Non-Calcified Coronary Artery Plaque on Coronary Computed Tomography Angiogram: Prevalence and Significance
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Non-Calcified Plaque (NCP) Detected by CCTA in Symptomatic Patients
3.2. Non-Calcified Plaque (NCP) Detected by CCTA in Asymptomatic Patients
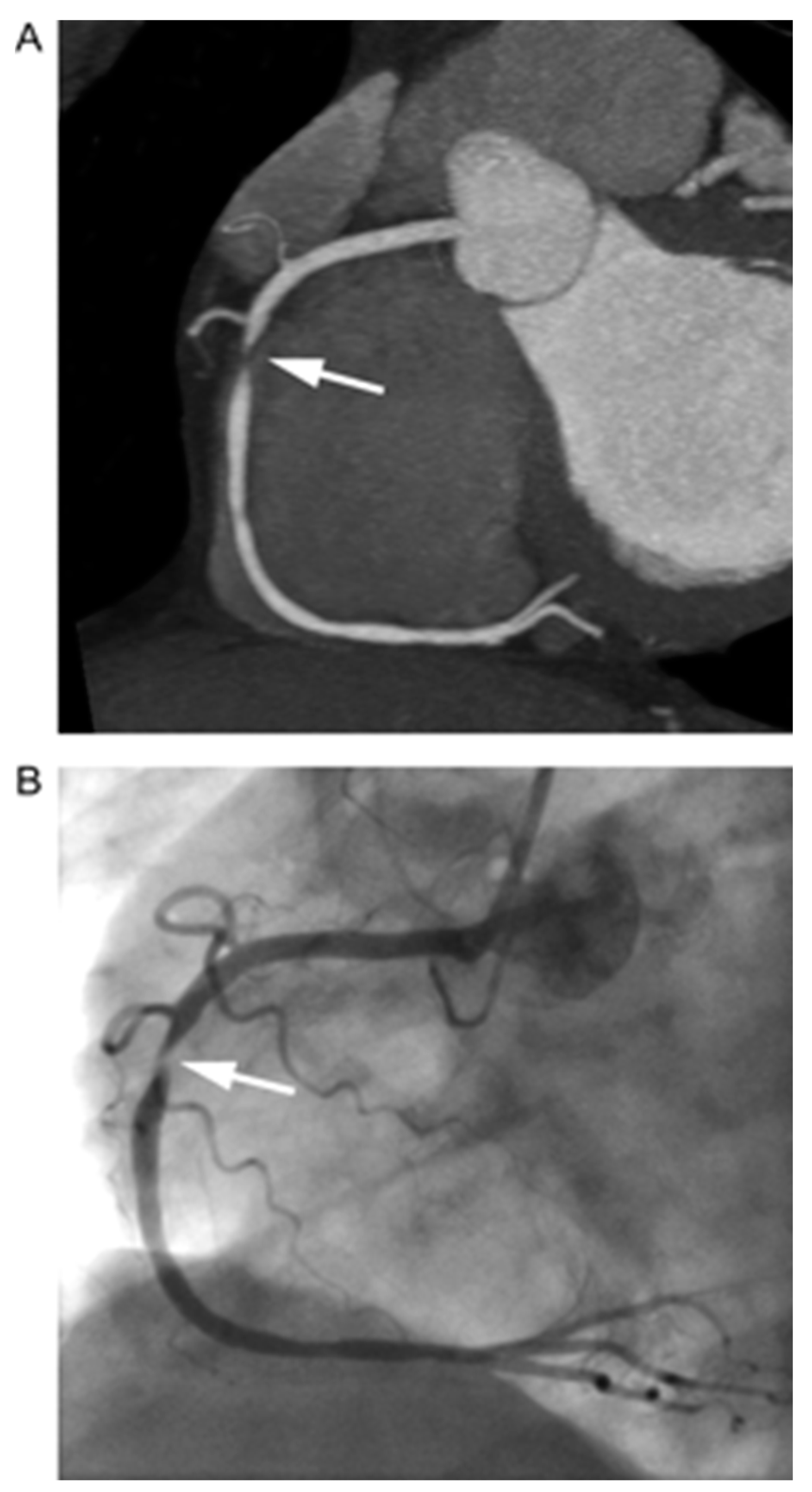
3.3. Comparison of CCTA Non-Calcified Plaque (NCP) with IVUS-VH
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NCP | Non-calcified plaque |
| CACS | Coronary artery calcium score |
| HRP | High-risk plaque |
| MACE | Major adverse cardiovascular events |
| RI | Remodeling index |
| MI | Myocardial infarction |
| HR | Hazard ratio |
| RF | Risk factors |
| CVD | Cardiovascular disease |
| IVUS | Intravascular ultrasound |
| VH | Virtual histology |
| DSCT | Dual-source CT scan |
| STEMI | ST-elevation myocardial infarction |
| NSTEMI | Non-ST elevation myocardial infarction |
| TCFA | Thin-cap fibro-atheroma |
| T2DM | Type II diabetes mellitus |
References
- Brown, J.C.; Gerhardt, T.E.; Kwon, E. Risk Factors for Coronary Artery Disease. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Hecht, H.S.; Cronin, P.; Blaha, M.J.; Budoff, M.J.; Kazerooni, E.A.; Narula, J.; Yankelevitz, D.; Abbara, S. 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: A report of the Society of Cardiovascular Computed Tomography and Society of Thoracic Radiology. J. Cardiovasc. Comput. Tomogr. 2017, 11, 74–84. [Google Scholar] [CrossRef]
- Anderson, H.; Masri, S.C.; Abdallah, M.S.; Chang, A.M.; Cohen, M.G.; Elgendy, I.Y.; Gulati, M.; LaPoint, K.; Madan, N.; Moussa, I.D.; et al. 2022 ACC/AHA Key Data Elements and Definitions for Chest Pain and Acute Myocardial Infarction: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Data Standards. Circ. Cardiovasc. Qual. Outcomes 2022, 15, e000112. [Google Scholar] [CrossRef]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef]
- Shaw, L.J.; Blankstein, R.; Bax, J.J.; Ferencik, M.; Bittencourt, M.S.; Min, J.K.; Berman, D.S.; Leipsic, J.; Villines, T.C.; Dey, D.; et al. Society of Cardiovascular Computed Tomog-raphy/North American Society of Cardiovascular Imaging—Expert Consensus Document on Coronary CT Imaging of Atherosclerotic Plaque. J. Cardiovasc. Comput. Tomogr. 2021, 15, 93–109. [Google Scholar] [CrossRef]
- Adamson, P.D.; Williams, M.C.; Dweck, M.R.; Mills, N.L.; Boon, N.A.; Daghem, M.; Bing, R.; Moss, A.J.; Mangion, K.; Flather, M.; et al. Guiding Therapy by Coronary CT Angiography Improves Outcomes in Patients with Stable Chest Pain. J. Am. Coll. Cardiol. 2019, 74, 2058–2070. [Google Scholar] [CrossRef]
- Williams, M.C.; Moss, A.J.; Dweck, M.; Adamson, P.D.; Alam, S.; Hunter, A.; Shah, A.S.V.; Pawade, T.; Weir-McCall, J.R.; Roditi, G.; et al. Coronary Artery Plaque Characteristics As-sociated With Adverse Outcomes in the SCOT-HEART Study. J. Am. Coll. Cardiol. 2019, 73, 291–301. [Google Scholar] [CrossRef]
- Mortensen, M.B.; Dzaye, O.; Steffensen, F.H.; Bøtker, H.E.; Jensen, J.M.; Sand, N.P.R.; Kragholm, K.H.; Sørensen, H.T.; Leipsic, J.; Mæng, M.; et al. Impact of Plaque Burden Versus Stenosis on Ischemic Events in Patients with Coronary Atherosclerosis. J. Am. Coll. Cardiol. 2020, 76, 2803–2813. [Google Scholar] [CrossRef]
- Cury, R.C.; Abbara, S.; Achenbach, S.; Agatston, A.; Berman, D.S.; Budoff, M.J.; Dill, K.E.; Jacobs, J.E.; Maroules, C.D.; Rubin, G.D.; et al. CAD-RADSTM Coronary Artery Disease—Reporting and Data System. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. J. Cardiovasc. Comput. Tomogr. 2016, 10, 269–281. [Google Scholar] [CrossRef]
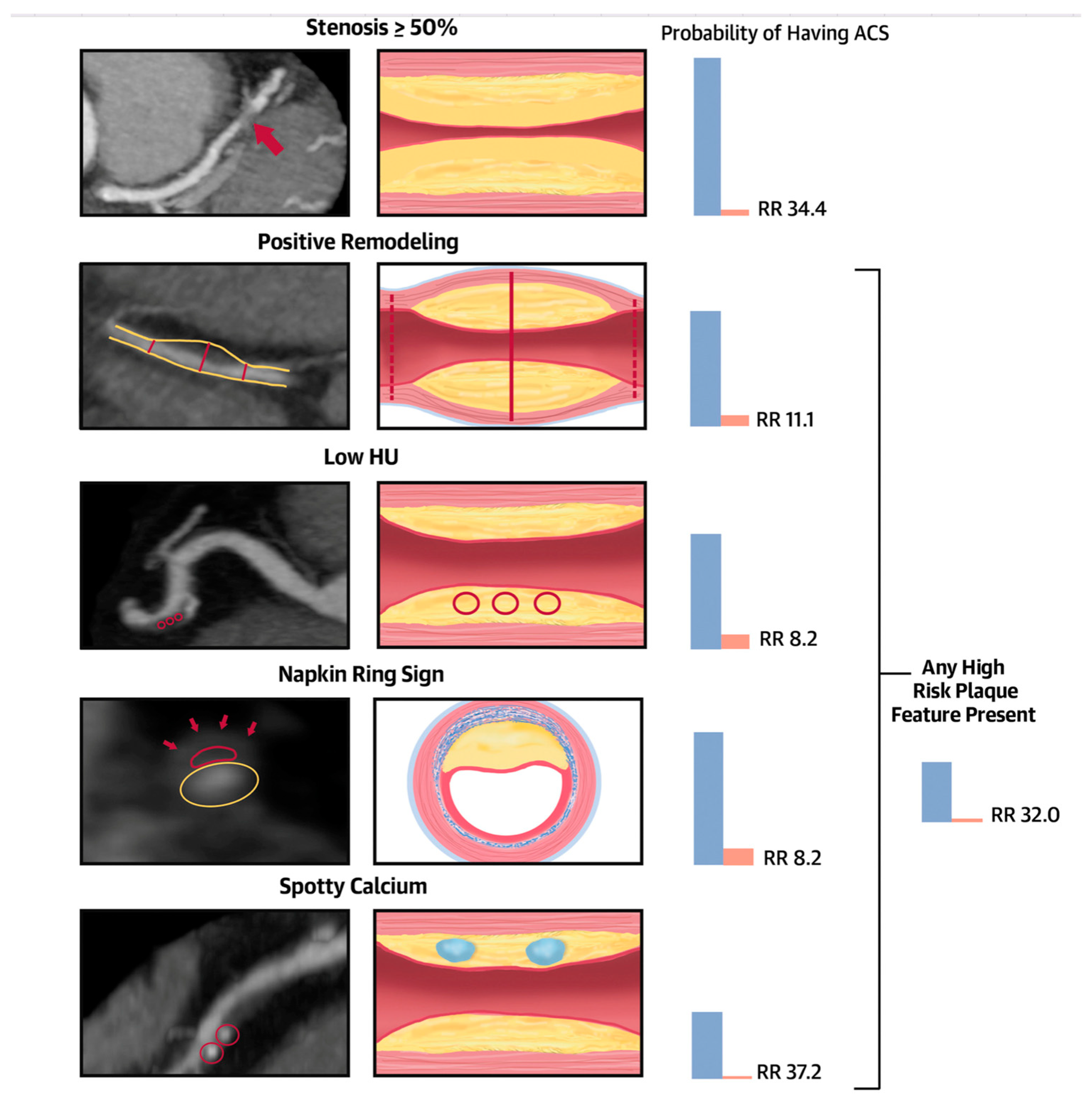
- Motoyama, S.; Ito, H.; Sarai, M.; Kondo, T.; Kawai, H.; Nagahara, Y.; Harigaya, H.; Kan, S.; Anno, H.; Takahashi, H.; et al. Plaque Characterization by Coronary Computed Tomography Angiography and the Likelihood of Acute Coronary Events in Mid-Term Follow-Up. J. Am. Coll. Cardiol. 2015, 66, 337–346. [Google Scholar] [CrossRef]
- Puchner, S.B.; Liu, T.; Mayrhofer, T.; Truong, Q.A.; Lee, H.; Fleg, J.L.; Nagurney, J.T.; Udelson, J.E.; Hoffmann, U.; Ferencik, M. High-risk plaque detected on coronary CT angiography predicts acute coronary syndromes independent of significant stenosis in acute chest pain: Results from the ROMICAT-II trial. J. Am. Coll. Cardiol. 2014, 64, 684–692. [Google Scholar] [CrossRef]
- Maurovich-Horvat, P.; Schlett, C.L.; Alkadhi, H.; Nakano, M.; Otsuka, F.; Stolzmann, P.; Scheffel, H.; Ferencik, M.; Kriegel, M.F.; Seifarth, H.; et al. The Napkin-Ring Sign Indicates Advanced Atherosclerotic Lesions in Coronary CT Angiography. JACC: Cardiovasc. Imaging 2012, 5, 1243–1252. [Google Scholar] [CrossRef]
- Achenbach, S.; Raggi, P. Imaging of coronary atherosclerosis by computed tomography. Eur. Heart J. 2010, 31, 1442–1448. [Google Scholar] [CrossRef]
- Hausleiter, J.; Meyer, T.; Hadamitzky, M.; Kastrati, A.; Martinoff, S.; Schömig, A. Prevalence of Noncalcified Coronary Plaques by 64-Slice Computed Tomography in Patients With an Intermediate Risk for Significant Coronary Artery Disease. J. Am. Coll. Cardiol. 2006, 48, 312–318. [Google Scholar] [CrossRef]
- Nance, J.W.; Schlett, C.L.; Schoepf, U.J.; Oberoi, S.; Leisy, H.B.; Barraza, J.M.; Headden, G.F.; Nikolaou, K.; Bamberg, F. Incremental Prognostic Value of Different Components of Coronary Atherosclerotic Plaque at Cardiac CT Angiography beyond Coronary Calcification in Patients with Acute Chest Pain. Radiology 2012, 264, 679–690. [Google Scholar] [CrossRef]
- Liu, T.; Maurovich-Horvat, P.; Mayrhofer, T.; Puchner, S.B.; Lu, M.T.; Ghemigian, K.; Kitslaar, P.H.; Broersen, A.; Pursnani, A.; Hoffmann, U.; et al. Quantitative coronary plaque analysis predicts high-risk plaque morphology on coronary computed tomography angiography: Results from the ROMICAT II trial. Int. J. Cardiovasc. Imaging 2018, 34, 311–319. [Google Scholar] [CrossRef]
- Al-Muhaidb, S.M.; Aljebreen, A.M.M.; AlZamel, Z.A.; Fathala, A. Prevalence of noncalcified plaques and coronary artery stenosis in patients with coronary calcium scores of zero. Coron. Artery Dis. 2021, 32, 179–183. [Google Scholar] [CrossRef]
- Williams, M.C.; Kwiecinski, J.; Doris, M.; McElhinney, P.; D’Souza, M.S.; Cadet, S.; Adamson, P.D.; Moss, A.J.; Alam, S.; Hunter, A.; et al. Low-Attenuation Noncalcified Plaque on Coronary Computed Tomography Angiography Predicts Myocardial Infarction: Results from the Multicenter SCOT-HEART Trial (Scottish Computed Tomography of the HEART). Circulation 2020, 141, 1452–1462. [Google Scholar] [CrossRef]
- Osborne-Grinter, M.; Kwiecinski, J.; Doris, M.; McElhinney, P.; Cadet, S.; Adamson, P.D.; Moss, A.J.; Alam, S.; Hunter, A.; Shah, A.S.V.; et al. Association of coronary artery calcium score with qualitatively and quantitatively assessed adverse plaque on coronary CT angiography in the SCOT-HEART trial. Eur. Hear. J.—Cardiovasc. Imaging 2022, 23, 1210–1221. [Google Scholar] [CrossRef]
- Villines, T.C.; Hulten, E.A.; Shaw, L.J.; Goyal, M.; Dunning, A.; Achenbach, S.; Al-Mallah, M.; Berman, D.S.; Budoff, M.J.; Cademartiri, F.; et al. Prevalence and Severity of Coronary Artery Disease and Adverse Events Among Symptomatic Patients With Coronary Artery Calcification Scores of Zero Undergoing Coronary Computed Tomography Angiography: Results From the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) Registry. J. Am. Coll. Cardiol. 2011, 58, 2533–2540. [Google Scholar] [CrossRef]
- Rodriguez, K.; Kwan, A.C.; Lai, S.; Lima, J.A.; Vigneault, D.; Sandfort, V.; Pattanayak, P.; Ahlman, M.A.; Mallek, M.; Sibley, C.T.; et al. Coronary Plaque Burden at Coronary CT An-giography in Asymptomatic Men and Women. Radiology 2015, 277, 73–80. [Google Scholar] [CrossRef]
- Nezarat, N.; Budoff, M.J.; Luo, Y.; Darabian, S.; Nakanishi, R.; Li, D.; Sheidaee, N.; Kim, M.; Alani, A.; Matsumoto, S.; et al. Presence, Characteristics, and Volumes of Coronary Plaque Determined by Computed Tomography Angiography in Young Type 2 Diabetes Mellitus. Am. J. Cardiol. 2017, 119, 1566–1571. [Google Scholar] [CrossRef] [PubMed]
- Kral, B.G.; Becker, L.C.; Vaidya, D.; Yanek, L.R.; Qayyum, R.; Zimmerman, S.L.; Dey, D.; Berman, D.S.; Moy, T.F.; Fishman, E.K.; et al. Noncalcified Coronary Plaque Volumes in Healthy People with a Family History of Early Onset Coronary Artery Disease. Circ. Cardiovasc. Imaging 2014, 7, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.; Suh, J.-W.; Chang, H.-J.; Kim, K.-I.; Jeon, E.J.; Choi, S.I.; Cho, Y.-S.; Youn, T.-J.; Chae, I.-H.; Kim, C.-H.; et al. Prevalence and Prognostic Implication of Non-Calcified Plaque in Asymptomatic Population with Coronary Artery Calcium Score of Zero. Korean Circ. J. 2013, 43, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Chun, E.J.; Kim, K.J.; Kim, J.A.; Yoo, J.Y.; Choi, S.I. Asymptomatic subjects with zero coronary calcium score: Coronary CT angiographic features of plaques in event-prone patients. Int. J. Cardiovasc. Imaging 2013, 29, 29–36. [Google Scholar] [CrossRef]
- Yang, J.; Dou, G.; Tesche, C.; De Cecco, C.N.; Jacobs, B.E.; Schoepf, U.J.; Chen, Y. Progression of coronary atherosclerotic plaque burden and relationship with adverse cardiovascular event in asymptomatic diabetic patients. BMC Cardiovasc. Disord. 2019, 19, 39. [Google Scholar] [CrossRef]
- Jin, K.N.; Chun, E.J.; Lee, C.-H.; Kim, J.A.; Lee, M.S.; Choi, S.I. Subclinical coronary atherosclerosis in young adults: Prevalence, characteristics, predictors with coronary computed tomography angiography. Int. J. Cardiovasc. Imaging 2012, 28, 93–100. [Google Scholar] [CrossRef]
- Yoo, D.H.; Chun, E.J.; Choi, S.I.; Kim, J.A.; Jin, K.N.; Yeon, T.-J.; Choi, D.-J. Significance of noncalcified coronary plaque in asymptomatic subjects with low coronary artery calcium score: Assessment with coronary computed tomography angiography. Int. J. Cardiovasc. Imaging 2011, 27, 27–35. [Google Scholar] [CrossRef]
- Cho, I.; Al’Aref, S.J.; Berger, A.; Ó Hartaigh, B.; Gransar, H.; Valenti, V.; Lin, F.Y.; Achenbach, S.; Berman, D.S.; Budoff, M.J.; et al. Prognostic value of coronary computed tomographic angiography findings in asymptomatic individuals: A 6-year follow-up from the prospective multicentre international CONFIRM study. Eur. Heart J. 2018, 39, 934–941. [Google Scholar] [CrossRef]
- Lee, S.; Choi, E.-K.; Chang, H.-J.; Kim, C.-H.; Seo, W.-W.; Park, J.J.; Il, C.S.; Chun, E.-J.; Chang, S.-A.; Kim, H.-K.; et al. Subclinical Coronary Artery Disease as Detected by Coronary Computed Tomography Angiography in an Asymptomatic Population. Korean Circ. J. 2010, 40, 434–441. [Google Scholar] [CrossRef]
- Nasir, K.; Cainzos-Achirica, M.; Valero-Elizondo, J.; Ali, S.S.; Havistin, R.; Lakshman, S.; Blaha, M.J.; Blankstein, R.; Shapiro, M.D.; Arias, L.; et al. Coronary Atherosclerosis in an Asymptomatic, U.S. Population: Miami Heart Study at Baptist Health South Florida. JACC Cardiovasc. Imaging 2022, 15, 1604–1618. [Google Scholar] [CrossRef]
- Iwasaki, K.; Matsumoto, T.; Aono, H.; Furukawa, H.; Samukawa, M. Prevalence of non-calcified coronary plaque on 64-slice computed tomography in asymptomatic patients with zero and low coronary artery calcium. Can. J. Cardiol. 2010, 26, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Schepis, T.; Marwan, M.; Pflederer, T.; Seltmann, M.; Ropers, D.; Daniel, W.G.; Achenbach, S. Quantification of non-calcified coronary atherosclerotic plaques with dual-source computed tomography: Comparison with intravascular ultrasound. Heart 2010, 96, 610–615. [Google Scholar] [CrossRef] [PubMed]
- Obaid, D.R.; Calvert, P.A.; Gopalan, D.; Parker, R.A.; Hoole, S.P.; West, N.E.; Goddard, M.; Rudd, J.H.F.; Bennett, M.R. Atherosclerotic plaque composition and clas-sification identified by coronary computed tomography: Assessment of computed tomography-generated plaque maps com-pared with virtual histology intravascular ultrasound and histology. Circ. Cardiovasc. Imaging 2013, 6, 655–664. [Google Scholar] [CrossRef] [PubMed]
- Carrascosa, P.M.; Capuñay, C.M.; Garcia-Merletti, P.; Carrascosa, J.; Garcia, M.J. Characterization of Coronary Atherosclerotic Plaques by Multidetector Computed Tomography. Am. J. Cardiol. 2006, 97, 598–602. [Google Scholar] [CrossRef]
- Hara, T.; Yamada, S.; Hayashi, T.; Ikeda, Y.; Yamashiro, K.; Mizutani, K.; Iwata, S.; Okajima, K.; Tsukishiro, Y.; Matsumoto, K.; et al. Accuracy of Nonstenotic Coronary Atherosclerosis Assessment by Multi-Detector Computed Tomography. Circ. J. 2007, 71, 911–914. [Google Scholar] [CrossRef][Green Version]
- Sakakura, K.; Yasu, T.; Kobayashi, Y.; Katayama, T.; Sugawara, Y.; Funayama, H.; Takagi, Y.; Ikeda, N.; Ishida, T.; Tsuruya, Y.; et al. Noninvasive Tissue Characterization of Coronary Arterial Plaque by 16-Slice Computed Tomography in Acute Coronary Syndrome. Angiology 2006, 57, 155–160. [Google Scholar] [CrossRef]
- Hur, J.; Kim, Y.J.; Lee, H.J.; Nam, J.E.; Choe, K.O.; Seo, J.S.; Choi, D.H.; Kim, J.-S.; Choi, B.W. Quantification and characterization of obstructive coronary plaques using 64-slice computed tomography: A comparison with intravascular ultrasound. J. Comput. Assist. Tomogr. 2009, 33, 186–192. [Google Scholar] [CrossRef]
- Yang, X.; Gai, L.Y.; Li, P.; Chen, Y.D.; Li, T.; Yang, L. Diagnostic accuracy of dual-source CT angiography and coronary risk stratification. Vasc. Health Risk Manag. 2010, 6, 935–941. [Google Scholar] [CrossRef][Green Version]
| Reference | Publication (Month, Year) | Study Design | No. of Patients | Age (Years) | Male (%) | Patient Population | Prevalence of NCP | Follow-Up Available Y/N If Y, Duration: | Key Findings of the Study: |
|---|---|---|---|---|---|---|---|---|---|
| Hausleiter et al. [14] | July 2006 | Prospective | 161 | 41–69 | 69.5 | Symptomatic patients at intermediate risk for CAD | 29.8% (48 pts) isolated NCP in 10 (6.2%) | N | -The NCP were the only manifestation of CAD in 6.2% of the study population -Patients with noncalcified plaques were characterized by significantly higher LDL, C-reactive protein levels as well as a trend for more diabetes mellitus. |
| Nance. et al. [15] | September 2012 | Prospective | 458 | 55 ± 11 | 36 | Acute chest pain patients at low-to-intermediate risk for CAD | Isolated NCP in 215 (47%) | Y (13 months) | Events during follow-up: -None (plaque absent) -11/215 (5%) (isolated NCP) Independent predictor of MACE: -Extent of plaque (HR 151.77, p < 0.001) -Presence of mixed plaque (HR, 86.96; p = 0.002) |
| Liu et al. [16] | August 2017 | Randomized Controlled (ROMICAT II trial) | 501 (473 with CCTA) | 56.1 ± 7.8 | 62.7 | Acute chest pain patients presenting to ED without ischemic EKG changes or troponin elevation | -260/473 (54%) -Isolated NCP 197/260 (75.8%) -At least 1-HRP feature in 166 (63.8%) | N | -Spotty calcification: 151 (58.1%) -Positive remodeling: 55 (21.2%), -Low HU plaque: 39 (15.0%), NRS: 26 (10.0%) |
| Al-Muhaidb et al. [17] | May 2021 | Retrospective | 299 with 0 CACS | Chest pain with no prior history of CAD | Isolated NCP 6.4% (19/299) | Y (2 years) | -Patients with NCP: 52.6% had no stenosis; 26.3% had <25% stenosis; 21% had 25–50% stenosis; none had >50% stenosis. Strong correlation of NCP was noted with: -Male sex (p = 0.001); -Smoking (p = 0.004); -Hypertension, (p = 0.042). | ||
| William et al. [18] | 2020 | Randomized Controlled (SCOT-HEART Trial) | 1769 | 58 ± 10 | 56 | Patients with stable chest pain | - | Y (4.7 years) | LAP and associations: -CACS (r = 0.62; p < 0.001); -CV risk score (r = 0.34; p < 0.001); -luminal stenosis (r = 0.83; p < 0.001). -LAP burden was the strongest predictor of MI (aHR, 1.60 (95% CI, 1.10–2.34) per doubling; p = 0.014), irrespective of CV risk score, CACS, or stenosis percentage. >4% LAP burden → 5 × more likely to have MI (HR, 4.65; 95% CI, 2.06–10.5; p < 0.001). |
| Osborne-Grinter et al. [19] | 2022 | Randomized Controlled (SCOT-HEART Trial) | 1769 529 (36%) with 0 CACS | 58 ± 10 | 56 | Patients with stable chest pain | Isolated NCP 14% | Y (5 years) | -14% → non-obstructive CAD. -2% → obstructive CAD. -2% → adverse plaque visually. -13% → LAP burden > 4%. -41 MI in total population,4 in zero CACS (10%). |
| Villines et al. [20] | 2011 | CONFIRM registry | 10,037 5128 (51%) with 0 CACS | 57 ± 12 | 56 | Symptomatic patients without known CAD | Isolated NCP 13% | Y (2.1 years) | Patients with zero CACS: -13% → nonobstructive stenosis -3.5% → >50% stenosis -1.4% → >70% stenosis -3.9% with a CACS zero and ≥50% stenosis experienced an event (HR: 5.7; 95% CI: 2.5 to 13.1; p < 0.001) vs. 0.8% of patients with CACS zero and no obstructive CAD |
| Reference | Month/Year | Design | No. of Patients | Patient Population | Age (Years) | Women (%) | Prevalence of NCP | Median Follow Up (Y/N) | Outcome Variable | Key Findings of the Study |
|---|---|---|---|---|---|---|---|---|---|---|
| Rodriguez et al. [21] | June 2015 | Prospective | 202 | Asymptomatic > 55 years old eligible for statin therapy | 65.5 ± 6.9 | 36 | - | Y (8 years) | Assessment of coronary plaque burden | Total plaque index: >In men vs. women by 5.01 mm2; p < 0.03); >In patients on increased simvastatin doses (by 0.44 mm2/10 mg; p = 0.02). NCP index was positively correlated with: -Systolic BP (β = 0.80 mm2/10 mm Hg; p = 0.03); -Diabetes (β = 4.47 mm2; p = 0.03); -LDL (β = 0.04 mm2/mg/dL; p = 0.02). |
| Nezarat et al. [22] | March 2017 | Prospective, case–control | 181 | Asymptomatic -86 DM patients (25–40 years) with ≥5 years DM type II. -95 non-DM age-/gender-matched. | 25–40 | DM: 56 Non-DM: 46 | In DM with zero CACS 46% | N | Extent, severity, and volumes of coronary plaque in DM patients < 40 years of age | -Prevalence of any plaque: 59% (DM); 20% (no DM). -Total plaque scores, segment involvement scores, and quantitative plaque volume increased in DM. |
| Kral et al. [23] | May 2014 | Prospective | 805 | Gene STAR family study (4000 pts). Asymptomatic patients with no prior CAD were included. | 51.1 ± 10.8 | 56 | NCP volume most accounted for in all age -In men < 55 (>70%) -In women < 55 (>80%) | N | Assessment of NCP volumes in patients with family history of early-onset CAD. | -NCP volume increased with age (p < 0.001). -NCP higher in men than women (p < 0.001). -NCP, as a percentage of total plaque, was inversely related to age (p < 0.01). |
| Cho et al. [24] | March 2013 | Retrospective | 4491 with 0 CACS | Asymptomatic subjects undergoing CCTA as part of general health evaluation | 48 ± 8 | 43 | 7% (313 pts) | Y (22 months) | Prevalence and prognostic valve of NCP | -No clinical events at 90 days regardless of presence of NCP. |
| Lee et al. [25] | June 2013 | Retrospective | 8668 (6531 with 0 CACS) | Asymptomatic patients without prior CAD undergoing CCTA as part of general health evaluation | 49.8 ± 8.9 | 44 | 6.75% (441 pts) | Y (26.4 +/− 14.4 months) | Cardiac events (death, ACS, or subsequent revascularization) | -All cardiac events 0.18% (12 pts) occurred in patients with NCP and with lower HU and higher RI. |
| Yang et al. [26] | February 2019 | Retrospective | 197 | Asymptomatic with DM and suspected CAD with baseline and follow-up CCTA. | 63.1 ± 17 | 40 | - | Y (41.8 months) | -Progression of coronary atherosclerotic plaque. -Association of plaque with cardiac outcomes (cardiac death, non-fatal MI, and revascularization). | -Patients with CACS ≤ 10 had a more pronounced increase in the volume of LAP on CCTA; while -Presence of CACS > 10 had an increase in dense coronary calcium; -10.2% (20 patients) with events (CAC, CAC density and lipid volume independently predicted events). |
| Jin et al. [27] | October 2012 | Retrospective | 914 | Asymptomatic adults under 45 years old without known cardiovascular disease who had undergone CCTA. | 40.4 ± 3.4 (men) 40.7 ± 2.9 (women) | 40 | -6.9% (63 pts). -58% of the segments (most common) 5.3% (46 pts) in 0 CACS 42.5% (17 pts) in CACS > 0) | - | -Characteristics and predictors of subclinical coronary atherosclerosis -Cardiac events (cardiac death, non-fatal MI, unstable angina, revascularization > 90 days after CCTA) | -Male gender, diabetes mellitus, and amount of smoking → independent predictors of NCP. -On multivariate analysis: 2.2 HR for subclinical coronary atherosclerosis and 49.17 HR for NCP. |
| Yoo et al. [28] | December 2011 | Retrospective | 7515 -6040 (80.4%) with 0 CACS -707 (9.4%) with low CACS | 30.2 | 0 CACS: 6.9% Low CACS:31.5% | Y (4 years) | Significance of non-calcified coronary plaque. | -Cardiac events in low CACS 2.6% vs. 0.27% in 0 CACS (p < 0.001). | ||
| Cho et al. [29] | March 2018 | Prospective multicentered registry (CONFIRM long-term study) | 1226 selected from 17,181 pts. | Asymptomatic with no prior CAD history and no intervention < 90 days from CCTA. | 58 ± 12 | 34 | - | Y (5.9 ± 1.2 years) | -Comprehensive CAD assessment by CCTA improves risk prediction for future mortality over a traditional RF model and also when CACS was considered. | -78 deaths at follow-up. -Compared with the traditional RF alone (C-statistic 0.64), CCTA detection of plaque improved incremental prognostic utility beyond traditional RF alone (C-statistics range 0.71–0.73, all p < 0.05; incremental χ2 range 20.7–25.5, all p < 0.001). -NCP or mixed plaque in a single segment (HR 2.34, 95% CI 1.23–4.48; p = 0.010) or multi-segments (HR 2.50, 95% CI 1.48–4.21; p = 0.001) were shown to increase the risk of all-cause death as compared with individuals without any plaque, even after adjustment of traditional RF. |
| Lee et al. [30] | September 2010 | Prospective | 4320 | Asymptomatic individuals who underwent CCA during a routine health check. | 50 ± 9 years | 39 | Prevalence of isolated NCP 5% (801 pts) | N | Determine the prevalence and characteristics of subclinical CAD using CCTA | -Coronary artery plaques were present in 1053 (24%) individuals. -25% (10 pts) with NCP had significant stenosis; most of them were classified into low- or moderate-risk groups according to NCEP risk stratification guidelines. -Amongst men (≤55 years) and women (≤65 years), 30% of subjects with significant stenosis were classified into a low-risk group by NCEP amongst which 60% had low (0 to 100) calcium scores. |
| Nasir et al. [31] | September 2022 | Prospective | 2359 | Asymptomatic individuals from Greater Miami Area. | Mean age 53 years | 50 | Prevalence of isolated NCP 16% | -N | Assess the burden of total coronary plaque, plaque subtypes, and HRP features. | -49% had plaque on CCTA. -58% participants had CACS of 0. -0.8% with CACS 0 had ≥ 50% stenosis; 0.1% had stenosis ≥ 70%. -2.3% of the plaques in 0 CACS were HRP. -Male sex, overweight, and obesity were independent predictors of plaque if CAC was 0. |
| Iwasaki et al. [32] | August 2010 | Retrospective | -502 -224 patients with 0/mild CACS. | Asymptomatic individuals evaluated in an outpatient primary prevention program. | 62.4 ± 10.4 (no CAC) 67.4 ± 8.5 (mild CAC) | 41 | -Prevalence of NCP was 11.1% in patients with no CAC -Prevalence of NCP was 23.4% in mild CAC group (p = 0.0142) | -N | Assess prevalence of NCP | -Patients with no CAC were younger. -Multiple plaques were detected in 2.6% of the group with no CAC and 3.7% of the group with mild CAC (p = 0.5934). |
| Reference | Month/Year | Study Population | Purpose of the Study | Key Findings of the Study | Limitations of CCTA: |
|---|---|---|---|---|---|
| Obaid et al. [34] | August 2013 | 57 | Compare CT generated plaque maps with IVUS-VH. | Correlation between CT and IVUS: Necrotic core: r = 0.41 (p = 0.002); Fibrous plaque: r = 0.54 (p < 0.001); Calcified plaque: r = 0.59 (p < 0.001); Total plaque: r = 0.62 (p < 0.001). Diagnostic accuracy of CT vs. IVUS-VH: Calcified plaque (83% versus 92%); Necrotic core (80% versus 65%); Fibroatheroma (80% versus 79%). | -VH-IVUS could identify TCFA with a diagnostic accuracy between 74% and 82% (depending on the TCFA definition used). -Spatial resolution of CCTA prevents direct identification of TCFA. |
| Carrascosa et al. [35] | March 2006 | 40 (Mean age: 52, 80% Males) | Compare plaque composition between DSCT and IVUS. | 276 plaques examined by IVUS and DSCT. -Calcified plaque (using CT cut off of 185 HU identified 273/276 plaques (99%). -Fibrous/soft plaques (using CT cut off of 88 HU identified 192/233 (82%)) | -Results were obtained utilizing a 4-detector scanner with no multicycle reconstruction capability. |
| Schepis et al. [33] | April 2010 | 70 -100 individual NCP (1 to 3 plaques per patient) | Compare NCP volumes on DSCT vs. IVUS. | -Mean total plaque volume by DSCT was 89 ± 66 mm3 (range 14–400 mm3). -Mean total plaque volume by IVUS was 90 ± 73 mm3 (range 16–409 mm3). The mean difference between DSCT and IVUS was 1 ± 34 mm3 (range −131–85 mm3). -Correlation between two modalities (r = 0.89, p < 0.001) | -Modest agreement between DSCT and IVUS (Bland–Altman limits of agreement −67 to +65 mm3). |
| Hara et al. [36] | June 2007 | 33 | Accuracy of non-stenotic atherosclerotic assessment using CCTA vs. IVUS. | -56 proximal lesions from 33 patients assessed. -vessel size R2 = 0.614. -lumen size R2 = 0.750. -percentage plaque R2 = 0.824. | - |
| Sakakura et al. [37] | March 2006 | 16 | Plaque characterization in patients within 7 days from ACS using combined CCTA and IVUS | -23 plaques identified by IVUS (6 soft, 11 intermediate, and 6 calcified plaques). -CT HU for these plaques: Soft → 50.6 ± 14.8 HU Intermediate → 131 ± 1.0 HU Calcified → 721 ± 231 HU | - |
| Hur et al. [38] | March 2009 | 39 | Quantification and characterization of obstructive coronary plaque using 64-slice CCTA compared to IVUS | Correlation coefficients: -Lumen r = 0.712 -Vessel r = 0.654 -Plaque area r = 0.753 -Percentage luminal obstruction r = 0.799 Mean CT density values for plaque: Soft (n = 10) 54 ± 13 HU Fibrous (n = 11) 82 ± 17 HU Mixed (n = 31) 162 ± 57 HU Calcified plaques (n = 9) 392 ± 155 HU | CT density measurements not significantly different between soft and fibrous plaques (p = 0.224). -Reliable classification of NCP as vulnerable or stable plaque based on CT density measurements is currently limited. |
| Yang et al. [39] | October 2010 | 46 | Assessment of diagnostic accuracy of DSCT compared to IVUS | -Correlation coefficients: -Luminal cross-sectional area 0.82 (p < 0.01, CI 0.67–0.89). -External elastic membrane cross-sectional area 0.78 (p < 0.01, CI 0.67–0.86). -No significant difference in the distributive characteristics of the lesions in patients with NSTEMI and stable angina pectoris patients was noted. | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alyami, B.; Santer, M.; Seetharam, K.; Velu, D.; Gadde, E.; Patel, B.; Hamirani, Y.S. Non-Calcified Coronary Artery Plaque on Coronary Computed Tomography Angiogram: Prevalence and Significance. Tomography 2023, 9, 1755-1771. https://doi.org/10.3390/tomography9050140
Alyami B, Santer M, Seetharam K, Velu D, Gadde E, Patel B, Hamirani YS. Non-Calcified Coronary Artery Plaque on Coronary Computed Tomography Angiogram: Prevalence and Significance. Tomography. 2023; 9(5):1755-1771. https://doi.org/10.3390/tomography9050140
Chicago/Turabian StyleAlyami, Bandar, Matthew Santer, Karthik Seetharam, Dhivya Velu, Eswar Gadde, Bansari Patel, and Yasmin S. Hamirani. 2023. "Non-Calcified Coronary Artery Plaque on Coronary Computed Tomography Angiogram: Prevalence and Significance" Tomography 9, no. 5: 1755-1771. https://doi.org/10.3390/tomography9050140
APA StyleAlyami, B., Santer, M., Seetharam, K., Velu, D., Gadde, E., Patel, B., & Hamirani, Y. S. (2023). Non-Calcified Coronary Artery Plaque on Coronary Computed Tomography Angiogram: Prevalence and Significance. Tomography, 9(5), 1755-1771. https://doi.org/10.3390/tomography9050140







