The Diagnostic Performance of Multi-Detector Computed Tomography (MDCT) in Depiction of Acute Spondylodiscitis in an Emergency Department
Abstract
:1. Introduction
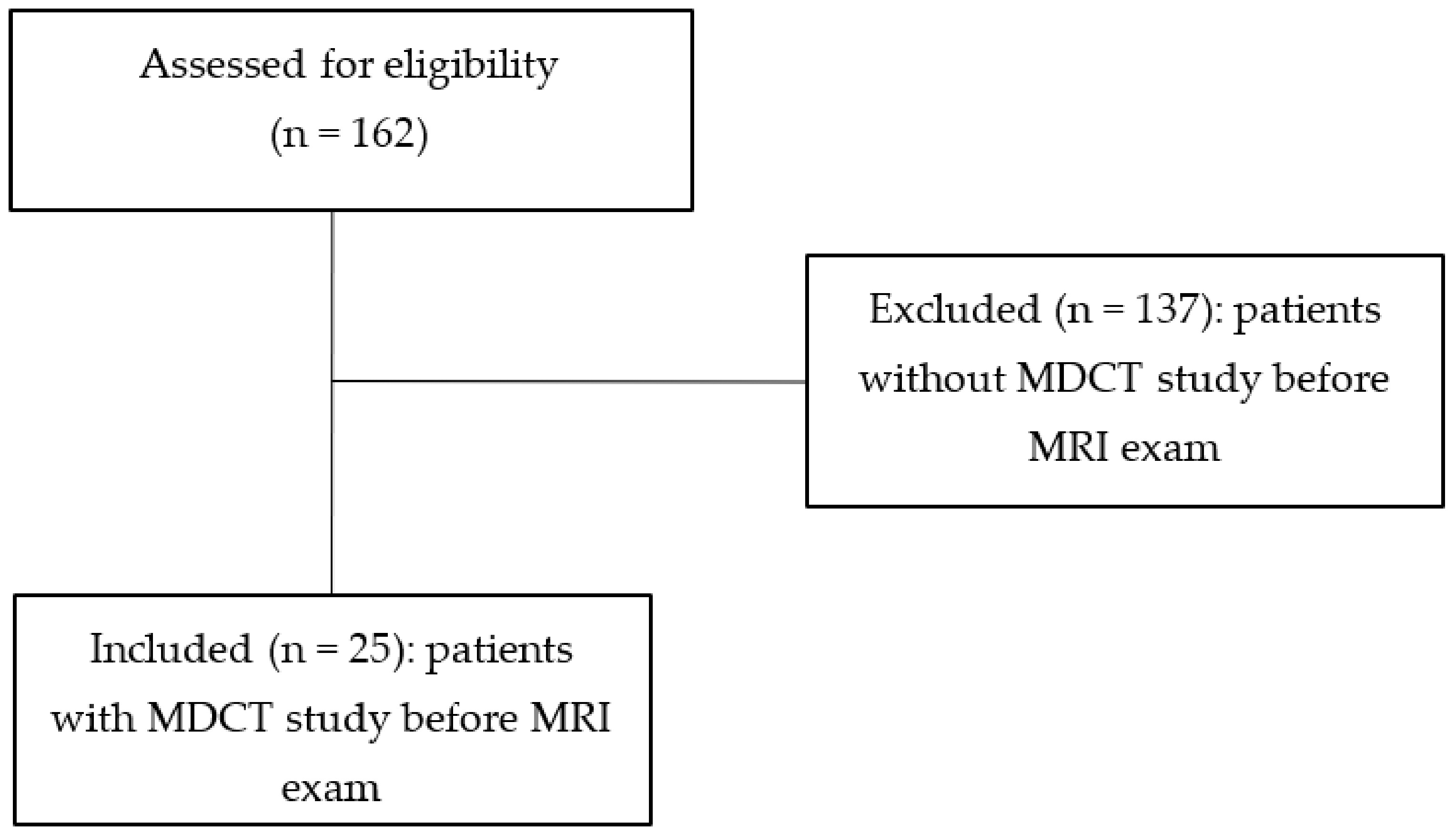
2. Materials and Methods
2.1. Patients
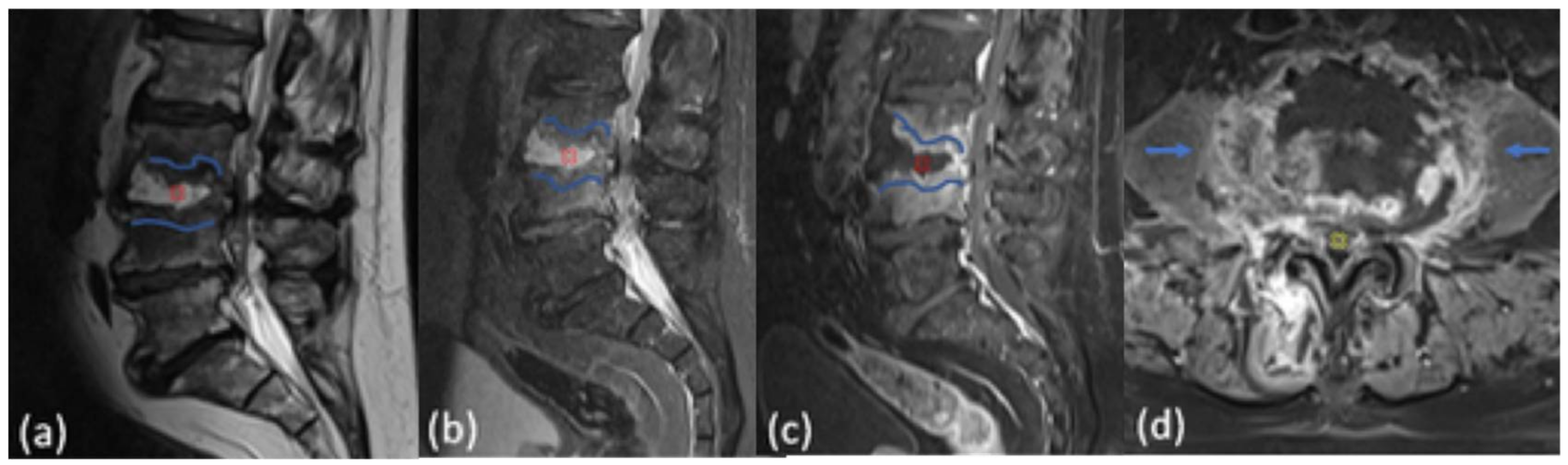
2.2. MR Imaging
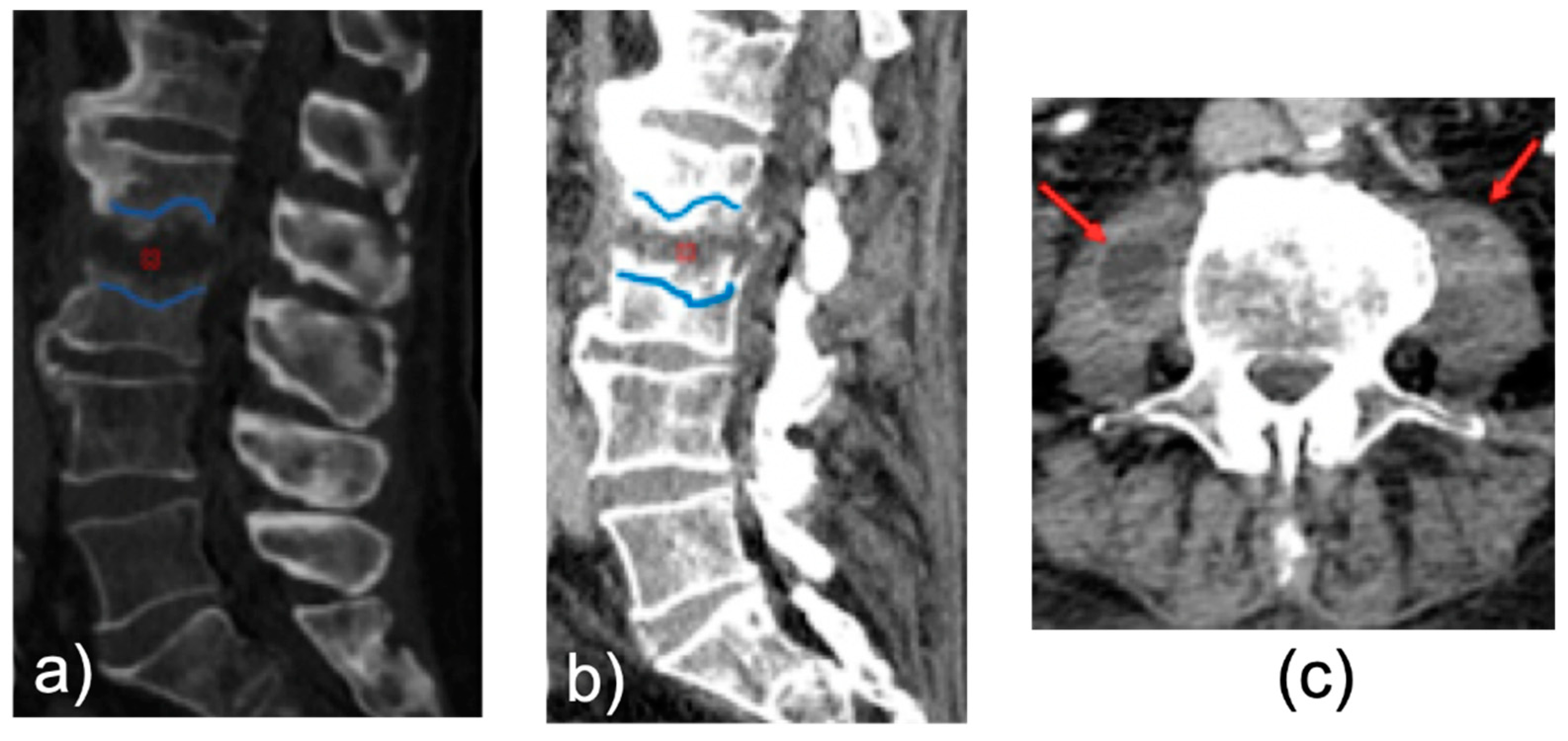
2.3. MDCT Imaging
2.4. Image Analyses
2.5. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grammatico, L.; Baron, S.; Rusch, E.; Lepage, B.; Surer, N.; Desenclos, J.C.; Besnier, J.M. Epidemiology of vertebral osteomyelitis (VO) in France: Analysis of hospital-discharge data 2002–2003. Epidemiol. Infect. 2008, 136, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Lora-Tamayo, J.; Euba, G.; Narváez, J.A.; Murillo, O.; Verdaguer, R.; Sobrino, B.; Narváez, J.; Nolla, J.M.; Ariza, J. Changing Trends in the Epidemiology of Pyogenic Vertebral Osteomyelitis: The Impact of Cases with No Microbiologic Diagnosis. Semin. Arthritis Rheum. 2011, 41, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Kowalski, T.J.; Osmon, D.R.; Enzler, M.; Steckelberg, J.M.; Huddleston, P.M.; Nassr, A.; Mandrekar, J.M.; Berbari, E.F. Long-Term Outcome of Pyogenic Vertebral Osteomyelitis: A Cohort Study of 260 Patients. Open Forum Infect. Dis. 2014, 1, ofu107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zimmerli, W. Vertebral Osteomyelitis. N. Engl. J. Med. 2010, 362, 1022–1029. [Google Scholar] [CrossRef]
- Berbari, E.F.; Kanj, S.S.; Kowalski, T.J.; Darouiche, R.O.; Widmer, A.F.; Schmitt, S.K.; Hendershot, E.F.; Holtom, P.D.; Huddleston, P.M.; Petermann, G.W.; et al. 2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adults. Clin. Infect. Dis. 2015, 61, e26–e46. [Google Scholar] [CrossRef] [Green Version]
- Luney, M.; Adiamah, A.; Pearson, L. Thoracic spondylodiscitis presenting as abdominal pain. BMJ Case Rep. 2016, 2016, bcr2015213846. [Google Scholar] [CrossRef]
- Diehn, F.E. Imaging of spine infection. Radiol. Clin. North Am. 2012, 50, 777–798. [Google Scholar] [CrossRef]
- Modic, M.T.; Feiglin, D.H.; Piraino, D.W.; Boumphrey, F.; Weinstein, M.A.; Duchesneau, P.M.; Rehm, S. Vertebral osteomyelitis: Assessment using, M.R. Radiology 1985, 157, 157–166. [Google Scholar] [CrossRef]
- Ledermann, H.P.; Schweitzer, M.E.; Morrison, W.B.; Carrino, J.A. MR Imaging Findings in Spinal Infections: Rules or Myths? Radiology 2003, 228, 506–514. [Google Scholar] [CrossRef]
- Mete, B.; Vanli, E.; Yemisen, M.; Balkan, I.I.; Dagtekin, H.; Ozaras, R.; Saltoglu, N.; Mert, A.; Ozturk, R.; Tabak, F. The Role of Invasive and Non-Invasive Procedures in Diagnosing Fever of Unknown Origin. Int. J. Med. Sci. 2012, 9, 682–689. [Google Scholar] [CrossRef] [Green Version]
- Hillen, T.J.; Wessell, D.E. Multidetector CT scan in the evaluation of chest pain of nontraumatic musculoskeletal origin. Thorac. Surg. Clin. 2010, 20, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Henes, F.O.; Nüchtern, J.V.; Groth, M.; Habermann, C.R.; Regier, M.; Rueger, J.M.; Adam, G.; Großterlinden, L.G. Comparison of diagnostic accuracy of Magnetic Resonance Imaging and Multidetector Computed Tomography in the detection of pelvic fractures. Eur. J. Radiol. 2012, 81, 2337–2342. [Google Scholar] [CrossRef] [PubMed]
- Henes, F.O.; Groth, M.; Kramer, H.; Schaefer, C.; Regier, M.; Derlin, T.; Adam, G.; Bannas, P. Detection of occult vertebral fractures by quantitative assessment of bone marrow attenuation values at MDCT. Eur. J. Radiol. 2014, 83, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Abbey, D.M.; Hosea, S.W. Diagnosis of vertebral osteomyelitis in a community hospital by using computed tomography. Arch. Intern. Med. 1989, 149, 2029–2035. [Google Scholar] [CrossRef] [PubMed]
- Wirtz, D.C.; Genius, I.; Wildberger, J.E.; Adam, G.; Zilkens, K.W.; Niethard, F.U. Diagnostic and therapeutic management of lumbar and thoracic spondylodiscitis–an evaluation of 59 cases. Arch. Orthop. Trauma Surg. 2000, 120, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Begemann, P.G.; Kemper, J.; Gatzka, C.; Stork, A.; Nolte-Ernsting, C.; Adam, G. Value of multiplanar reformations (MPR) in multidetector CT (MDCT) of acute vertebral fractures: Do we still have to read the transverse images? J. Comput. Assist. Tomogr. 2004, 28, 572–580. [Google Scholar] [CrossRef]
- Wedegartner, U.; Gatzka, C.; Rueger, J.M.; Adam, G.; Multislice, C.T. Multislice CT (MSCT) in the detection and classification of pelvic and acetabular fractures. RöFo Fortschr. Auf Dem Geb. Röntgenstrahlen Nukl. 2003, 175, 105–111. [Google Scholar]
- Wang, D.; Li, L.; Li, N.; He, J. MDCT Evaluation of Costal Bone Lesions: Comparison of Axial, Multiplanar, and 3D Volume-Rendered Images. Medicine 2015, 94, e889. [Google Scholar] [CrossRef]
- Arbelaez, A.; Restrepo, F.; Castillo, M. Spinal Infections: Clinical and Imaging Features. Top. Magn. Reson. Imaging 2014, 23, 303–314. [Google Scholar] [CrossRef]
- Go, J.L.; Rothman, S.; Prosper, A.; Silbergleit, R.; Lerner, A. Spine infections. Neuroimaging Clin. N. Am. 2012, 22, 755–772. [Google Scholar] [CrossRef]
- Stäbler, A.; Reiser, M.F. Imaging of spinal infection. Radiol. Clin. North Am. 2001, 39, 115–135. [Google Scholar] [CrossRef]
- Golimbu, C.; Firooznia, H.; Rafii, M. CT of osteomyelitis of the spine. Am. J. Roentgenol. 1984, 142, 159–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Epstein, N.E. Timing and prognosis of surgery for spinal epidural abscess: A review. Surg. Neurol. Int. 2015, 6, S475–S486. [Google Scholar] [CrossRef] [Green Version]
- Mavrogenis, A.F.; Igoumenou, V.; Tsiavos, K.; Megaloikonomos, P.; Panagopoulos, G.N.; Vottis, C.; Giannitsioti, E.; Papadopoulos, A.; Soultanis, K.C. When and how to operate on spondylodiscitis: A report of 13 patients. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 31–40. [Google Scholar] [CrossRef]
- Ghobrial, G.M.; Beygi, S.; Viereck, M.J.; Maulucci, C.M.; Sharan, A.; Heller, J.; Jallo, J.; Prasad, S.; Harrop, J.S. Timing in the surgical evacuation of spinal epidural abscesses. Neurosurg. Focus 2014, 37, E1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schorn, C.; Obenauer, S.; Funke, M.; Hermann, K.P.; Kopka, L.; Grabbe, E. Slice sensitivity profile and image pixel noise of multi-slice spiral CT in comparison with single slice spiral CT. RöFo Fortschr. Auf Dem Geb. Röntgenstrahlen Nukl. 1999, 171, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Gosangi, B.; Mandell, J.C.; Weaver, M.J.; Uyeda, J.W.; Smith, S.E.; Sodickson, A.D.; Khurana, B. Bone Marrow Edema at Dual-Energy CT: A Game Changer in the Emergency Department. Radiographics 2020, 40, 859–874. [Google Scholar] [CrossRef]
- Saba, L.; De Filippo, M.; Saba, F.; Fellini, F.; Marcy, P.Y.; Dagan, R.; Voituriez, P.; Aelvoet, J.; Klotz, G.; Bernard, R.; et al. Dual energy CT and research of the bone marrow edema: Comparison with MRI imaging. Indian J. Radiol. Imaging 2019, 29, 386–390. [Google Scholar] [CrossRef]
- Urban, B.A.; Fishman, E.K. Tailored helical CT evaluation of acute abdomen. Radiographics 2000, 20, 725–749. [Google Scholar] [CrossRef] [Green Version]
- Hammond, N.A.; Nikolaidis, P.; Miller, F.H. Left lower-quadrant pain: Guidelines from the American College of Radiology appropriateness criteria. Am. Fam. Physician 2010, 82, 766–770. [Google Scholar]
| Patients | Sex | Age |
|---|---|---|
| 1 | M | 60 |
| 2 | F | 65 |
| 3 | M | 61 |
| 4 | M | 63 |
| 5 | M | 63 |
| 6 | F | 70 |
| 7 | M | 57 |
| 8 | M | 58 |
| 9 | M | 57 |
| 10 | F | 65 |
| 11 | M | 63 |
| 12 | F | 70 |
| 13 | M | 61 |
| 14 | M | 69 |
| 15 | F | 64 |
| 16 | M | 60 |
| 17 | F | 71 |
| 18 | M | 67 |
| 19 | M | 65 |
| 20 | F | 70 |
| 21 | F | 64 |
| 22 | M | 65 |
| 23 | F | 71 |
| 24 | F | 70 |
| 25 | M | 69 |
| Disease Present | Disease Absent | |
|---|---|---|
| MDCT Positive | 13 | 0 |
| MDCT Negative | 6 | 6 |
| Finding | Location | Number |
|---|---|---|
| edema-related changes | vertebral body | 22 (100%) |
| erosive bone changes | vertebral body | 9 (40.9%) |
| inflammatory tissue | paravertebral and or epidural space | 21(95.5%) |
| contrast enhancement | vertebral body and or intervertebral disc | 22 (100%) |
| Finding | Location | Number |
|---|---|---|
| erosive bone changes | vertebral body | 13 (86%) |
| inflammatory tissue | paravertebral and or epidural space | 14 (94%) |
| contrast enhancement | vertebral body and or intervertebral disc | 9 CECT (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Negro, A.; Somma, F.; Tortora, M.; Lugarà, M.; Tamburrini, S.; Coppola, M.G.; Piscitelli, V.; Fasano, F.; Sicignano, C.; Vargas, O.; et al. The Diagnostic Performance of Multi-Detector Computed Tomography (MDCT) in Depiction of Acute Spondylodiscitis in an Emergency Department. Tomography 2022, 8, 1895-1904. https://doi.org/10.3390/tomography8040160
Negro A, Somma F, Tortora M, Lugarà M, Tamburrini S, Coppola MG, Piscitelli V, Fasano F, Sicignano C, Vargas O, et al. The Diagnostic Performance of Multi-Detector Computed Tomography (MDCT) in Depiction of Acute Spondylodiscitis in an Emergency Department. Tomography. 2022; 8(4):1895-1904. https://doi.org/10.3390/tomography8040160
Chicago/Turabian StyleNegro, Alberto, Francesco Somma, Mario Tortora, Marina Lugarà, Stefania Tamburrini, Maria Gabriella Coppola, Valeria Piscitelli, Fabrizio Fasano, Carmine Sicignano, Ottavia Vargas, and et al. 2022. "The Diagnostic Performance of Multi-Detector Computed Tomography (MDCT) in Depiction of Acute Spondylodiscitis in an Emergency Department" Tomography 8, no. 4: 1895-1904. https://doi.org/10.3390/tomography8040160
APA StyleNegro, A., Somma, F., Tortora, M., Lugarà, M., Tamburrini, S., Coppola, M. G., Piscitelli, V., Fasano, F., Sicignano, C., Vargas, O., Pace, G., Giardiello, M., Iannuzzi, M., Toro, G., De Simone, F., Catalano, M., Carbone, R., Rocco, C., Saturnino, P. P., ... D’Agostino, V. (2022). The Diagnostic Performance of Multi-Detector Computed Tomography (MDCT) in Depiction of Acute Spondylodiscitis in an Emergency Department. Tomography, 8(4), 1895-1904. https://doi.org/10.3390/tomography8040160







