Introduction
Severe acute pancreatitis (SAP) is a pathological entity that may have a fulminant evolution. SAP incidence is continuously increasing in recent years, and it is estimated to be 20-100 per 100,000, due to multiple factors (like daily stress, unhealthy eating, obesity that have also a continuously increasing incidence, etc.) [
1]. The frequency of SAP is 15-20% and is associated with high mortality rate and long ICU stay [
2,
3]. Despite the efforts of intensive care team and early treatment, the mortality rate remains around 30-40% [
4]. Several theories have been postulated regarding the increase in PAS cases: better diagnostics and management, lifestyle factors, host factors (obesity, comorbidities, age) increasing the life expectancy of the population. In commonly used severity scores, older age correlates more with disease severity or mortality rate [
5]. In Ranson’s criteria age is summed only if the patient has over 55 years old [
6], in Apache II only if it is over >44 [
7] and in clinical score BISAP age only if it exceeds 60 years old [
8].
The predictive role of comorbidities is poorly debated regarding AP severity also the development of cardiac complications such as myocardial infarction, acute heart failure and acute arrhythmias, as well as respiratory complications can prolong the length of hospitalization in ICU and days of mechanical ventilation [
9].
The length of hospitalization in ICU is depending on intubation days, represented by mechanical ventilation and cardiac complication. If patient develops, myocardial infarction, acute cardiac failure or acute arrhythmia such as acute fibrillation, flutter, the weaning is most likely unsuccessful [
10].
The paper aims to establish which patients with SAP are prone to develop cardiac complications and those who will have a difficult weaning from the ventilator.
Results
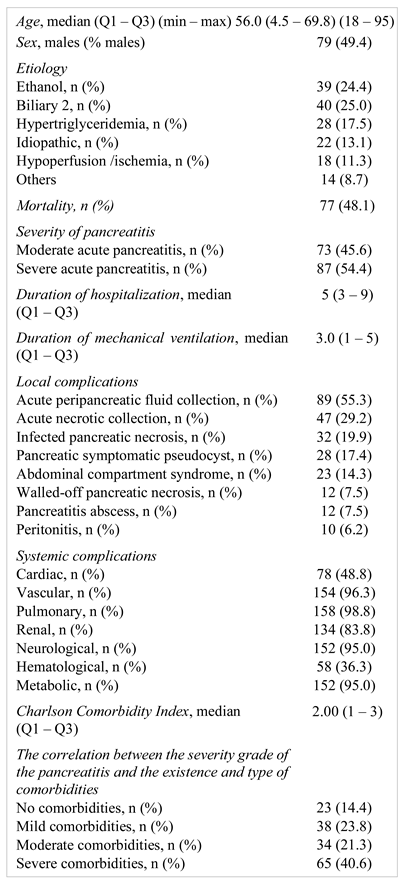
The studied group includes 161 patients with acute pancreatitis hospitalized in the intensive care unit of the emergency university hospital in Bucharest. They all met the criteria for admission in ICU and for the diagnosis of acute pancreatitis, also for the severity criteria. Most were mechanically intubated and some developed cardiac complications and some had difficult weaning.
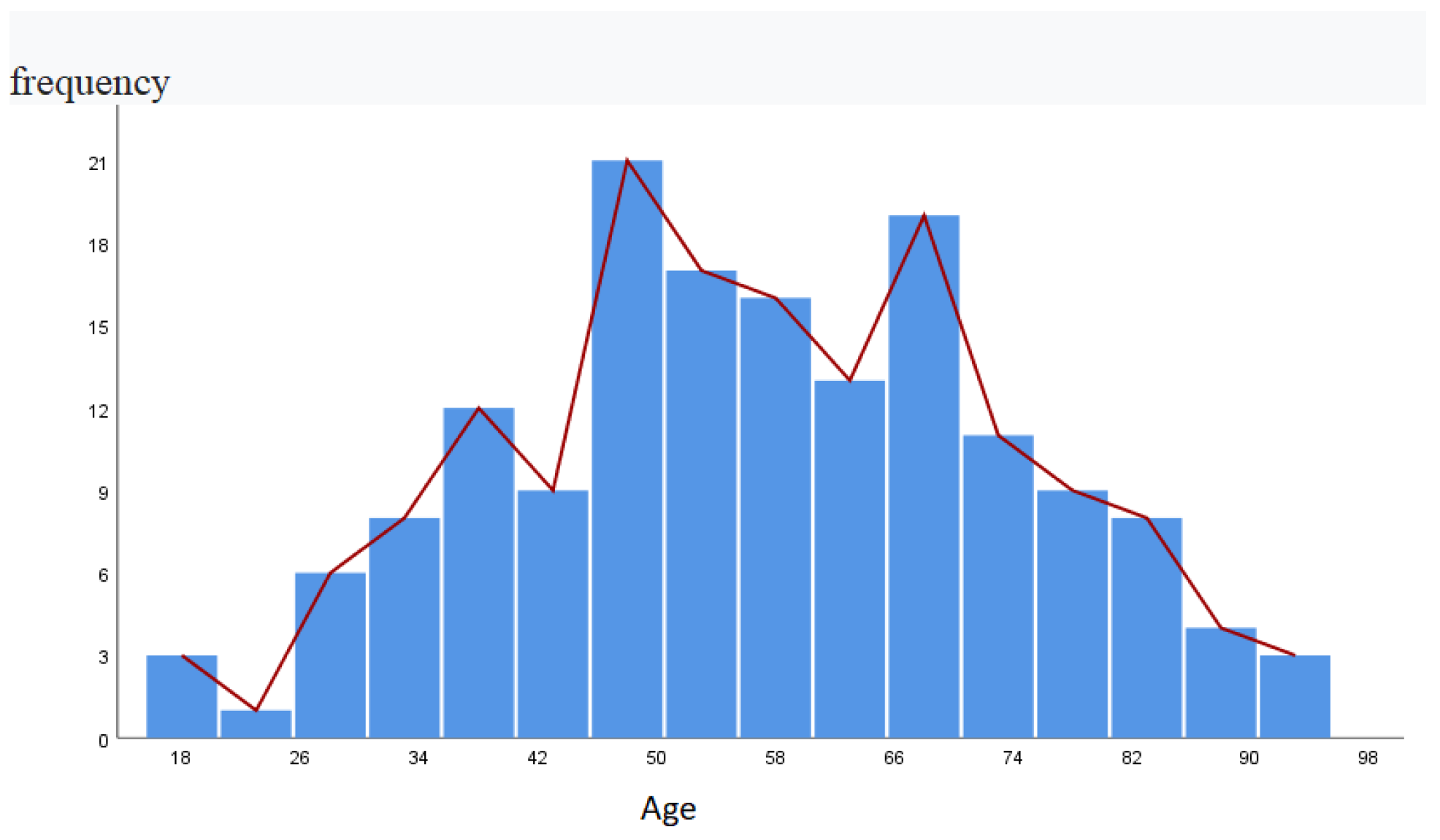
There were 81 women and 80 men, of which only 52% survived. In the table below we describe main characteristics of the studied group like age, sex, etiology for the pancreatitis, severity, complication type, CCI and mortality mentioning that three cases were due to medicinal SAP. Median age obtained from the group was 56 years. The most numerous patients were those in the 61-70 age group, 32 in number, followed by the 51-60 age group, 31 in number (
Table 1).
We further investigated the distribution of cases resulting in fatal outcome along with the age in the study group (
Figure 1).
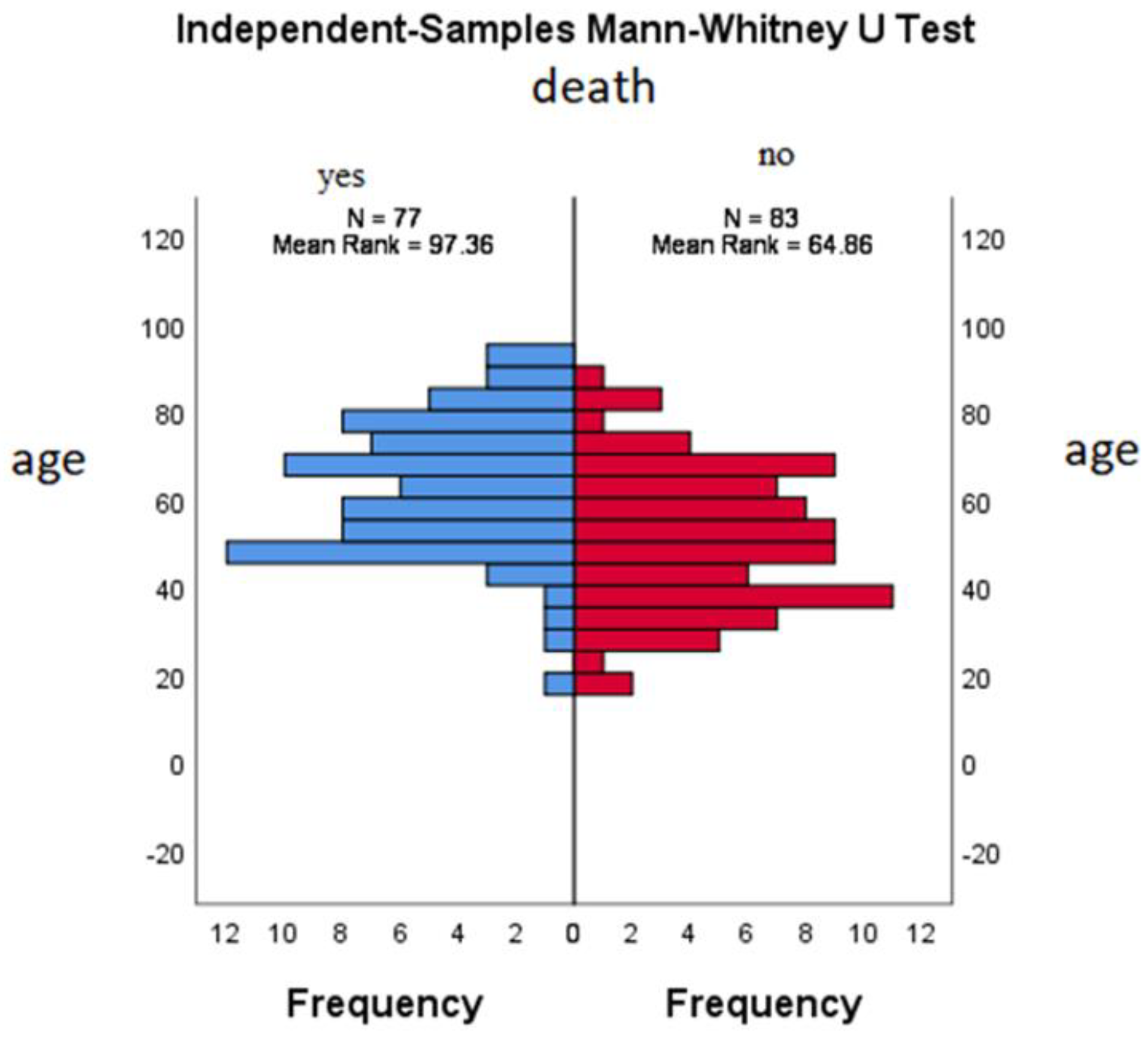
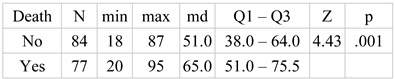
Following the non-parametric comparative analysis Mann-Whitney there was a significant difference between the median age at survival (md=51.0) Q1 – Q3 (38.0 – 64.0) and the median age of death (md=65.0) Q1 – Q3 (51.0 – 75.5), for a standard test value of Z=4.43 and p<.001 (
Table 2,
Figure 2).
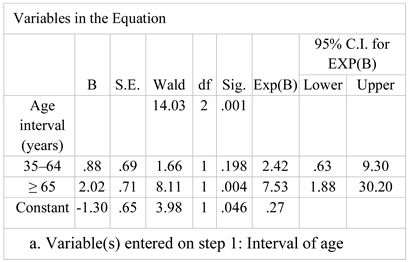
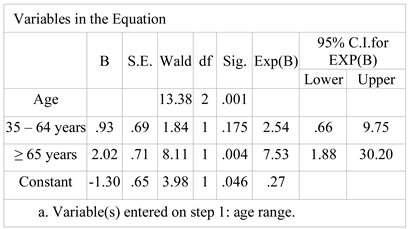
Applying a binary logistic regression analysis for age, a reduced predictive capacity was identified (Nagelkerke R-square=.122) and a percentage of correct prediction of 64.4%, with a higher ability to correctly predict survival of 77.1% and very low for death (50.6%) (
Table 3).
Considering the young age range (18 – 34 years) as a comparison criterion, a 2.42 (95% CI: .63 – 9.30) times higher chance of death was identified for the middle age range (35 – 64 years), but lacking statistical significance (Wald=1.66 and p=.198), and a 7.53 (95% CI: 1.88 – 30.20) times higher chance for the high age range (≥65 years) that is statistically significant for Wald=8.11 and p<.01. (
Figure 3).
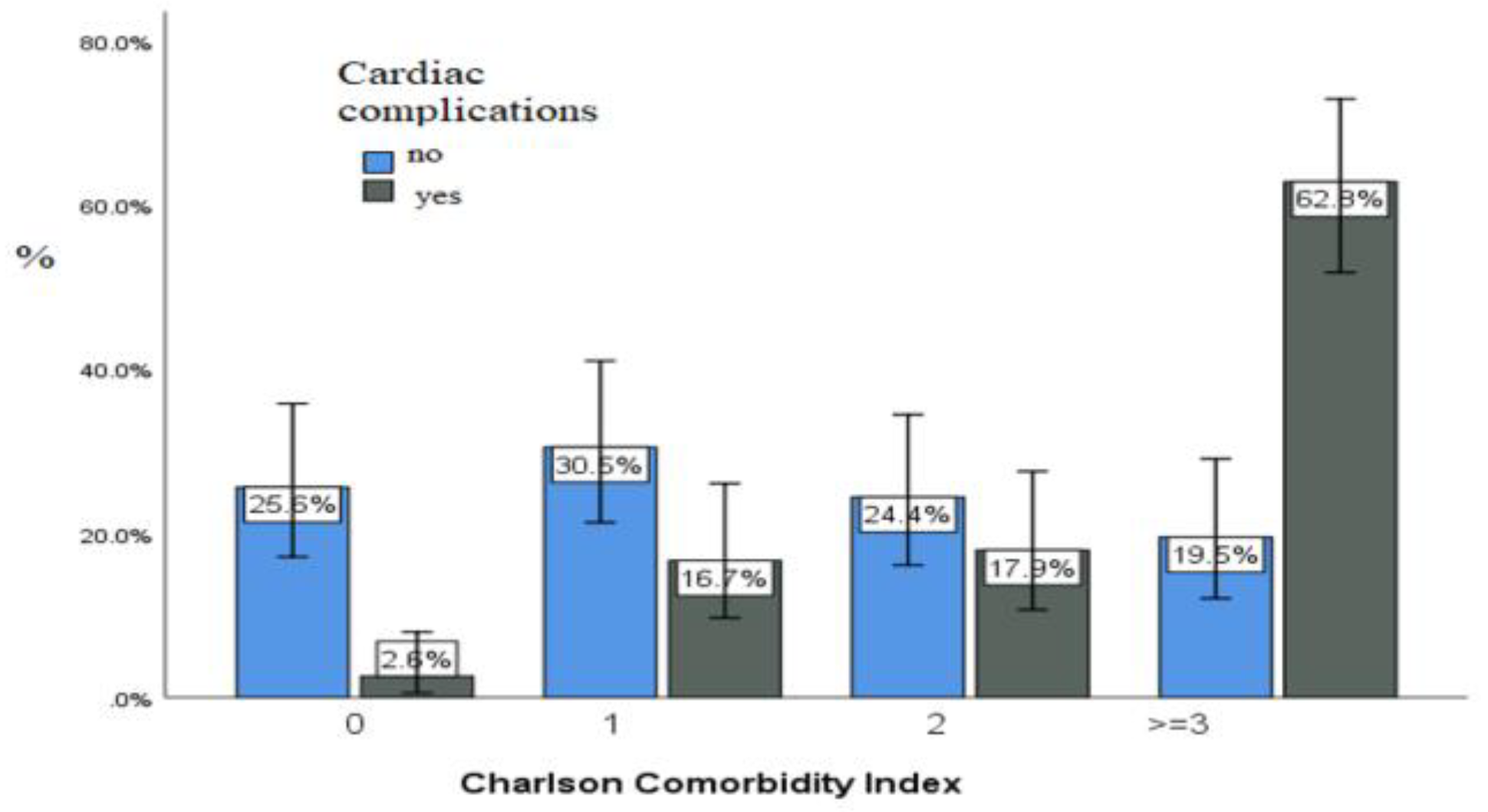
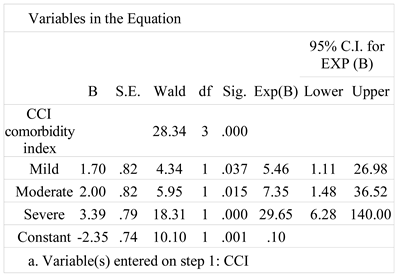
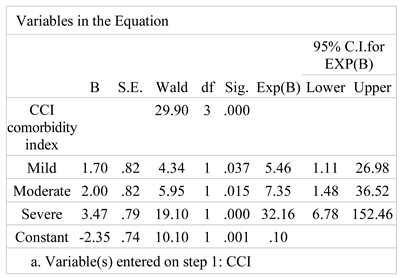
Applying a binary logistic regression analysis, a good predictive ability (Nagelkerke R-square=.285) and a correct prediction percentage of 71.3% were identified, with a higher correct survival predictive ability of 79.5% and lower for death (62.3%) (
Table 4).
Considering the lack of comorbidities as a comparison criterion, a 5.46 (CI 95%: 1.11 – 26.98) times higher chance of death due to mild comorbidity (1 serious illness) was identified, statistically significant (Wald=4.346 and p=. 037), and a 29.65 (95% CI: 6.28 – 140.00) times higher odds for severe comorbidity (≥ 3 serious chronic diseases) which is statistically significant for Wald=18.31 and p<.001.
Using a multivariate binary logistic regression model using CCI level and age did not improve prediction over CCI-based prediction.
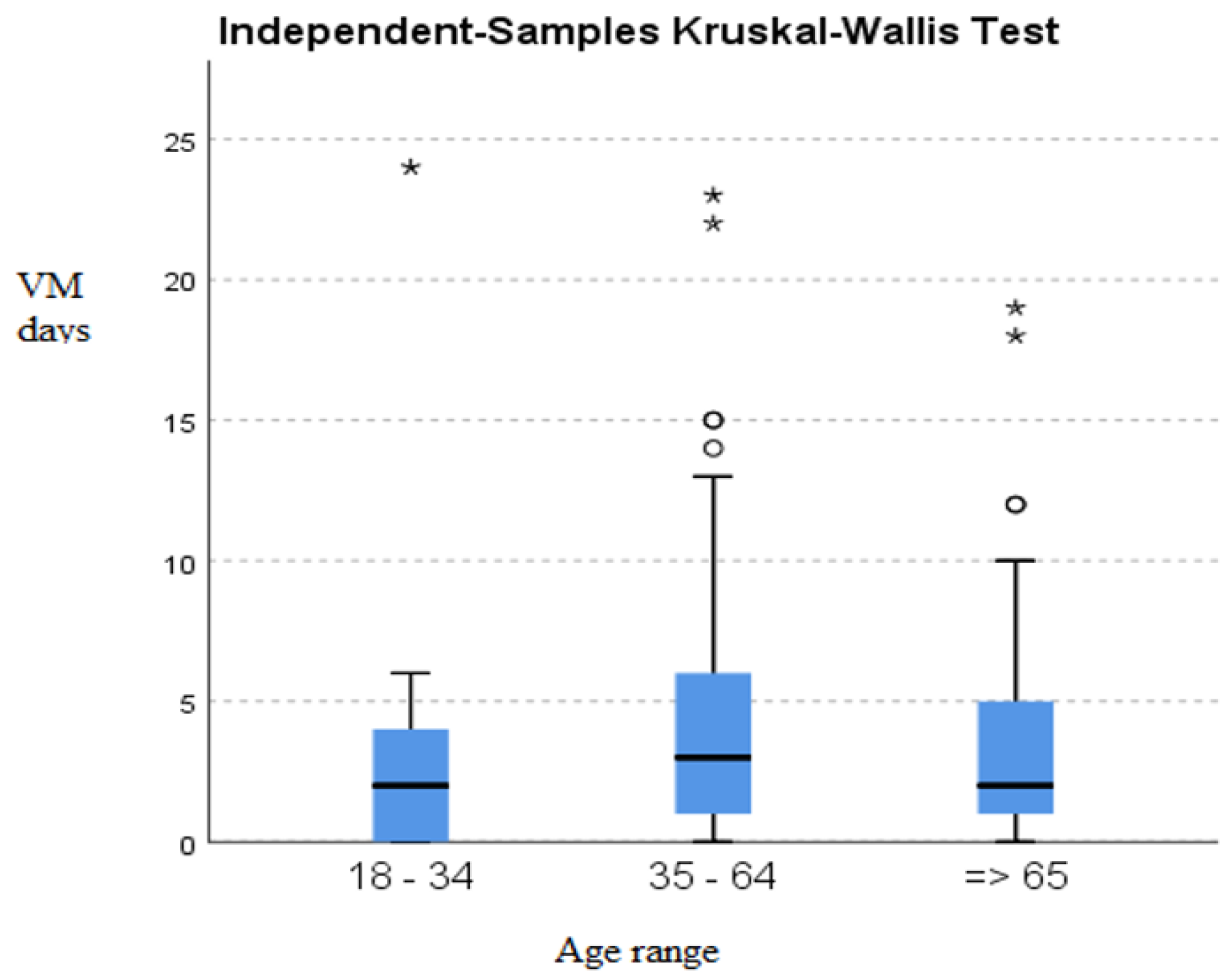
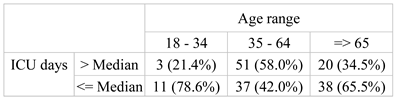
The non-parametric comparative analysis (test of the median) of the length of hospitalization in intensive care unit according to the age range indicated a statistically significant difference for a value of the Chi-square [
2] test=11.55 and p=.003<.01. High proportions of durations of less than 5 days were observed for the 18-34 years (78.6%) and ≥ 65 years (65.5%), and a high proportion of ICU hospitalizations of more than 5 days for those aged between 35 and 64 years old (
Table 5,
Figure 4).
Applying a binary logistic regression analysis identified a reduced predictive ability (Nagelkerke R-square=.117) and a percentage of correct prediction of 63.7%, with a higher correct predictive ability of survival of 76.8% and reduced for death (50.0%) (
Table 7).
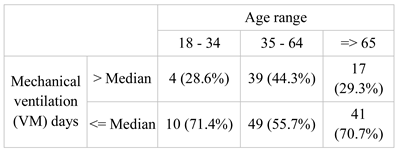
The non-parametric comparative analysis (median test) of the duration of intubation according to the age range indicated a statistically insignificant difference for a value of the Chi-square [
2] test=3.88 and p=0.144<0.05. High shares of durations of less than three days were observed for the 18-34 years (71.4%) and ≥ 65 years (70.7%), and a lower share for those aged between 35 and 64 (55.7%) (
Figure 5).
Applying a binary logistic regression analysis identified a reduced predictive ability (Nagelkerke R-square=.117) and a percentage of correct prediction of 63.7%, with a higher correct predictive ability of survival of 76.8% and reduced for death (50.0%) (
Table 7).
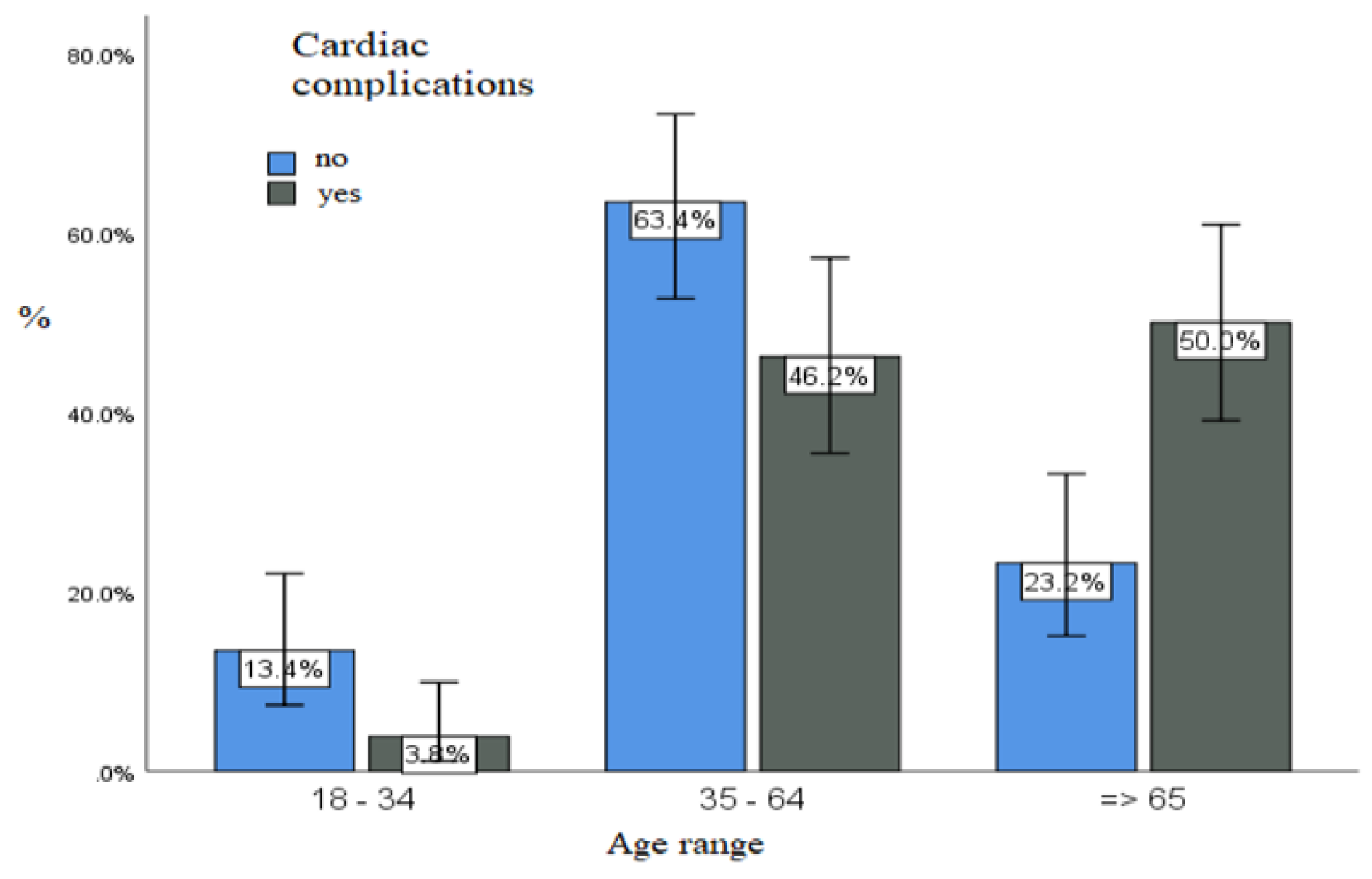
Considering the young age range (18 – 34 years) as a comparison criterion, a 2.54 (95% CI: .66 – 9.75) times higher chance of cardiac complications was identified for the middle age range (35 – 64 years), but lacking statistical significance (Wald=1.84 and p=.175). A 7.53 (95% CI: 1.88 – 30.20) times higher odds for the high age range (≥65 years) which is statistically significant for Wald=8.11 and p=.004<.01 (
Figure 7).
Applying a binary logistic regression analysis, a good predictive ability (Nagelkerke R-square=.299) and a percentage of correct prediction of 71.9% were identified, with a higher correct predictive ability of survival of 80.5% and lower for cardiac complications (62.8%) (
Table 8).
Considering the lack of comorbidities as a comparison criterion, we find a 5.46 (95% CI: 1.11 – 26.98) times higher chance of cardiac complication was identified for mild comorbidity (1 serious disease), statistically significant (Wald=4.34 and p= .037), and a 32.16 (95% CI: 6.78 – 152.46) times higher odds for severe comorbidity (≥ 3 serious chronic diseases) which is statistically significant for Wald=19.10 and p<.001.
Discussions
Acute pancreatitis is a common cause for presentation in emergency. In most cases, the etiology involves a coexisting biliary pathology. Other factors may be chronic ethanol consumption, hypertriglyceridemia and ischemic factors [
13]. A rare cause of acute pancreatitis was reported by Nasri et al. [
14]. He reported a patient with neglected traumatic diaphragmatic hernia, who developed acute pancreatitis by stretching of the transverse mesocolon, resulting in pancreatic mobility, and herniation [
14]. In these complicated cases, preoperative CT exam is extremely valuable for diagnosis and management [
15].
In acute pancreatitis, the inflammatory changes may be limited to the pancreas, or more life-threatening, affecting all organs and systems. Predicting the severity and outcome of the patients admitted for acute pancreatitis is still a subject of research. Moreover, recent studies found a bidimensional correlation between inflammation and coagulation, with the endothelial cells playing at interface role [
16,
17,
18]. Microvascular changes in severe acute pancreatitis were documented not only at the pancreas level, but also in other organs, like colon and ileum, liver, lungs, kidneys, heart and brain, and play a major role in the organ failure from early stages [
17]. Multiple cytokines and biomarkers of inflammation were investigated in clinical studies [
19]. T lymphocytes play a vital role in the immune responses at multiple levels [
20,
21]. While neutrophils and monocytes/macrophages have been hypothesized to be the major leukocyte populations infiltrating the inflamed pancreas, local imbalances in T cells in the inflammatory sites and in circulation have been observed in pancreatitis [
20], suggesting a potential future therapeutic target.
Multiple researchers found NLR to be and encouraging tool to estimate the severity of systemic involvement [
22,
23,
24]. In a recent study of Halaseh et al. [
24], increased NLR was found to be a predictor for early mortality.
In our study, those who died were older than survivors. For the young age interval, as well as for the middle age we obtained a similar mortality a 2.42 (95% CI: .63 – 9.30). On the other hand, for elderly patients, age correlated with high mortality, statistically significant, a 7.53 (95% CI: 1.88 – 30.20) times higher chance for the high age range (≥65 years) that is statistically significant for Wald=8.11 and p<.01.
Zsolt Szakács [
5] published in 2019 a multicentric study on 1203 patients hospitalized with acute pancreatitis in 18 centers from Hungary. Among the main findings of the research, age over 65 was a strong predictor with borderline significance, both for acute pancreatitis severity and length of stay over 9 days, concluding that older patients must be admitted promptly to ICU due to their high risk of death.
In the study of Frey et al named “Co-morbidity is a Strong Predictor of Early Death and Multi-organ System Failure among Patients with Acute Pancreatitis”, patients with no CCI died in 1,1% cases, while the percentage reached 3.8% in patients with 3 or more comorbidities, due to organ failure in 2 or more organs. Specific comorbid conditions associated with the highest incidence of death within 91 days were recent cancer, chronic heart failure, chronic renal failure, and malnutrition [
25]. Advancing age was also a very strong independent predictor of early death, especially in patients who had one or more comorbidities. In the study of Frey et al. [
25], early death was encountered in 0.1% of patients aged 54 or younger, while the percentage increased up to 7.1% in cases aged 75 or older, associating 3 or more comorbidities. Thus, the authors support the idea that age and comorbidities should be carefully evaluated in the risk management plan of the patients admitted with acute pancreatitis.
In our study we observed that patients without comorbidities have a low-rate mortality. For those with CCI score=1 there is a slightly higher risk, and for those with 2 comorbidities, CCI=2 it is a higher risk. On the other hand, if the patient presents a CCI score >=3, meaning three or more serious chronic diseases, the risk of death is very high-29.65 (95% CI: 6.28 – 140.00) times higher odds for severe comorbidity which is statistically significant for Wald=18.31 and p<.001. Cardiovascular disease (CVD) represents a group of disorders of the heart and/or blood vessels that includes peripheral arterial disease, stroke, coronary heart failure, high blood pressure, and other vascular and/or cardiac conditions, which are the leading cause of morbidity and mortality worldwide [
26]. In our study, the presence of cardiovascular comorbidities was associated with higher mortality, in older age group.
Our study demonstrated that age does not bring any improvement over the prediction of CCI. Zsolt Szakács’s study concluded that “age strongly influences the outcome of acute pancreatitis. They found also that age correlates with CCI and observed a moderate, positive correlation between age and CCI (r = 0.334, p < 0.001)” [
5]. Unlike them, we observed a weaker positive correlation between age and CCI. In old patients we have greater CCI so the results are similar, but in young patient with CCI >3, age is not a reliable predictor of rate mortality.
Atsuhiko Murata et al. [
27] demonstrated that comorbidities substantially influenced the prognosis of older patients with acute pancreatitis and cardiovascular and renal comorbidities act like significant factors affecting the prognostic. Moreover, Murata found that cardiovascular, malignant and renal diseases were significantly associated with higher in-hospital mortality in older patients with acute pancreatitis [
27].
McNabb-Baltar et al. [
28] investigated the relationship between the incidence and severity of comorbidity using CCI, and found that patients with a CCI≥3 were more likely to be admitted to the ICU. In this study, use of the CCI score was advantageous in assessing the impact of comorbidity on outcomes of patients. In addition, they focused on elderly patients, whose comorbidities were a greater influence on outcomes compared with younger patients [
28].
Vasilopoulos and Kotwal [
29] investigated the role of modified CCI on the mortality. Therefore, we obtained a reliable parameter, directly proportional to the risk of death. Unlike the linear and directly proportional relation of death and CCI, they found that age correlated with death only for the elderly [
29].
In our study, the cardiac complications were more frequent in the 35-64 age range. In these patients, the cardiac events were also associated with a high survival rate of 78%. This results also meant the establishment of early optimal treatment, managing all the biological imbalances that led to cardiac complications improves survival [
30]. In the elderly, the presence of a new heart disease correlated with a high death rate of 50%.
If CCI score is greater than 2, the chances of developing a cardiac complication grow. The more advanced the age, the greater the risk of the impact of the new heart disease. The results of our study showed that length of hospitalization in therapy was short < 5 days for the young and the elderly. Mortality rate in the elderly was high, and survival low. For patients of 35-65 years, we correlated results with long ICU hospitalization and more local complications, p=.003<.01.
Difficult weaning was associated with death especially in elderly. The intubation period was short <3 days in young people and was successfully concluded, and short <3 days in the elderly but associated with risk of death.
In a metanalysis of Mikó et al. [
31], diabetes mellitus was found to be a risk factors for local and systemic complications in patients with acute pancreatitis and with a tendency to higher mortality. These findings may be explained by multiple mechanisms such as chronic low-grade inflammation, increased enteral permeability, impaired phagocytosis and altered immune defense [
31,
32]. However, Graham et al. [
33] found no differences in mortality in diabetic and non-diabetic patients hospitalized in ICU. These findings may be explained by the protective antioxidant and anti-inflammatory effects of exogenous insulin used for treating hyperglycemia in diabetic patients [
34,
35].
Li et al. [
36] found that the number of comorbidities correlated well with an increased rate of organ failure in patients PAS, influencing the final outcome. In addition, cardiovascular and renal diseases were significant factors affecting both in-hospital mortality and length of stay in older patients with acute pancreatitis.