A Rare Case of Thymic Rosai-Dorfman Disease Mimicking Malignancy on 18F-FDG PET/CT
Abstract
1. Background
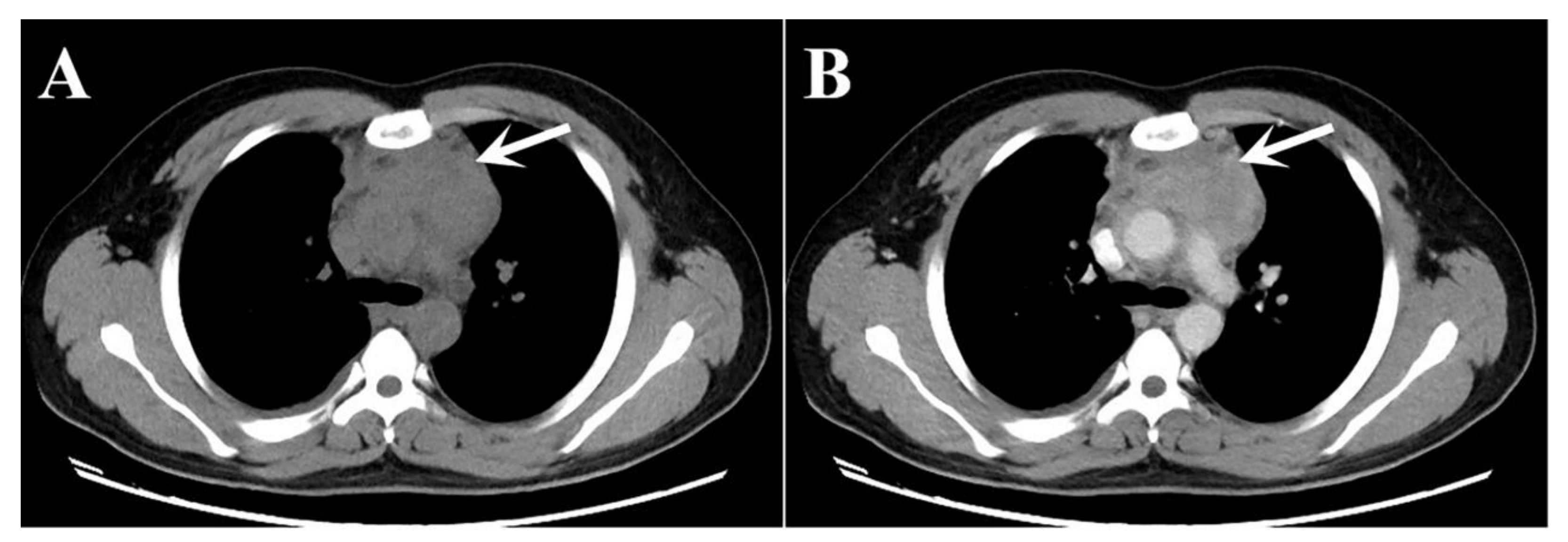
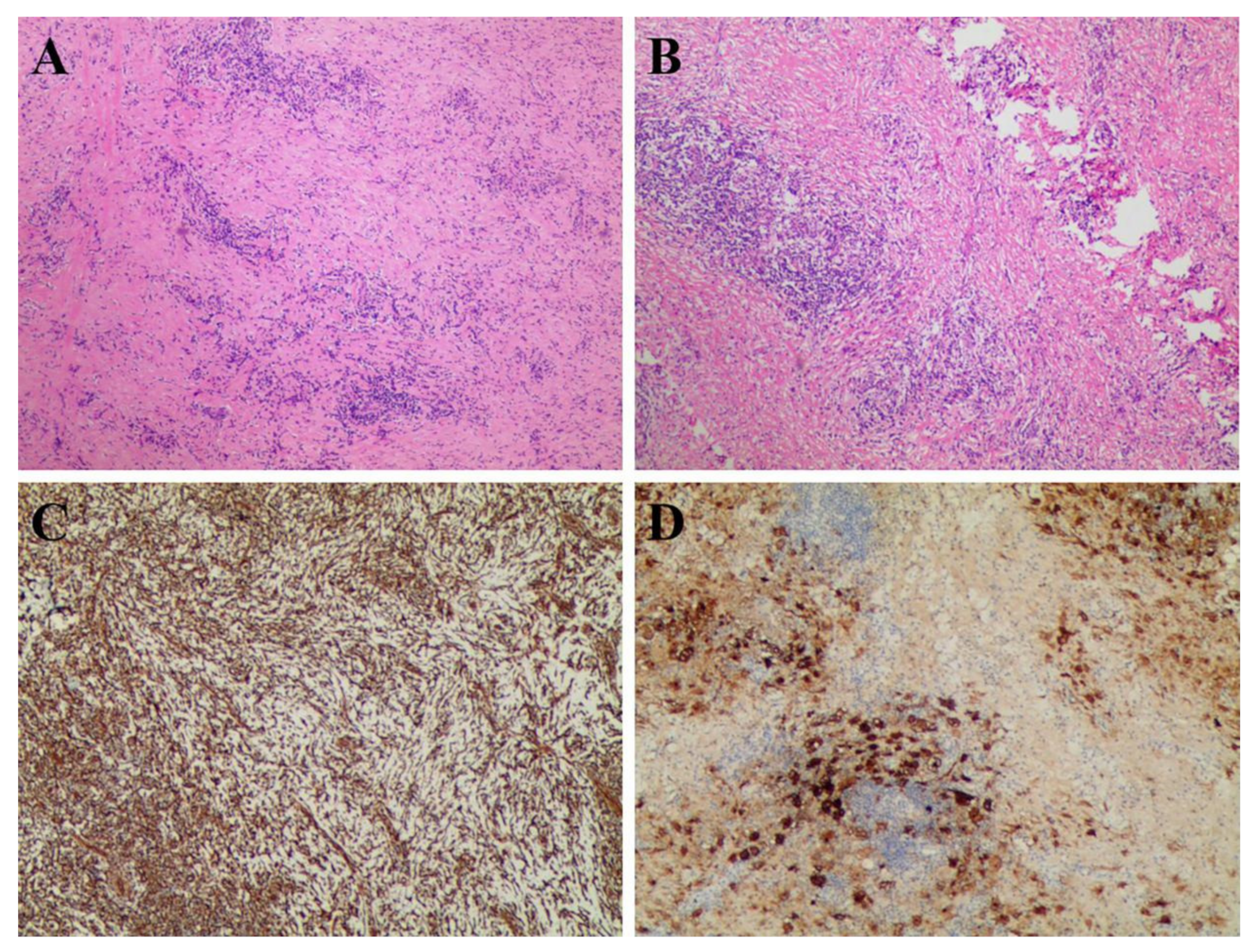
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosai, J.; Dorfman, R.F. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch Pathol. 1969, 87, 63–70. [Google Scholar] [PubMed]
- Henter, J.I.; Elinder, G.; Söder, O.; Ost, A. Histiocytosis syndromes in children. Lancet 1987, 1, 1091–1092. [Google Scholar] [CrossRef] [PubMed]
- Bruce-Brand, C.; Schneider, J.W.; Schubert, P. Rosai-Dorfman disease: An overview. J. Clin. Pathol. 2020, 73, 697–705. [Google Scholar] [CrossRef] [PubMed]
- Usmani, S.; Ahmed, D.A.T.; Elhaggracy, R.S.; Pinto, K.; Al Kandari, F. Rosai-Dorman disease mimicking lymphoma on 18F-FDG PET/CT. J. Pak. Med. Assoc. 2022, 72, 579–580. [Google Scholar] [CrossRef] [PubMed]
- Foucar, E.; Rosai, J.; Dorfman, R. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): Review of the entity. Semin. Diagn. Pathol. 1990, 7, 19–73. [Google Scholar] [PubMed]
- Liu, B.; Lee, N.J.; Otero, H.J.; Servaes, S.; Zhuang, H. Rosai-Dorfman disease mimics lymphoma on FDG PET/CT in a pediatric patient. Clin. Nucl. Med. 2014, 39, 206–208. [Google Scholar] [CrossRef]
- Ahmed, A.; Crowson, N.; Magro, C.M. A comprehensive assessment of cutaneous Rosai-Dorfman disease. Ann. Diagn. Pathol. 2019, 40, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Bai, Y.; Dong, A.; Zuo, C. FDG PET/CT in Isolated Thoracic Vertebral Rosai-Dorfman Disease. Clin. Nucl. Med. 2022, 47, e135–e136. [Google Scholar] [CrossRef] [PubMed]
- Zadeh, M.Z.; Wen, Z.; States, L.J.; Zhuang, H. An isolated osseous Rosai-Dorfman disease shown on FDG PET/CT. Clin. Nucl. Med. 2019, 44, 485–488. [Google Scholar] [CrossRef] [PubMed]
- Lim, R.; Wittram, C.; Ferry, J.A.; Shepard, J.A. FDG PET of Rosai-Dorfman disease of the thymus. AJR Am. J. Roentgenol. 2004, 182, 514. [Google Scholar] [CrossRef] [PubMed]
- Emile, J.F.; Abla, O.; Fraitag, S.; Horne, A.; Haroche, J.; Donadieu, J.; Requena-Caballero, L.; Jordan, M.B.; Abdel-Wahab, O.; Allen, C.E.; et al. Histiocyte Society. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood 2016, 127, 2672–2681. [Google Scholar] [CrossRef] [PubMed]
- Haghighat Jahromi, A.; Goodman, A.M.; Hoh, C.K. Rosai-Dorfman-Destombes (RDD) disease presenting as palindromic rheumatism. BMC Med. Imaging 2021, 21, 72. [Google Scholar] [CrossRef] [PubMed]
- Mosheimer, B.A.; Oppl, B.; Zandieh, S.; Fillitz, M.; Keil, F.; Klaushofer, K.; Weiss, G.; Zwerina, J. Bone Involvement in Rosai-Dorfman Disease (RDD): A Case Report and Systematic Literature Review. Curr. Rheumatol. Rep. 2017, 19, 29. [Google Scholar] [CrossRef] [PubMed]
- Xue, Q.; Miao, W. Spontaneous Recovery of Rosai-Dorfman Disease on FDG PET/CT. Clin. Nucl Med. 2017, 42, 608–609. [Google Scholar] [CrossRef] [PubMed]
- Karunanithi, S.; Singh, H.; Sharma, P.; Naswa, N.; Kumar, R. 18F-FDG PET/CT imaging features of Rosai Dorfman disease: A rare cause of massive generalized lymphadenopathy. Clin. Nucl. Med. 2014, 39, 268–269. [Google Scholar] [CrossRef] [PubMed]
- Furia, S.; Nannini, N.; Pascarella, A.; Breda, C. Mediastinal Rosai-Dorfman Disease with Widespread Lesions: When Surgical Biopsy Is Needed. Ann. Thorac. Surg. 2020, 109, e45–e47. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jia, T.; Zhang, B.; Zhang, X.; Xu, X.; Sang, S.; Deng, S. A Rare Case of Thymic Rosai-Dorfman Disease Mimicking Malignancy on 18F-FDG PET/CT. Tomography 2022, 8, 2839-2843. https://doi.org/10.3390/tomography8060237
Jia T, Zhang B, Zhang X, Xu X, Sang S, Deng S. A Rare Case of Thymic Rosai-Dorfman Disease Mimicking Malignancy on 18F-FDG PET/CT. Tomography. 2022; 8(6):2839-2843. https://doi.org/10.3390/tomography8060237
Chicago/Turabian StyleJia, Tongtong, Bin Zhang, Xiaoyi Zhang, Xin Xu, Shibiao Sang, and Shengming Deng. 2022. "A Rare Case of Thymic Rosai-Dorfman Disease Mimicking Malignancy on 18F-FDG PET/CT" Tomography 8, no. 6: 2839-2843. https://doi.org/10.3390/tomography8060237
APA StyleJia, T., Zhang, B., Zhang, X., Xu, X., Sang, S., & Deng, S. (2022). A Rare Case of Thymic Rosai-Dorfman Disease Mimicking Malignancy on 18F-FDG PET/CT. Tomography, 8(6), 2839-2843. https://doi.org/10.3390/tomography8060237






