1. Introduction
Mastectomy patients who have undergone breast tissue removal for breast cancer treatment experience not only physical pain, but also psychological anxiety and damage to the physical image, which may restrict them from social activities and affect their human relations [
1,
2,
3,
4]. According to the National Cancer Information Center [
5], in 2018, 64.8% of patients with breast cancer in Korea underwent a total mastectomy, which is the total excision of skin and lymph nodes, including the entire breast tissue and nipples, and only 26% underwent breast-conserving surgery, which is the removal of cancer without breast tissue. Patients who underwent surgical excision experienced physical pain, such as an imbalance in body shape due to loss of breasts, muscular pain, paresthesia, lymphedema, and muscle weakness, while approximately 30% experienced functional obstruction [
6]. Additionally, in a study by Al-Ghazal et al. [
7], patients who had undergone mastectomy developed diverse physical symptoms, including scoliosis or shoulder pain due to an imbalance in their body weight. Another study revealed that 78% of mastectomy patients had their upper body distorted by up to 3
[
8].
Although an increasing number of patients are undergoing breast reconstruction, surgery is not always an option owing to medical issues, which is why there remains a high percentage of breast cancer patients who do not have their breasts reconstructed. Therefore, mastectomy bras and breast prostheses are suggested as a substitute for breasts [
9,
10]. This suggestion is related to a study reporting that wearing a breast prosthesis improved upper limb motility [
11]. Therefore, the mastectomy brassiere and breast prosthesis will help reduce physical pain along the mastectomy, and thus need suitable fitting. However, wearing inappropriate mastectomy bras and breast prostheses may instead cause physical deformation or musculoskeletal pain. Gho et al. [
12] claimed that the unbalanced movement of the left and right breasts causes patients to recognize the incompleteness of their body image, thereby causing psychological distress. Therefore, each bra should be personalized and customized for the right bra fit that reflects the body shapes of mastectomy patients. The need to solve the left–right imbalance and variability in the position of a brassiere for breast cancer patients has been mentioned in numerous studies [
13,
14], yet functionality has not been improved. This problem necessitates the need to study and produce bras that are suitable for the body shapes of mastectomy patients. At present, there are insufficient human body data on total mastectomy patients, which would have aided in the production process. Moreover, mastectomy patients have different areas or forms of excision, such as breasts and axillary lymph nodes, depending on the stage or method of surgery, which makes it difficult to categorize the body shapes for certain areas of measurement. In addition, the current human body measurement method used for manufacturing has a disadvantage: accurate measurement cannot be made because the bottom surface of the breast cannot be determined. In addition, as mastectomy patients tend to avoid revealing their affected parts [
15,
16], it may be a burden on them to expose their excised breasts to others to collect human body data for customizing bras. Thus, it is necessary to establish contactless body measurement methods to minimize repeated exposure of the body as well as skin contact to ensure the patients’ mental stability.
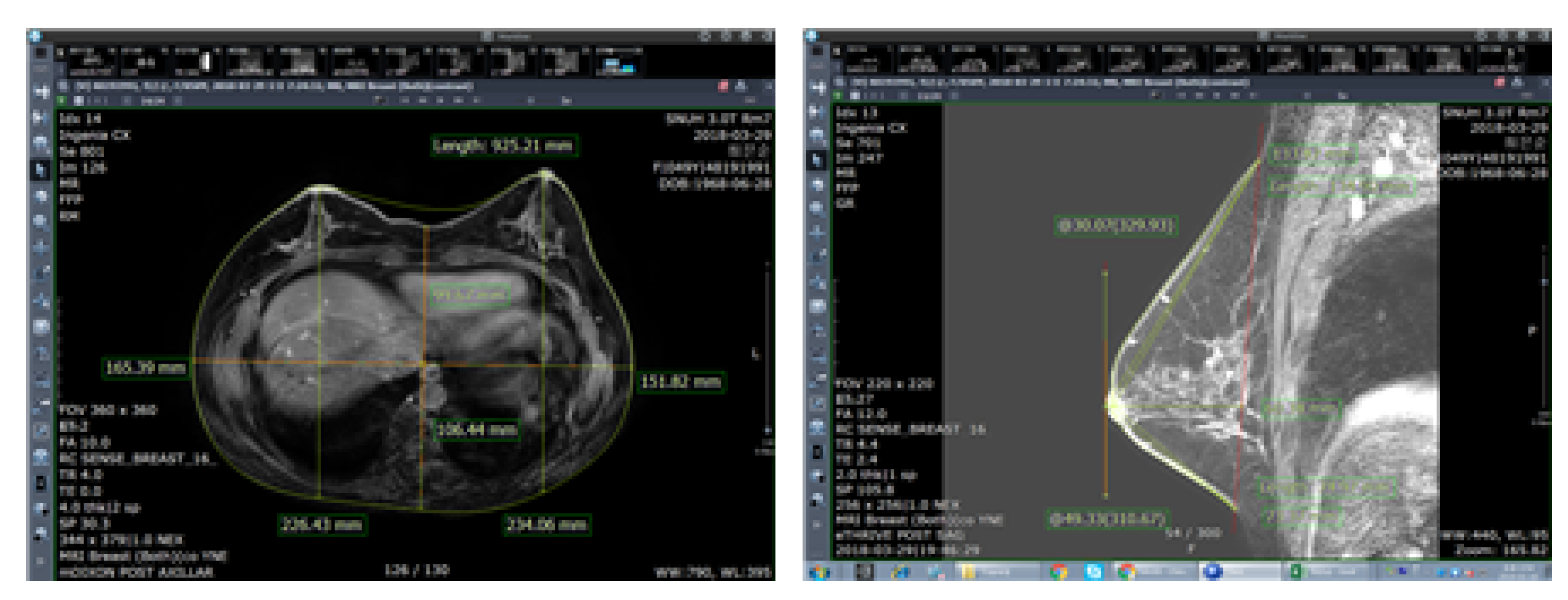
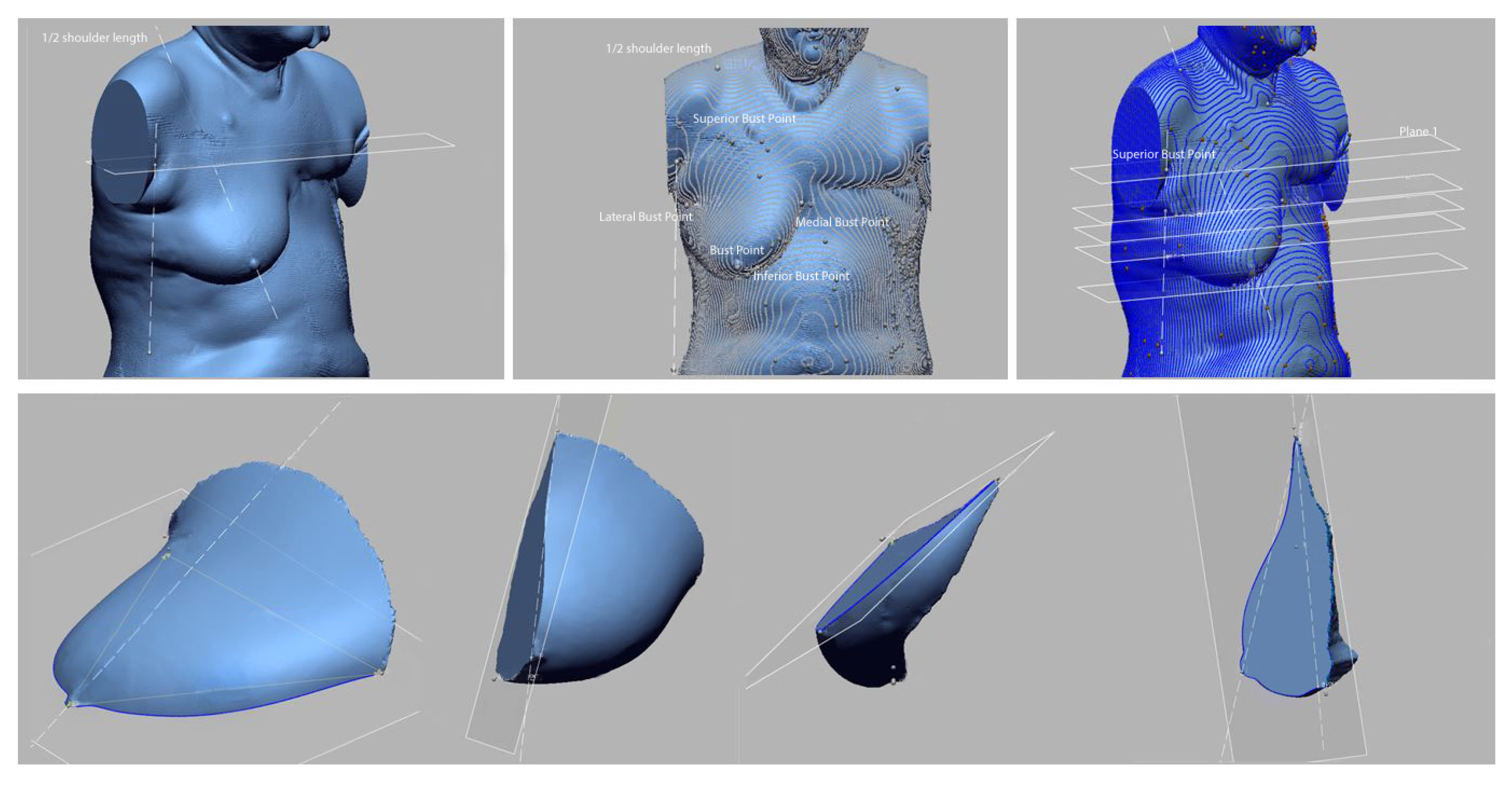
Methods of collecting breast-related human body data include using human body images, such as magnetic resonance imaging (MRI) and computed tomography (CT) for medical purposes or anthropometric 3D body scanning for ergonomic purposes. As MRI is scanned from multiple angles, more stereoscopic human body data can be obtained. Thus, MRI is used for various purposes, such as restoration of the human body or volume measurements and for ergonomic purposes. Nonetheless, the shape of breasts may vary in MRI and 3D body scanning depending on the posture, which results in different measurements of detailed items. However, to the best of our knowledge, there has been no research on the posture that best displays the characteristics of breasts and is thus suitable for bra design. Therefore, this study uses MRI data, a medical imaging technique, to measure similar results of breast volume as 3D body scanning and compare it using anthropometric data, thereby identifying that the volume of the two data is the same. Nevertheless, as breasts are soft and easily change shape, cups in various designs can be worn as long as the under-bust circumference and bra cup size match [
17].
Consequently, this study hypothesizes that the volume of breasts will remain the same, even when the shape changes because breasts are comprised of adipose substances and do not have bones. If the volume is constant, the drafting of the bra pattern will be possible. If so, it will be possible to make clothes, even if medical images are used, not necessarily according to the human body measurement method. Therefore, this study assumes that the breast volume is the same, despite the difference in measurement methods. To prove the possibility, this study was designed to illuminate areas showing differences in measured values for different measurement methods and to compare breast volumes. Therefore, this study will test the hypothesis that, despite the different correlations and measurement methods, the breast volume remains the same by measuring the volume of the two different visual data. If the hypothesis is proven, it is possible to suggest the possibility that human data collected for medical purposes can be used for manufacturing clothing. Therefore, it is possible to supplement the limitations of the 3D-SIM measurement method and use the measurement method considering the psychological state of the patient in the manufacture of ergonomic clothing. In addition, the possibility of convergence research in medical and clothes engineering is presented by introducing various methods of utilizing data that have been mainly used for medical purposes.
4. Results
4.1. Anthropometric Comparison
The average age of the participants in 3D-SIM was 49.75, ranging from 45 to 54. According to the BMI standard, two participants were overweight and two were normal weight. All four participants had one of their breasts fully removed, owing to breast cancer, did not receive reconstructive surgery, and had breastfeeding experience. They received lymphadenectomy along with breast cancer surgery, but three out of the four patients suffered from edema (
Table 5).
4.2. Comparison of Characteristics Based on Human Body Data Images
Among the projective images for medical purposes, anthropometric measurements that can apply anthropometric measurement and the images containing anthropometric data to be used in bra design were MRI data. Therefore, in this study, 3D-SIM and MRI data were chosen for comparison. The results of comparing each character are shown in
Table 6.
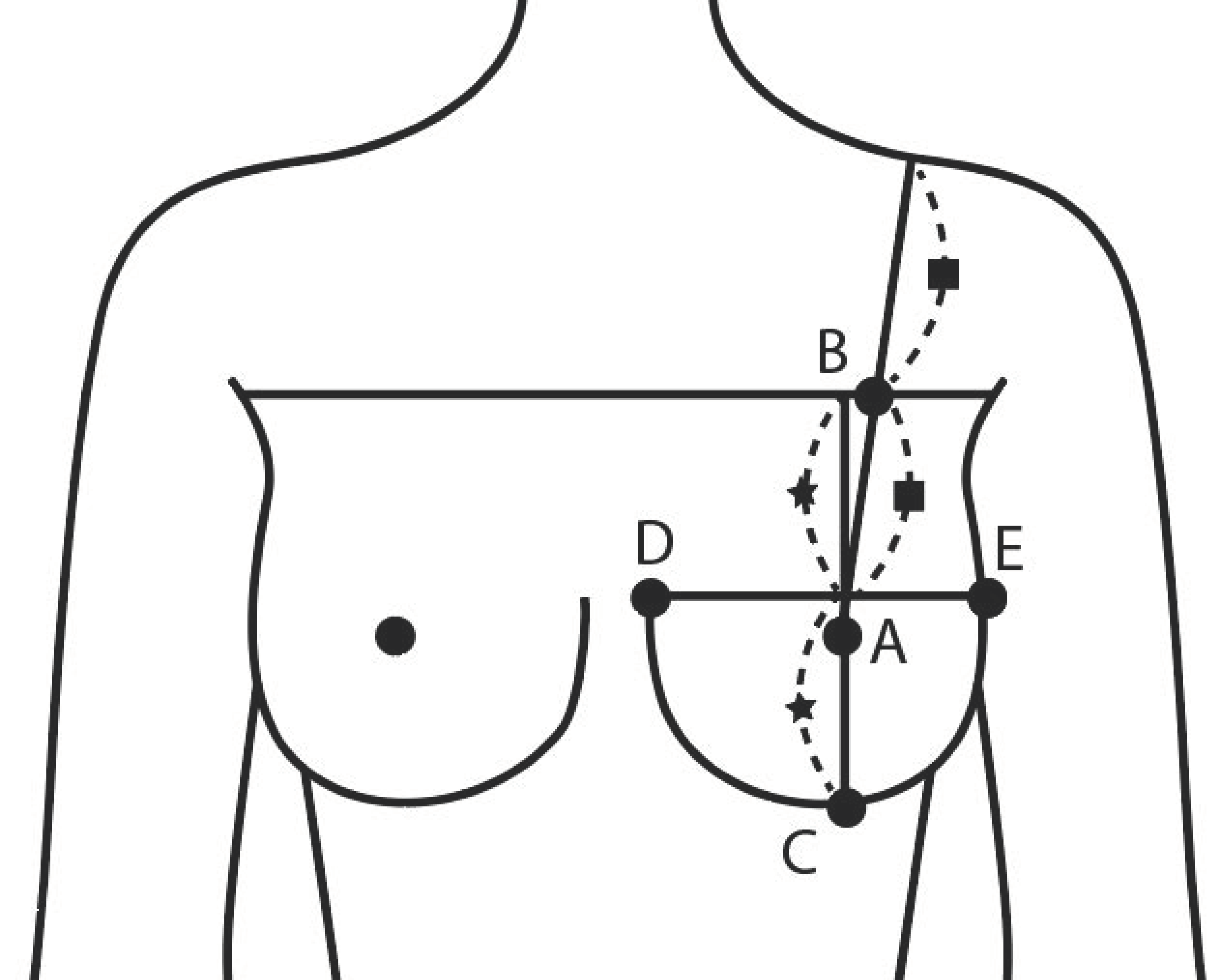
As image data by postures of 3D-SIM and MRI are different, each item can be different measurements. As follows in
Table 6, it was possible to obtain the circumference, depth, breadth, and angle items without a difference in the imaging method. Most items of length can be measured, but MRI could not measure the related shoulder, as most of the MRI focused on the breast and obtained a sectional image. However, for depth, 3D-SIM cannot measure projective items, such as bust point depth, and the breadth or height of the breast base area cannot be measured, owing to the uncertainty of the breast base in 3D-SIM. For height, MRI scans only the upper body, and thus it was impossible to measure the height.
4.3. Anthropometric Comparison
The results of analyzing human body data based on imaging of the participants are shown in
Table 7. Ten items showed a statistically significant difference and were found to be affected by the measuring method: bust depth, under-bust depth, bust breadth, under-bust breadth, lateral bust-point length, lateral bust-point surface length, upper bust slope angle, chest depth, bust point height, and circumference surface length.
In particular, the difference in items, such as depth and breadth, may be due to the difference between the standing position and prone position, where the depth was lower and the breadth higher on 3D-SIM than on MRI data. The upper bust slope angle on MRI data increased, as the breasts sagging downward were generally affected by gravity by 3D-SIM.
Lateral bust-point length was the item statistically affected by posture among the superior, inferior, medial, and lateral bust-points, surrounding the breasts. In general, breasts spread out in a radial form from the body; thus, the length from bust-point to lateral bust-point was longer than the length from the bust-point to medial bust-point, but as axillary muscles of saggy breasts tend to droop due to lack of elasticity, the lateral bust-point length tends to be longer than the medial bust-point length. Moreover, the lateral bust-point and medial bust-point on 3D-SIM data were longer than MRI data, as the breasts droop downward. In addition, in the case of saggy breasts, the bust circumference line of 3D-SIM data is lower than the bust location of MRI data, owing to gravity. Saggy breasts have lower chest and bust point depth, as they droop downward, compared to hemispherical breasts, but when affected equally by gravity as shown in MRI data, chest and bust point depth were statistically proven to be longer than 3D-SIM.
Lateral bust point length was the item statistically affected by posture among superior bust point, inferior bust point, medial bust point, and lateral bust point surrounding the breasts. In general, breasts spread out in radial form from the body, and thus the length from bust point to lateral bust point was longer than the length from bust point to medial bust point, but since axillary muscles of saggy breasts tend to droop due to lack of elasticity, the lateral bust point length tends to be longer than the medial bust point length. Moreover, the lateral bust point and medial bust point on 3D-SIM data were longer than MRI data since the breasts droop downward. Moreover, in the case of saggy breasts, the bust circumference line of 3D-SIM data is lower than the bust location of MRI data due to gravity. Saggy breasts have lower chest depth and bust point depth since they droop downward, compared to hemispherical breasts, but when affected equally by gravity as shown in MRI data, chest depth and bust point depth were statistically proved to be longer than 3D-SIM.
4.4. Comparison of Breast Volume in MRI and 3D-SIM Data
Breast volume of MRI and 3D-SIM was obtained using the formulas above, and the results of a paired samples t-test to determine whether the two have different data are shown in
Table 8. The results were
t = 0.617 and
p = 0.581, not showing a statistically significant difference at a significance level of 0.05, indicating no difference in the total volume of the two data (
Table 8).
To validate the size of breast volume obtained from the formulas, this study used the breast volume provided in Hologic R2 and Volpara, which is the mammography system among PPM data of patients (
Table 9). Breast volume measured in the program above has a linear relationship of r2 = 0.89 with the actual breast volume and has high predictive power [
49], and thus is used as the comparison group to validate the MRI and 3D-SIM volume data. The difference in breast volume between the three measurement methods was statistically analyzed using the Friedman test. The results were ×2 = 3.50 and
p = 0.17 at a 0.05 significance level, showing no difference between the three volumes. This experiment proved that the measurement of breast volume is statistically similar regardless of breast shape.
5. Discussion
A total of 68.4% of breast cancer patients worldwide choose mastectomy for breast cancer treatment. It is because mastectomy has been effective in preventing active cancer metastasis so far [
50,
51]. Mastectomy patients have been wearing mastectomy bras or breast prostheses to supplement their physical body and for body image treatment [
52,
53]. Patients who choose mastectomy for breast cancer treatment suffer not only psychological pain due to body loss, but also physical pain due to body imbalance. Therefore, it is recommended to wear a bra with an artificial breast for excision patients. However, as wearing a bra and artificial breast that do not fit the body well increases pain, it is necessary to manufacture an individually tailored bra and artificial breast.
Body data are obtained through body scanning using anthropometric methods that can be used with 3D-SIM data to design customized mastectomy bras. However, there is the discomfort of having to reveal one’s body to others. In addition, the anthropometric posture causes the breasts to sag, thereby not perfectly revealing the breast characteristics.
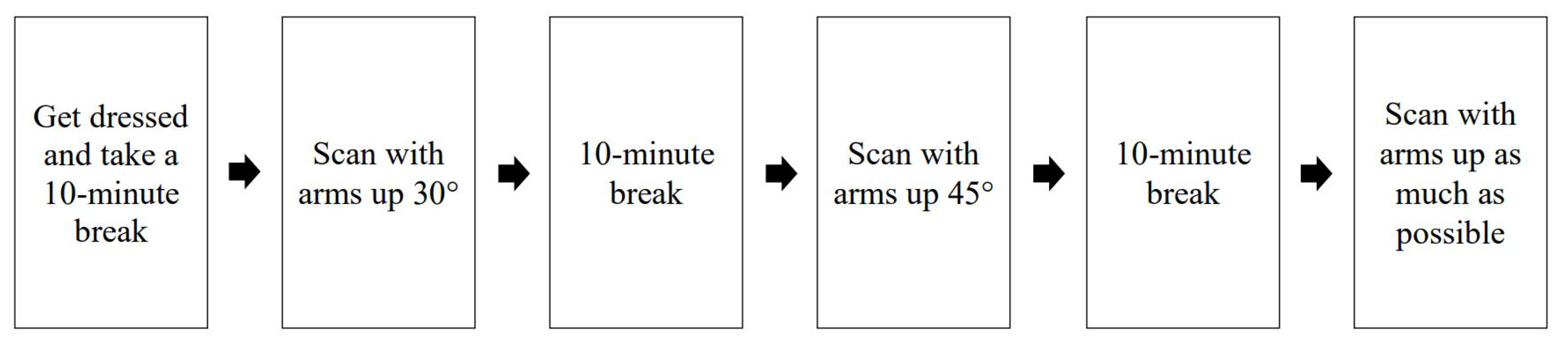
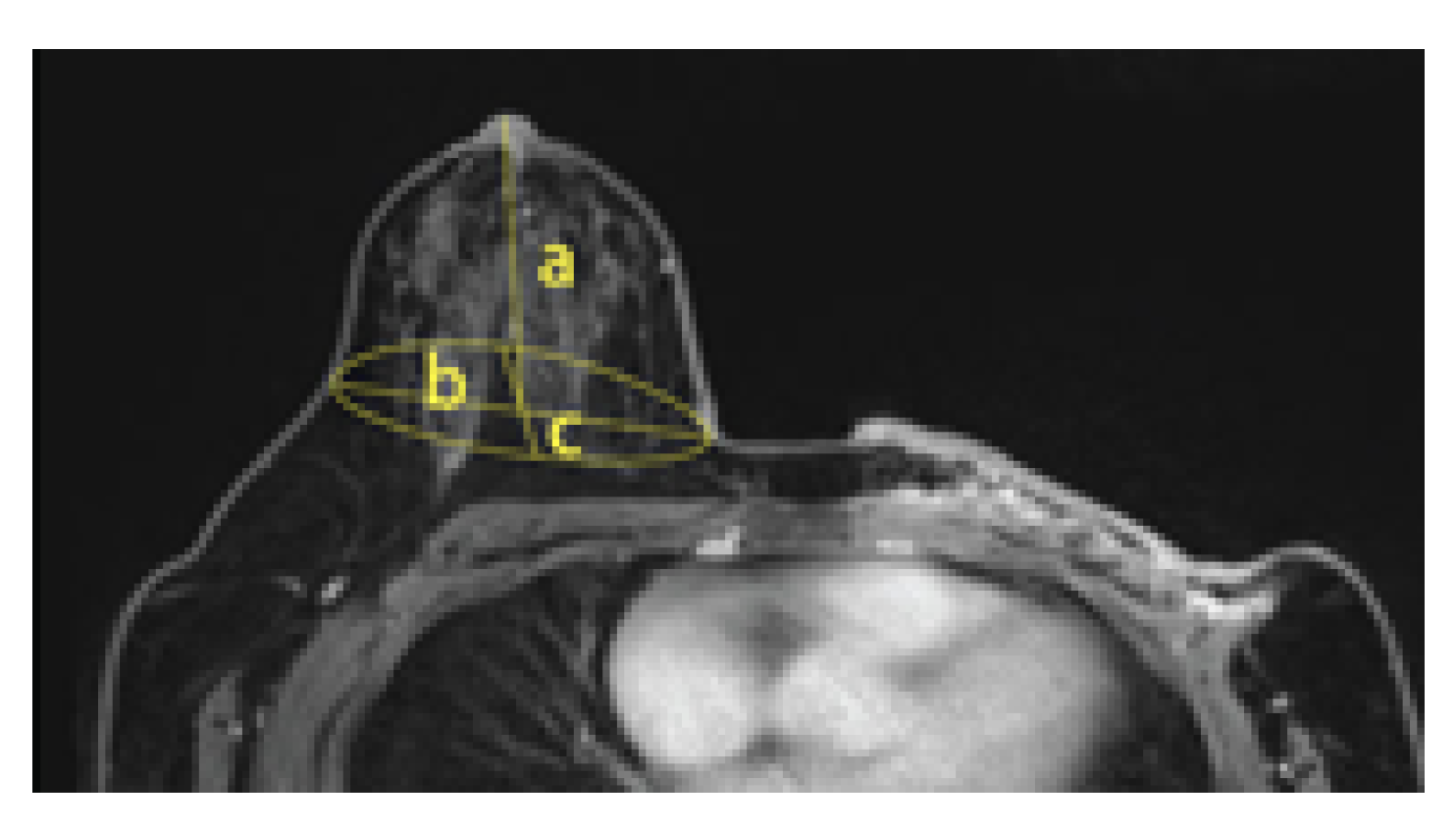
Thus, this study was designed to test the hypothesis that, as the breast consists of adipose tissue and a few muscles, breasts have consistent volume regardless of shape, owing to posture. Additionally, the relevant volume measurements from the medical image, not the anthropometric image data, can be used to make mastectomy bras. Therefore, this study used image data for medical purposes as human body data that can limit exposure to the human body while well-displaying breast characteristics. MRI can scan the inside of the human body, skeletal structure, and outline simultaneously, using nuclear magnetic resonance, while 3D-SIM can film the surface of the human body, using white structured light. Both methods are contactless measurements using energy sources that are harmless to the human body. As for posture, MRI requires the patient to lie prone on the device and let the breasts droop through the holes of the bed; therefore, the bust will be in an ellipsoid shape (sloth) and is completely separated from the body.
However, 3D-SIM requires the patient to be in a standing position; thus, the breasts are affected by gravity. Saggy breasts or big breasts tend to hang down, which folds with the body, making it difficult to accurately measure the under-bust circumference. Moreover, saggy breasts have a bust circumference line lower than the under-bust circumference line, which makes it difficult to define the accurate position of the anthropometric bust circumference line. MRI measures parts that are not visibly identifiable, such as the rib cage and breast base area, but the images are sectional, and thus additional processing is required to obtain the overall human body shape data. Moreover, the measurement points cannot be marked, owing to the sectional composition, and the scope of image acquisition is not consistent depending on the technician and purpose, thereby omitting parts that can be the standard for body measurements, such as anterior neck point, shoulder, and back. While 3D-SIM can obtain 3D data of the body surface and thus can apply the same measurement method as anthropometry, the projection of the breast base form and under-bust outline is unclear, thereby possibly distorting the breast base area when the breasts are too saggy. In addition, as the under-bust circumference line cannot be identified, the participants may be requested to rescan the under-bust circumference line by correcting the saggy breasts, thereby increasing their fatigue.
As PPM by MRI and 3D-SIM are scanned in different postures, the shape of the scanned breasts is also different. The measurements of the detailed items of breasts were also different in the two forms. By comparing the two data, 18 items with matching items were measured. MRI data for medical purposes and anthropometric data of 3D-SIM showed statistically significant measurements differences in 10 items: bust depth, under-bust depth, bust breadth, under-bust breadth, lateral bust point length, lateral bust point surface length, upper bust slope angle, chest depth, bust point height, and circumference surface length. Moreover, in 3D-SIM, the breasts overlap with the upper body for the under-bust circumference line and inferior bust point. Thus, the under-bust circumference line was secured by overlapping with the image securing the under-bust circumference line with different arm angles. The items showing differences in posture were breast thickness, breast width, and lower breast width. Compared with the 3D data, the PPM data showed a decrease in thickness and an increase in width. In addition, in the data of 3D-SIM, the breast is sagging. In addition, the average age of the subjects was 49.75 years; the previous research result, which proved that breast sagging occurred due to age in the 40s and older, was supported [
54]. Therefore, 3D-SIM data showed that the length of the lateral point was longer than MRI data, and the upper breast inclination angle was smaller. Although no statistically significant difference could be found, by taking the MRI measuring posture, a tendency for the length between the superior bust point to the inferior bust point tending to be longer than the 3D-SIM data was shown, but the length between the medial and lateral tended to be shorter. In general, the length between the lateral bust point and bust point is longer than the length between the medial and bust point; however, in the case of PPM, there is no such difference, suggesting the possibility of eliminating the variable of breast deformity due to sewage of the breast. In addition, it was statistically proven that the depth of the chest and the depth of the bust point greatly increased in the PPM data [
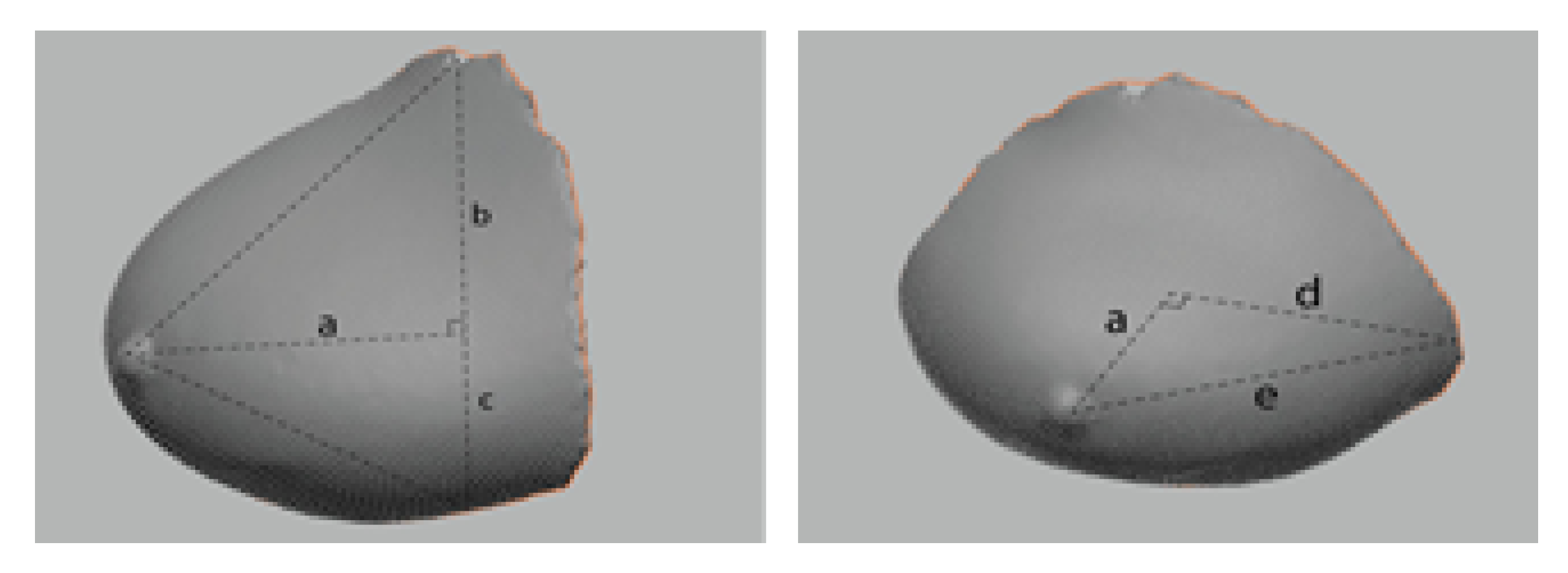
55]. Moreover, to measure the breast volume, the breast of 3D-SIM data was separated into two parts by a line between the lateral and the medial bust points through the bust point. For the upper part, the formula for calculating the cone volume was applied, while the hemispherical volume calculation formula was applied to the lower part. Therefore, breast volume for PPM by MRI and 3D-SIM was measured to identify the applicability of MRI data, which proved that there was no statistical difference in volume. In other words, making bras using MRI data with high human body reproducibility can reduce additional exposure or contact with the human body, thereby seeking the mental stability of mastectomy patients and applying all kinds of data collected in the treatment process to bra design. Moreover, by applying the characteristics of non-resected breasts to the design, the prototype bras can be adequately used on non-resected breasts as well. Using MRI data can make up for the insufficient human body data of total mastectomy patients in Korea, and the diversity of excision can be reflected in the bra design. Therefore, by using MRI data, custom bras can be made without additional body measurements.
Despite the strength of this study, there remain two major limitations. First, in the case of MRI data, although the breast is completely separated from the rib cage and the volume of the breast can be appropriately measured, there is a disadvantage that the projection range is limited to the torso. Moreover, the method and scope of taking pictures are not standardized, compared to taking images for the 3D-SIM. As MRI data scan only the torso of the human body, the scope of scanning may vary depending on the technician, thereby cropping some parts occasionally. Therefore, it is necessary to standardize the scope of scanning to use MRI data for such purposes as making bras. The second major limitation of this study is that only four mastectomy patients agreed to participate. However, the significance of the study lies in the fact that it has provided the possibility of producing bras and breast prostheses for mastectomy patients using medical images. In the future, we plan to design a drawing method that can produce a bra by setting a formula suitable for bra production using the changed length and conducting an experiment to verify the fit. Additionally, further research can be conducted on making bras based on the results of this study for a healthy body and improved clothing habits for mastectomy patients.