Long-Term Outcomes of Ultrasound-Guided Hydrodistension for Adhesive Capsulitis: A Prospective Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Measurements
- (1)
- They exhibited a blood glucose level that equaled or exceeded 126 mg/dL.
- (2)
- The HbA1c test, which provides a long-term view of average blood sugar levels, was another diagnostic tool. If a patient had a measurement of HbA1c that was equal to or surpassed 6.5%, and this reading was observed consistently in two distinct tests, they were diagnosed as diabetic.
- (3)
- An oral glucose tolerance test was also utilized as a diagnostic measure. In this test, patients are administered a glucose solution orally, and their blood glucose levels are subsequently measured. A diagnosis of diabetes was made if, 2 h after the glucose intake, and the patient’s blood glucose levels reached or exceeded 200 mg/dL.
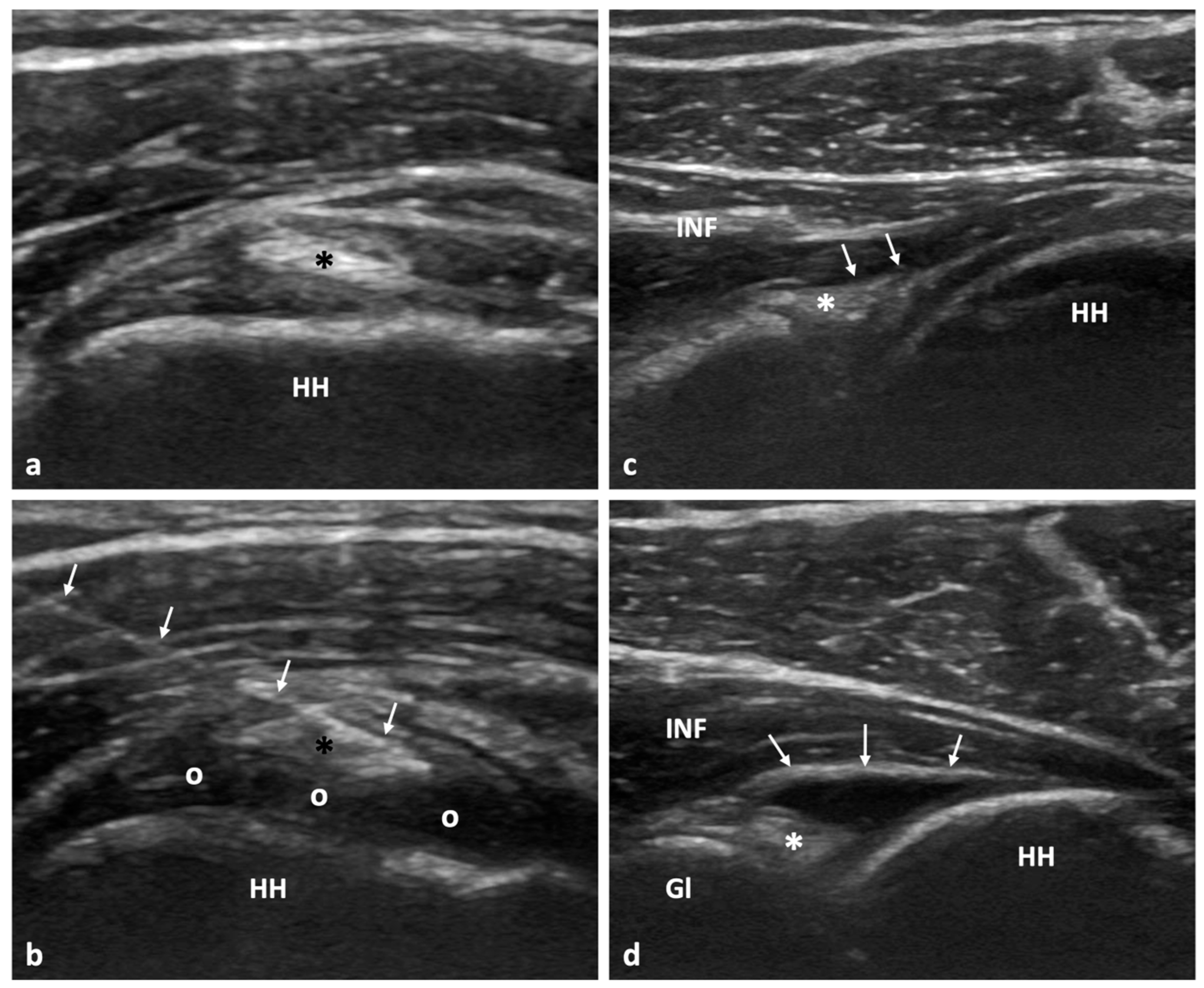
2.3. Diagnostic US Examination and US-Guided Hydrodistention
2.4. Statistical Analysis
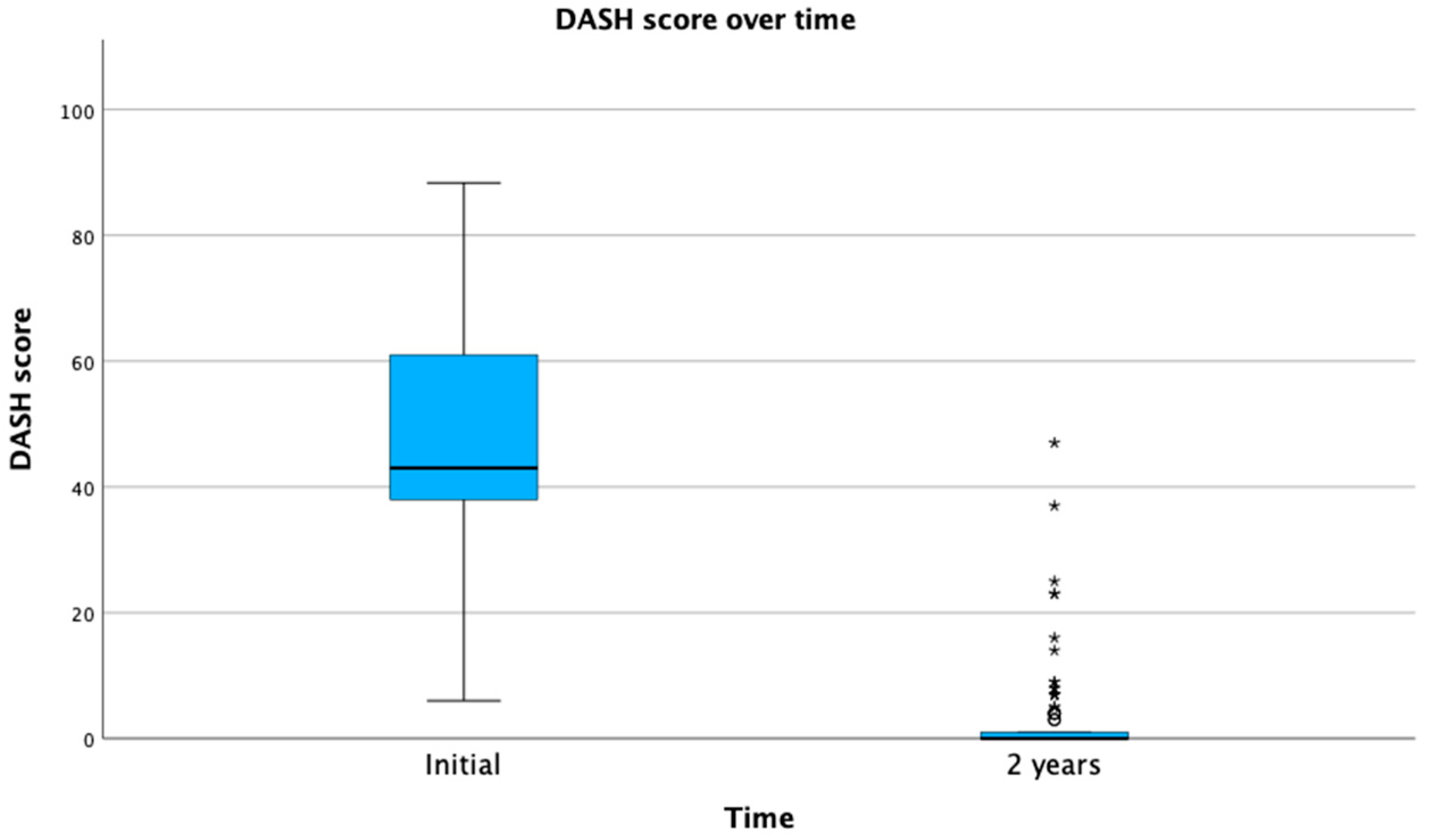
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nasri, H.Z.; Malik, R.A.; Charalambous, C.P. Adhesive capsulitis of the shoulder and diabetes: A meta-analysis of prevalence. Muscle Ligaments Tendons J. 2016, 6, 26–34. [Google Scholar] [CrossRef]
- Sharma, S.; Jacobs, L. The case for surgical treatment of the frozen shoulder. Ann. R. Coll. Surg. Engl. 2011, 93, 343. [Google Scholar] [CrossRef] [PubMed]
- Walker, D.J.; Hakim, A.J.; Cherkas, L.F.; Spector, T.D.; MacGregor, A.J. Genetic associations between frozen shoulder and tennis elbow: A female twin study. Rheumatology 2003, 42, 739–742. [Google Scholar] [CrossRef]
- Le, H.V.; Lee, S.J.; Nazarian, A.; Rodriguez, E.K. Adhesive capsulitis of the shoulder: Review of pathophysiology and current clinical treatments. Shoulder Elb. 2017, 9, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Kelley, M.J.; Mcclure, P.W.; Leggin, B.G. Frozen Shoulder: Evidence and a Proposed Model Guiding Rehabilitation. J. Orthop. Sports Phys. Ther. 2009, 39, 135–148. [Google Scholar] [CrossRef] [PubMed]
- Dimitri-Pinheiro, S.; Klontzas, M.E.; Pimenta, M.; Vassalou, E.E.; Soares, R.; Karantanas, A.H. Ultrasound-guided hydrodistension for adhesive capsulitis: A longitudinal study on the effect of diabetes on treatment outcomes. Skelet. Radiol. 2023, 52, 1005–1014. [Google Scholar] [CrossRef] [PubMed]
- Rymaruk, S.; Peach, C. Indications for hydrodilatation for frozen shoulder. EFORT Open Rev. 2017, 2, 462–468. [Google Scholar] [CrossRef]
- Dias, R.; Cutts, S.; Massoud, S. Clinical Review: Frozen Shoulder. BMJ 2005, 331, 1453–1456. [Google Scholar] [CrossRef]
- Al Khayyat, S.G.; Falsetti, P.; Conticini, E.; Frediani, B.; Galletti, S.; Stella, S.M. Adhesive capsulitis and ultrasound diagnosis, an inseparable pair: A novel review. J. Ultrasound 2023, 26, 369–384. [Google Scholar] [CrossRef]
- Fields, B.K.K.; Skalski, M.R.; Patel, D.B.; White, E.A.; Tomasian, A.; Gross, J.S.; Matcuk, G.R., Jr. Adhesive capsulitis: Review of imaging findings, pathophysiology, clinical presentation, and treatment options. Skelet. Radiol. 2019, 48, 1171–1184. [Google Scholar] [CrossRef] [PubMed]
- Zappia, M.; Di Pietto, F.; Aliprandi, A.; Pozza, S.; De Petro, P.; Muda, A.; Sconfienza, L.M. Multi-modal imaging of adhesive capsulitis of the shoulder. Insights Imaging 2016, 7, 365–371. [Google Scholar] [CrossRef]
- Sconfienza, L.M.; Chianca, V.; Messina, C.; Albano, D.; Pozzi, G.; Bazzocchi, A. Upper Limb Interventions. Radiol. Clin. N. Am. 2019, 57, 1073–1082. [Google Scholar] [CrossRef] [PubMed]
- Pimenta, M.; Vassalou, E.E.; Klontzas, M.E.; Dimitri-Pinheiro, S.; Ramos, I.; Karantanas, A.H. Ultrasound-guided hydrodilatation for adhesive capsulitis: Capsule-preserving versus capsule-rupturing technique. Skelet. Radiol. 2023. epub ahead of print. [Google Scholar] [CrossRef]
- Watson, L.; Bialocerkowski, A.; Dalziel, R.; Balster, S.; Burke, F.; Finch, C. Hydrodilatation (distension arthrography): A long-term clinical outcome series. Br. J. Sports Med. 2007, 41, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Pimenta, M.; Vassalou, E.E.; Dimitri-Pinheiro, S.; Klontzas, M.E.; Ramos, I.; Karantanas, A.H. Ultrasound-Guided Hydrodistension for Adhesive Capsulitis. J. Ultrasound Med. 2022, 42, 665–674. [Google Scholar] [CrossRef]
- Ricci, V.; Mezian, K.; Chang, K.-V.; Özçakar, L. Clinical/Sonographic Assessment and Management of Calcific Tendinopathy of the Shoulder: A Narrative Review. Diagnostics 2022, 12, 3097. [Google Scholar] [CrossRef]
- Sconfienza, L.M.; Adriaensen, M.; Albano, D.; Allen, G.; Gómez, M.P.A.; Bazzocchi, A.; Beggs, I.; Bignotti, B.; Chianca, V.; Corazza, A.; et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: A Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—Part I, shoulder. Eur. Radiol. 2019, 30, 903–913. [Google Scholar] [CrossRef] [PubMed]
- Buchbinder, R.; Green, S.; Youd, J.M.; Johnston, R.V.; Cumpston, M. Arthrographic distension for adhesive capsulitis (frozen shoulder). Cochrane Database Syst. Rev. 2008, 1, CD007005. [Google Scholar] [CrossRef]
- Brealey, S.; Armstrong, A.L.; Brooksbank, A.; Carr, A.J.; Charalambous, C.P.; Cooper, C.; Corbacho, B.; Dias, J.; Donnelly, I.; Goodchild, L.; et al. United Kingdom Frozen Shoulder Trial (UK FROST), multi-centre, randomised, 12 month, parallel group, superiority study to compare the clinical and cost-effectiveness of Early Structured Physiotherapy versus manipulation under anaesthesia versus arthroscopic capsular release for patients referred to secondary care with a primary frozen shoulder: Study protocol for a randomised controlled trial. Trials 2017, 18, 614. [Google Scholar] [CrossRef]
- Pimenta, M.; Vassalou, E.E.; Cardoso-Marinho, B.; Klontzas, M.E.; Dimitri-Pinheiro, S.; Karantanas, A.H. The role of MRI and Ultrasonography in Diagnosis and Treatment of Glenohumeral Joint Adhesive Capsulitis. Mediterr. J. Rheumatol. 2023, 34, 7–15. [Google Scholar] [CrossRef]
- Martinoli, C. Musculoskeletal ultrasound: Technical guidelines. Insights Imaging 2010, 1, 99–141. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.-T.; Chang, K.-V.; Han, D.-S.; Chang, C.-H.; Yang, F.-S.; Lin, C.-P. Effectiveness of Glenohumeral Joint Dilatation for Treatment of Frozen Shoulder: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Sci. Rep. 2017, 7, 10507. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.-T.; Hsiao, M.-Y.; Tu, Y.-K.; Wang, T.-G. Comparative Efficacy of Intra-Articular Steroid Injection and Distension in Patients With Frozen Shoulder: A Systematic Review and Network Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 1383–1394.e6. [Google Scholar] [CrossRef] [PubMed]
- Saltychev, M.; Laimi, K.; Virolainen, P.; Fredericson, M. Effectiveness of Hydrodilatation in Adhesive Capsulitis of Shoulder: A Systematic Review and Meta-Analysis. Scand. J. Surg. 2018, 107, 285–293. [Google Scholar] [CrossRef]
- Klauser, A.S.; Tagliafico, A.; Allen, G.M.; Boutry, N.; Campbell, R.; Court-Payen, M.; Grainger, A.; Guerini, H.; McNally, E.; O’connor, P.J.; et al. Clinical indications for musculoskeletal ultrasound: A Delphi-based consensus paper of the European society of musculoskeletal radiology. Eur. Radiol. 2012, 22, 1140–1148. [Google Scholar] [CrossRef]
- Silverstein, J.H.; Gordon, G.; Pollock, B.H.; Rosenbloom, A.L. Long-term glycemic control influences the onset of limited joint mobility in type 1 diabetes. J. Pediatr. 1998, 132, 944–947. [Google Scholar] [CrossRef]
- Rodeo, S.A.; Hannafin, J.A.; Tom, J.; Warren, R.F.; Wickiewicz, T.L. Immunolocalization of cytokines and their receptors in adhesive capsulitis of the shoulder. J. Orthop. Res. 1997, 15, 427–436. [Google Scholar] [CrossRef]
- Ryu, J.-D.; Kirpalani, P.A.; Kim, J.-M.; Nam, K.-H.; Han, C.-W.; Han, S.-H. Expression of vascular endothelial growth factor and angiogenesis in the diabetic frozen shoulder. J. Shoulder Elb. Surg. 2006, 15, 679–685. [Google Scholar] [CrossRef]
- Dworacka, M.; Winiarska, H.; Borowska, M.; Abramczyk, M.; Bobkiewicz-Kozlowska, T.; Dworacki, G. Pro-Atherogenic Alterations in T-Lymphocyte Subpopulations Related to Acute Hyperglycaemia in Type 2 Diabetic Patients. Circ. J. 2007, 71, 962–967. [Google Scholar] [CrossRef]
- Lee, J.C.; Sykes, C.; Saifuddin, A.; Connell, D. Adhesive capsulitis: Sonographic changes in the rotator cuff interval with arthroscopic correlation. Skelet. Radiol. 2005, 34, 522–527. [Google Scholar] [CrossRef]
- Walmsley, S.; Osmotherly, P.G.; Walker, C.J.; Rivett, D.A. Power Doppler Ultrasonography in the Early Diagnosis of Primary/Idiopathic Adhesive Capsulitis: An Exploratory Study. J. Manip. Physiol. Ther. 2013, 36, 428–435. [Google Scholar] [CrossRef]
- Tandon, A.; Dewan, S.; Bhatt, S.; Jain, A.K.; Kumari, R. Sonography in diagnosis of adhesive capsulitis of the shoulder: A case–control study. J. Ultrasound 2017, 20, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Elnady, B.; Rageh, E.M.; Hussein, M.S.; Abu-Zaid, M.H.; Desouky, D.E.-S.; Ekhouly, T.; Rasker, J.J. In shoulder adhesive capsulitis, ultrasound-guided anterior hydrodilatation in rotator interval is more effective than posterior approach: A randomized controlled study. Clin. Rheumatol. 2020, 39, 3805–3814. [Google Scholar] [CrossRef] [PubMed]
- Ricci, V.; Chang, K.; Özçakar, L. Ultrasound-Guided Hydrodilatation of the Shoulder Capsule at the Rotator Interval: Technical Tips and Tricks. Pain Pract. 2020, 20, 948–949. [Google Scholar] [CrossRef] [PubMed]
- Çınar, M.; Akpınar, S.; Derincek, A.; Circi, R.E.; Uysa, M. Comparison of arthroscopic capsular release in diabetic and idiopathic frozen shoulder patients. Arch. Orthop. Trauma Surg. 2009, 130, 401–406. [Google Scholar] [CrossRef] [PubMed]


| Diabetes | ||||
|---|---|---|---|---|
| No | Yes | Total | ||
| Recurrence | No | 152 | 22 | 174 |
| Yes | 11 | 17 | 28 | |
| Total | 163 | 39 | 202 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimitri-Pinheiro, S.; Klontzas, M.E.; Vassalou, E.E.; Pimenta, M.; Soares, R.; Karantanas, A.H. Long-Term Outcomes of Ultrasound-Guided Hydrodistension for Adhesive Capsulitis: A Prospective Observational Study. Tomography 2023, 9, 1857-1867. https://doi.org/10.3390/tomography9050147
Dimitri-Pinheiro S, Klontzas ME, Vassalou EE, Pimenta M, Soares R, Karantanas AH. Long-Term Outcomes of Ultrasound-Guided Hydrodistension for Adhesive Capsulitis: A Prospective Observational Study. Tomography. 2023; 9(5):1857-1867. https://doi.org/10.3390/tomography9050147
Chicago/Turabian StyleDimitri-Pinheiro, Sofia, Michail E. Klontzas, Evangelia E. Vassalou, Madalena Pimenta, Raquel Soares, and Apostolos H. Karantanas. 2023. "Long-Term Outcomes of Ultrasound-Guided Hydrodistension for Adhesive Capsulitis: A Prospective Observational Study" Tomography 9, no. 5: 1857-1867. https://doi.org/10.3390/tomography9050147
APA StyleDimitri-Pinheiro, S., Klontzas, M. E., Vassalou, E. E., Pimenta, M., Soares, R., & Karantanas, A. H. (2023). Long-Term Outcomes of Ultrasound-Guided Hydrodistension for Adhesive Capsulitis: A Prospective Observational Study. Tomography, 9(5), 1857-1867. https://doi.org/10.3390/tomography9050147









