Idiopathic Normal Pressure Hydrocephalus: The Real Social and Economic Burden of a Possibly Enormous Underdiagnosis Problem
Abstract
:1. Introduction
1.1. Background
1.2. Objective
2. Materials and Methods
2.1. Participants and Study Setting
2.2. Inclusion and Exclusion Criteria
- -
- over the age of 65;
- -
- who had access to the Emergency Departments of the province of Latina;
- -
- and whose personal data and medical history data can be found in our electronic medical records archive.
- -
- who had an obvious increase in the size of the ventricles;
- -
- and in whom other intracranial pathologies were excluded; in order to avoid interference on the CSF dynamics in particular, we excluded all patients who had a previous or concurrent history of intracranial bacterial, viral, or fungal infections—and of course, any intracranial hemorrhage.
2.3. Data Sources and Investigated Variables
- The callosal angle as measured at the coronal slice depicting the Monro foramina, suspicious if ≤80°. This was recorded both as a dichotomous variable (0/1->80°/<80°) and as a continuous variable, namely, the exact angle measured;
- The presence of a possible disproportion between the subarachnoid spaces of the basal cisterns and of the vertex sulci (DESH, Disproportionately Enlarged Subarachnoid Space Hydrocephalus). This was recorded as a dichotomous variable (0/1–absent/present);
- Evan’s index, measured as the maximal frontal horn ventricular width divided by the wider inner transverse intracranial diameter (ventriculomegaly if it was 0.3 or greater). This was recorded both as a dichotomous variable (0/1-<0.3/>0.3) and as a continuous variable, namely, the exact Evan’s Index measured;
- Enlarged intracranial ventricles. This was recorded as a dichotomous variable (0/1–absent/present).
2.4. Outcome Measures
2.5. Statistical Methods and Potential Sources of Bias
3. Results
Main Results
4. Discussion
4.1. Main Results and Interpretation
4.2. Limitations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hakim, S.; Adams, R.D. The special clinical problem of symptomatic hydrocephalus with normal cerebrospinal fluid pressure. Observations on cerebrospinal fluid hydrodynamics. J. Neurol. Sci. 1965, 2, 307–327. [Google Scholar] [CrossRef]
- Skalický, P.; Mládek, A.; Vlasák, A.; De Lacy, P.; Beneš, V.; Bradáč, O. Normal pressure hydrocephalus-an overview of pathophysiological mechanisms and diagnostic procedures. Neurosurg. Rev. 2020, 43, 1451–1464. [Google Scholar] [CrossRef]
- Martín-Láez, R.; Caballero-Arzapalo, H.; López-Menéndez, L.Á.; Arango-Lasprilla, J.C.; Vázquez-Barquero, A. Epidemiology of Idiopathic Normal Pressure Hydrocephalus: A Systematic Review of the Literature. World Neurosurg. 2015, 84, 2002–2009. [Google Scholar] [CrossRef] [PubMed]
- Kiefer, M.; Unterberg, A. The differential diagnosis and treatment of normal-pressure hydrocephalus. Dtsch. Arztebl. Int. 2012, 109, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Kockum, K.; Lilja-Lund, O.; Larsson, E.M.; Rosell, M.; Söderström, L.; Virhammar, J.; Laurell, K. The idiopathic normal-pressure hydrocephalus Radscale: A radiological scale for structured evaluation. Eur. J. Neurol. 2018, 25, 569–576. [Google Scholar] [CrossRef]
- Park, H.Y.; Kim, M.; Suh, C.H.; Lee, D.H.; Shim, W.H.; Kim, S.J. Diagnostic performance and interobserver agreement of the callosal angle and Evans’ index in idiopathic normal pressure hydrocephalus: A systematic review and meta-analysis. Eur. Radiol. 2021, 31, 5300–5311. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, P.; Albini-Riccioli, L.; Giannini, G.; Milletti, D.; Sorenson, T.J.; Stanzani-Maserati, M.; Oppi, F.; Elder, B.D.; Cevoli, S.; Cortelli, P.; et al. Anterior Callosal Angle: A New Marker of Idiopathic Normal Pressure Hydrocephalus? World Neurosurg. 2020, 139, e548–e552. [Google Scholar] [CrossRef]
- Benedetto, N.; Gambacciani, C.; Aquila, F.; Di Carlo, D.T.; Morganti, R.; Perrini, P. A new quantitative method to assess disproportionately enlarged subarachnoid space (DESH) in patients with possible idiopathic normal pressure hydrocephalus: The SILVER index. Clin. Neurol. Neurosurg. 2017, 158, 27–32. [Google Scholar] [CrossRef]
- Ryska, P.; Slezak, O.; Eklund, A.; Malm, J.; Salzer, J.; Zizka, J. Radiological markers of idiopathic normal pressure hydrocephalus: Relative comparison of their diagnostic performance. J. Neurol. Sci. 2020, 408, 116581. [Google Scholar] [CrossRef] [PubMed]
- Reddy, G.K.; Bollam, P.; Caldito, G. Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg. 2014, 81, 404–410. [Google Scholar] [CrossRef]
- Kim, M.J.; Seo, S.W.; Lee, K.M.; Kim, S.T.; Lee, J.I.; Nam, D.H.; Na, D.L. Differential diagnosis of idiopathic normal pressure hydrocephalus from other dementias using diffusion tensor imaging. AJNR Am. J. Neuroradiol. 2011, 32, 1496–1503. [Google Scholar] [CrossRef]
- Krzastek, S.C.; Robinson, S.P.; Young, H.F.; Klausner, A.P. Improvement in lower urinary tract symptoms across multiple domains following ventriculoperitoneal shunting for idiopathic normal pressure hydrocephalus. Neurourol. Urodyn. 2017, 36, 2056–2063. [Google Scholar] [CrossRef]
- Anile, C.; De Bonis, P.; Albanese, A.; Di Chirico, A.; Mangiola, A.; Petrella, G.; Santini, P. Selection of patients with idiopathic normal-pressure hydrocephalus for shunt placement: A single-institution experience. J. Neurosurg. 2010, 113, 64–73. [Google Scholar] [CrossRef]
- Pesce, A.; Palmieri, M.; Scattolin, A.; Guerrini, F.; Czosnyka, M.; Czosnyka, Z.; Marano, M.; di Lazzaro, V.; Pompucci, A.; Iuliano, L.; et al. Global Neurocognitive and Frontal Functions Analysis and Precision Intrathecal Pressure Measurement to Settle the Diagnostic Dilemma of the Normal Pressure Hydrocephalus: A Preliminary Experience. World Neurosurg. 2022, 167, e1432–e1439. [Google Scholar] [CrossRef]
- Razay, G.; Wimmer, M.; Robertson, I. Incidence, diagnostic criteria and outcome following ventriculoperitoneal shunting of idiopathic normal pressure hydrocephalus in a memory clinic population: A prospective observational cross-sectional and cohort study. BMJ Open 2019, 9, e028103. [Google Scholar] [CrossRef] [PubMed]
- Tisell, M.; Höglund, M.; Wikkelsø, C. National and regional incidence of surgery for adult hydrocephalus in Sweden. Acta Neurol. Scand. 2005, 112, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Marmarou, A.; Young, H.F.; Aygok, G.A. Estimated incidence of normal pressure hydrocephalus and shunt outcome in patients residing in assisted-living and extended-care facilities. Neurosurg. Focus 2007, 22, E1. [Google Scholar] [CrossRef] [PubMed]
- Israelsson, H.; Larsson, J.; Eklund, A.; Malm, J. Risk factors, comorbidities, quality of life, and complications after surgery in idiopathic normal pressure hydrocephalus: Review of the INPH-CRasH study. Neurosurg. Focus 2020, 49, E8. [Google Scholar] [CrossRef]
- Casmiro, M.; D’Alessandro, R.; Cacciatore, F.M.; Daidone, R.; Calbucci, F.; Lugaresi, E. Risk factors for the syndrome of ventricular enlargement with gait apraxia (idiopathic normal pressure hydrocephalus): A casecontrol study. J. Neurol. Neurosurg. Psychiatry 1989, 52, 847–852. [Google Scholar] [CrossRef]
- Krauss, J.K.; Regel, J.P.; Vach, W.; Droste, D.W.; Borremans, J.J.; Mergner, T. Vascular risk factors and arteriosclerotic disease in idiopathic normal-pressure hydrocephalus of the elderly. Stroke 1996, 27, 24–29. [Google Scholar] [CrossRef]
- Ghaffari-Rafi, A.; Gorenflo, R.; Hu, H.; Viereck, J.; Liow, K. Role of psychiatric, cardiovascular, socioeconomic, and demographic risk factors on idiopathic normal pressure hydrocephalus: A retrospective case-control study. Clin. Neurol. Neurosurg. 2020, 193, 105836. [Google Scholar] [CrossRef] [PubMed]
- Lemcke, J.; Meier, U. Idiopathic normal pressure hydrocephalus (iNPH) and co-morbidity: An outcome analysis of 134 patients. Acta Neurochir. Suppl. 2012, 114, 255–259. [Google Scholar] [CrossRef]
- Wang, Z.; Zhang, Y.; Hu, F.; Ding, J.; Wang, X. Pathogenesis and pathophysiology of idiopathic normal pressure hydrocephalus. CNS Neurosci. Ther. 2020, 26, 1230–1240. [Google Scholar] [CrossRef]
- Capone, P.M.; Bertelson, J.A.; Ajtai, B. Neuroimaging of normal pressure hydrocephalus and hydrocephalus. Neurol. Clin. 2020, 38, 171–183. [Google Scholar] [CrossRef]
- del Mar Matarín, M.; Pueyo, R.; Poca, M.A.; Falcón, C.; Mataró, M.; Bargalló, N.; Sahuquillo, J.; Junqué, C. Post-surgical changes in brain metabolism detected by magnetic resonance spectroscopy in normal pressure hydrocephalus: Results of a pilot study. J. Neurol. Neurosurg. Psychiatry 2007, 78, 760–763. [Google Scholar] [CrossRef]
- Miskin, N.; Serulle, Y.; Wu, W.; Bruno, M.; Damadian, B.; Davis, A.; Golomb, J.; George, A. Post-shunt gait improvement correlates with increased cerebrospinal fluid peak velocity in normal pressure hydrocephalus: A retrospective observational phase contrast magnetic resonance imaging study. Int. J. Sci. Study 2015, 3, 48–54. [Google Scholar]
- Toma, A.K.; Papadopoulos, M.C.; Stapleton, S.; Kitchen, N.D.; Watkins, L.D. Systematic review of the outcome of shunt surgery in idiopathic normal-pressure hydrocephalus. Acta Neurochir. 2013, 155, 1977–1980. [Google Scholar] [CrossRef] [PubMed]
- Mori, E.; Ishikawa, M.; Kato, T.; Kazui, H.; Miyake, H.; Miyajima, M.; Nakajima, M.; Hashimoto, M.; Kuriyama, N.; Tokuda, T.; et al. Japanese Society of Normal Pressure Hydrocephalus. Guidelines for management of idiopathic normal pressure hydrocephalus: Second edition. Neurol. Med. Chir. 2012, 52, 775–809. [Google Scholar] [CrossRef] [PubMed]
- Andersson, J.; Rosell, M.; Kockum, K.; Lilja-Lund, O.; Söderström, L.; Laurell, K. Prevalence of idiopathic normal pressure hydrocephalus: A prospective, population-based study. PLoS ONE 2019, 14, e0217705. [Google Scholar] [CrossRef]
- Conn, H.O.; Lobo, F.M. What do physicians know about normal pressure hydrocephalus and when did they know it? A survey of 284 physicians. Yale J. Biol. Med. 2008, 81, 19. [Google Scholar]
- Available online: https://www.ordinemedicilatina.it/wp-content/uploads/2022/04/Programma-30-Aprile-2022.pdf (accessed on 15 October 2023).
- Available online: https://www.quotidianosanita.it/allegati/allegato1086448.pdf (accessed on 15 October 2023).
- Available online: https://www.asl.vt.it/Staff/SistemiInformativi/Documentazione/sio/pdf/Decr_U00310_04_07_2013.pdf (accessed on 15 October 2023).
- Tullberg, M.; Persson, J.; Petersen, J.; Hellström, P.; Wikkelsø, C.; Lundgren-Nilsson, Å. Shunt surgery in idiopathic normal pressure hydrocephalus is cost-effective—A cost utility analysis. Acta Neurochir. 2018, 160, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Alvi, M.A.; Brown, D.; Yolcu, Y.U.; Zreik, J.; Bydon, M.; Cutsforth-Gregory, J.K.; Graff-Radford, J.; Jones, D.T.; Graff-Radford, N.R.; Elder, B.D. Predictors of adverse outcomes and cost after surgical management for idiopathic normal pressure hydrocephalus: Analyses from a national database. Clin. Neurol. Neurosurg. 2020, 197, 106178. [Google Scholar] [CrossRef] [PubMed]
| N = 192 Patients | |
|---|---|
| Sex | Male N = 106 − 55% |
| Female N = 86 − 45% | |
| Age | 82.1 years ± 10.9 |
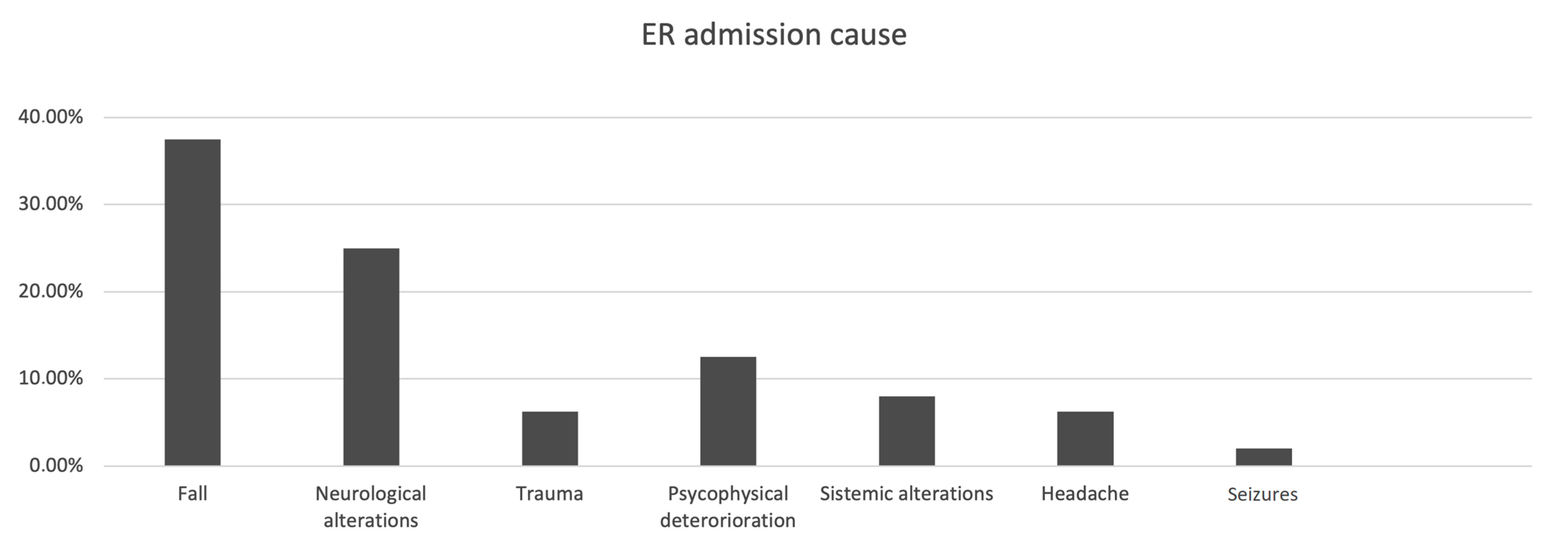
| Reason of Emergency Room admission | Fall 37.50% (72/192 patients) |
| Neurological deficit 25.00% (48/192 patients) | |
| Trauma 25.00% (48/192 patients) | |
| Cognitive impairment 12.50% (24/192 patients) | |
| Clinical manifestations | None 59.37% (114/192 patients) |
| Neurological deficit 15.7% (30/192 patients) | |
| Cognitive impairment 20.83% (40/192 patients) | |
| Seizure 1.57% (3/192 patients) | |
| Astenia 3.12% (6/192 patients) | |
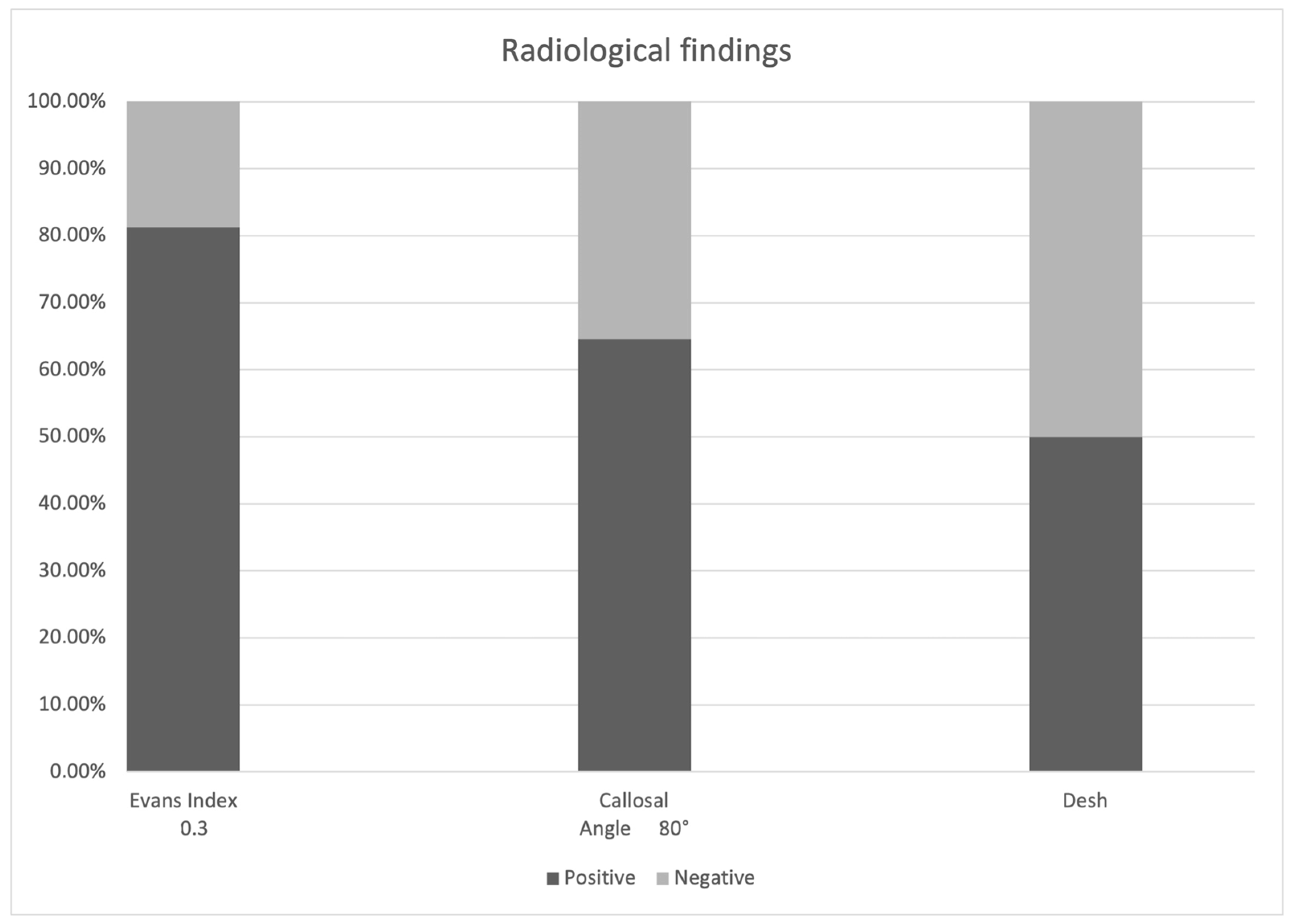
| Evans index ≥ 0.3 | 81.25% (156/192 patients) |
| Callosal angle ≤ 80° | 64.58% (124/192 patients) |
| DESH | 50.00% (96/192 patients) |
| Cortical atrophy | 32.81% (63/192 patients) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrella, G.; Ciarlo, S.; Elia, S.; Piaz, R.D.; Nucera, P.; Pompucci, A.; Palmieri, M.; Pesce, A. Idiopathic Normal Pressure Hydrocephalus: The Real Social and Economic Burden of a Possibly Enormous Underdiagnosis Problem. Tomography 2023, 9, 2006-2015. https://doi.org/10.3390/tomography9060157
Petrella G, Ciarlo S, Elia S, Piaz RD, Nucera P, Pompucci A, Palmieri M, Pesce A. Idiopathic Normal Pressure Hydrocephalus: The Real Social and Economic Burden of a Possibly Enormous Underdiagnosis Problem. Tomography. 2023; 9(6):2006-2015. https://doi.org/10.3390/tomography9060157
Chicago/Turabian StylePetrella, Gianpaolo, Silvia Ciarlo, Stefania Elia, Rita Dal Piaz, Paolo Nucera, Angelo Pompucci, Mauro Palmieri, and Alessandro Pesce. 2023. "Idiopathic Normal Pressure Hydrocephalus: The Real Social and Economic Burden of a Possibly Enormous Underdiagnosis Problem" Tomography 9, no. 6: 2006-2015. https://doi.org/10.3390/tomography9060157
APA StylePetrella, G., Ciarlo, S., Elia, S., Piaz, R. D., Nucera, P., Pompucci, A., Palmieri, M., & Pesce, A. (2023). Idiopathic Normal Pressure Hydrocephalus: The Real Social and Economic Burden of a Possibly Enormous Underdiagnosis Problem. Tomography, 9(6), 2006-2015. https://doi.org/10.3390/tomography9060157





