Abstract
Post-partum depression is one of the most severe types of depression and can be developed at any age, no matter of cultural of social status. Objectives. To determine the factors associated with the psychological impact of pregnancy and to emphasize the psychological and psychiatric risks after giving birth for a woman. Materials and Methods. The study enrolled 35 patients diagnosed with postpartum depression that have been hospitalized in a tertiary-care center for psychiatric disorders between 2016 and 2020. Data were collected from patients’ observation charts. Results. The incidence of postpartum depression is higher in the age range 30-45 years old for primiparous women who are from urban areas, unemployed and not integrated in a family (unbalanced families or single parents), with medium level of education (high school) and alcohol addiction. One of 35 patients committed infanticide. Conclusions. Even if the postpartum depression is known worldwide it is still underdiagnosed, with certain factors concurring to that. Postpartum depression requires the identification of risk conditions in pregnant women and individualized therapy in a patient-centered, holistic manner.
Introduction
Postpartum depression is the most studied puerperal disorder in psychiatry [1]. During pregnancy and childbirth, major endocrine changes bring with them normal psychological modifications in women, but sometimes these changes take the form of pathological, neurotic or psychotic mental disorders [1].
Postpartum depression refers to a major depressive episode that occurs during or shortly after pregnancy (within four weeks after delivery), and it is not considered a distinct illness. Negative parenting practices, marital conflict, poor maternal-infant bonding, breastfeeding difficulties, and adverse outcomes in the child's physical and psychological development are all potential consequences of postpartum depression. Remission of symptoms, on the other hand, reduces the risk of psychiatric and behavioral problems in the child [2].
More and more women choose to hide their symptoms and do not seek specialized help to maintain their social integrity, not to be blamed by the people around them or to be accused of not being able to take care of their own child [1]. This is the reason why it is necessary to use a method of prevention, especially in pregnant women who, following the anamnesis, present risk factors of the occurrence of postnatal depression (history of anxiety-depressive disorder, lack of family or social support network, precarious economic status or level of instruction and education) [1].
Early detection is a crucial step in addressing maternal mental disorders during the postpartum period. To screen for postpartum depression, primary care settings typically employ the Edinburgh Postnatal Depression Scale. This 10-item self-report measure was specifically developed for use in community samples of postpartum mothers and involves women choosing one of four responses (scored 0 to 3) to indicate the extent to which each statement corresponds to their mood over the past 7 days. The total score is calculated by summing up the item scores, with higher scores indicating more depressive symptoms. The Edinburgh Postnatal Depression Scale has proven to be an effective tool for identifying postpartum depression in women [3].
A woman`s transition to motherhood is a period that includes an increased level of psychological vulnerability and in the case of some women this can generate a lot of stress and can be a complicated process [4].
A reconceptualization of the role of the mother from the perspective of pregnant women susceptible to developing postpartum depression is necessary and can be achieved by normalizing this concept in relation to the various experiences of future mother (single women, women who have a psychiatric history or those who struggle with certain addictions), social stigma having a greater negative effect on them.
The association of pharmacological therapy with psychotherapy leads to superior therapeutic results. Psychotherapy in a pluralistic approach is free from adverse reactions and at the same time there is no risk of refusal or abandonment of therapy by patients who will cite as a reason the passage of antidepressant drugs to the fetus through milk [5].
We proposed this theme for study because the trends of postpartum depression are worrying, the condition being a main cause of disability both locally and worldwide. Worldwide, postpartum depression has been reported in almost 10–20 % of mothers. The prevalence of postpartum depression in low-middle income countries is the highest (20.14%) in comparison with upper-middle- and high-income countries. One in seven women experiences peripartum depression [6,7].
Our study aims to assess the incidence rate of women who have experienced postpartum depression and have sought specialized help to overcome the depressive crises they face, to determine the differences in incidence according to the age of the patients, the environment from which they come, the standard of living and the level of education, the reasons why they presented to the doctor and the symptoms that appeared during the hospitalization, but also depending on the treatment and recommendations they received up to that time.
Materials and Methods
The study was approved by the Review Board of the hospital where we conducted the study. Our study is a non-interventional study, which respects the confidentiality requirements imposed, the rights of patients according to the Helsinki Declaration on Patient Research, and compliance with the processing of personal data provided by Law no. 190/2018.
Type of study. The study is a retrospective observational study, which includes cases of postpartum depression diagnosed and hospitalized at „Elisabeta Doamna” hospital of Psychiatry from Galati in the period 2016-2020.
Inclusion criteria were: women at reproductive age 18 and 45, diagnosis of postpartum depression, hospitalized patients.
Exclusion criteria were: age less than 18 years (this being the official age limit for an adult) or older than 45 years, patients with no previous history of depression or other mental disorders.
Sources and methods of data collection: The data was obtained by studying the observation charts of patients who were admitted in the hospital and the computer database of the study hospital.
We analyzed clinical and anamnestic data such as age of the patients, the environment from which they come, the standard of living and the level of education, marital status, employment status, smoker status and alcohol use.
Statistical analyses were performed with SPSS (Statistical Package for the Social Sciences) and Microsoft Excel version 12 for Windows. Results were expressed as numbers and percentages.
Results
The results were obtained following a 5-year study which enrolled inpatients from a tertiary-care center for psychiatric disorders, who developed postpartum depression. Data were centralized in the form of tables and graphs. A number of 35 patients diagnosed with postpartum depression were included, the average number of cases of postpartum depression in the study period being 7 cases per year (Figure 1).
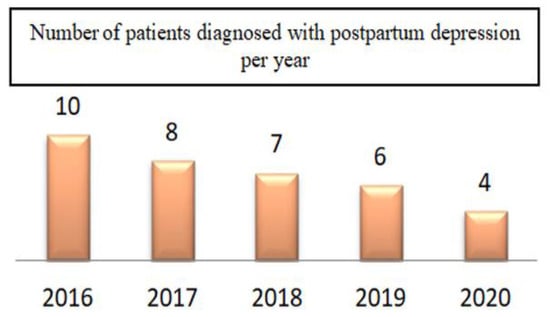
Figure 1.
Incidence of patients diagnosed with postpartum depression in the period 2016 – 2020.
The mean age of the patients was 35, ranging from 21 to 45 years. A maximum incidence has been observed in patients aged between 30 and 45 years (Figure 2).
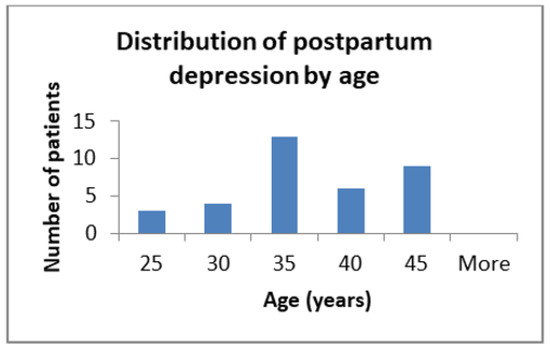
Figure 2.
Distribution of postpartum depression by age.

Table 1.
Main characteristics of the study population.
Table 1.
Main characteristics of the study population.
| Parameter | Number | Percentage |
| Environment (urban) | 19 | 54,3% |
| Marital status (married) | 17 | 48,6% |
| Employment status (employed) | 9 | 25,7% |
| Level of education | ||
| First cycle | 8 | 22,9% |
| High school | 19 | 54,3% |
| Higher levels | 8 | 22,9 |
| Primiparous women | 21 | 60% |
| Active smokers | 17 | 48,6% |
| Alcohol consumers | 20 | 57,1% |
Statistics on patients’ backgrounds showed a higher ratio of patients from urban to rural areas (54.3% vs. 45.7%).
Regarding living conditions, it was observed that depressive disorder was frequently diagnosed, in a proportion of about 48%, in patients living with the family. Next in line are the single mothers, in a proportion of 37%. 43% of all patients are unemployed. 26% of the studied patients that developed postnatal depression were employed mothers who were paid and had a stable job.
From the level of education perspective, 43% have high school education, followed by mothers who graduated only the primary education cycle, in percentage of 22.9%, on the third place being those with higher education levels in percentage of 20%.
In our study, the results showed that 60% of mothers who give birth to their first child developed postpartum depression and have severe symptoms. 49% of the mothers participating in our study who developed this pathology were frequent or occasional alcoholics, and 57% of them were active smokers during pregnancy.
The symptoms in women who took part in this study range from seemingly simple to severe symptoms, such as suicidal ideation or infanticide.
As seen in Table 2, the predominant symptom, which the patients diagnosed with postnatal depression most frequently accused, was depressive mood. Over 77% of the women included in the study felt, during pregnancy and after giving birth to their children, a depressive state associated with episodes of insomnia (65.71%), sadness and anhedonia (60%).

Table 2.
Incidence of symptoms associated with depression.
23% of women included in the study fought about the idea of suicide. 14% stated that they had faced the idea of infanticide, and one of these mothers, whose symptoms worsened and who had frequent ideas of infanticide, developed postpartum psychosis and killed her baby.
57% of the women included in our study experienced agitation in the postpartum period, which affected their relationship with those around them but also with their babies, inducing agitation in them as well. As seen in Figure 3, of the mothers who experienced psychomotor agitation, 35% associated this condition with involuntary tremor, irascibility (65%), delusional ideas (30%) and temporal-spatial disorientation (40%).
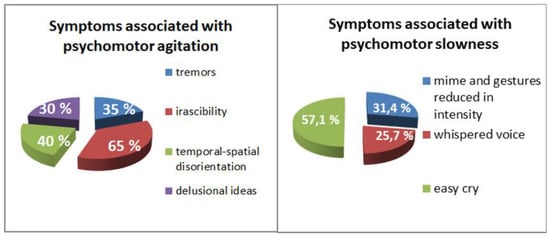
Figure 3.
Symptoms associated with psychomotor agitation (left). Symptoms associated with psychomotor slowness (right).
In patients who did not show psychomotor agitation, the changes were manifested by slowness. Approximately 31% of new mothers showed psychomotor slowness associated with a whispered voice (25.7%), 31.43% facial expressions and gestures diminished in intensity and easy crying 57.14%.
97% of the women who took part in the study received antidepressant medication. Breast-feeding was discontinued in patients receiving psychiatric treatment. 94% of the women had antidepressant and anxiolytic treatment in combination, and 60% of the patients received antipsychotic treatment, as well as hypnotic treatment.
Only 40% of women diagnosed with postpartum depression associated drug treatment with psychotherapy.
Discussions
In this study a very low incidence of postpartum depression was found. We believe that the prevalence of postpartum depression, discovered in our study, is not representative of the magnitude of the problem. In our country, postpartum depression is an underdiagnosed condition due to the low level of support and social stigmatization and differences in socio-economic environments (poverty, nutrition, stress). Another cause of the underdiagnosis of postpartum depression in our country is the lack of screening and encouragement programs for the new mothers.
Since our study includes a year from the Coronavirus disease (COVID-19) pandemic period, in which hospital presentations were low, we can assume that the COVID-19 pandemic was also a factor that led to the decrease in the incidence of postpartum depression diagnosis.
According to a study conducted in 2006 in the USA, the diagnosis rate of postpartum depression depends on the economic level of the country, the level of the education of the women, in less developed countries, both economically and socially, this condition is underdiagnosed [8].
Due to the low level of information of young women, they present themselves to the psychiatrist less often, the condition being underdiagnosed among them [9,10].
We can assume that a pregnancy occurring at a young age or at an advanced age can come with the thought that the mother will not be able to handle the responsibilities that come with a child.
Comparing the results of our study of the distribution of cases by age with the results of a study conducted in Saudi Arabia in 2020, we found similar results, the ratio of occurrence of postpartum depression being over 60% for age categories between 30 and 45 years, women belonging to this age category being much more responsible and more interested in their health, so they go to the doctor for diagnosis and treatment [11].
When we discuss the environment of origin, we observe similar results to those in our study in a study conducted in Canada in 2013, showing that the higher prevalence of postpartum depression was in the case of women living in urban areas compared to those coming from rural areas, because in rural areas, was a nonsignificant gradient of risk: women with less connection to larger urban centers were at lower risk of postpartum depression than women in areas with greater connection [12].
As shown in other studies as well, conditions such as metabolic disorders, stress caused by work and living conditions, could be factors that may determine the difference between the number of cases from the two environments [12,13].
Metabolic analyses indicate that mothers diagnosed with postpartum depression have higher levels of serum oxidative stress-related metabolites, such as adenylosuccinate, glutathione-disulfide, and Adenosine triphosphate, eight weeks after delivery. Additionally, at six weeks postpartum, these mothers exhibit changes in uric metabolites linked to amino acid metabolism, neurotransmitter metabolism, and bacterial populations. These findings suggest a potential link between metabolic disturbances and postpartum depression. The identification of specific metabolic markers may aid in the early detection and treatment of postpartum depression. Further research is needed to better understand the relationship between metabolic changes and postpartum depression [14,15].
We observe that women living with their families were the most diagnosticated, family members observing the behavioral changes of new mothers and giving them the necessary support to seek specialized help. Next category of most diagnosticated women with postpartum depression are single mothers, who are interested in their mood and how it affects the baby's life, this fact determining them to seek the help of a psychiatrist. The fewest diagnoses are given to mothers who live with either their concubines or their parents, who neglect their condition and avoid providing them with the necessary support to recognize the symptoms.
Regarding financial conditions we can see a higher rate of occurrence of postpartum depression among mothers without a job, the possible trigger of depression being the stress they endure thinking that they will not be able to support themselves financially and that they will not be able to fulfill their maternal pregnancy at the level they expected.
The correlation between the birth of the first child and the development of postnatal depressive syndrome has been intensively studied and demonstrated in numerous studies [16,17,18]. This is due to the obsessive thoughts that the mother will not be able to cope with a child and will not be able to face this challenge, therefore ending up enjoying less her own baby and see motherhood as a torment. One study conducted in 2012 in Germany showed that over half of mothers who developed postpartum depression were pregnant with or had their first child [19,20]. Comparing the data from our study with that from the study mentioned above, we observed that the trend is the same, 65% of the patients diagnosed being primiparous.
Also, alcohol consumption is an important risk factor. The results of our study show an approximately equal ratio between women who consume alcohol during pregnancy and lactation and those who did not. One study conducted in 2021 in China showed that maternal alcohol consumption is significantly associated with the risk of developing postpartum depression [21]. These results emphasize the necessity of enhancing health awareness, improving the public health policies and regulations concerning alcohol use, and strengthening the prevention and intervention of maternal alcohol consumption to promote maternal mental health [21].
Alcohol-consuming mothers motivated that this addiction helped them get through the hardships of pregnancy and postpartum period more easily, being happier and calmer after drinking alcohol, not thinking about the consequences after giving birth to the fetus.
Depressive symptomatology is complex and women can experience these symptoms even during pregnancy, but if their attending physician does not properly monitor them or if the family neglects and associates the pregnant woman's feelings only with hormonal changes during pregnancy, without taking into account that she may suffer from depression, the disorder is discovered only after birth when it is already in a rather severe form, which is more difficult to respond to treatment and can develop into psychosis [22,23,24].
Based on our results, we can observe that depressive symptoms are often exacerbated, sometimes unexplained, affecting the mothers most of the day, but also the relationship with those around them. Thoughts of death or suicidal ideation appeared in mothers with postpartum depression as a possible solution and a reasonable alternative to get rid of the feelings that were crushing them and the stress of the new responsibility, on average about 23% of women included in the study fought about the idea of suicide. 14% stated that they had faced the idea of infanticide, and one of these mothers, whose symptoms worsened and who had frequent ideas of infanticide, developing postpartum psychosis, killed her baby. A study of 706 new mothers with postpartum depression in Brazil in 2020 shows that about 15% of them had suicidal thoughts, and statistics show that age, working and living conditions, the way they gave birth to their children, their gender or alcohol abuse did not play a significant role in the risk of suicide. The authors of the study concluded that the increased risk of suicide is associated with primiparity, personal psychological history, severe episodes of mood swings, and separation from partners [25].
It is important to note that when the mother has psychotic symptoms accompanied by recurrent thoughts of death or infanticide, she should be separated from the fetus [26].
We observed that some women included in our study experienced symptoms associated with psychomotor slowness such as: easy cry, whispered voice, reduced facial expressions and gestures. A study published in 2015, shows that in a percentage of 80%, women who reported the frequent occurrence of crying episodes and who, in addition, did not benefit from the support of their life partner, presented a much higher risk of onset of postpartum depression [27].
An important role in early diagnosis of postpartum depression may have biological markers such as serum serotonin. As a further discussion it might be taken into consideration as a screening factor for all pregnant patients and it also can be used as a surveillance marker in correlation with the anxiety and depression scales for the entire perinatal period [28,29,30].
Studies confirm the benefits obtained by initiating psychotherapy interventions in addition to pharmacological treatment [31]. Studies show that problem-solving therapy is effective in the care of mothers prone to postpartum depression [32]. The method of applying this type of therapy also includes the use of motivational interviewing [33] as a working tool for acceptance, understanding and involvement in the role of mother (“good mother”) and maybe will reduce the problems a mother will encounter after birth.
It is recognized that pharmacological therapy (antidepressants and hormonal preparations) combined with psychotherapy leads to superior therapeutic results [34,35,36]. The major obstacle in the case of pharmacological therapy is that the drugs pass to the fetus through breast milk and many mothers are reluctant to this treatment indication [37]. In contrast, psychological and social therapies are devoid of adverse reactions and allow a holistic approach based on solving problems [38,39,40].
This article performs a complex evaluation of risk-factors associated with postpartum depression ranging from women’s age, environment, marital status, socio-economic status, noxius habits, etc. It also closely analyses the types and severity of symptoms which occurred.
However, the study’s main disadvantage was the limited number of patients and reduced statistical power. More complex statistical analyses were not possible because of the limited sample.
Conclusions
The profile of the patient with postpartum depression as depicted in our study can be defined as: primiparous woman, aged 30-45 years, from the urban area, who either lives with the family (but does not benefit from its support) or single mother, with medium level of education (high school), with a psychiatric history before birth (anxiety, depression), without occupation or employed, consuming ethanol and tobacco. Symptoms ranged from mild to severe, including forms of psychosis and suicidal and infanticide thoughts. A very low incidence of postpartum depression was found, which most probably does not reflect the reality, but the delicate problem of underdiagnosis.
In conclusion, postpartum depression requires the identification of risk factors in pregnant women and the individualized choice of therapy in a patient-centered, holistic manner, in with psychotherapy acts from a dual perspective, therapeutic and supportive, complementing or acting independently depending on the psychological profile of the pregnant woman and the situational context.
Highlights
- ✓
- Postpartum depression was more frequent in primiparous women, aged 30-45 years, from the urban area, either who live with the family (but do not benefit from its support) or single mothers, with medium level of education (high school), with a psychiatric history before birth (anxiety, depression), consuming ethanol and tobacco.
- ✓
- Symptoms ranged from mild to severe, including forms of psychosis and suicidal and infanticide thoughts.
- ✓
- A very low incidence of postpartum depression was found, which most probably does not reflect the reality, but the delicate problem of underdiagnosis.
Compliance with ethical standards
Any aspect of the work covered in this manuscript has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Conflict of interest disclosure
There are no known conflicts of interest in the publication of this article. The manuscript was read and approved by all authors.
References
- Qi, W.; Wang, Y.; Li, C.; et al. Predictive models for predicting the risk of maternal postpartum depression: A systematic review and evaluation [published online ahead of print, 2023 Apr 19]. J Affect Disord. 2023, 333, 107–120. [Google Scholar] [CrossRef] [PubMed]
- Low, S.R.; Bono, S.A.; Azmi, Z. The effect of emotional support on postpartum depression among postpartum mothers in Asia: A systematic review [published online ahead of print, 2023 Apr 18]. Asia Pac Psychiatry. 2023, e12528. [Google Scholar] [CrossRef]
- van der Zee-van den Berg, A.I.; Boere-Boonekamp, M.M.; Groothuis-Oudshoorn, C.G.M.; Reijneveld, S.A. The Edinburgh Postpartum Depression Scale: Stable structure but subscale of limited value to detect anxiety. PLoS One. 2019, 14, e0221894. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, J.; Shuai, H.; et al. Mapping global prevalence of depression among postpartum women. Transl Psychiatry. 2021, 11, 543. [Google Scholar] [CrossRef]
- Milgrom, J.; Gemmill, A.W.; Ericksen, J.; Burrows, G.; Buist, A.; Reece, J. Treatment of postnatal depression with cognitive behavioural therapy, sertraline and combination therapy: a randomised controlled trial. Aust N Z J Psychiatry. 2015, 49, 236–245. [Google Scholar] [CrossRef]
- Hofheimer, J.A.; McGowan, E.C.; Smith, L.M.; et al. Risk Factors for Postpartum Depression and Severe Distress among Mothers of Very Preterm Infants at NICU Discharge [published online ahead of print, 2023 Apr 18]. Am J Perinatol. 2023. [Google Scholar] [CrossRef]
- Davé, S.; Petersen, I.; Sherr, L.; Nazareth, I. Incidence of maternal and paternal depression in primary care: a cohort study using a primary care database. Arch Pediatr Adolesc Med. 2010, 164, 1038–1044. [Google Scholar] [CrossRef]
- Halbreich, U.; Karkun, S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J Affect Disord. 2006, 91, 97–111. [Google Scholar] [CrossRef]
- Di Florio, A.; Putnam, K.; Altemus, M.; et al. The impact of education, country, race and ethnicity on the self-report of postpartum depression using the Edinburgh Postnatal Depression Scale. Psychol Med. 2017, 47, 787–799. [Google Scholar] [CrossRef]
- Zhang, X.; Zuo, X.; Matheï, C.; et al. Impact of a postpartum care rehabilitation program to prevent postpartum depression at a secondary municipal hospital in Qingdao China: a cross-sectional study. BMC Pregnancy Childbirth. 2023, 23, 239. [Google Scholar] [CrossRef]
- Al Nasr, R.S.; Altharwi, K.; Derbah, M.S.; et al. Prevalence and predictors of postpartum depression in Riyadh, Saudi Arabia: A cross sectional study. PLoS One. 2020, 15, e0228666. [Google Scholar] [CrossRef]
- Vigod, S.N.; Tarasoff, L.A.; Bryja, B.; Dennis, C.L.; Yudin, M.H.; Ross, L.E. Relation between place of residence and postpartum depression. CMAJ. 2013, 185, 1129–1135. [Google Scholar] [CrossRef] [PubMed]
- Villegas, L.; McKay, K.; Dennis, C.L.; Ross, L.E. Postpartum depression among rural women from developed and developing countries: a systematic review. J Rural Health. 2011, 27, 278–288. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, Z.; Vlaikou, A.M.; Theodoridou, D.; et al. Unraveling the Serum Metabolomic Profile of Post-partum Depression. Front Neurosci. 2019, 13, 833. [Google Scholar] [CrossRef]
- Sandu, C.; Bica, C.; Salmen, T.; et al. Gestational diabetes - modern management and therapeutic approach (Review). Exp Ther Med. 2021, 21, 81. [Google Scholar] [CrossRef]
- Silverman, M.E.; Reichenberg, A.; Savitz, D.A.; et al. The risk factors for postpartum depression: A population-based study. Depress Anxiety. 2017, 34, 178–187. [Google Scholar] [CrossRef]
- Loghin, M.G.; Gorescki, P.G.; Sima, R.M.; Pleș, L.; Balan, D.G.; Paunica, I.; Bălălău, O.D. The obstetrical management of HIV-positive pregnancy. J Mind Med Sci. 2022, 9, 111–117. [Google Scholar] [CrossRef]
- Aslam, M.; Nawab, T.; Ahmad, A.; Abedi, A.J.; Azmi, S.A. Postpartum depression and its clinico-social correlates - A community-based study in aligarh. Indian J Public Health. 2022, 66, 473–479. [Google Scholar] [CrossRef]
- Goecke, T.W.; Voigt, F.; Faschingbauer, F.; Spangler, G.; Beckmann, M.W.; Beetz, A. The association of prenatal attachment and perinatal factors with pre- and postpartum depression in first-time mothers. Arch Gynecol Obstet. 2012, 286, 309–316. [Google Scholar] [CrossRef]
- Socea, B.; Carap, A.; Bratu, O.G.; Diaconu, C.C.; Dimitriu, M.; Socea, L.I.; Bobic, S.; Constantin, V.D. The role of the composite and biologic meshes in the trocar site hernia repair following laparoscopic surgery. Materiale Plastice 2018, 55, 146–148. [Google Scholar]
- Qiu, X.; Sun, X.; Li, H.O.; Wang, D.H.; Zhang, S.M. Maternal alcohol consumption and risk of postpartum depression: a meta-analysis of cohort studies. Public Health. 2022, 213, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Raza, S.K.; Raza, S. Postpartum Psychosis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Valverde, N.; Mollejo, E.; Legarra, L.; Gómez-Gutiérrez, M. Psychodynamic Psychotherapy for Postpartum Depression: A Systematic Review [published online ahead of print, 2023 Apr 8]. Matern Child Health J. 2023. [Google Scholar] [CrossRef]
- Howard, S.; Witt, C.; Martin, K.; et al. Co-occurrence of depression, anxiety, and perinatal posttraumatic stress in postpartum persons. BMC Pregnancy Childbirth. 2023, 23, 232. [Google Scholar] [CrossRef]
- de Avila Quevedo, L.; Scholl, C.C.; de Matos, M.B.; et al. Suicide Risk and Mood Disorders in Women in the Postpartum Period: a Longitudinal Study. Psychiatr Q. 2021, 92, 513–522. [Google Scholar] [CrossRef]
- Trull, T.J.; Vergés, A.; Wood, P.K.; Jahng, S.; Sher, K.J. The structure of Diagnostic and Statistical Manual of Mental Disorders (4th edition, text revision) personality disorder symptoms in a large national sample. Personal Disord. 2012, 3, 355–369. [Google Scholar] [CrossRef]
- Pilkington, P.D.; Whelan, T.A.; Milne, L.C. Maternal Crying and Postpartum Distress: The Moderating Role of Partner Support. J Reprod Infant Psychol. 2016, 34, 64–76. [Google Scholar] [CrossRef]
- Moroianu, L.A.; Cecilia, C.; Ardeleanu, V.; et al. Clinical Study of Serum Serotonin as a Screening Marker for Anxiety and Depression in Patients with Type 2 Diabetes. Medicina (Kaunas). 2022, 58, 652. [Google Scholar] [CrossRef]
- Moroianu, M.; Moroianu, L.A.; Ciubara, A.; Matei, M. Persistent Depressive Disorder: the Clinical Approach of the Patient Associating Depression and Dental Pathology - Case Report and Clinical Considerations. BRAIN. Broad Research In Artificial Intelligence And Neuroscience 2022, 13, 229–238. [Google Scholar]
- Pană, M.; Sima, R.M.; Bălălău, O.D.; Stănescu, A.D.; Pleş, L.; Poenaru, M.O. The quality of sexual life after vaginal surgical interventions. J Mind Med Sci. 2020, 7, 201–205. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Sherbourne, C.D.; Roy-Byrne, P.; et al. Effects of co-occurring depression on treatment for anxiety disorders: analysis of outcomes from a large primary care effectiveness trial. J Clin Psychiatry. 2012, 73, 1509–1516. [Google Scholar] [CrossRef][Green Version]
- Fitelson, E.; Kim, S.; Baker, A.S.; Leight, K. Treatment of postpartum depression: clinical, psychological and pharmacological options. Int J Womens Health. 2010, 3, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Curis, C.; Ciubară, A.B.; Nechita, A.; Nechita, L.; Kantor, K.; Moroianu, A.L. The Role of the Motivational Interview in Treatment Acceptance. Case Report. The Medical-Surgical Journal. 2018, 122, 375–380. [Google Scholar]
- Coca, K.P.; Chien, L.Y.; Lee, E.Y.; Souza, A.C.P.; Hong, S.A.; Chang, Y.S. Factors associated with postpartum depression symptoms among postpartum women in five countries during the COVID-19 pandemic: an online cross-sectional study. BMC Psychiatry. 2023, 23, 171. [Google Scholar] [CrossRef]
- Nakić Radoš, S.; Tadinac, M.; Herman, R. Anxiety During Pregnancy and Postpartum: Course, Predictors and Comorbidity with Postpartum Depression. Acta Clin Croat. 2018, 57, 39–51. [Google Scholar] [CrossRef]
- Moya, E.; Mzembe, G.; Mwambinga, M.; et al. Prevalence of early postpartum depression and associated risk factors among selected women in southern Malawi: a nested observational study. BMC Pregnancy Childbirth. 2023, 23, 229. [Google Scholar] [CrossRef]
- Luo, F.; Zhu, Z.; Du, Y.; Chen, L.; Cheng, Y. Risk Factors for Postpartum Depression Based on Genetic and Epigenetic Interactions. Mol Neurobiol. 2023. [Google Scholar] [CrossRef]
- Wells, T. Postpartum Depression: Screening and Collaborative Management. Prim Care. 2023, 50, 127–142. [Google Scholar] [CrossRef]
- Dimitriu, M.; Pantea Stoian, A.; Roșu, G.; Dan, A.; Caimacan, A.; Zygouropoulos, N.; Pacu, I.; Socea, B.; Ionescu, C.; Gheorghiu, D.C.; Bacalbașa, N.; Cîrstoveanu, C.; Haradja, H.; Gheorghiu, N.; Al-Azawi, A.; Măcău, A.-M.; Pleș, L.; Merlo, E.M.; Settineri, S.; Jacotă–Alexe, F. Postpartum Depression - a serious, dangerous, disabling, extremely frequent condition that is almost completely ignored in Romania. Mediterr J Clin Psychol. 2020, 8. [Google Scholar] [CrossRef]
- Mehedintu, C.; Bratila, E.; Pantea-Stoian, A.; et al. The analysis of weight gain evolution related to presence or abssence og gestational diabetes and associated risk factors in pregnancy and postpartum. Interdiab 2018: Diabetes Mellitus as Cardiovascular Disease, Edited by: Serafinceanu, C.; Negoita, O.; Elian, V. Book Series: International Conference on Interdisciplinary Management of Diabetes Mellitus and its Complications. 2018;735-745.
© 2023 by the author. 2023 Andra Iancu, Valeria-Anca Pietroșel, Teodor Salmen, Cristina Ioana Bica, Ioana Păunică, Liliana Florina Andronache, Florentina Gherghiceanu, Cecilia Curis