Introduction
Acute cholecystitis is one of the most common diseases in digestive surgery, most of the time the main cause being represented by the presence of gallstones in the gallbladder. They can cause local irritation or obstruction of the cystic duct, which frequently induce biliary infections (through transient bacteremia or through the ascent of bacteria from the duodenum through the common bile duct). Generally, the clinical manifestations are characterized by the presence of pain in the right flank or right upper quadrant, associated with vomiting, altered bowel movements, and even mild jaundice in some cases. In severe forms, the presentation of the patient with acute cholecystitis can often be non-specific (with altered biological/clinical status, i.e., comatose, multiple organ failure, etc.), being more common in patients with multiple comorbidities or in the elderly, whose immunity is often compromised [
1,
2].
Regarding the epidemiology of acute cholecystitis, it can occur at any age, with age groups between 29 and 70 presenting different rates of incidence. The factors that influence the incidence of acute cholecystitis are mainly represented by gender and age. Women have an increased rate of gallstones, due to the hormonal profile which can affect cholesterol metabolism [
3,
4]. The colic pain in women is related in 18.8% of cases to biliary/ lithiasic etiology, compared to the male population of the same age in which the characteristic pain occurs in less than 10% of cases. With increasing age, the risk of acute cholecystitis increases. At over 70 years of age, this condition occurs in 15% of the male population and 24% of the female population, reaching double percentages after the age of 90 [
5,
6], The elderly often present altered symptomatology and reduced pain, so classic clinical manifestations are not very evident. The form of presentation is most often late, associating local complications as well as systemic comorbidities (hypertension, diabetes, peripheral arterial disease, cerebrovascular diseases or carotid artery stenosis, etc.) [
7,
8]. All these factors lead to the development of acute cholecystitis frequently in severe forms of the disease, with a higher rate of intraoperative and postoperative complications and lower survival rates, compared to the younger population with milder forms of the disease.
The diagnosis of acute cholecystitis is based on both the patient's clinical examination and paraclinical investigations. The specific parameters that would lead to a better identification and classification of the severity of this disease were developed during an International Congress held in Tokyo in 2006. For a clinical diagnosis, it is necessary that the symptomatology be specific, being represented especially by pain (with the classic description) in association with systemic manifestations such as fever, leukocytosis or the presence of inflammatory markers. Specific imaging methods are needed to confirm gallbladder distress [
9,
10,
11].
Imaging diagnosis in acute cholecystitis is mainly based on abdominal ultrasound. This procedure can detect an increased volume of the gallbladder, thickening of the gallbladder wall, the presence or absence of gallstones, the presence or absence of pericholecystic fluid, the presence of air in the gallbladder wall (which would suggest an important inflammatory process associated with gangrene), the diameter of the main bile duct, etc. The sensitivity and specificity of this imaging procedure reach predictable values in over 80% of cases [
12,
13,
14].
Taking into account all these parameters, the severity of acute cholecystitis was divided into 3 degrees. The severe form includes those patients who present in association with acute cholecystitis a newly established organ failure, associated marked leukocytosis, or the presence of a peri-cholecystic plastron when the symptoms last more than 72 hours. In contrast, the mild form of acute cholecystitis does not meet any of the criteria listed above [
15,
16].
The source of the inflammation of the gallbladder wall can be secondary to multiple factors. Thus, an ischemic process and/or disorders determined by the improper evacuation of bile (with or without the presence of gallstones) can be detected at this level. In addition, severe bacterial infections can cause a rapid and sudden onset of the disease. In some young patients, even malformations of the biliary tract can be identified. When the syndrome characterized by acute inflammation of the gallbladder is not associated with the presence of gallstones, the disease is known as acute alithiasic cholecystitis [
17,
18]. Most of the time, the severe forms of acute cholecystitis occur in the elderly population, who usually have multiple associated comorbidities. Yet, in intensive care units, a wide variety of vasoactive agents are often used, which can cause a centralization of the circulation to support vital functions, but which induce a certain degree of peripheral ischemia [
19,
20,
21]. In the case of acute alithiasic cholecystitis, therapeutic principles are similar to the clinical forms that present lithiasis. If the patient's general condition is compatible with cholecystectomy, surgical therapy should generally be performed as soon as possible. Where it is not indicated/ possible, cholecystostomy can be an alternative surgical treatment. This procedure has the role of relaxing the gallbladder, being necessary to be associated with a treatment that includes broad-spectrum antibiotics, with the ability to concentrate and excrete in the bile ducts [
22,
23].
The population over 65 is considered to be (due to the changes taking place in their social and cultural activities) the elderly population. Most of the time such patients are retired and have a less demanding physical and mental activity. In the absence of compensatory activities, some of the patients develop a mild form of depression (caused by loneliness and the feeling of not being able to be useful to society), which makes them stop caring adequately about their health. Another factor that adds to the lack of concern related to the state of health is the absence of regular medical investigations. In the state of retirement, such controls either no longer exist, or are left to the discretion of the person if and when they should be investigated (routinely or for possible pre-existing organic conditions) [
24,
25].
The present study is a retrospective evaluation carried out over a period of 4 years. This study aims to highlight the diagnostic peculiarities of acute cholecystitis in the population over 65 years of age, as well as to identify the best therapeutic approaches. The evaluation was based on data related to the manifestations presented by the patient, etiology and associated symptoms, using the Tokyo criteria as an objective tool in establishing the positive diagnosis and severity of acute cholecystitis.
Results
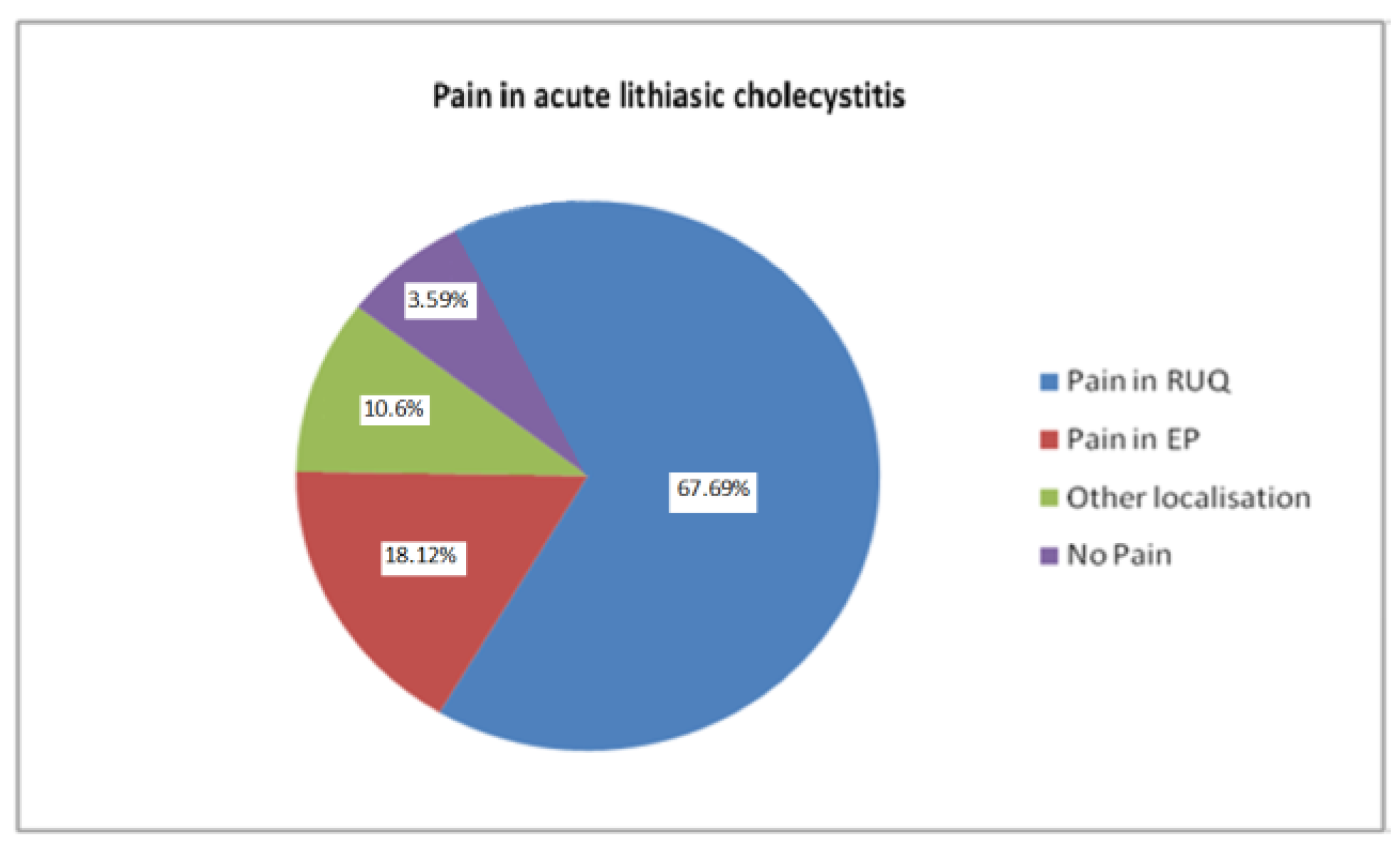
Following the inclusion and exclusion criteria, 585 patients were enrolled, of whom 60.34% were women and 39.66% men, the majority (68.38%) coming from the urban environment, and the remaining patients (31.62%) coming from the rural side. Their ages ranged from 65 to 101 years, with a mean age of 72.83 years. The clinical evaluation found that the classic presentation with pain in the right hypochondrium was the most common (67.69% of patients). 18.12% experienced pain in the epigastrium, 10.6% another pain location, while 3.59% did not experience pain or it could not be clinically objectived (
Figure 1).
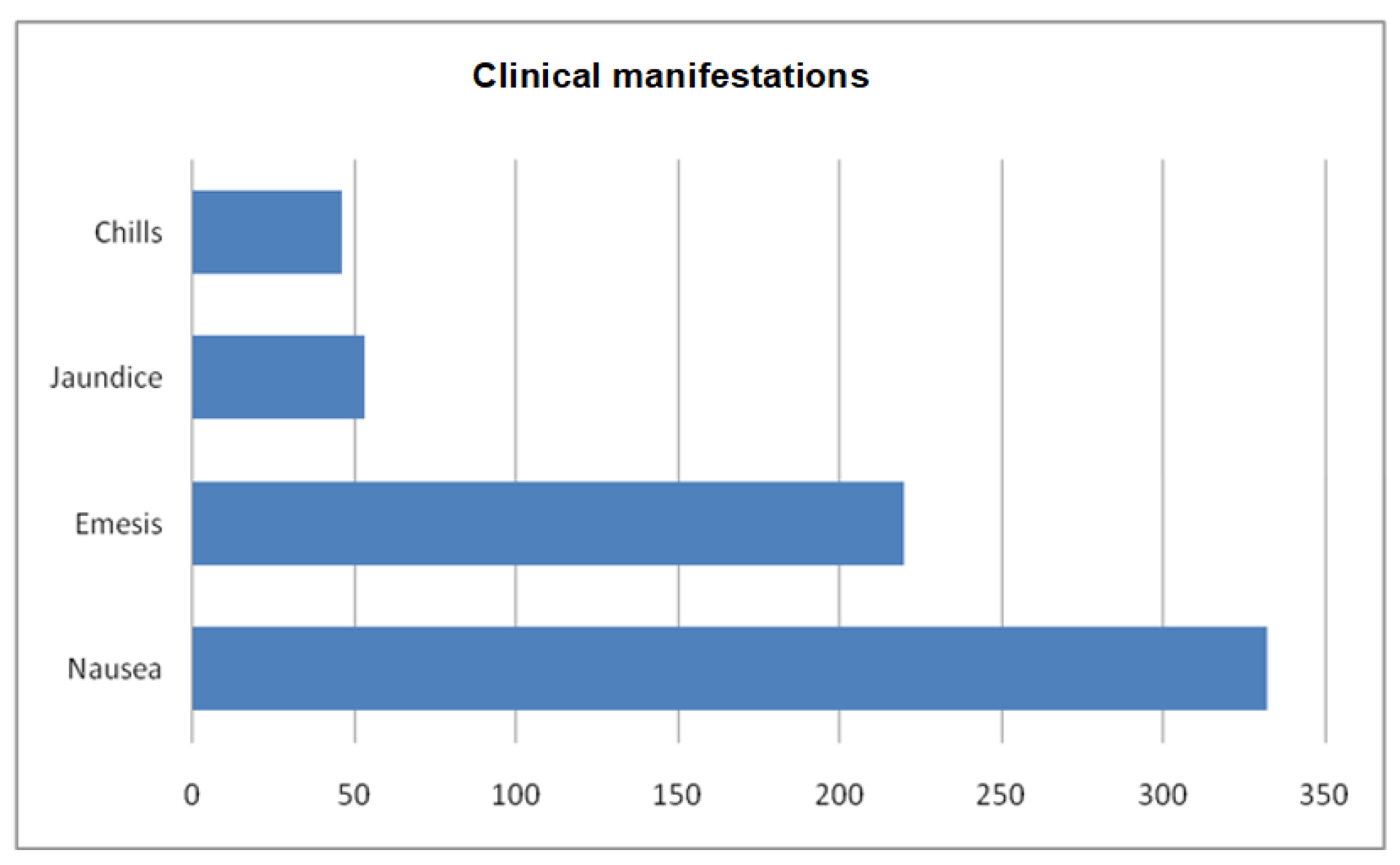
Symptoms associated with pain were: nausea, vomiting, jaundice and chills, as presented in
Figure 2.
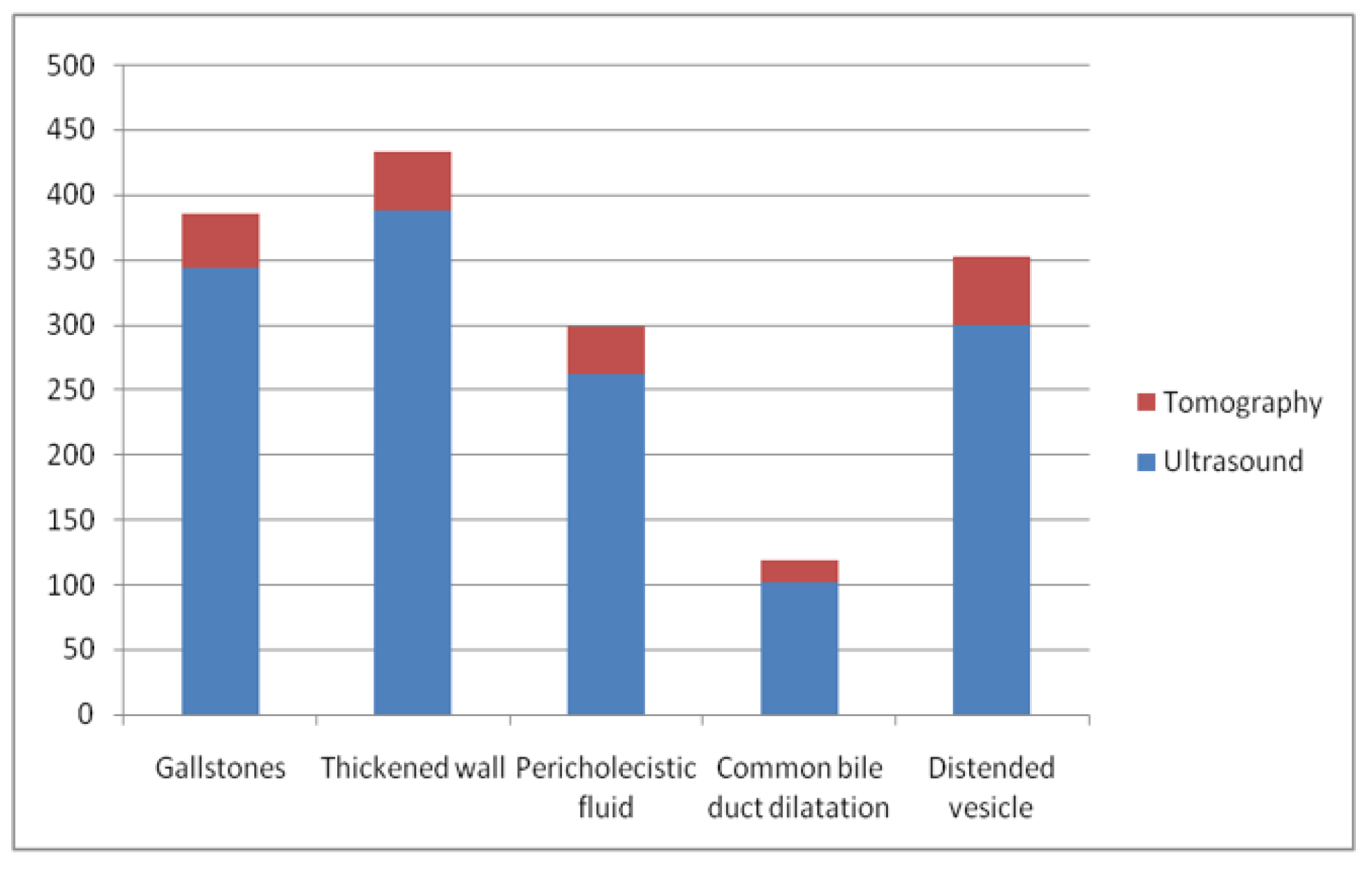
The imaging methods used for the diagnosis of acute cholecystitis were represented by ultrasound in 86.49% of cases, computed tomography in 11.45% of cases and the rest of the patients were investigated by other methods such as MRI, simple abdominal radiography or intraoperative examination (
Figure 3).
The etiology of acute cholecystitis was in more than 91% of cases caused by lithiasis, so that 537 patients (91.79%) presented gallstones in the gallbladder, the remaining 48 patients (8.21%) did not present lithiasis inside the gallbladder or in the bile fluid (during imaging or microscopic examination).
In the present study, patient-related comorbidities had a major impact on therapeutic conduct. Thus, cardiovascular pathology was the most frequently encountered, being primarily represented by hypertension (324 patients had a systolic blood pressure value of over 140 mmHg at the time of admission), atherosclerotic coronary disease (153 patients), atrial fibrillation (in 82 patients), and 78 patients had varying severity degrees of congestive heart failure. Respiratory failure due to the presence of COPD was present in only 15 patients. The presence of elevated blood glucose levels (characteristic of diabetes) was observed in 158 patients. Dementia, secondary to vascular etiology or in the context of Alzheimer's disease, was present in the study population in 23 of the patients (in varying degrees of severity).
The chronic treatment followed by the patients enrolled in the study group was mainly represented by antihypertensives, the most used being beta-blockers (283 having 2 administrations per day, together with statins in 141 patients). Administration of chronic anticoagulant treatment was identified in 90 patients. 82 of them had atrial fibrillation, and the rest had either a history of ischemic stroke (four patients) or a history of pulmonary thromboembolism (in three patients), while one patient was bedridden following a relatively recent orthopedic intervention.
Regarding the severity of the disease at the time of presentation, 60.34% of the patients had a mild form, 31.46% a moderate form and 8.2% a severe form of evolution, in which there was dysfunction of other organs (cardiac, renal or liver) since admission. The treatment methods performed in the study group were represented by laparoscopic cholecystectomy in most patients (61.19% of cases). 33.50% patients underwent open intervention, while 5.31% cases needed simultaneous cholecystectomy and exploration/intervention on the common bile duct (4.63% were fitted with a drainage method with either Kehr tube or transcystic drainage, and 0.68% of patients underwent a biliodigestive diversion).
Regarding the assessment of the severity of acute cholecystitis, 353 patients were included in the I degree of disease severity, only one patient progressing to the II degree after 24 hours of conservative treatment. The etiology in this group was largely represented by the presence of gallstones. The surgical treatment performed by the patients according to the degree of severity is presented in
Table 1.
Discussions
The current study included both patients with a clinical picture suggestive of acute cholecystitis and patients whose symptoms were nonspecific/diminished. The alteration of symptoms was caused by the presence of several factors (neurological damage secondary to diabetic neuropathy or vascular dementia, in the context of Alzheimer's disease, or as a result of late presentation to the emergency room, in a comatose state, when an adequate anamnesis related to comorbidities could not be obtained). The factors that contributed to these forms of presentation are mostly related to socio-economic conditions. Thus, over 60% of hospitalized and treated patients came to the emergency room being brought by the public ambulance system, not having permanent caregivers or constant and/or adequate family support. An extreme of this situation was identified in 4 cases, where the neighbors noticed the lack of activity of the one who lived in the next apartment. They alerted/called the emergency number to report this situation. Ambulance personnel found the elderly person unconscious and extremely dehydrated. Following investigations and treatment, the cause of their decompensation was identified, in the form of severe acute cholecystitis (phlegmonous/ gangrenous, with local complications). After the acute cholecystitis event, the patients were put in touch with their relatives, 14.87% of them receiving permanent postoperative care from them, while the rest were admitted to permanent centers.
A study conducted on the Romanian population revealed that the elderly over 65 have a rather low average income, which would not be able to provide (in addition to basic needs) a permanent assistant or a supervisor, able to recognize in due time a possible onset/decompensation of the disease, which would lead to a faster presentation to the doctor [
30]. Other factors that led to the atypical presentation of patients with acute cholecystitis are represented by immunosenescence, some of the patients even being in the context of a severe systemic disease. Other patients were under complex multidrug treatment, in some cases including a sedative/hypnotic. All this, together with the psychiatric changes of elderly patients, can influence the sensation of pain and the awareness of the state of health in which they are [
31]. Thus, in a group of patients from Romania aged between 55 and 90 years old, major or moderate depression was found in approximately 50% of the cases. This leads to a lower ability to take care of their own health, some of the respondents even refusing to adhere to treatment or to present themselves to health service providers [
32].
The classic presentation with pain in the right hypochondrium was found in most patients whose age was between 65 and 75 years. They had a good level or control of blood pressure and blood glucose, with a p-index <0.001, which represents a strong statistical association. Regarding the etiology of acute cholecystitis, those caused by gallstones had both types of presentation. In 537 patients in whom a gallstone was identified, 63.68% of the cases presented typical pain symptoms, the rest having an atypical pain location, or the pain could not be objectified or present.
Acute alithiasic cholecystitis was more commonly identified in patients who had associated cardiovascular disease, most often with inadequate blood pressure control, systemic atherosclerosis, and/or diabetes. This condition was detected in 20 patients who presented to the emergency department, the remaining 14 patients being identified in the intensive care unit. They were treated with digestive rest and prolonged parenteral nutrition, 11 patients requiring vasopressor treatment and orotracheal intubation, while 3 patients underwent major surgery in the recent past. Thus, there was a close connection between acute alithiasic cholecystitis and the presence of patients in the intensive care unit. This correlation was due to microcirculatory changes caused by vasoconstriction (induced by positive inotropic substances or secondary to systemic arteriosclerosis), as well as due to increased blood viscosity secondary to insensible fluid losses in such patients [
33,
34,
35]. Secondary to prolonged parenteral nutrition that puts the digestive system at rest, there is a bacterial overpopulation and atrophy of the mucosa at the digestive level, which causes a decrease in its ability to act as a local barrier. This favors both transient bacteremia (seeding microorganisms in several distant areas) and the decrease in the elimination of bile from the gallbladder (favoring its distension and ischemia, which further accentuates ileus and atrophy of the mucosa). In this way, a vicious circle is established that favors the occurrence of acute alithiasic cholecystitis [
36,
37]. The clinical manifestations of patients with acute alithiasic cholecystitis who presented to the emergency room were represented by the presence of pain in the right upper quadrant, along with nausea, vomiting and dizziness in 17 cases, while 2 patients presented symptoms characteristic of acute surgical abdomen (generalized abdominal pain and peritoneal irritation). A patient was brought to the Emergency Department with a Glasgow Coma Scale of 11, and with apparent pain on palpation of the right hypochondrium. Regarding the diagnosis of patients in the intensive care unit, it was based on the clinic, persistent inflammatory syndrome and fever. Later, through imaging, other possible causes were excluded and gallbladder suffering was identified through the presence of several criteria of acute cholecystitis. In 7 cases an exploratory laparoscopy was required to establish the diagnosis.
In the present study, the treatment of the patients had several components. The first was represented by the conservative drug treatment, which had the role of controlling the infection and inducing a certain degree of remission of the disease, and the second was the surgical treatment as a form of curative therapy.
The main part of the conservative treatment is represented by the administration of antibiotics, which is most often empirically/statistically established (cultures taken from the patients' gall bladder show a wide range of microorganisms). Thus, among the gram-negative bacteria isolated, the most frequently encountered are Escherichia coli and Klebsiella spp., causing infections in up to 88% of patients. Relatively similar infection rates were found with enterococci and streptococci, which are some of the most common gram-positive germs [
38].
Particular attention should be paid when concomitant disorders of the biliary tract are encountered. In addition to the broad spectrum of antimicrobials, the antibiotic must penetrate well into the affected tissue. In the case of acute cholecystitis, it is necessary to choose an antibiotic that concentrates at the biliary level, thus obtaining local bactericidal concentrations by administering small systemic doses of the antibiotic [
39,
40]. Beta-lactams represent a class of antibiotics that cover all these therapeutic requirements. Ampicillin or amoxicillin in combination with sulbactam have both a broad spectrum against gram-positive bacteria and a good concentration in the biliary tract [
41]. For gram-negative bacteria, piperacillin-tazobactam or third- or fourth-generation cephalosporins are preferred as first-line treatment [
42].
In the present study, after the diagnosis of acute cholecystitis and its classification in degrees of severity, antibiotic treatment was initiated. If patients met the criteria for sepsis, antibiotic treatment was initiated immediately, along with the other treatment components of severe inflammatory response, adequate hydration, and maintenance of a mean blood pressure above 90 mmHg. The first choice of antibiotic therapy for grades I and II severity of acute cholecystitis was the combination of amoxicillin 1000 mg with clavulanic acid 200 mg every 8 hours. The dynamic evolution of temperature and degree of local pain were monitored, while leukocytosis and C-reactive protein were re-evaluated after 24 hours. In combination with antibiotic treatment, analgesics (to achieve good pain control), non-steroidal anti-inflammatory drugs, proton pump inhibitors and antiemetics should be administered.
If the patient evolved with an increase in temperature and pain, and humoral with an increase of more than 50% in inflammation markers or the appearance of an organ failure, the antibiotic regimen was changed. Thus, Piperacillin 4g in association with Tazobactam 0.5g was administered once every 8 hours, while the surgical intervention was performed as soon as the general condition of the patient allowed it.
For the severe form of cholecystitis, the first antibiotic treatment recommendation was Ceftriaxone 2g in the first hour after admission to the surgery department. If the patient's condition did not improve within the next 4 hours, he was transferred to the operating room for emergency surgery.
The surgical treatment in the present study included several surgical techniques. Laparoscopic cholecystectomy was performed according to the American technique (with the installation of 3 working trocars and an optical trocar), while classic cholecystectomy was performed through a right subcostal incision. If complications such as cholecysto-choledochal fistulas, cholecysto-duodenal fistulas, choledochal lithiasis, angiocholitis (or other intraoperative events) were identified intraoperatively, the intervention also aimed at solving them (when possible), or they were solved in a secondary operator time.
Regarding laparoscopic cholecystectomy, this is currently the gold standard of treatment, being indicated in over 75% of patients with mild acute cholecystitis [
43,
44,
45]. In the current study, it was performed in 73.09% of cases, with several factors that led to this result being identified. Thus, 4 patients out of the 353 were hospitalized between May 2020 and July 2020, being tested positive for SARS-COV 2 infection. According to the provisions developed by the Romanian Ministry of Health, laparoscopic interventions would generate aerosols with a higher risk of respiratory infection to the medical staff, which is why open intervention was recommended in such cases. Another factor that led to lower rates of performing laparoscopic cholecystectomies was represented by the anticoagulant treatment administered to 2 of the patients, 10 and 14 hours before the intervention. Considering that there is an increased risk of bleeding, classic cholecystectomy was performed in order to have a better control of possible bleeding events.
Intraoperative exploration of the abdomen and gall bladder was a useful tool of diagnosis. 331 of the patients were confirmed intraoperatively with acute edematous cholecystitis. 22 patients were preoperatively classified as severity I degree, without organ dysfunction or accentuated inflammatory syndrome (the average leukocytosis of these patients being 12,543). However, in 5 cases it was observed intraoperatively that the walls of the gallbladder showed areas of uneven ischemia with a tendency to spontaneous effusion, while 17 out of 22 patients presented a gallbladder with a much-increased volume and significant adhesions to adjacent organs. The 5 patients described above were all men with a chronic history of atherosclerosis, and 2 of them also had elevated blood glucose levels. Consequently, the microvascular damage also contributed to the reduced clinical and paraclinical form of manifestation in these patients.
The patients in the study group who were assessed as having a moderate degree of acute cholecystitis were a heterogeneous group. Out of the 184 subjects, 12 patients did not present stones in the gallbladder or in the bile ducts.
The basic therapeutic procedure of patients with moderate severity of acute cholecystitis was mainly represented by laparoscopic cholecystectomy (93 cases). Thus, intraoperatively, 48 cases of acute edematous cholecystitis were identified, 27 cases with empyema located at the level of the gallbladder, and in the remaining 18 cases, areas of irregular necrosis at the level of the gallbladder wall were identified. In these last cases there were 6 patients who required conversion. In 4 cases the cystic duct could not be identified safely, so the risk of a lesion located on the common bile duct was high. In one patient a blood vessel injury occurred during Callot triangle dissection due to the presence of an aberrant right hepatic artery that was tractioned by the inflammatory process (requiring vascular suture under distal and proximal control), and in 1 patient conversion was required due to the occurrence of unforeseen technical problems.
Classic cholecystectomy was indicated in patients with moderate severity in proportion of 41.84% (77 cases). In these patients, acute cholecystitis was identified in different forms: edematous (34 patients), gangrenous (17 patients) and cholecystic empyema (in the remaining 26 patients). In the case of the 17 patients with acute gangrenous cholecystitis, 8 did not present gallstones, being admitted to intensive care, with positive intraoperative support, following acute events. These acute events were represented by: acute myocardial infarction with low ejection fraction (3 patients), one patient with ischemic stroke and 4 patients with polytrauma due to a road accident whose injury balance included diffuse axonal injuries, open fractures of the lower limbs and severe pulmonary contusion. The other 9 patients had an important neurological history: senile dementia or in the context of Alzheimer's disease (not being able to communicate effectively with family members or medical staff), diabetes and peripheral atherosclerosis, while 3 of them suffered minor amputations in the lower limbs.
Exploration of the common bile duct/CBD was necessary when choledocholithiasis was associated and the other methods failed to achieve good patency of the common bile duct. Also, CBD exploration was performed in an emergency situation that associated angiocholitis, as well as in elective patients (after stabilization by drug treatment) laparoscopic exploration was used for patients with a good general condition, to verify the condition of the main bile duct affected by lithiasis. After releasing tension from the bile duct, the surgeon has several options, such as: primary closure of the common bile duct, T-tube placement, or anastomosis [
46,
47,
48]. The exploration of the common bile duct was performed in 13 patients from the group of those with a moderate form of the disease, of which 12 presented jaundices (average direct bilirubin being 5.12 mg/dl), high fever (38.3
0C) and high clinical suspicion of cholangitis. After performing the imaging investigations, dilation of the common bile duct and the presence of migrated stones were detected, emergency surgery was chosen as the therapeutic method given their severe condition.
During the exploration of the peritoneal cavity, an important inflammatory mass consisting of the gallbladder, omentum and transverse colon was identified, which required a difficult dissection that revealed a dilated common bile duct. This aspect was observed in 6 of the cases; after performing the cholecystectomy, a cloudy, purulent bile flow was observed that required intraoperative cholangiography. This procedure revealed the presence of a large calculus embedded in the distal portion of the duct. Due to the inflammation of the structures around the common bile duct and the altered general condition of the patients, the transcystic drainage method was chosen. Evacuation of bile through the T-tube was done in 5 cases, in 4 of the patients because of the increased size of the stones that could not be evacuated by another method. In the fifth case, the presence of a stricture of the common bile duct in the supraduodenal portion was noted. In all five cases, the cholangitis was caused by mechanical obstruction, which led to an inflammatory process around the adjacent structures further generating friable adhesions.
In the two patients in whom anastomoses were performed, lesions of the main bile duct caused by inflammation were found. This determined the creation of a cholecysto-choledochal fistula, which required a hepato-jejunal anastomosis as a therapeutic solution.
Regarding the patients classified in the third degree of severity, with newly established organ dysfunction, laparoscopy was used as a therapeutic method in only 7 cases, all of these patients being detected intraoperatively with gangrenous acute alithiasic cholecystitis. The biological profile of these patients is defined by the presence of elevated blood glucose values, positive inotropic treatment administered in the intensive care unit, and the presence of systemic atherosclerosis. Five of these patients had a history of acute myocardial infarction, stroke or infrainguinal occlusive disease. Initially, these patients underwent diagnostic laparoscopy because the cause of the developed organ failures could not be identified and medical treatment failed to improve the general condition of the patients.
The open approach was the most used, because 16 of the patients presented with a surgical abdomen, but without associating the pneumoperitoneum. Among these, in 9 cases the presence of bile in the peritoneal cavity was identified, due to the perforation of the gallbladder as a result of a process of ischemia and gangrene at this level. In the rest of the patients, acute pyocholecystitis with local accumulation of pus that disseminated in the peritoneal cavity was found.
Exploration and instrumentation of the common bile duct was common in this subgroup of patients. Its drainage through the cystic duct was the most frequently used procedure, because it is a fast method of evacuation of purulent bile in the case of association of a severe acute lithic cholecystitis with a cholangitis. T-tube use was required in only 4 patients. Two of them had large stones embedded at the cysto-choledochal junction that could not be extracted by other methods, and the others two had an abnormal communication between the common bile duct and the gallbladder.
Biliodigestive anastomoses were used only in 3 particular cases. Two patients presented necrosis of the common bile duct secondary to the fulminant inflammatory process and faceted stones, which traumatized the main biliary tract (hepato-jejunal anastomosis being required as a last therapeutic solution). One patient had acute cholecystitis as well as clinical and paraclinical diagnostic criteria for angiocholitis. Transcystic laparoscopic drainage was initially decided, but during cannulation of the cystic stump the common hepatic duct was injured. This required the creation (by open approach) of an anastomosis between the right and left hepatic ducts and a jejunal loop.
Mortality rates for our study were 5.12%. Most of the patients were diagnosed with a severe form of acute cholecystitis, the cause of death being represented by multiple organ failure in 18 patients, and bronchopneumonia associated with prolonged ventilation in 5 cases. Acute myocardial infarction and ventricular tachycardia caused death in 4 and 3 patients respectively, their average age being almost 81.4 years.
The current study is a retrospective evaluation which, although performed on a large group of patients, has some limitations. Thus, some of the patients enrolled in the study live in an urban environment, where physical activity, food profile and access to health services are different from the rural area. In the rural environment, physical activity is significantly present even among the elderly population, and the diet is based on own/local production that has a better quality (it is less likely to develop cardiovascular diseases and gallstones due to unhealthy eating) [
49,
50]. Conversely, in the urban environment, physical activity is limited and the quality of food is lower. Another limitation is that this evaluation is a single-center study, which cannot incorporate all patient characteristics from the entire region of the country.