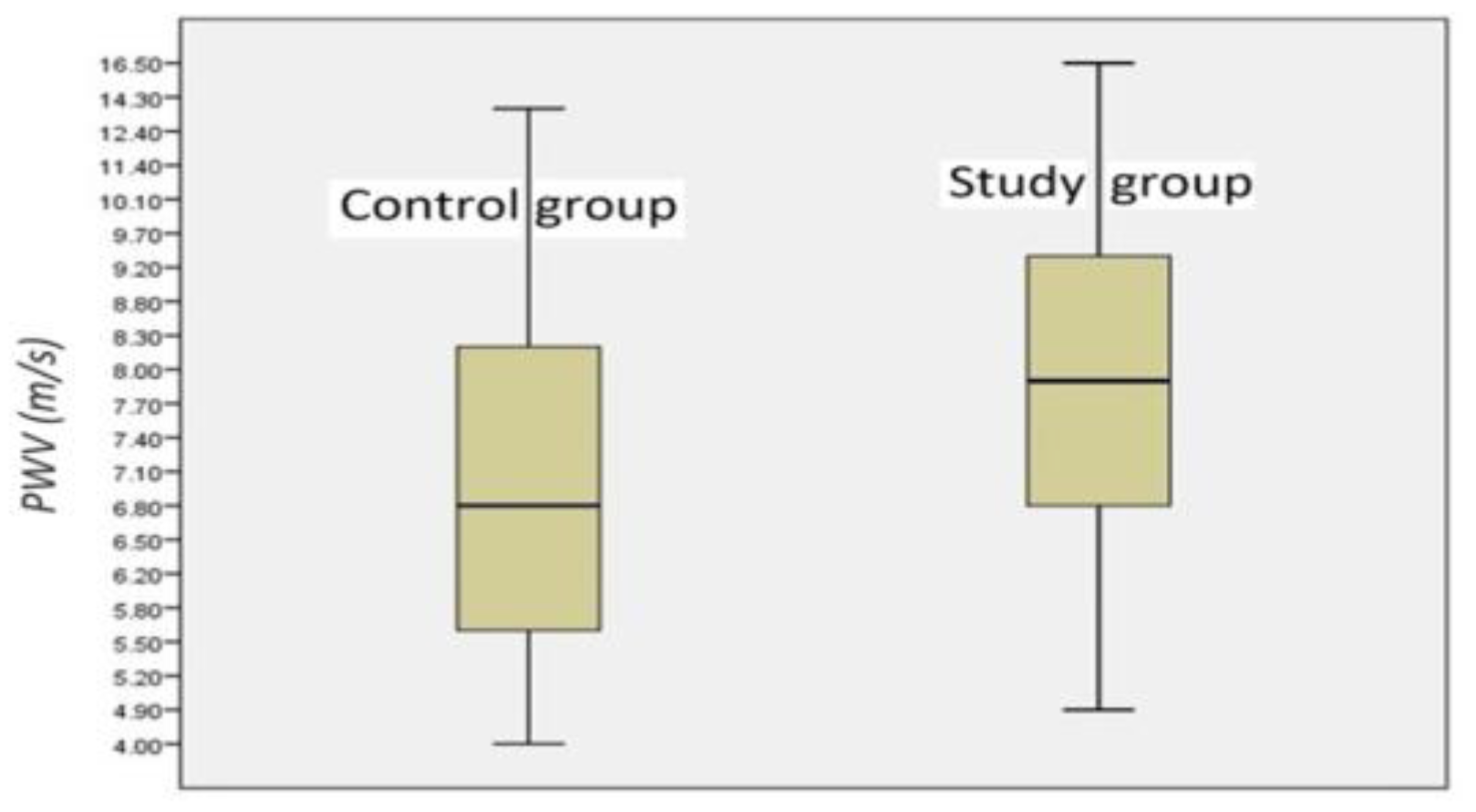
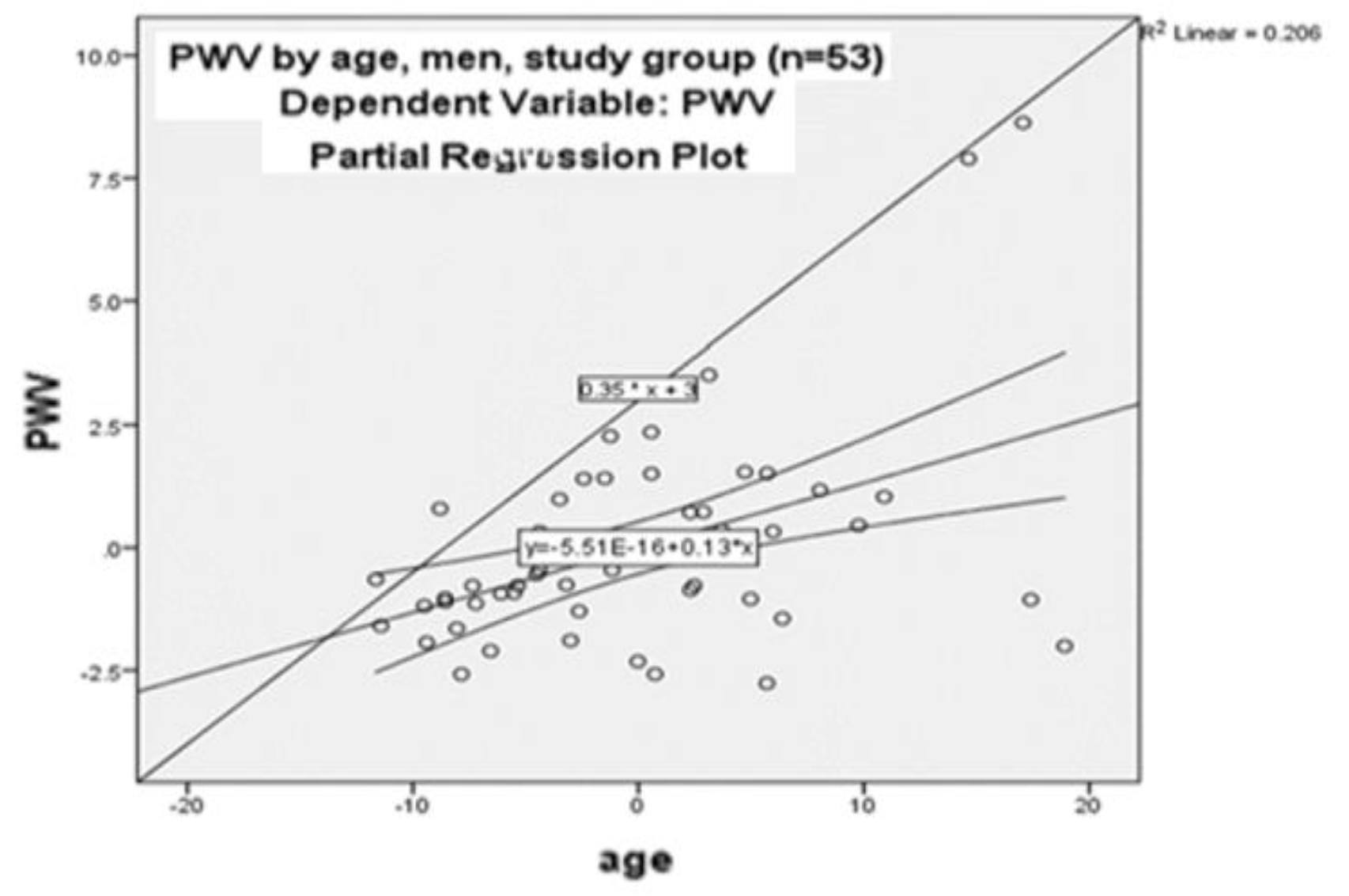
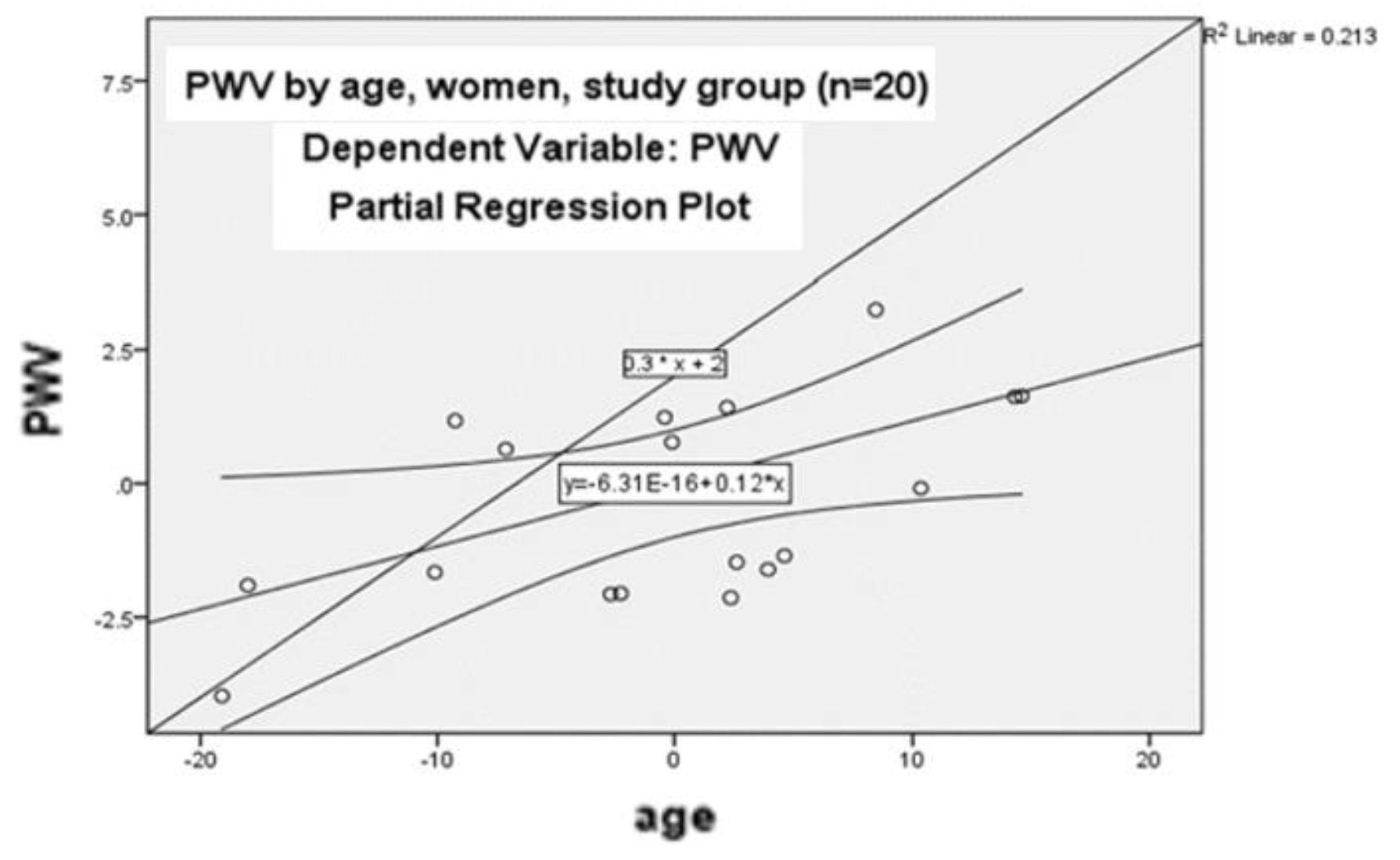
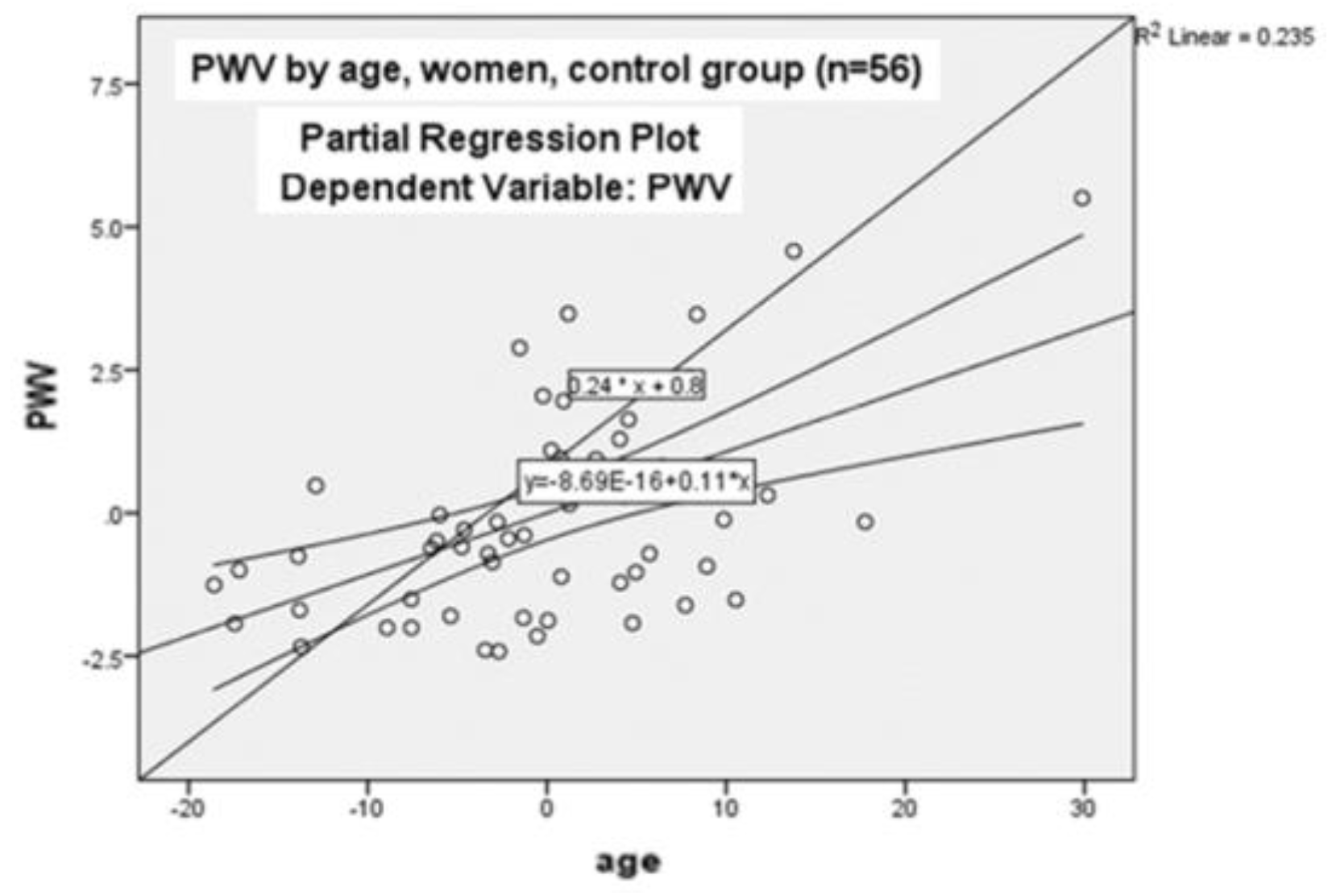
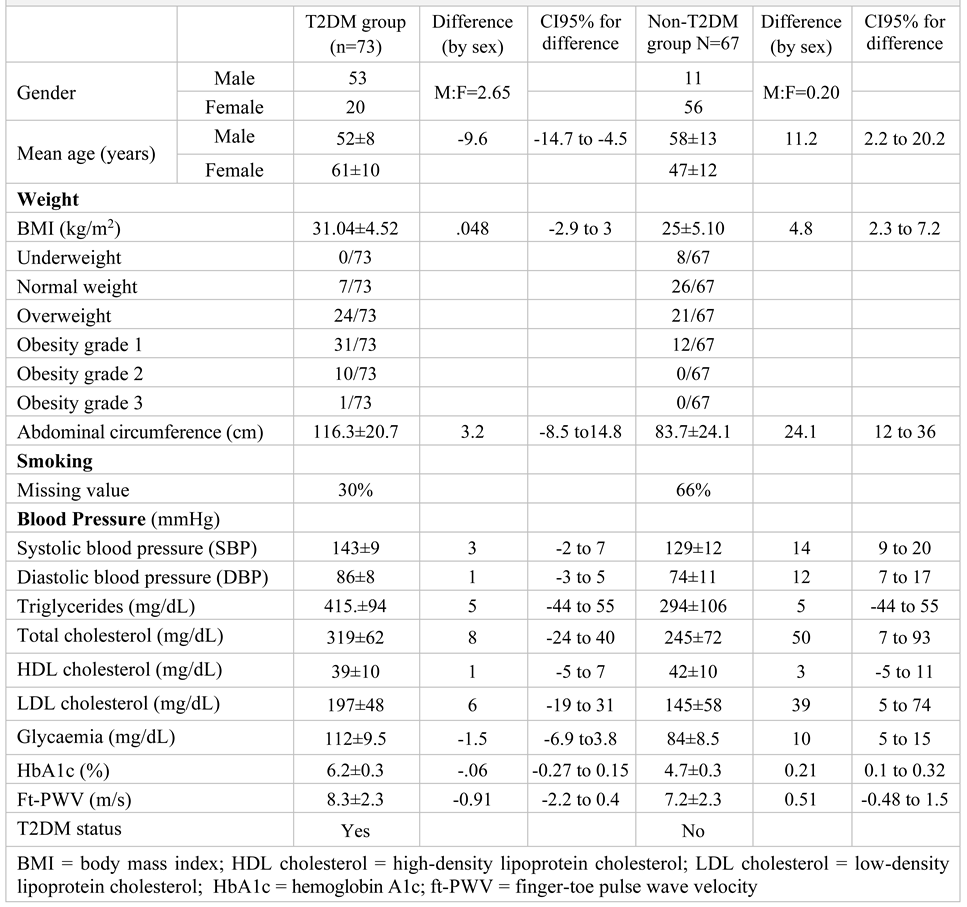
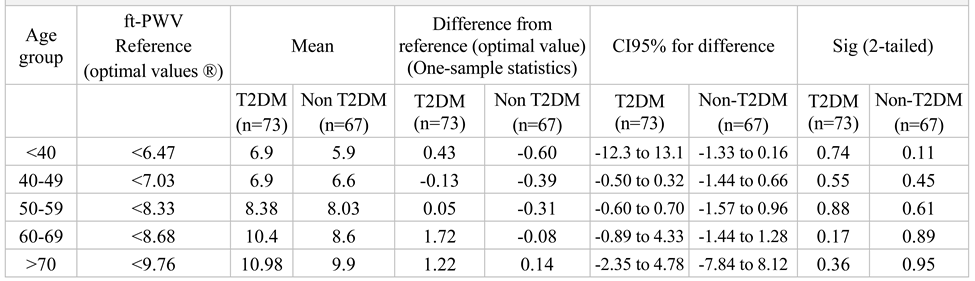
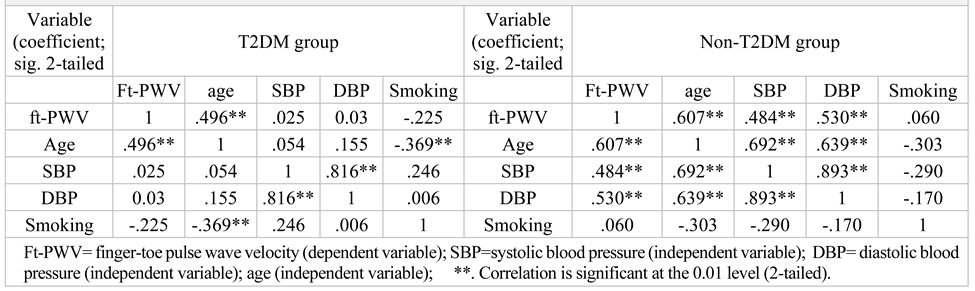
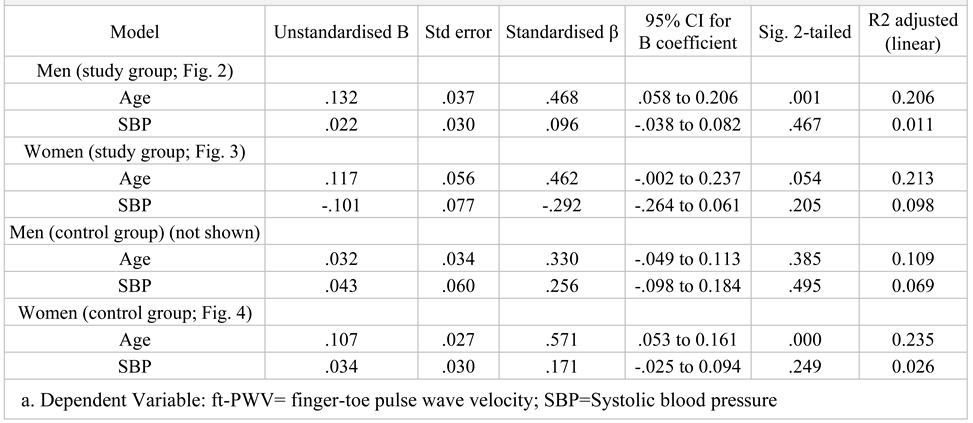
Results
Discussions
Conclusions
Informed Consent Statement
Conflicts of Interest
References
- Yan, Z.; Xu, Y.; Li, K.; Liu, L. Association between high-density lipoprotein cholesterol and type 2 diabetes mellitus: Dual evidence from NHANES database and Mendelian randomization analysis. Front. Endocrinol. 2024, 15, 1272314. [Google Scholar] [CrossRef] [PubMed]
- Cho, N.H.; Shaw, J.E.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.D.; Ohlrogge, A.W.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef]
- Cosentino, F.; Grant, P.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [PubMed]
- Oradea, O.C.C.E.H.O.; Baidog, A.; Bungau, S.; Behl, T.; Ratiu, I.; Aron, R.A.C.; Ursu, F.; Lazar, L.; Vesa, C.M. "Interrelationships between hyperuricemia, metabolic syndrome and chronic kidney disease in patients with diabetes mellitus". Arch. Balk. Med Union 2020, 55, 453–461. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4·4 million participants. Lancet 2016, 387, 1513–1530. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; Graham, I.M. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Thomopoulos, C.; Parati, G.; Zanchetti, A. Effects of blood-pressure-lowering treatment on outcome incidence in hypertension: 10 -Should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials. J. Hypertens. 2017, 35, 922–944. [Google Scholar] [CrossRef]
- Criqui, M.H.; Aboyans, V. Epidemiology of Peripheral Artery Disease. Circ. Res. 2015, 116, 1509–1526. [Google Scholar] [CrossRef]
- Patoulias, D.; Papadopoulos, C.; Stavropoulos, K.; Zografou, I.; Doumas, M.; Karagiannis, A. Prognostic value of arterial stiffness measurements in cardiovascular disease, diabetes, and its complications: The potential role of sodium-glucose co-transporter-2 inhibitors. J. Clin. Hypertens. 2020, 22, 562–571. [Google Scholar] [CrossRef]
- Zheng, M.; Zhang, X.; Chen, S.; Song, Y.; Zhao, Q.; Gao, X.; Wu, S. Arterial Stiffness Preceding Diabetes: A Longitudinal Study. Circ. Res. 2020, 127, 1491–1498. [Google Scholar] [CrossRef]
- Lou, Y.-M.; Liao, M.-Q.; Wang, C.-Y.; Chen, H.-E.; Peng, X.-L.; Zhao, D.; Gao, X.-P.; Xu, S.; Wang, L.; Ma, J.-P.; et al. Association between brachial-ankle pulse wave velocity and risk of type 2 diabetes mellitus: Results from a cohort study. BMJ Open Diabetes Res. Care 2020, 8, e001317. [Google Scholar] [CrossRef]
- Marushchak, M.; Hevko, U.; Krynytska, I.; Danylevych, Y.; Danchak, S.; Mazur, L. Does comorbid obesity or chronic pancreatitis influence the choice and effectiveness of glucose-lowering therapy in type 2 diabetic patients? Arch. Balk. Med Union 2021, 56, 24–32. [Google Scholar] [CrossRef]
- Stoica, R.A.; Diaconu, C.C.; Rizzo, M.; Toth, P.P.; Stefan, S.D.; Serafinceanu, C.; Nikolic, D.; Poiana, C.; Ionescu-Tirgoviste, C.; Pantea-Stoian, A. Weight loss programmes using low carbohydrate diets to control the cardiovascular risk in adolescents (Review). Exp. Ther. Med. 2021, 21, 9522. [Google Scholar] [CrossRef]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; Nathan, D.M.; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002, 346, 393–403. [Google Scholar] [CrossRef]
- Schutz, D.D.; Busetto, L.; Dicker, D.; Farpour-Lambert, N.; Pryke, R.; Toplak, H.; Widmer, D.; Yumuk, V.; Schutz, Y. European Practical and Patient-Centred Guidelines for Adult Obesity Management in Primary Care. Obes. Facts 2019, 12, 40–66. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46 (Suppl. 1), S128–S139. [Google Scholar] [CrossRef]
- Liang, Y.; Zhou, R.; Chen, H.; Cao, B.; Fan, W.; Liu, K.; Zhong, Q.; Huang, Y.; Wu, X.; Zou, M. Associations of blood biomarkers with arterial stiffness in patients with diabetes mellitus: A population-based study. J. Diabetes 2023, 15, 853–865. [Google Scholar] [CrossRef]
- Hansen, T.W.; Staessen, J.A.; Torp-Pedersen, C.; Rasmussen, S.; Thijs, L.; Ibsen, H.; Jeppesen, J. Prognostic Value of Aortic Pulse Wave Velocity as Index of Arterial Stiffness in the General Population. Circulation 2006, 113, 664–670. [Google Scholar] [CrossRef]
- Salvi, P.; Scalise, F.; Rovina, M.; Moretti, F.; Salvi, L.; Grillo, A.; Gao, L.; Baldi, C.; Faini, A.; Furlanis, G.; et al. Noninvasive Estimation of Aortic Stiffness Through Different Approaches. Hypertension 2019, 74, 117–129. [Google Scholar] [CrossRef]
- Obeid, H.; Khettab, H.; Marais, L.; Hallab, M.; Laurent, S.; Boutouyrie, P. Evaluation of arterial stiffness by finger–toe pulse wave velocity: Optimization of signal processing and clinical validation. J. Hypertens. 2017, 35, 1618–1625. [Google Scholar] [CrossRef]
- Alivon, M.; Phuong, T.V.-D.; Vignon, V.; Bozec, E.; Khettab, H.; Hanon, O.; Briet, M.; Halimi, J.-M.; Hallab, M.; Plichart, M.; et al. A novel device for measuring arterial stiffness using finger-toe pulse wave velocity: Validation study of the pOpmètre®. Arch. Cardiovasc. Dis. 2015, 108, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Heffernan, K.S.; Stoner, L.; London, A.S.; Augustine, J.A.; Lefferts, W.K. Estimated pulse wave velocity as a measure of vascular aging. PLoS ONE 2023, 18, e0280896. [Google Scholar] [CrossRef]
- Chobot, A.; Górowska-Kowolik, K.; Sokołowska, M.; Jarosz-Chobot, P. Obesity and diabetes—Not only a simple link between two epidemics. Diabetes/Metabolism Res. Rev. 2018, 34, e3042. [Google Scholar] [CrossRef]
- Forouhi, N.G.; Wareham, N.J. Epidemiology of diabetes. Medicine 2014, 42, 698–702. [Google Scholar] [CrossRef]
- Neeland, I.J.; Poirier, P.; Després, J.-P. Cardiovascular and Metabolic Heterogeneity of Obesity: Clinical Challenges and Implications for Management. Circulation 2018, 137, 1391–1406. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice, Committee; ElSayed, N.A.; Aleppo, G.; Bannuru, R.R.; Bruemmer, D.; Collins, B.S.; Ekhlaspour, L.; Hilliard, M.E.; Johnson, E.L.; Khunti, K.; et al. 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes—2024. Diabetes Care 2023, 47 (Suppl. 1), S11–S19. [Google Scholar] [CrossRef]
- Vazquez, G.; Duval, S.; Jacobs, D.R., Jr.; Silventoinen, K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiologic Rev. 2007, 29, 115–128. [Google Scholar] [CrossRef]
- Elias, M.F.; Crichton, G.E.; Dearborn, P.J.; Robbins, M.A.; Abhayaratna, W.P. Associations between Type 2 Diabetes Mellitus and Arterial Stiffness: A Prospective Analysis Based on the Maine-Syracuse Study. Pulse 2017, 5, 88–98. [Google Scholar] [CrossRef]
- Neeland, I.J.; Ross, R.; Després, J.-P.; Matsuzawa, Y.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: A position statement. Lancet Diabetes Endocrinol. 2019, 7, 715–725. [Google Scholar] [CrossRef]
- Strasser, B.; Arvandi, M.; Pasha, E.; Haley, A.; Stanforth, P.; Tanaka, H. Abdominal obesity is associated with arterial stiffness in middle-aged adults. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 495–502. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; et al. 10. Cardiovascular Disease and Risk Management: Standards of Care in Diabe-tes-2023. Diabetes Care 2023, 46 (Suppl. 1), S158–S190. [Google Scholar] [CrossRef] [PubMed]
- Tomiyama, H.; Hashimoto, H.; Hirayama, Y.; Yambe, M.; Yamada, J.; Koji, Y.; Shiina, K.; Yamamoto, Y.; Yamashina, A. Synergistic acceleration of arterial stiffening in the presence of raised blood pressure and raised plasma glucose. Hypertension 2006, 47, 180–188. [Google Scholar] [CrossRef]
- Oh, Y.S. Arterial stiffness and hypertension. Clin. Hypertens. 2018, 24, 17. [Google Scholar] [CrossRef]
- Socea, B.; Silaghi, A.; Rebegea, L.F.; Balan, D.G.; Balalau, C.; Tenea-Cojan, T.Ș.; Mihai, D.A.; Paunica, I. Diabetes mellitus: Interdisciplinary medical, surgical and psychological therapeutic approach. J. Mind Med Sci. 2023, 10, 217–236. [Google Scholar] [CrossRef]
- Adam, C.A.; Anghel, R.; Marcu, D.T.M.; Mitu, O.; Roca, M.; Mitu, F. Impact of Sodium–Glucose Cotransporter 2 (SGLT2) Inhibitors on Arterial Stiffness and Vascular Aging—What Do We Know So Far? (A Narrative Review). Life 2022, 12, 803. [Google Scholar] [CrossRef]
- Kim, J.M.; Kim, S.S.; Kim, I.J.; Kim, J.H.; Kim, B.H.; Kim, M.K.; Lee, S.H.; Lee, C.W.; Kim, M.C.; Ahn, J.H.; et al. Arterial stiffness is an independent predictor for risk of mortality in patients with type 2 diabetes mellitus: The REBOUND study. Cardiovasc. Diabetol. 2020, 19, 1–9. [Google Scholar] [CrossRef]
- Popa, S.; Mota, M.; Popa, A.; Mota, E.; Timar, R.; Serafinceanu, C.; Cheta, D.; Graur, M.; Hancu, N. Prevalence of dyslipidemia and its association with cardiometabolic factors and kidney function in the adult Romanian population: The PREDATORR study. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 596–602. [Google Scholar] [CrossRef]
- Trujillo-Hernández, B.; Trujillo-Magallón, E.; Trujillo-Magallón, M.; Brizuela-Araujo, C.A.; García-Medina, M.A.; González-Jiménez, M.A.; López-Peña, G.A.; Minakata-Nieto, J.; Rincón-Gutiérrez, L.A.; Tintos-Rueda, T.; et al. Frecuencia del síndrome metabólico y factores de riesgo en adultos con y sin diabetes mellitus e hipertensión arterial [Frequency of metabolic syndrome and risk factors in adults with and without diabetes mellitus and arterial hypertension]. Rev Salud Publica (Bogota) 2017, 19, 609–616. [Google Scholar] [CrossRef]
- Tanasescu, D.; Moisin, A.; Fleaca, R.; Popa, C.; Bacila, C.; Mohor, C.; Gherman, C.D.; Gaspar, B.; Tanasescu, C. Modern therapeutic options in diabetic foot ulcer. J. Mind Med Sci. 2022, 9, 285–293. [Google Scholar] [CrossRef]
- Hernán, M.A.; Sauer, B.C.; Hernández-Díaz, S.; Platt, R.; Shrier, I. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J. Clin. Epidemiology 2016, 79, 70–75. [Google Scholar] [CrossRef]
 |
 |
 |
 |
© 2024 by the authors. 2024 Sanda Maria Crețoiu, Mihaela Adela Iancu, Laura Maria Condur, Teodor Salmen, Andreea Steriu, Ana Maria Alexandra Stănescu, Irina Anca Eremia, Cristina Mihaela Olariu, Eliza Elena Cinteză, Camelia Cristina Diaconu.
Share and Cite
Crețoiu, S.M.; Iancu, M.A.; Condur, L.M.; Salmen, T.; Steriu, A.; Stănescu, A.M.A.; Eremia, I.A.; Olariu, C.M.; Cinteză, E.E.; Diaconu, C.C. Management of Macrovascular Diabetic Complications: A Single-Center Case Series Analysis of Consecutively Attending Patients in Primary Care. J. Mind Med. Sci. 2024, 11, 114-122. https://doi.org/10.22543/2392-7674.1451
Crețoiu SM, Iancu MA, Condur LM, Salmen T, Steriu A, Stănescu AMA, Eremia IA, Olariu CM, Cinteză EE, Diaconu CC. Management of Macrovascular Diabetic Complications: A Single-Center Case Series Analysis of Consecutively Attending Patients in Primary Care. Journal of Mind and Medical Sciences. 2024; 11(1):114-122. https://doi.org/10.22543/2392-7674.1451
Chicago/Turabian StyleCrețoiu, Sanda Maria, Mihaela Adela Iancu, Laura Maria Condur, Teodor Salmen, Andreea Steriu, Ana Maria Alexandra Stănescu, Irina Anca Eremia, Cristina Mihaela Olariu, Eliza Elena Cinteză, and Camelia Cristina Diaconu. 2024. "Management of Macrovascular Diabetic Complications: A Single-Center Case Series Analysis of Consecutively Attending Patients in Primary Care" Journal of Mind and Medical Sciences 11, no. 1: 114-122. https://doi.org/10.22543/2392-7674.1451
APA StyleCrețoiu, S. M., Iancu, M. A., Condur, L. M., Salmen, T., Steriu, A., Stănescu, A. M. A., Eremia, I. A., Olariu, C. M., Cinteză, E. E., & Diaconu, C. C. (2024). Management of Macrovascular Diabetic Complications: A Single-Center Case Series Analysis of Consecutively Attending Patients in Primary Care. Journal of Mind and Medical Sciences, 11(1), 114-122. https://doi.org/10.22543/2392-7674.1451



