Myocarditis Following COVID-19 Vaccination: Cardiac Imaging Findings in 118 Studies
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction and Synthesis
3. Results
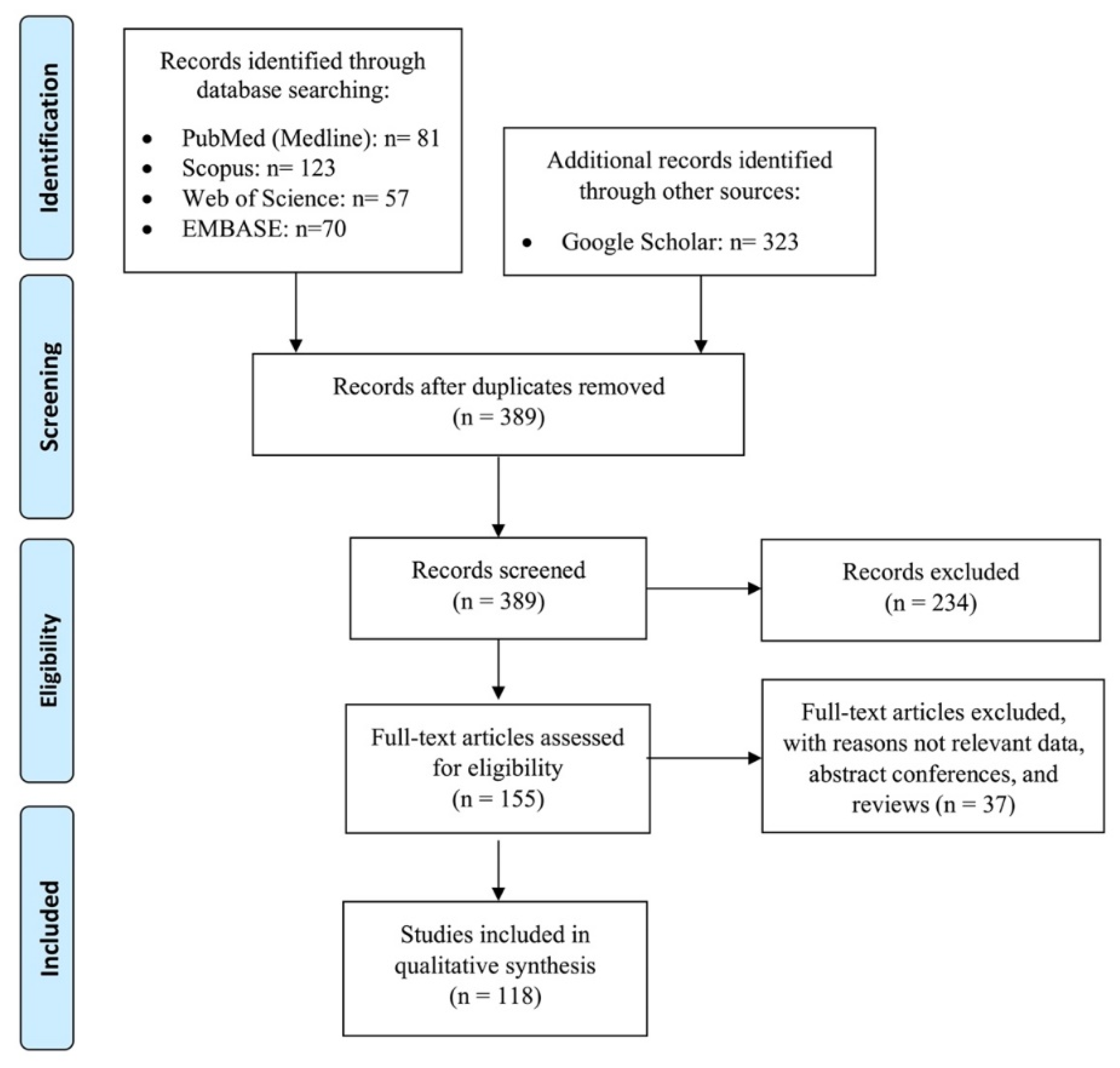
3.1. Literature Search
3.2. Patients’ Characteristics
3.3. Clinical and Laboratory Findings
3.4. Presentation Date
3.5. Imaging Findings
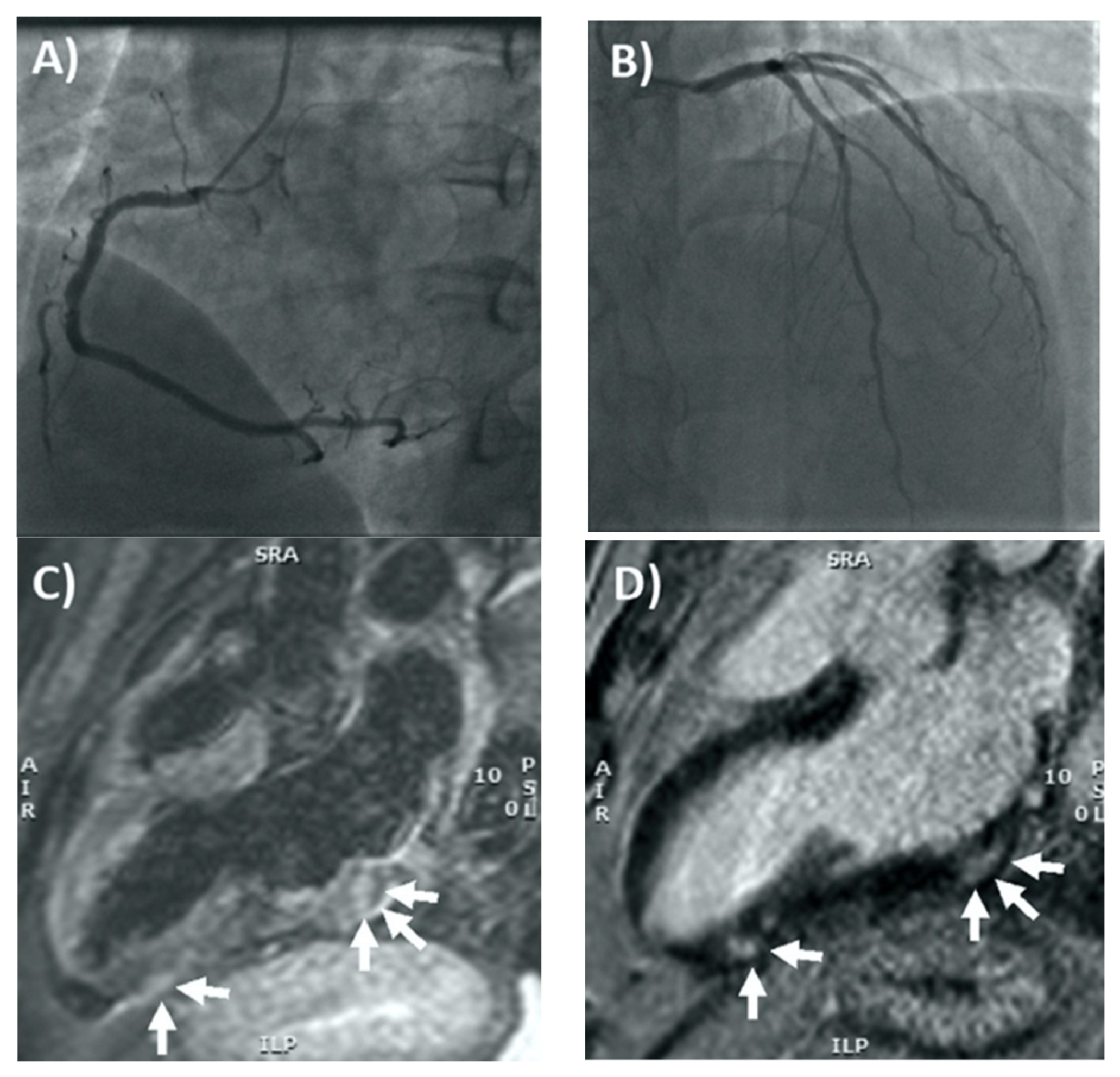
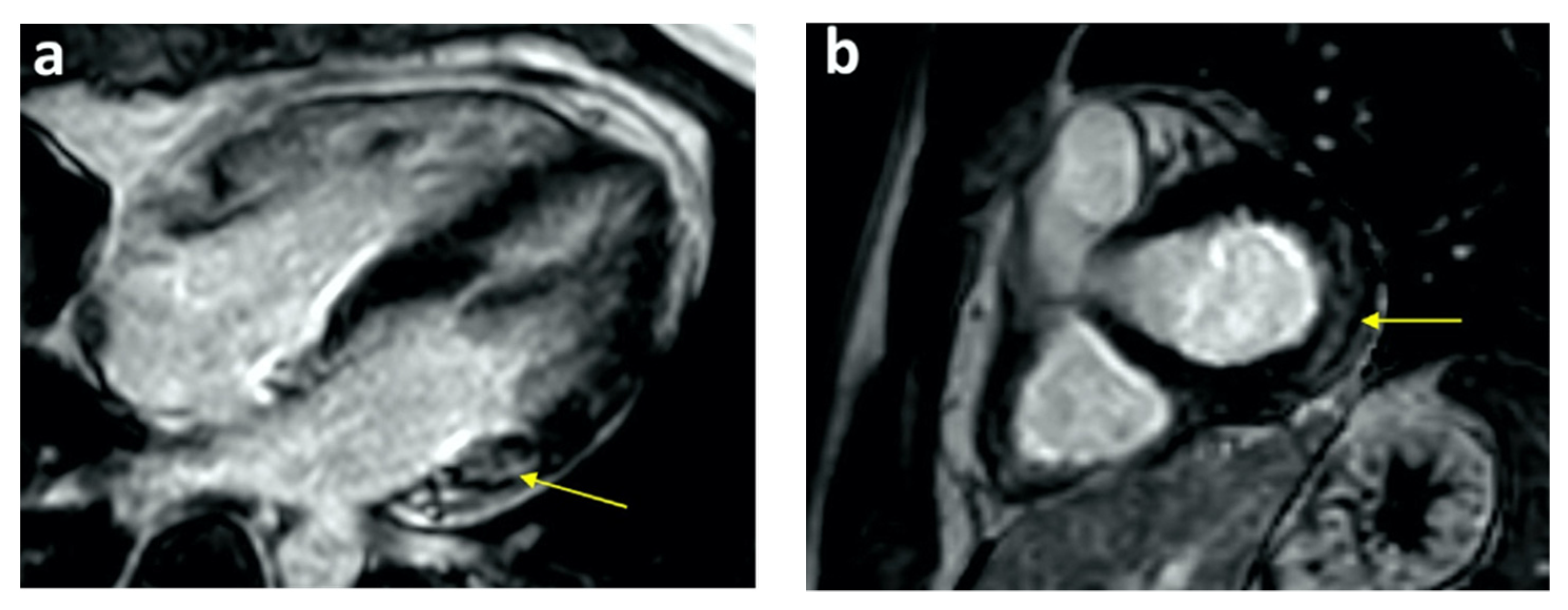
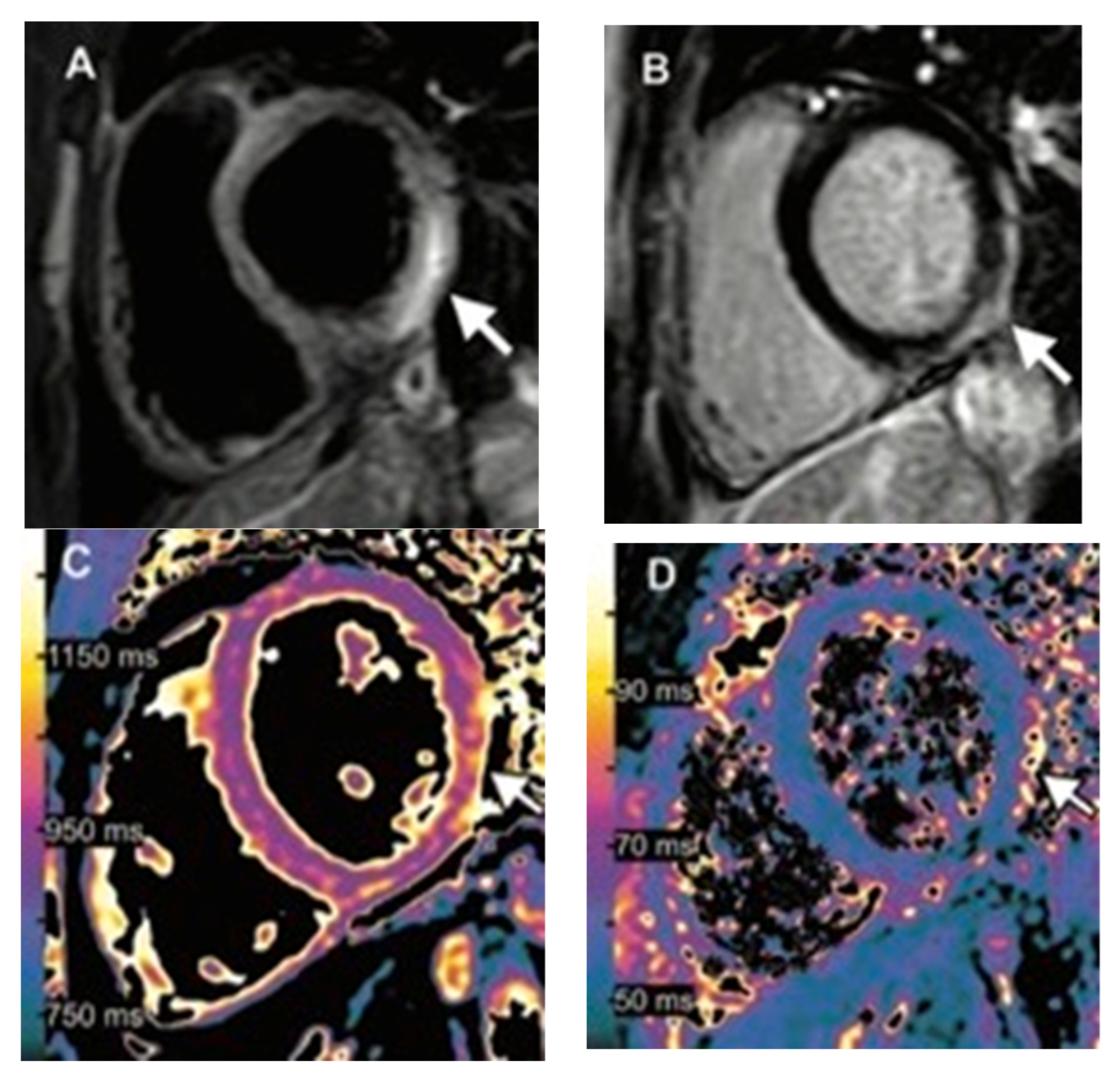
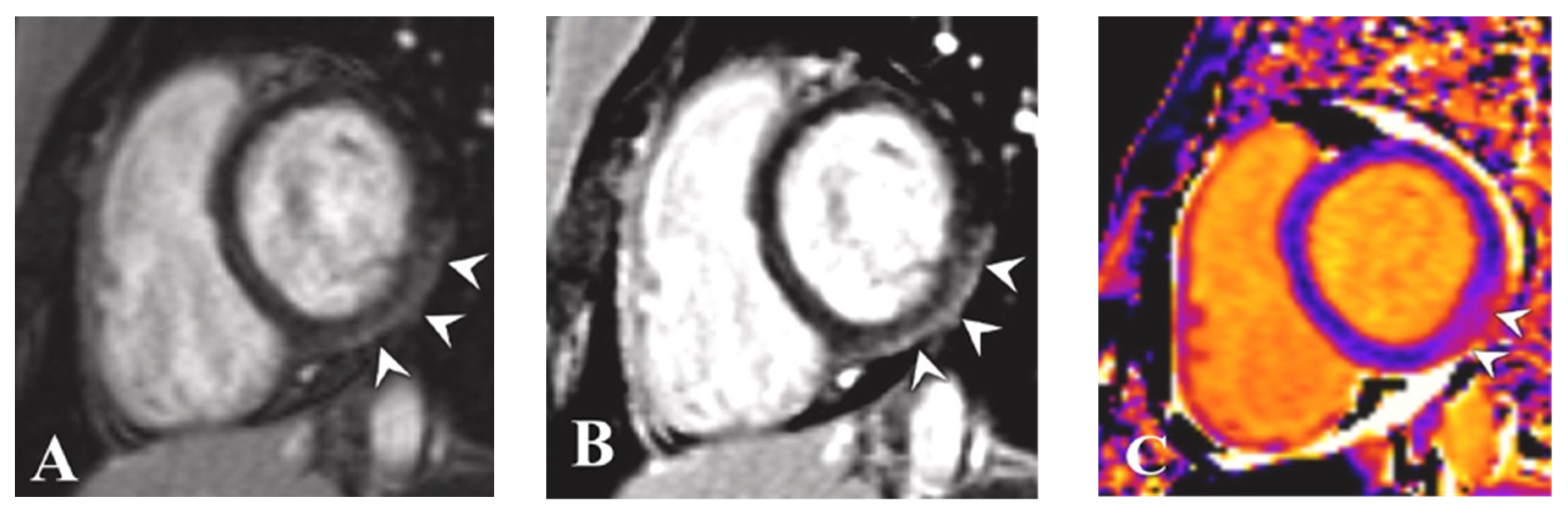
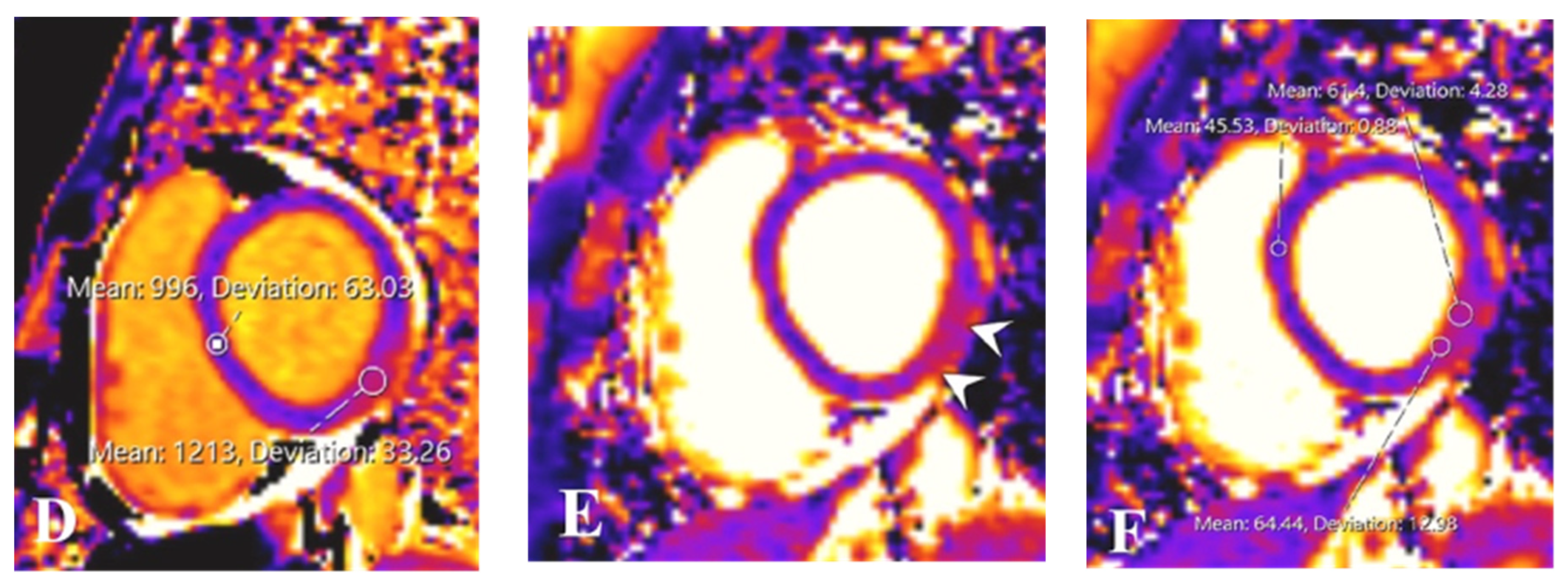
3.5.1. CMRI and CCTA
3.5.2. Echocardiography
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
Appendix A
- Keyword Search Strategy
- Medline (PubMed)
- (“coronavirus 2” [Title/Abstract] OR “coronavirus 2” [Mesh] OR “coronavirus infections” [Title/Abstract] OR “coronavirus infections” [Mesh] OR “COVID-19” [Title/Abstract] OR “COVID-19” [Mesh] OR “coronavirus” [Title/Abstract] OR “coronavirus” [Mesh] OR “2019-nCoV” [Title/Abstract] OR “COVID-2019” [Title/Abstract] OR “COVID19” [Title/Abstract] OR “nCoV” [Title/Abstract] OR “coronavirus disease 2019” [Title/Abstract] OR “2019 novel coronavirus” [Title/Abstract] OR “severe acute respiratory syndrome” [Title/Abstract] OR “SARS-CoV-19” [Title/Abstract] OR “SARS-CoV-2” [Title/Abstract] OR “2019-CoV-19” [Title/Abstract] OR “SARS-CoV” [Title/Abstract] OR “2019nCoV” [Title/Abstract] OR “coronavirinae” [Title/Abstract] OR “2019 Novel Coronavirus Infection” [Title/Abstract] OR “2019 nCoV Infection” [Title/Abstract] OR “Bat coronavirus” [Title/Abstract] OR “betacoronavirus*” [Title/Abstract] OR “coronavirus Infection Disease 2019” [Title/Abstract] OR “COVID*” [Title/Abstract] OR “Novel Coronavirus Pneumonia” [Title/Abstract] OR “Wuhan virus” [Title/Abstract]) AND (“Vaccination” [Title/Abstract] OR “Vaccination” [Mesh] OR “Vaccines” [Title/Abstract] OR “Vaccines” [Mesh] OR “Mass Vaccination” [Title/Abstract] OR “Mass Vaccination” [Mesh] OR “Immunization” [Title/Abstract] OR “Immunization” [Mesh] OR “Immunization Programs” [Title/Abstract] OR “Immunization Programs” [Mesh] OR “Vaccination*” [Title/Abstract] OR “Vaccin*” [Title/Abstract] OR “Vaccination program” [Title/Abstract] OR “Vaccine” [Title/Abstract] OR “Vaccine-mediated protection” [Title/Abstract] OR “Post-vaccine” [Title/Abstract] OR “Post vaccine” [Title/Abstract] OR “Vaccination-induced” [Title/Abstract] OR “Post-vaccination” [Title/Abstract] OR “Post vaccination” [Title/Abstract] OR “Immunization*” [Title/Abstract] OR “Pfizer vaccine” [Title/Abstract] OR “Pfizer-BioNTech COVID-19 vaccine” [Title/Abstract] OR “Moderna vaccine” [Title/Abstract] OR “mRNA vaccine” [Title/Abstract] OR “Astra-Zeneca vaccine” [Title/Abstract] OR “anti-SARS-CoV-2 vaccine” [Title/Abstract] OR “BNT162b2 mRNA COVID-19 vaccine” [Title/Abstract]) AND (“Myocarditis” [Title/Abstract] OR “Myocarditis” [Mesh] OR “Myopericarditis” [Title/Abstract] OR “Cardiomayopathy” [Title/Abstract] OR “Pricarditis” [Title/Abstract] OR “Myocardial lesion” [Title/Abstract] OR “acute myocarditis” [Title/Abstract] OR “myocard*” [Title/Abstract] OR “Dilated Cardiomyopathy” [Title/Abstract])
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Yazdanpanah, F.; Hamblin, M.R.; Rezaei, N. The immune system and COVID-19: Friend or foe? Life Sci. 2020, 256, 117900. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention COVID Data Tracker. 2021. Available online: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (accessed on 29 July 2021).
- Le, T.T.; Cramer, J.P.; Chen, R.; Mayhew, S. Evolution of the COVID-19 vaccine development landscape. Nat. Rev. Drug Discov. 2020, 19, 667–668. [Google Scholar] [CrossRef]
- Thanh Le, T.; Andreadakis, Z.; Kumar, A.; Gómez Román, R.; Tollefsen, S.; Saville, M.; Mayhew, S. The COVID-19 vaccine development landscape. Nat. Rev. Drug Discov. 2020, 19, 305–306. [Google Scholar] [CrossRef]
- Keshavarz, P.; Yazdanpanah, F.; Rafiee, F.; Mizandari, M. Lymphadenopathy following COVID-19 Vaccination: Imaging Findings Review. Acad. Radiol. 2021, 28, 1058–1071. [Google Scholar] [CrossRef]
- Diaz, G.A.; Parsons, G.T.; Gering, S.K.; Meier, A.R.; Hutchinson, I.V.; Robicsek, A. Myocarditis and Pericarditis after Vaccination for COVID-19. JAMA 2021, 326, 1210–1212. [Google Scholar] [CrossRef] [PubMed]
- Isaak, A.; Feisst, A.; Luetkens, J.A. Myocarditis following COVID-19 Vaccination. Radiology 2021, 301, E378–E379. [Google Scholar] [CrossRef] [PubMed]
- Nassar, M.; Nso, N.; Gonzalez, C.; Lakhdar, S.; Alshamam, M.; Elshafey, M.; Abdalazeem, Y.; Nyein, A.; Punzalan, B.; Durrance, R.J.; et al. COVID-19 vaccine-induced myocarditis case report with literature review. Diabetes Metab. Syndr. 2021, 15, 102205. [Google Scholar] [CrossRef] [PubMed]
- Bangalore, S.; Sharma, A.; Slotwiner, A.; Yatskar, L.; Harari, R.; Shah, B.; Ibrahim, H.; Friedman, G.H.; Thompson, C.; Alviar, C.L.; et al. ST-Segment Elevation in Patients with Covid-19—A Case Series. N. Engl. J. Med. 2020, 382, 2478–2480. [Google Scholar] [CrossRef] [PubMed]
- Tajbakhsh, A.; Gheibi Hayat, S.M.; Taghizadeh, H.; Akbari, A.; Inabadi, M.; Savardashtaki, A.; Johnston, T.P.; Sahebkar, A. COVID-19 and cardiac injury: Clinical manifestations, biomarkers, mechanisms, diagnosis, treatment, and follow up. Expert Rev. Anti. Infect. Ther. 2021, 19, 345–357. [Google Scholar] [CrossRef]
- Siripanthong, B.; Nazarian, S.; Muser, D.; Deo, R.; Santangeli, P.; Khanji, M.Y.; Cooper, L.T.; Chahal, C.A.A. Recognizing COVID-19–related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020, 17, 1463–1471. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Cavalotti, C.; Milazzo, A.; Pedrotti, P.; Soriano, F.; Schroeder, J.W.; Morici, N.; Giannattasio, C.; Frigerio, M.; Metra, M.; et al. Temporal Relation between Second Dose BNT162b2 mRNA Covid-19 Vaccine and Cardiac involvement in a Patient with Previous SARS-COV-2 Infection. Int. J. Cardiol. Heart Vasc. 2021, 34, 100774. [Google Scholar] [CrossRef] [PubMed]
- Habib, M.B.; Hamamyh, T.; Elyas, A.; Altermanini, M.; Elhassan, M. Acute myocarditis following administration of BNT162b2 vaccine. IDCases 2021, 25, e01197. [Google Scholar] [CrossRef] [PubMed]
- Mansour, J.; Short, R.G.; Bhalla, S.; Woodard, P.K.; Verma, A.; Robinson, X.; Raptis, D.A. Acute myocarditis after a second dose of the mRNA COVID-19 vaccine: A report of two cases. Clin. Imaging 2021, 78, 247–249. [Google Scholar] [CrossRef] [PubMed]
- McLean, K.; Johnson, T.J. Myopericarditis in a previously healthy adolescent male following COVID-19 vaccination: A case report. Acad. Emerg. Med. 2021, 28, 918–921. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, B.; Kamat, I.; Hotez, P.J. Myocarditis with COVID-19 mRNA Vaccines. Circulation 2021, 144, 471–484. [Google Scholar] [CrossRef] [PubMed]
- Fazlollahi, A.; Zahmatyar, M.; Noori, M.; Nejadghaderi, S.A.; Sullman, M.J.M.; Shekarriz-Foumani, R.; Kolahi, A.; Singh, K.; Safiri, S. Cardiac complications following mRNA COVID-19 vaccines: A systematic review of case reports and case series. Rev. Med. Virol. 2022, 32, e2318. [Google Scholar] [CrossRef] [PubMed]
- Shiyovich, A.; Witberg, G.; Aviv, Y.; Eisen, A.; Orvin, K.; Wiessman, M.; Grinberg, T.; Porter, A.; Kornowski, R.; Hamdan, A. Myocarditis following COVID-19 vaccination: Magnetic resonance imaging study. Eur. Heart J. Cardiovasc. Imaging 2021, 23, jeab230. [Google Scholar] [CrossRef]
- Kuntz, J.; Crane, B.; Weinmann, S.; Naleway, A.L.; Vaccine Safety Datalink Investigator Team. Myocarditis and pericarditis are rare following live viral vaccinations in adults. Vaccine 2018, 36, 1524–1527. [Google Scholar] [CrossRef]
- Yamamoto, H.; Hashimoto, T.; Ohta-Ogo, K.; Ishibashi-Ueda, H.; Imanaka-Yoshida, K.; Hiroe, M.; Yokochi, T. A case of biopsy-proven eosinophilic myocarditis related to tetanus toxoid immunization. Cardiovasc. Pathol. 2018, 37, 54–57. [Google Scholar] [CrossRef]
- Barton, M.; Finkelstein, Y.; Opavsky, M.A.; Ito, S.; Ho, T.; Ford-Jones, L.E.; Taylor, G.; Benson, L.; Gold, R. Eosinophilic myocarditis temporally associated with conjugate meningococcal C and hepatitis B vaccines in children. Pediatr. Infect. Dis. J. 2008, 27, 831–835. [Google Scholar] [CrossRef]
- Engler, R.J.; Nelson, M.R.; Collins, L.C., Jr.; Spooner, C.; Hemann, B.A.; Gibbs, B.T.; Atwood, J.E.; Howard, R.S.; Chang, A.S.; Cruser, D.L.; et al. A prospective study of the incidence of myocarditis/pericarditis and new onset cardiac symptoms following smallpox and influenza vaccination. PLoS ONE 2015, 10, e0118283. [Google Scholar] [CrossRef] [Green Version]
- Staff, T. Israel Said Probing Link between P3zer Shot and Heart Problem in Men under 30. 2021. Available online: https://www.timesofisrael.com/israel-said-probing-link-between-pfizer-shot-and-heart-problem-in-men-under-30/ (accessed on 17 May 2021).
- Prevention CDC COVID-19 VaST Work Group Report. Available online: https://www.cdc.gov/vaccines/acip/work-groups-vast/report-2021-05-17.html (accessed on 17 May 2021).
- Boehmer, T.K.; Kompaniyets, L.; Lavery, A.M.; Hsu, J.; Ko, J.Y.; Yusuf, H.; Romano, S.D.; Gundlapalli, A.V.; Oster, M.E.; Harris, A.M. Association Between COVID-19 and Myocarditis Using Hospital-Based Administrative Data—United States, March 2020-January 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1228–1232. [Google Scholar] [CrossRef] [PubMed]
- Mele, D.; Flamigni, F.; Rapezzi, C.; Ferrari, R. Myocarditis in COVID-19 patients: Current problems. Intern. Emerg. Med. 2021, 16, 1123–1129. [Google Scholar] [CrossRef]
- Ferreira, V.M.; Schulz-Menger, J.; Holmvang, G.; Kramer, C.M.; Carbone, I.; Sechtem, U.; Kindermann, I.; Gutberlet, M.; Cooper, L.T.; Liu, P.; et al. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations. J. Am. Coll. Cardiol. 2018, 72, 3158–3176. [Google Scholar] [CrossRef]
- Pan, J.A.; Lee, Y.J.; Salerno, M. Diagnostic Performance of Extracellular Volume, Native T1, and T2 Mapping Versus Lake Louise Criteria by Cardiac Magnetic Resonance for Detection of Acute Myocarditis: A Meta-Analysis. Circ. Cardiovasc. Imaging 2018, 11, e007598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luetkens, J.A.; Faron, A.; Isaak, A.; Dabir, D.; Kuetting, D.; Feisst, A.; Schmeel, F.; Sprinkart, A.M.; Thomas, D. Comparison of Original and 2018 Lake Louise Criteria for Diagnosis of Acute Myocarditis: Results of a Validation Cohort. Radiol. Cardiothorac. Imaging 2019, 1, e190010. [Google Scholar] [CrossRef]
- Friedrich, M.G.; Marcotte, F. Cardiac magnetic resonance assessment of myocarditis. Circ. Cardiovasc. Imaging 2013, 6, 833–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsiao, J.F.; Koshino, Y.; Bonnichsen, C.R.; Yu, Y.; Miller, F.A., Jr.; Pellikka, P.A.; Cooper, L.T., Jr.; Hector, R.; Villarraga, H.R. Speckle tracking echocardiography in acute myocarditis. Int. J. Cardiovasc. Imaging 2013, 29, 275–284. [Google Scholar] [CrossRef]
- Albert, E.; Aurigemma, G.; Saucedo, J.; Gerson, D.S. Myocarditis following COVID-19 vaccination. Radiol. Case Rep. 2021, 16, 2142–2145. [Google Scholar] [CrossRef] [PubMed]
- Rosner, C.M.; Genovese, L.; Tehrani, B.N.; Atkins, M.; Bakhshi, H.; Chaudhri, S.; Damluji, A.A.; de Lemos, J.A.; Desai, S.S.; Emaminia, A.; et al. Myocarditis Temporally Associated with COVID-19 Vaccination. Circulation 2021, 144, 502–505. [Google Scholar] [CrossRef] [PubMed]
- Keshavarz, P.; Yazdanpanah, F.; Azhdari, S.; Kavandi, H.; Nikeghbal, P.; Bazyar, A.; Rafiee, F.; Nejati, S.F.; Sadabad, F.E.; Rezaei, N. Coronavirus disease 2019 (COVID-19): A systematic review of 133 Children that presented with Kawasaki-like multisystem inflammatory syndrome. J. Med. Virol. 2021, 93, 5458–5473. [Google Scholar] [CrossRef] [PubMed]
- Jhaveri, R.; Adler-Shohet, F.C.; Blyth, C.C.; Chiotos, K.; Gerber, J.S.; Green, M.; Kociolek, L.; Martin-Blais, R.; Palazzi, D.; Shane, A.L.; et al. Weighing the Risks of Perimyocarditis with the Benefits of SARS-CoV-2 mRNA Vaccination in Adolescents. J. Pediatr. Infect. Dis. Soc. 2021, 10, 937–939. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, T.; Cattafi, A.; Carerj, M.L.; Booz, C.; Ascenti, G.; Cicero, G.; Blandino, A.; Mazziotti, S. Myocarditis After SARS-CoV-2 Vaccination: A Vaccine-Induced Reaction? Can. J. Cardiol. 2021, 37, 1665–1667. [Google Scholar] [CrossRef]
- Deb, A.; Abdelmalek, J.; Iwuji, K.; Nugent, K. Acute Myocardial Injury Following COVID-19 Vaccination: A Case Report and Review of Current Evidence from Vaccine Adverse Events Reporting System Database. J. Prim. Care Community Health 2021, 12, 21501327211029230. [Google Scholar] [CrossRef]
- Bautista García, J.; Peña Ortega, P.; Bonilla Fernández, J.A.; Cárdenes León, A.; Ramírez Burgos, L.; Caballero Dorta, E. Acute myocarditis after administration of the BNT162b2 vaccine against COVID. Rev. Esp. Cardiol. 2021, 74, 812–814. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.E.; Cavalcante, J.L.; Han, B.K.; Gössl, M. Possible Association Between COVID-19 Vaccine and Myocarditis: Clinical and CMR Findings. Cardiovasc. Imaging 2021, 14, 1856–1861. [Google Scholar] [CrossRef]
- Watkins, K.; Griffin, G.; Septaric, K.; Simon, E.L. Myocarditis after BNT162b2 vaccination in a healthy male. Am. J. Emerg. Med. 2021, 50, e1–e2. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Kaur, P.; Cedeno, L.; Brahimi, T.; Patel, P.; Virk, H.; Shamoon, F.; Bikkina, M. COVID-19 mRNA Vaccine and Myocarditis. Eur. J. Case Rep. Intern. Med. 2021, 8, 002681. [Google Scholar] [CrossRef] [PubMed]
- Muthukumar, A.; Narasimhan, M.; Li, Q.Z.; Mahimainathan, L.; Hitto, I.; Fuda, F.; Batra, K.; Jiang, X.; Zhu, C.; Schoggins, J.; et al. In-Depth Evaluation of a Case of Presumed Myocarditis after the Second Dose of COVID-19 mRNA Vaccine. Circulation 2021, 144, 487–498. [Google Scholar] [CrossRef] [PubMed]
- Minocha, P.K.; Better, D.; Singh, R.K.; Hoque, T. Recurrence of Acute Myocarditis Temporally Associated with Receipt of the mRNA Coronavirus Disease 2019 (COVID-19) Vaccine in a Male Adolescent. J. Pediatr. 2021, 238, 321–323. [Google Scholar] [CrossRef] [PubMed]
- Dickey, J.B.; Albert, E.; Badr, M.; Laraja, K.M.; Sena, L.M.; Gerson, D.S.; Saucedo, J.E.; Qureshi, W.; Aurigemma, G.P. A Series of Patients with Myocarditis following SARS-CoV-2 Vaccination with mRNA-1279 and Bnt162b. Cardiovasc. Imaging 2021, 14, 1862–1863. [Google Scholar] [CrossRef]
- Kim, H.W.; Jenista, E.R.; Wendell, D.C.; Azevedo, C.F.; Campbell, M.J.; Darty, S.N.; Parker, M.A.; Kim, R.J. Patients with Acute Myocarditis following mRNA COVID-19 Vaccination. JAMA Cardiol. 2021, 6, 1196–1201. [Google Scholar] [CrossRef] [PubMed]
- Larson, K.F.; Ammirati, E.; Adler, E.D.; Cooper, L.T.; Hong, K.N.; Saponara, G.; Couri, D.; Cereda, A.; Procopio, A.; Cavalotti, C.; et al. Myocarditis After BNT162b2 and mRNA-1273 Vaccination. Circulation 2021, 144, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Vidula, M.K.; Ambrose, M.; Glassberg, H.; Chokshi, N.; Chen, T.; Ferrari, V.A.; Han, Y. Myocarditis and Other Cardiovascular Complications of the mRNA-Based COVID-19 Vaccines. Cureus 2021, 13, e15576. [Google Scholar] [CrossRef] [PubMed]
- Marshall, M.; Ferguson, I.D.; Lewis, P.; Jaggi, P.; Gagliardo, C.; Collins, J.S.; Shaughnessy, R.; Caron, R.; Fuss, C.; Corbin, K.J.E.; et al. Symptomatic Acute Myocarditis in 7 Adolescents after Pfizer-BioNTech COVID-19 Vaccination. Pediatrics 2021, 148. [Google Scholar] [CrossRef]
- Montgomery, J.; Ryan, M.; Engler, R.; Hoffman, D.; McClenathan, B.; Collins, L.; Loran, D.; Hrncir, D.; Herring, K.; Platzer, M.; et al. Myocarditis Following Immunization with mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol. 2021, 6, 1202–1206. [Google Scholar] [CrossRef] [PubMed]
- Abu Mouch, S.; Roguin, A.; Hellou, E.; Ishai, A.; Shoshan, U.; Mahamidm, L.; Zoabi, M.; Aisman, M.; Goldschmid, N.; Berar Yanay, N. Myocarditis following COVID-19 mRNA vaccination. Vaccine 2021, 39, 3790–3793. [Google Scholar] [CrossRef]
- Nevet, A. Acute myocarditis associated with anti-COVID-19 vaccination. Clin. Exp. Vaccine Res. 2021, 10, 196–197. [Google Scholar] [CrossRef]
- Schauer, J.; Buddhe, S.; Colyer, J.; Sagiv, E.; Law, Y.; Mallenahalli Chikkabyrappa, S.; Portman, M.A. Myopericarditis After the Pfizer Messenger Ribonucleic Acid Coronavirus Disease Vaccine in Adolescents. J. Pediatr. 2021, 238, 317–320. [Google Scholar] [CrossRef]
- Park, J.; Brekke, D.R.; Bratincsak, A. Self-limited myocarditis presenting with chest pain and ST segment elevation in adolescents after vaccination with the BNT162b2 mRNA vaccine. Cardiol. Young 2022, 32, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Cereda, A.; Conca, C.; Barbieri, L.; Ferrante, G.; Tumminello, G.; Lucreziotti, S.; Guazzi, M.; Mafrici, A. Acute myocarditis after the second dose of SARS-CoV-2 vaccine: Serendipity or atypical causal relationship? Anatol. J. Cardiol. 2021, 25, 522–523. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.B.; Choi, J.-i.; Hosseini, F.; Roberts, J.; Ramanathan, K.; Ong, K. Acute Myocarditis following mRNA-1273 SARS-CoV-2 Vaccination. CJC Open. 2021, 3, 1410–1412. [Google Scholar] [CrossRef] [PubMed]
- Starekova, J.; Bluemke, D.A.; Bradham, W.S.; Grist, T.M.; Schiebler, M.L.; Reeder, S.B. Myocarditis Associated with mRNA COVID-19 Vaccination. Radiology 2021, 301, e409–e411. [Google Scholar] [CrossRef]
- Di Tano, G.M.L.; Calvaruso, E.V.; Danzi, G.B. Recurrent Myocarditis after the First Dose of SARS-CoV-2 mRNA- 1273 Vaccine. Ann. Clin. Case Rep. 2021, 6, 2018. [Google Scholar]
- Khogali, F.; Abdelrahman, R. Unusual Presentation of Acute Perimyocarditis following SARS-COV-2 mRNA-1237 Moderna Vaccination. Cureus 2021, 13, e16590. [Google Scholar] [CrossRef] [PubMed]
- Tano, E.; San Martin, S.; Girgis, S.; Martinez-Fernandez, Y.; Sanchez Vegas, C. Perimyocarditis in Adolescents after Pfizer-BioNTech COVID-19 Vaccine. J. Pediatr. Infect. Dis. Soc. 2021, 10, 962–966. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.K.; Lavine, K.J.; Lin, C.Y. Myocarditis after Covid-19 mRNA Vaccination. N. Engl. J. Med. 2021, 385, 1332–1334. [Google Scholar] [CrossRef]
- Levin, D.; Shimon, G.; Fadlon-Derai, M.; Gershovitz, L.; Shovali, A.; Sebbag, A.; Bader, S.; Fink, N.; Gordon, B. Myocarditis following COVID-19 vaccination—A case series. Vaccine 2021, 39, 6195–6200. [Google Scholar] [CrossRef]
- Shumkova, M.; Vassilev, D.; Karamfiloff, K.; Ivanova, R.; Stoyanova, K.; Yaneva-Sirakova, T.; Gil, R.J. Acute myocarditis associated with the Pfizer/BioNTech vaccine. Kardiol. Pol. 2021, 79, 1282–1283. [Google Scholar] [CrossRef] [PubMed]
- Cimaglia, P.; Tolomeo, P.; Rapezzi, C. Acute myocarditis after SARS-CoV-2 vaccination in a 24-year-old man. Rev. Port. Cardiol. 2022, 41, 71–72. [Google Scholar] [CrossRef]
- Dionne, A.; Sperotto, F.; Chamberlain, S.; Baker, A.L.; Powell, A.J.; Prakash, A.; Castellanos, D.A.; Saleeb, S.F.; de Ferranti, S.D.; Newburger, J.W.; et al. Association of Myocarditis with BNT162b2 Messenger RNA COVID-19 Vaccine in a Case Series of Children. JAMA Cardiol. 2021, 6, 1446–1450. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, P.; Klingel, K.; Ohlmann-Knafo, S.; Hüttinger, S.; Sood, N.; Pickuth, D.; Kindermann, M. Biopsy-proven lymphocytic myocarditis following first mRNA COVID-19 vaccination in a 40-year-old male: Case report. Clin. Res. Cardiol. 2021, 110, 1855–1859. [Google Scholar] [CrossRef] [PubMed]
- Gautam, N.; Saluja, P.; Fudim, M.; Jambhekar, K.; Pandey, T.; Al’Aref, S. A Late Presentation of COVID-19 Vaccine-Induced Myocarditis. Cureus 2021, 13, e17890. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.C.; Kim, H.; Lee, H.J.; Kim, J.Y.; Kim, J.Y. Cardiac Imaging of Acute Myocarditis following COVID-19 mRNA Vaccination. J. Korean Med. Sci. 2021, 36, e229. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.S.; Steele, J.M.; Fonseca, B.; Huang, S.; Shah, S.; Maskatia, S.A.; Buddhe, S.; Misra, N.; Ramachandran, P.; Gaur, L.; et al. COVID-19 Vaccination-Associated Myocarditis in Adolescents. Pediatrics 2021, 148. [Google Scholar] [CrossRef] [PubMed]
- King, W.W.; Petersen, M.R.; Matar, R.M.; Budweg, J.B.; Cuervo Pardo, L.; Petersen, J.W. Myocarditis following mRNA vaccination against SARS-CoV-2, a case series. Am. Heart J. Plus Cardiol. Res. Pract. 2021, 8, 100042. [Google Scholar] [CrossRef] [PubMed]
- Matta, A.; Kallamadi, R.; Matta, D.; Bande, D. Post-mRNA COVID-19 Vaccination Myocarditis. Eur. J. Case Rep. Intern. Med. 2021, 8, 002769. [Google Scholar] [CrossRef] [PubMed]
- Patel, Y.R.; Louis, D.W.; Atalay, M.; Agarwal, S.; Shah, N.R. Cardiovascular magnetic resonance findings in young adult patients with acute myocarditis following mRNA COVID-19 vaccination: A case series. J. Cardiovasc. Magn. Reson. 2021, 23, 101. [Google Scholar] [CrossRef] [PubMed]
- Patrignani, A.; Schicchi, N.; Calcagnoli, F.; Falchetti, E.; Ciampani, N.; Argalia, G.; Mariani, A. Acute myocarditis following Comirnaty vaccination in a healthy man with previous SARS-CoV-2 infection. Radiol. Case Rep. 2021, 16, 3321–3325. [Google Scholar] [CrossRef] [PubMed]
- Sulemankhil, I.; Abdelrahman, M.; Negi, S.I. Temporal association between the COVID-19 Ad26.COV2.S vaccine and acute myocarditis: A case report and literature review. Cardiovasc. Revasc. Med. 2021, 38, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Tailor, P.D.; Feighery, A.M.; El-Sabawi, B.; Prasad, A. Case report: Acute myocarditis following the second dose of mRNA-1273 SARS-CoV-2 vaccine. Eur. Heart J. Case Rep. 2021, 5, ytab319. [Google Scholar] [CrossRef] [PubMed]
- Ujueta, F.; Azimi, R.; Lozier, M.R.; Poppiti, R.; Ciment, A. Lymphohistocytic myocarditis after Ad26.COV2.S viral vector COVID-19 vaccination. Int. J. Cardiol. Heart Vasc. 2021, 36, 100869. [Google Scholar] [CrossRef] [PubMed]
- Hung, Y.P.; Sun, K.S. A case of myopericarditis with pleuritis following AstraZeneca Covid-19 vaccination. QJM Int. J. Med. 2022, 114, 879–881. [Google Scholar] [CrossRef] [PubMed]
- Kaneta, K.; Yokoi, K.; Jojima, K.; Kotooka, N.; Node, K. Young Male with Myocarditis following mRNA-1273 Vaccination Against Coronavirus Disease-2019 (COVID-19). Circ. J. 2022, 86, 721. [Google Scholar] [CrossRef] [PubMed]
- Kaul, R.; Sreenivasan, J.; Goel, A.; Malik, A.; Bandyopadhyay, D.; Jin, C.; Sharma, M.; Levine, A.; Pan, S.; Fuisz, A.; et al. Myocarditis following COVID-19 vaccination. Int. J. Cardiol. Heart Vasc. 2021, 36, 100872. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Choi, J.H.; Jang, J.Y.; So, O.; Cho, E.; Choi, H.; Hong, K.S.; Park, K.T. A Case Report for Myopericarditis after BNT162b2 COVID-19 mRNA Vaccination in a Korean Young Male. J. Korean Med. Sci. 2021, 36, e277. [Google Scholar] [CrossRef] [PubMed]
- Koizumi, T.; Awaya, T.; Yoshioka, K.; Kitano, S.; Hayama, H.; Amemiya, K.; Enomoto, Y.; Yazaki, Y.; Moroi, M.; Nakamura, M. Myocarditis after COVID-19 mRNA vaccines. QJM Int. J. Med. 2021, 114, 741–743. [Google Scholar] [CrossRef] [PubMed]
- Maki, H.; Aikawa, T.; Ibe, T.; Oyama-Manabe, N.; Fujita, H. Biventricular systolic dysfunction in acute myocarditis after SARS-CoV-2 mRNA-1273 vaccination. Eur. Heart J. Cardiovasc. Imaging 2022, 23, e87. [Google Scholar] [CrossRef]
- Miqdad, M.A.; Nasser, H.; Alshehri, A.; Mourad, A.R. Acute Myocarditis following the Administration of the Second BNT162b2 COVID-19 Vaccine Dose. Cureus 2021, 13, e18880. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.D.; Mall, G.; Westphal, J.G.; Weingärtner, O.; Möbius-Winkler, S.; Schulze, P.C. Acute myocarditis after COVID-19 vaccination with mRNA-1273 in a patient with former SARS-CoV-2 infection. Esc. Heart Fail. 2021, 8, 4710–4714. [Google Scholar] [CrossRef] [PubMed]
- Onderko, L.; Starobin, B.; Riviere, A.E.; Hohl, P.K.; Phillips, C.T.; Morgan, R.B.; Welsh, A.; Francis, S.A.; Afari, M.E. Myocarditis in the Setting of Recent COVID-19 Vaccination. Case Rep. Cardiol. 2021, 2021, 6806500. [Google Scholar] [CrossRef] [PubMed]
- Pareek, M.; Asnes, J.; Baldassarre, L.; Casale, L.; Desai, N.; Elder, R.; Faherty, E.; Ferguson, I.; Fishman, R.; Ghazizadeh, Z.; et al. Myopericarditis after Covid-19 Vaccination—A Case Series. SSRN 2021. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3874571 (accessed on 6 May 2022).
- Perez, Y.; Levy, E.R.; Joshi, A.Y.; Virk, A.; Rodriguez-Porcel, M.; Johnson, M.; Roellinger, D.; Vanichkachorn, G.; Huskins, W.C.; Swift, M.D. Myocarditis following COVID-19 mRNA Vaccine: A Case Series and Incidence Rate Determination. Clin. Infect. Dis. 2021. [Google Scholar] [CrossRef]
- Sakaguchi, S.; Fujimoto, N.; Ichikawa, K.; Izumi, D.; Katsuta, K.; Takafuji, M.; Imanaka-Yoshida, K.; Dohi, K. Myopericarditis after COVID-19 mRNA Vaccination. Circ. J. 2022, 86, 472. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, P.; Demoulin, R.; Poyet, R.; Capilla, E.; Rohel, G.; Pons, F.; Jégo, C.; Sidibe, S.; Druelle, A.; Brocq, F.X.; et al. Acute Myocarditis after COVID-19 vaccination: A case report. Rev. Med. Interne 2021, 42, 797–800. [Google Scholar] [CrossRef] [PubMed]
- Sivakumaran, P.; Sunny, J.; Tsagkridi, A.; Khanji, M.Y. Myopericarditis following SARS-CoV-2 mRNA vaccine: The role of cardiac biomarkers and multimodality imaging. Eur. Heart J. Cardiovasc. Imaging 2022, 23, e134. [Google Scholar] [CrossRef] [PubMed]
- Viskin, D.; Topilsky, Y.; Aviram, G.; Mann, T.; Sadon, S.; Hadad, Y.; Flint, N.; Shmilovich, H.; Banai, S.; Havakuk, O. Myocarditis Associated with COVID-19 Vaccination: Echocardiography, Cardiac Tomography, and Magnetic Resonance Imaging Findings. Circ. Cardiovasc. Imaging 2021, 14, e013236. [Google Scholar] [CrossRef] [PubMed]
- Vollmann, D.; Eiffert, H.; Schuster, A. Acute Perimyocarditis following First Dose of mRNA Vaccine against COVID. Dtsch. Ärzteblatt Int. 2021, 118, 546. [Google Scholar] [CrossRef]
- Wilson, H.; Norris, M.D.; Frosch, O.; Agarwal, P.P. Late Gadolinium Enhancement after COVID-19 Vaccination. Radiol. Cardiothorac. Imaging 2021, 3, e210199. [Google Scholar] [CrossRef]
- Hasnie, A.A.; Hasnie, U.A.; Patel, N.; Aziz, M.U.; Xie, M.; Lloyd, S.G.; Prabhu, S.D. Perimyocarditis following first dose of the mRNA-1273 SARS-CoV-2 (Moderna) vaccine in a healthy young male: A case report. BMC Cardiovasc. Disord. 2021, 21, 375. [Google Scholar] [CrossRef] [PubMed]
- Habedank, D.; Lagast, A.; Novoa-Usme, M.; Atmowihardjo, I. A case of myocarditis in a 60-year-old man 48 h after mRNA vaccination against SARS. Covclin. Res. Cardiol. 2022, 111, 230–232. [Google Scholar] [CrossRef]
- Angel Goenawan, F.K.; Kenneth, S.; Seema, D. Recurrent mRNA (BNT162b2) Covid-19 Vaccine-Associated Pericarditis in an Elderly Man with Multiple Comorbidities. Am. J. Med. Case Rep. 2021, 9, 709–713. [Google Scholar] [CrossRef]
- Fleming-Nouri, A.; Haimovich, A.D.; Yang, D.; Schulz, W.L.; Coppi, A.; Taylor, R.A. Myopericarditis in young adults presenting to the emergency department after receiving a second COVID-19 mRNA vaccine. Acad. Emerg. Med. 2021, 28, 802. [Google Scholar] [CrossRef] [PubMed]
- Das, B.B.; Kohli, U.; Ramachandran, P.; Nguyen, H.H.; Greil, G.; Hussain, T.; Tandon, A.; Kane, C.; Avula, S.; Duru, C.; et al. Myopericarditis after messenger RNA Coronavirus Disease 2019 Vaccination in Adolescents 12 to 18 Years of Age. J. Pediatr. 2021, 238, 26–32.e1. [Google Scholar] [CrossRef]
- Chen, D.H.; Arefin, A.R.; Joshi, A.; Khanji, M.Y. Myopericarditis in a teenager following first mRNA COVID vaccine dose: The role of multi-parametric cardiovascular magnetic resonance. Eur. Heart J. Case Rep. 2021, 5, ytab371. [Google Scholar] [CrossRef] [PubMed]
- Chelala, L.; Jeudy, J.; Hossain, R.; Rosenthal, G.; Pietris, N.; White, C.S. Cardiac MRI Findings of Myocarditis after COVID-19 mRNA Vaccination in Adolescents. Am. J. Roentgenol. 2022, 218, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Boursier, C.; Chevalier, E.; Filippetti, L.; Imbert, L.; Roch, V.; Huttin, O.; Claudin, M.; Marie, P.Y. 68Ga-DOTATOC digital-PET imaging of inflammatory cell infiltrates in myocarditis following COVID-19 vaccination. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 1433–1434. [Google Scholar] [CrossRef]
- Badshah, M.; Shriver, J.; Rynders, B.; Sjovold, A.; Shaukat, M.H.S.; Rajpurohit, N. MODERNA mRNA-1273 vaccine-associated myopericarditis in a patient with a subclinical autoimmune predisposition. J. Cardio. Cases 2021, 24, 227–229. [Google Scholar] [CrossRef]
- Azir, M.; Inman, B.; Webb, J.; Tannenbaum, L. STEMI Mimic: Focal Myocarditis in an Adolescent Patient after mRNA COVID-19 Vaccine. J. Emerg. Med. 2021, 61, e129–e132. [Google Scholar] [CrossRef]
- Ambati, S.; Colon, M.; Mihic, M.; Sanchez, J.; Bakar, A. Acute Myopericarditis after COVID-19 Vaccine in Teenagers. Case Rep. Cardiol. 2021, 2021, 8268755. [Google Scholar] [CrossRef]
- Sokolska, J.M.; Kurcz, J.; Kosmala, W. Every rose has its thorns—Acute myocarditis following COVID-19 vaccination. Kardio. Pol. 2021, 79, 1153–1154. [Google Scholar] [CrossRef] [PubMed]
- Lazaros, G.; Anastassopoulou, C.; Hatziantoniou, S.; Kalos, T.; Soulaidopoulos, S.; Lazarou, E.; Vlachopoulos, C.; Vassilopoulos, D.; Tsakris, A.; Tsioufis, C. A case series of acute pericarditis following COVID-19 vaccination in the context of recent reports from Europe and the United States. Vaccine 2021, 39, 6585–6590. [Google Scholar] [CrossRef] [PubMed]
- Facetti, S.G.M.; Vecchi, A.L. Acute myocarditis in a young adult two days after Pfizer vaccine. G. Ital. Cardiol. 2021, 22, 891–893. [Google Scholar] [CrossRef]
- Meyer-Szary, J.; Bazgier, M.; Lubocka, P.; Dorniak, K.; Sabiniewicz, R. Cardiac magnetic resonance characteristics of acute myocarditis occurring after mRNA-based COVID-19 vaccines immunization. Cardiolj 2022, 29, 160–162. [Google Scholar] [CrossRef]
- Aikawa, T.; Ogino, J.; Kita, Y.; Funayama, N. Myocardial microthrombi after COVID-19 mRNA vaccination. Eur. Heartj. 2021, 42, 4501. [Google Scholar] [CrossRef] [PubMed]
- Bricoli, S.; Cacciola, G.; Barocelli, F.; Guerra, C.; Zardini, M. 553 Myocarditis after COVID-19 vaccination—A case series. Eur. Heart J. Suppl. 2021, 23. [Google Scholar] [CrossRef]
- Chachar, T.S.; Yousuf, N.; Sulaibikh, L.; Abdulqader, F.; Alqahtani, M. First Report of Acute Myocarditis Post-Pfizer-BioNTech COVID-19 Vaccination in the Kingdom of Bahrain. Cureus 2021, 13, e20313. [Google Scholar] [CrossRef] [PubMed]
- Eggebrecht, H.; Breitbart, P.; Koch, A.; Nowak, B.; Walther, C.; Voigtländer, T.; Liebetrau, C.; Metha, R.H.; Schmermund, A. Trends in ambulatory cardiology consultations for suspected myocarditis after COVID-19 vaccination. Clin. Res. Cardiol. 2022, 111, 237–239. [Google Scholar] [CrossRef]
- Istampoulouoglou, I.; Dimitriou, G.; Späni, S.; Christ, A.; Zimmermanns, B.; Koechlin, S.; Stoeckmann, O.; Winterhalder, C.; Marono, D.; Toma, V.; et al. Myocarditis and pericarditis in association with COVID-19 mRNA-vaccination: Cases from a regional pharmacovigilance centre. Glob. Cardiol. Sci. Pract. 2021, 2021, e202118. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.; Kim, M.C.; Kim, K.H.; Jeong, I.S.; Cho, Y.S.; Choi, Y.D.; Lee, J.E. Case Report: Acute Fulminant Myocarditis and Cardiogenic Shock after Messenger RNA Coronavirus Disease 2019 Vaccination Requiring Extracorporeal Cardiopulmonary Resuscitation. Front. Cardiovasc. Med. 2021, 8. [Google Scholar] [CrossRef]
- McCullough, J.; McCullough, J.P.; Korlipara, G.; Kaell, A. Myocarditis Post Moderna Vaccination: Review of Criteria for Diagnosis. Cureus 2021, 13, e19633. [Google Scholar] [CrossRef] [PubMed]
- Murakami, Y.; Shinohara, M.; Oka, Y.; Wada, R.; Noike, R.; Ohara, H.; Fujino, T.; Ikeda, T. Myocarditis following a COVID-19 Messenger RNA Vaccination: A Japanese Case Series. Intern. Med. 2022, 61, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Nagasaka, T.; Koitabashi, N.; Ishibashi, Y.; Aihara, K.; Takama, N.; Ohyama, Y.; Yokoyama, T.; Kaneko, Y. Acute Myocarditis Associated with COVID-19 Vaccination: A Case Report. J. Cardiol. Cases 2021. [Google Scholar] [CrossRef] [PubMed]
- Parmar, K.; Mekraksakit, P.; Del Rio-Pertuz, G.; Sethi, P.; Motes, A.; Hughes, M.; Wischmeyer, J.; Carbajal, L.; Sosa, E.A. Myocarditis following COVID-19 mRNA vaccination. Bayl. Univ. Med. Cent. Proc. 2022, 35, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Chakrabarti, S.S.; Gambhir, I.S.; Verma, A.; Kumar, I.; Ghosh, S.; Tiwari, A.; Chandan, G.; Chakrabarti, S.; Kaur, U. Acute Cardiac Events after ChAdOx1 nCoV-19 Corona Virus Vaccine: Report of Three Cases. Am. J. Ther. 2022. [Google Scholar] [CrossRef] [PubMed]
- Takeda, M.; Ishio, N.; Shoji, T.; Mori, N.; Matsumoto, M.; Shikama, N. Eosinophilic Myocarditis following Coronavirus Disease 2019 (COVID-19) Vaccination. Circ. J. 2021. [Google Scholar] [CrossRef] [PubMed]
- Tinoco, M.; Leite, S.; Faria, B.; Cardoso, S.; Von Hafe, P.; Dias, G.; Cardoso, F.; Pereira, T.; Machado, I.; Lourenço, A. Perimyocarditis following COVID-19 Vaccination. Clin. Med. Insights Cardiol. 2021, 15, 11795468211056634. [Google Scholar] [CrossRef] [PubMed]
- Ashutosh, T.; Sankha Shubhra, C.; Prasan Kumar, P.; Gaurav, K.; Upinder, K. Hyper-eosinophilic syndrome with myocarditis after inactivated SARS-CoV-2 vaccination: A case study. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Di Dedda, E.A.; Barison, A.; Aquaro, G.D.; Ismail, T.F.; Hua, A.; Mantini, C.; Ricci, F.; Pontone, G.; Volpe, A.; Secchi, F.; et al. Cardiac magnetic resonance imaging of myocarditis and pericarditis following COVID-19 vaccination: A multicenter collection of 27 cases. Eur. Radiol. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fronza, M.; Thavendiranathan, P.; Chan, V.; Karur, G.R.; Udell, J.A.; Wald, R.M.; Hong, R.; Hanneman, K. Myocardial Injury Pattern at MRI in COVID-19 Vaccine-associated Myocarditis. Radiology 2022, 212559. [Google Scholar] [CrossRef] [PubMed]
- Bews, H.; Bryson, A.; Bortoluzzi, T.; Tam, J.W.; Jassal, D.S. COVID-19 vaccination induced myopericarditis: An imager’s perspective. CJC Open 2022. [Google Scholar] [CrossRef] [PubMed]
- Manfredi, R.; Bianco, F.; Bucciarelli, V.; Ciliberti, G.; Guerra, F.; Schicchi, N.; Tavio, M.; Berton, E.; Surace, F.C.; Colaneri, M.; et al. Clinical Profiles and CMR Findings of Young Adults and Pediatrics with Acute Myocarditis Following mRNA COVID-19 Vaccination: A Case Series. Vaccines 2022, 10, 169. [Google Scholar] [CrossRef] [PubMed]
- Sharff, K.A.; Dancoes, D.M.; Longueil, J.L.; Lewis, P.F.; Johnson, E.S. Myopericarditis After COVID-19 Booster Dose Vaccination. Am. J. Cardiol. 2022, 172, 165–166. [Google Scholar] [CrossRef] [PubMed]
- Nunn, S.; Kersten, J.; Tadic, M.; Wolf, A.; Gonska, B.; Hüll, E.; Dietenberger, H.; Rottbauer, W.; Buckert, D. Case Report: Myocarditis After COVID-19 Vaccination—Case Series and Literature Review. Front. Med. 2022, 9, 836620. [Google Scholar] [CrossRef] [PubMed]
- Bengel, C.P.; Kacapor, R. A report of two cases of myocarditis following mRNA coronavirus disease 2019 vaccination. Eur. Heart J. Case Rep. 2022, 6, ytac004. [Google Scholar] [CrossRef] [PubMed]
- Ohnishi, M.; Tanaka, Y.; Nishida, S.; Sugimoto, T. Case report of acute myocarditis after administration of coronavirus disease 2019 vaccine in Japan. Eur. Heart J. Case Rep. 2022, 6, ytab534. [Google Scholar] [CrossRef] [PubMed]
- Owuor, H.; Gikonyo, A.; Ponoth, P.; Gikonyo, D. Covid Vaccine Induced Myocarditis: A Bolt from the Blue: A Case Report. J. Cardiovasc. Med. Surg. 2022, 7, 51–55. [Google Scholar] [CrossRef]
- Sano, M.; Murai, R.; Kim, K.; Furukawa, Y. Cardiac magnetic resonance findings in acute myocarditis after mRNA COVID-19 vaccination. J. Cardiol. Cases 2022. [Google Scholar] [CrossRef]
- Wong, J.; Sharma, S.; Yao, J.V.; Aggarwal, A.; Grigg, L. COVID-19 mRNA vaccine (Comirnaty)-induced myocarditis. Med. J. Aust. 2022, 216, 122–123. [Google Scholar] [CrossRef]
- Wu, B.; Mittal, N.; Adler, E.D.; Hong, K.N. Acute myocarditis after receiving first dose of BNT162b2 mRNA vaccine. J. Cardiol. Cases 2022. [Google Scholar] [CrossRef] [PubMed]
- Yen, K.C.; Ho, C.T.; Chin, S.C.; Su, H.C.; Lee, K.T.; Chu, P.H. Self-Limited Myocarditis after the First Dose of Coronavirus Disease 2019 Messenger RNA-1273 Vaccine in a Healthy Male. Acta Cardiol. Sin. 2022, 38, 210–213. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, A.; Rezaiye, M.; Goharrizi, M.A.S.B. Acute Myocarditis following the Third Dose of SARS-CoV-2 Vaccine; A Case Report. Res. Sq. 2022. [Google Scholar] [CrossRef]
- Lee, C.H.; Kong, E.J. FDG PET/MRI of Acute Myocarditis after mRNA COVID-19 Vaccination. Clin. Nucl. Med. 2022. [Google Scholar] [CrossRef] [PubMed]
- Kyaw, H.; Shajahan, S.; Gulati, A.; Synn, S.; Khurana, S.; Nazar, N.; Shrestha, S.; Kerstein, J. COVID-19 mRNA Vaccine-Associated Myocarditis. Cureus 2022, 14, e21009. [Google Scholar] [CrossRef] [PubMed]
- Kounis, N.G.; Koniari, I.; Mplani, V.; Plotas, P.; Velissaris, D. Hypersensitivity myocarditis and the pathogenetic conundrum of COVID 19 Vaccine Related Myocarditis. Cardiology 2022. [Google Scholar] [CrossRef] [PubMed]
- Van Kerkhove, O.; Renders, F.; Leys, M. A case of myocarditis following ChAdOx1 nCov-19 vaccination. Acta Cardiol. 2022, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, T.; Yahagi, K.; Sekiguchi, M.; Ishizawa, T.; Nonaka, H.; Setoguchi, N.; Watanabe, Y.; Nakase, M.; Horiuchi, Y.; Asami, M.; et al. Acute Myocarditis in a Patient Following mRNA-1273 SARS-CoV-2 Vaccination. Intern. Med. 2022. [Google Scholar] [CrossRef]
- Gill, J.; Mallari, A.J.P.; Zahra, F. Transient Myopericarditis following Vaccination for COVID. J. Med. Cases 2022, 13, 80–84. [Google Scholar] [CrossRef]
- Agdamag, A.C.C.; Gonzalez, D.; Carlson, K.; Konety, S.; McDonald, W.C.; Martin, C.M. Fulminant myocarditis following coronavirus disease 2019 vaccination: A case report. Eur. Heart J.—Case Rep. 2022, 6, ytac007. [Google Scholar] [CrossRef]
- Fosch, X.; Serra, J.; Torres, P.L.; Preda, L.; González, R.; Mojer, F. Acute myocarditis after a third dose of the BNT162b2 COVID-19 vaccine. Rev. Esp. De Cardiol. 2022. [Google Scholar] [CrossRef]
| Characteristics | Number (%) |
|---|---|
| Gender | |
| male | 462 (86.8) |
| female | 70 (13.2) |
| Age (range, y/o) | 12–80 |
| Vaccine type | |
| Pfizer-BioNTech | 367 (69) |
| Moderna | 137 (25.8) |
| Janssen/Johnson & Johnson | 6 (1.1) |
| AstraZeneca | 12 (2.3) |
| COVAXIN | 1 (0.1) |
| unknown | 9 (1.7) |
| Vaccine status | |
| first dosage | 62 (11.6) |
| second dosage | 333 (62.6) |
| booster dosage | 7 (1.4) |
| unknown | 130 (24.4) |
| Patients’ presentation | |
| chest pain | 429 (80.6) |
| fever/chills | 245 (46) |
| myalgia | 132 (24.8) |
| headache | 87 (16.3) |
| shortness of breath | 161 (30.2) |
| fatigue | 71 (13.3) |
| nausea/vomiting | 65 (12.2) |
| Comorbidities | |
| hypertension | 34 (6.4) |
| coronary artery disease | 10 (1.9) |
| autoimmune disease | 17 (3.2) |
| myocarditis history | 7(1.3) |
| others * | 45 (8.4) |
| Outcome | |
| discharged | 500 (94) |
| readmitted | 1 (0.1) |
| expired | 3 (0.6) |
| unknown | 28 (5.3) |
| Vaccine Type | Location of Enhancement (Based on Cardiac MRI Reported) | |
|---|---|---|
| Epicardial/Subepicardial | Pericardial | |
| Pfizer-BioNTech | 232 | 20 |
| Moderna | 70 | 9 |
| Janssen/Johnson & Johnson | 2 | 0 |
| AstraZeneca | 8 | 3 |
| Unknown type | 6 | 0 |
| Total | 318 | 32 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keshavarz, P.; Yazdanpanah, F.; Emad, M.; Hajati, A.; Nejati, S.F.; Ebrahimian Sadabad, F.; Azrumelashvili, T.; Mizandari, M.; Raman, S.S. Myocarditis Following COVID-19 Vaccination: Cardiac Imaging Findings in 118 Studies. Tomography 2022, 8, 1959-1973. https://doi.org/10.3390/tomography8040164
Keshavarz P, Yazdanpanah F, Emad M, Hajati A, Nejati SF, Ebrahimian Sadabad F, Azrumelashvili T, Mizandari M, Raman SS. Myocarditis Following COVID-19 Vaccination: Cardiac Imaging Findings in 118 Studies. Tomography. 2022; 8(4):1959-1973. https://doi.org/10.3390/tomography8040164
Chicago/Turabian StyleKeshavarz, Pedram, Fereshteh Yazdanpanah, Maryam Emad, Azadeh Hajati, Seyed Faraz Nejati, Faranak Ebrahimian Sadabad, Tamta Azrumelashvili, Malkhaz Mizandari, and Steven S. Raman. 2022. "Myocarditis Following COVID-19 Vaccination: Cardiac Imaging Findings in 118 Studies" Tomography 8, no. 4: 1959-1973. https://doi.org/10.3390/tomography8040164
APA StyleKeshavarz, P., Yazdanpanah, F., Emad, M., Hajati, A., Nejati, S. F., Ebrahimian Sadabad, F., Azrumelashvili, T., Mizandari, M., & Raman, S. S. (2022). Myocarditis Following COVID-19 Vaccination: Cardiac Imaging Findings in 118 Studies. Tomography, 8(4), 1959-1973. https://doi.org/10.3390/tomography8040164







