Retrospective Cohort Study of Frequency and Patterns of Orbital Injuries on Whole-Body CT with Maxillofacial Multi-Slice CT
Abstract
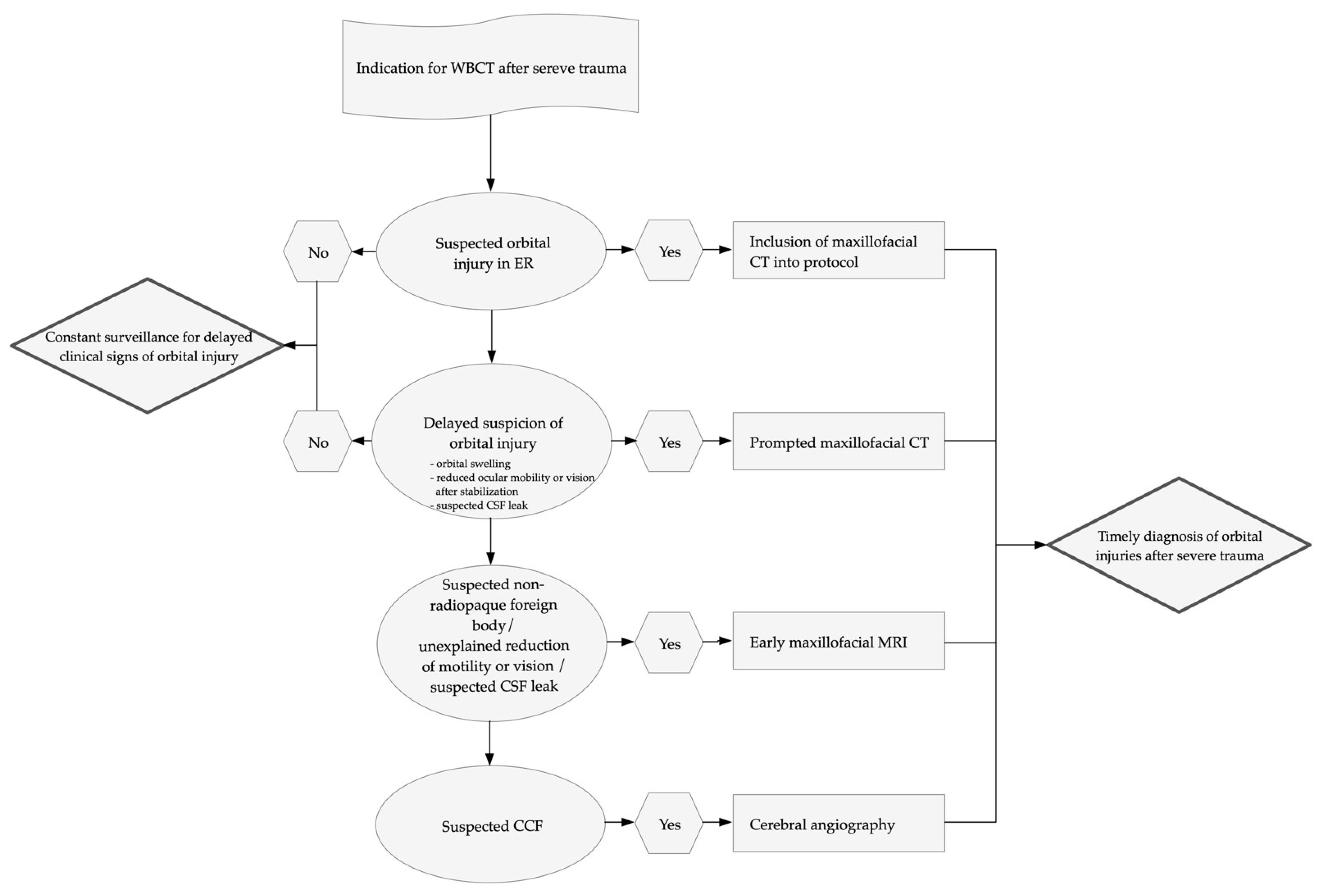
:1. Introduction
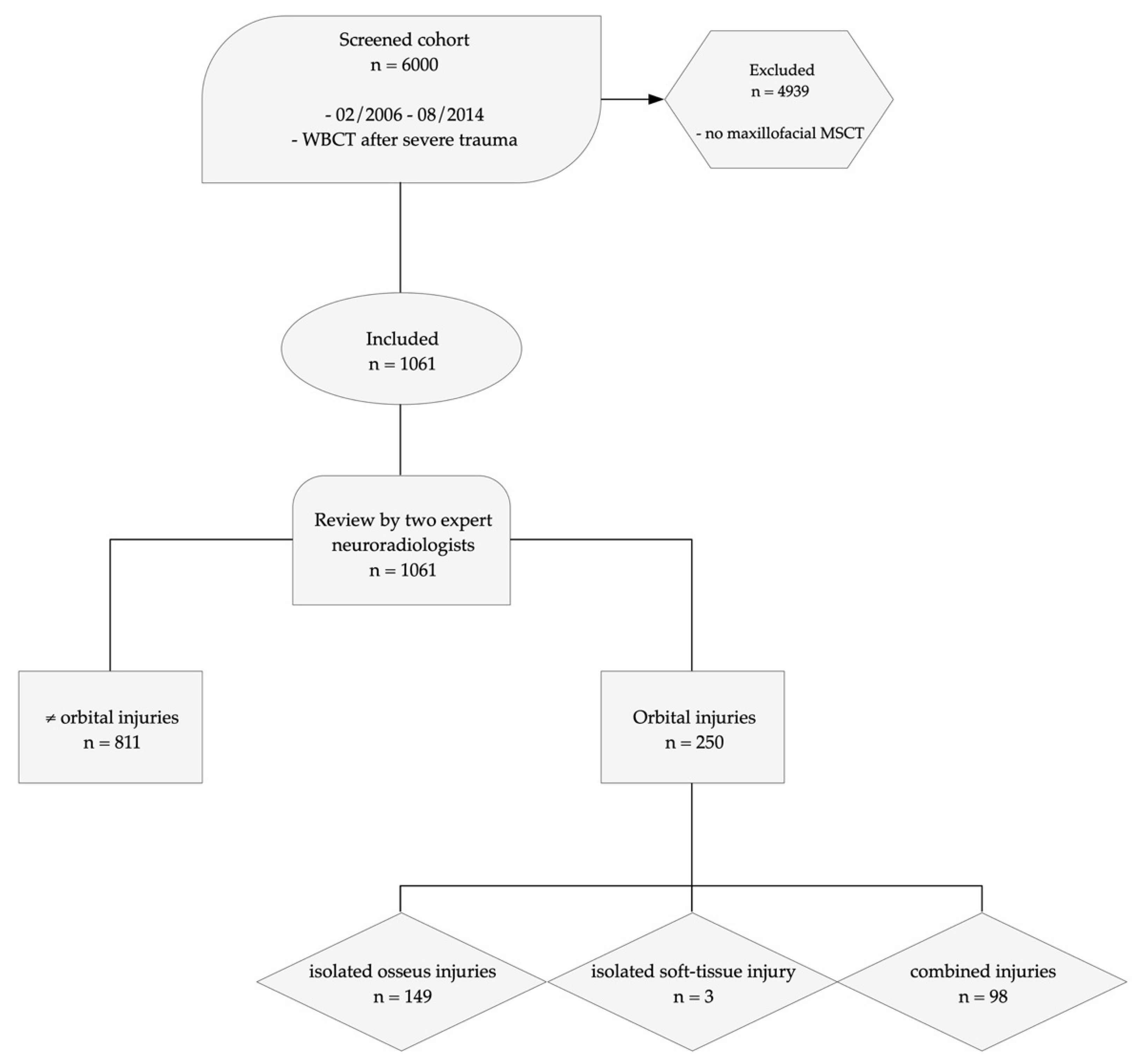
2. Materials and Methods
2.1. Study Design and Population
2.2. CT Protocol and Image Analysis
2.3. Diagnostic Criteria
2.4. Statistical Analysis
3. Results
3.1. Study Population
3.2. Frequency of Orbital Injuries
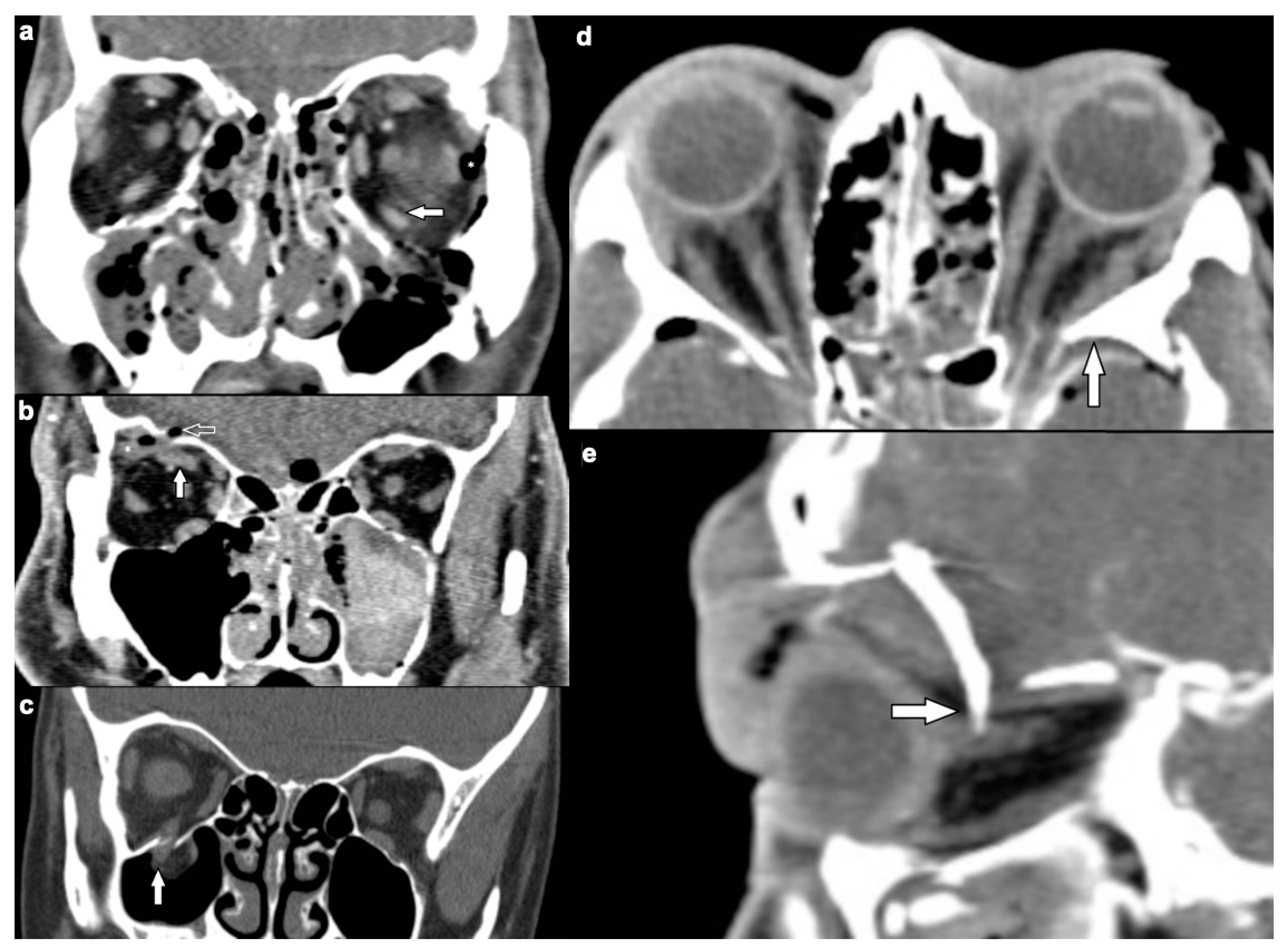
3.2.1. Osseous Injuries
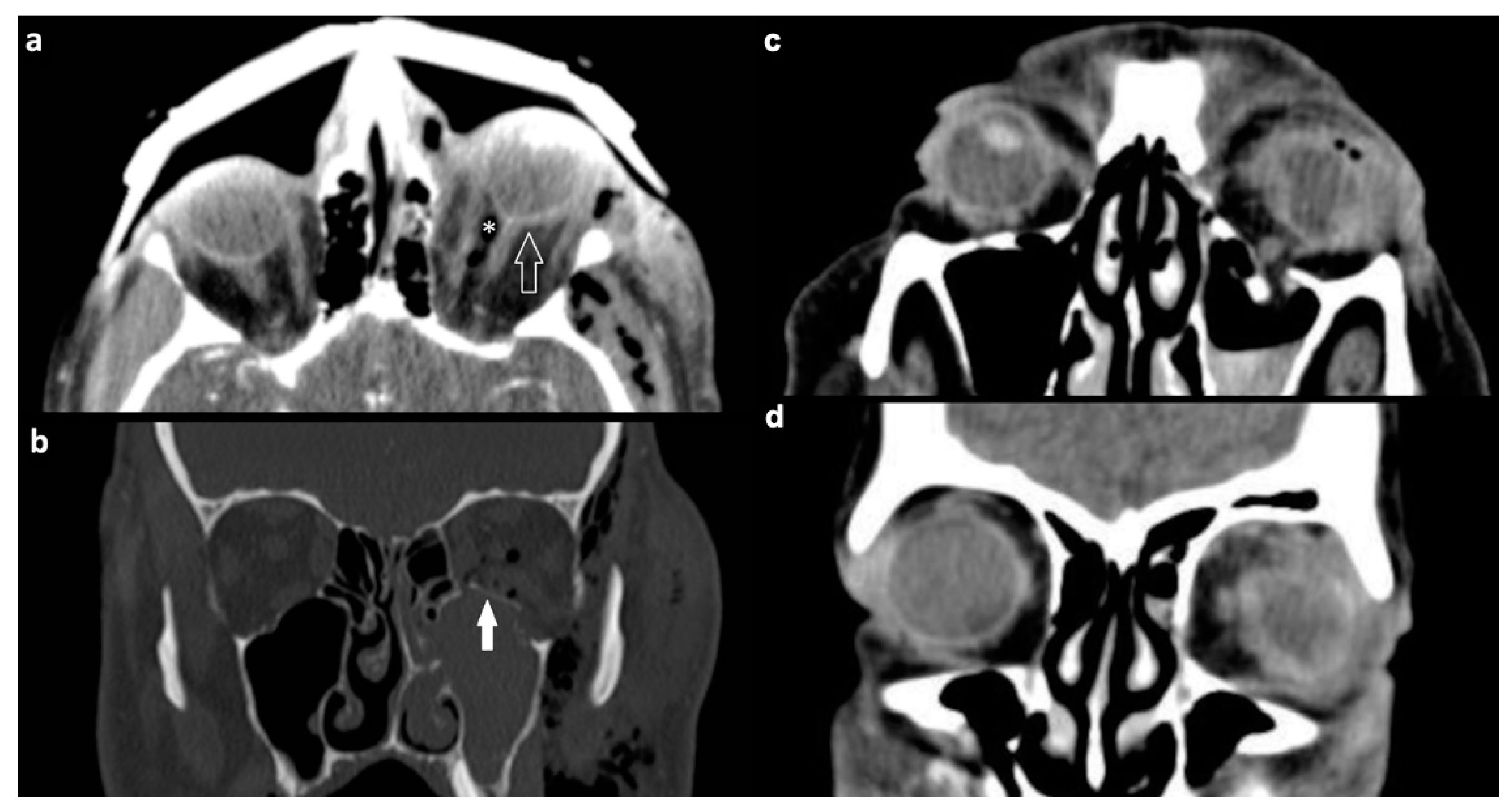
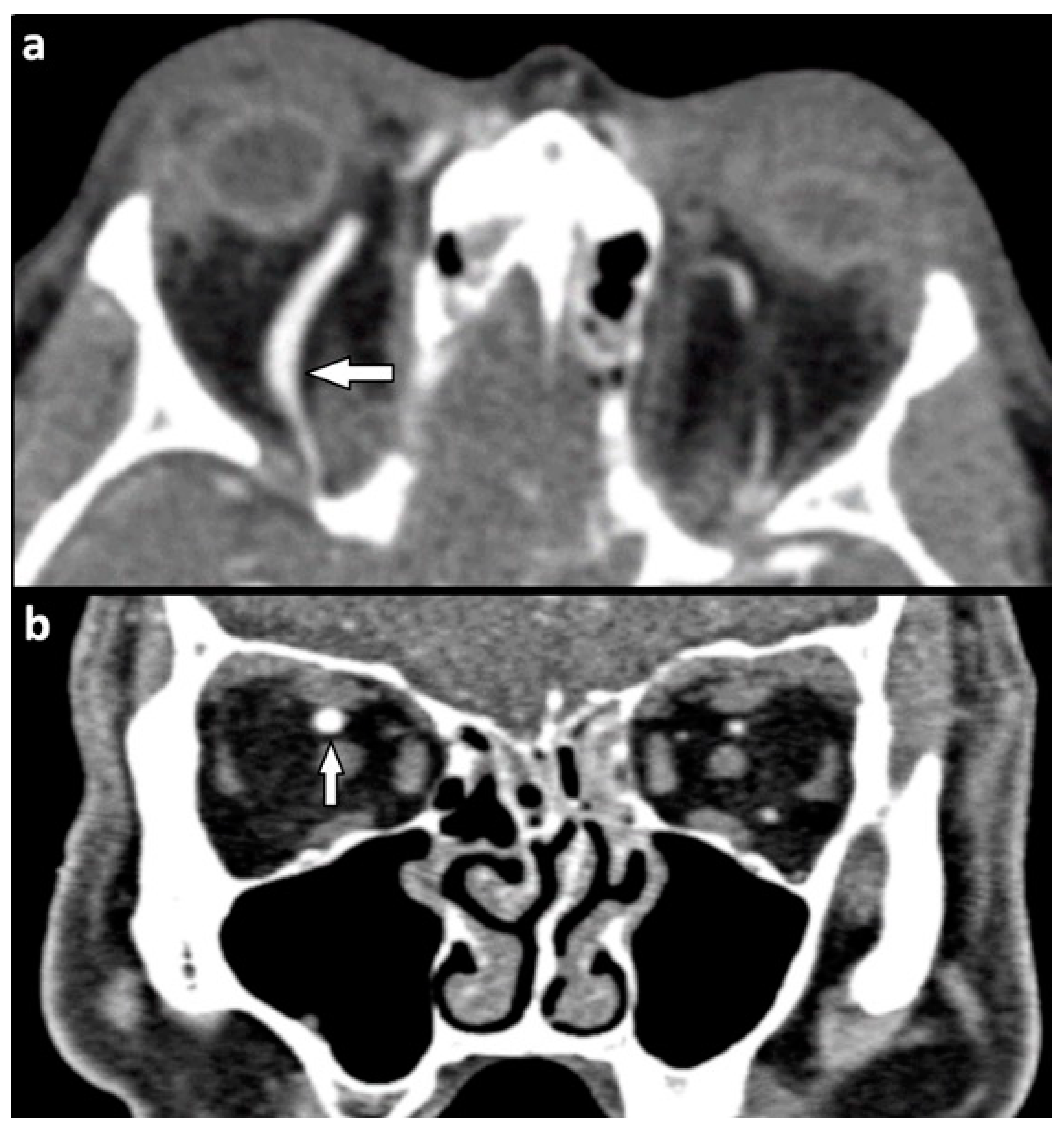
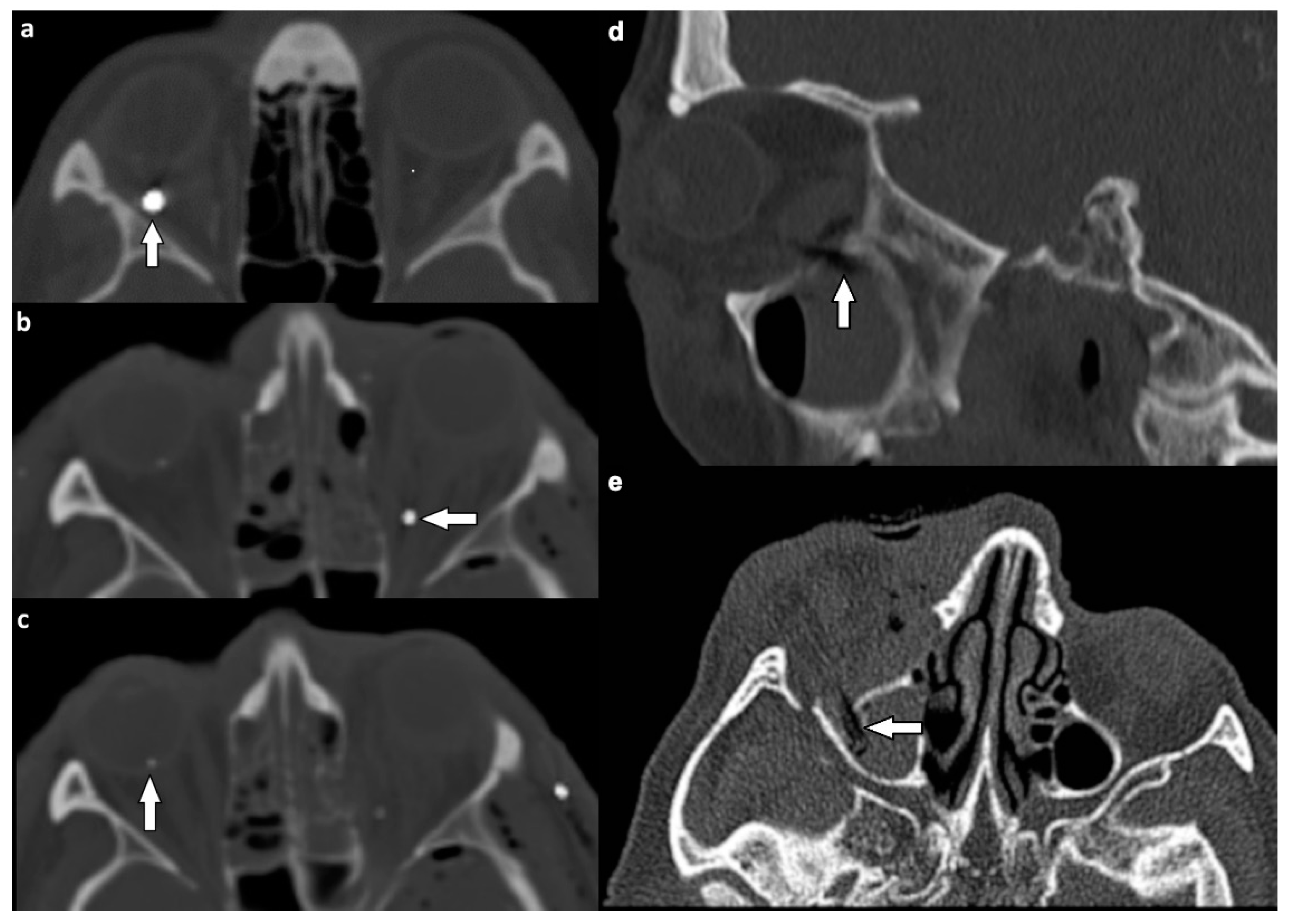
3.2.2. Soft Tissue Injuries
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chazen, J.L.; Lantos, J.; Gupta, A.; Lelli, G.J., Jr.; Phillips, C.D. Orbital soft-tissue trauma. Neuroimaging Clin. N. Am. 2014, 2, 425–437. [Google Scholar] [CrossRef] [PubMed]
- Caranci, F.; Cicala, D.; Cappabianca, S.; Briganti, F.; Brunese, L.; Fonio, P. Orbital fractures: Role of imaging. Semin. Ultrasound CT MRI 2012, 3, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Georgouli, T.; Pountos, I.; Chang, B.Y.; Giannoudis, P.V. Prevalence of ocular and orbital injuries in polytrauma patients. Eur. J. Trauma Emerg. Surg. 2011, 37, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Tonini, M.; Krainik, A.; Bessou, P.; Lefournier, V.; Boubagra, K.; Chiquet, C.; Le Bas, J.F. How helical CT helps the surgeon in oculo-orbital trauma. J. Neuroradiol. 2009, 36, 185–198. [Google Scholar] [CrossRef] [PubMed]
- de Vries, R.; Reininga, I.H.F.; Pieske, O.; Lefering, R.; El Moumni, M.; Wendt, K. Injury mechanisms, patterns and outcomes of older polytrauma patients—An analysis of the Dutch Trauma Registry. PLoS ONE 2018, 5, e0190587. [Google Scholar] [CrossRef] [PubMed]
- You, N.; Choi, M.S.; Roh, T.H.; Jeong, D.; Kim, S.H. Severe Facial Fracture is Related to Severe Traumatic Brain Injury. World Neurosurg. 2018, 111, e47–e52. [Google Scholar] [CrossRef] [PubMed]
- McCarty, J.C.; Kiwanuka, E.; Gadkaree, S.; Siu, J.M.; Caterson, E.J. Traumatic Brain Injury in Trauma Patients with Isolated Facial Fractures. J. Craniofac. Surg. 2020, 31, 1182–1185. [Google Scholar] [CrossRef] [PubMed]
- Betts, A.M.; O’Brien, W.T.; Davies, B.W.; Youssef, O.H. A systematic approach to CT evaluation of orbital trauma. Emerg. Radiol. 2014, 21, 511–531. [Google Scholar] [CrossRef] [PubMed]
- Hoffstetter, P.; Schreyer, A.G.; Schreyer, C.I.; Jung, E.M.; Heiss, P.; Zorger, N.; Framme, C. Multidetector CT (MD-CT) in the diagnosis of uncertain open globe injuries. RöFo 2010, 182, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; Brunese, L.; Daniele, S.; Faggian, A.; Guarnieri, G.; Muto, M.; Romano, L. Role of computed tomography in the assessment of intraorbital foreign bodies. Semin. Ultrasound CT MRI 2012, 33, 392–395. [Google Scholar] [CrossRef] [PubMed]
- Kubal, W.S. Imaging of orbital trauma. Radiographics 2008, 28, 1729–1739. [Google Scholar] [CrossRef] [PubMed]
- Winegar, B.A.; Gutierrez, J.E. Imaging of Orbital Trauma and Emergent Non-traumatic Conditions. Neuroimaging Clin. N. Am. 2015, 25, 439–456. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Jilani, M.; Frohman, L.; Baker, S. CT of orbital trauma. Emerg. Radiol. 2004, 10, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Benson, J.C.; Rydberg, C.; DeLone, D.R.; Johnson, M.P.; Geske, J.; Brinjikji, W.; Lanzino, G.; Cloft, H.; Luetmer, P.H. CT angiogram findings in carotid-cavernous fistulas: Stratification of imaging features to help radiologists avoid misdiagnosis. Acta Radiol. 2020, 61, 945–952. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.C.; Liao, T.C.; Yuan, W.H.; Lee, F.L.; Chen, S.J. Management and clinical outcomes of intraocular foreign bodies with the aid of orbital computed tomography. J. Chin. Med. Assoc. 2014, 77, 433–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adesanya, O.O.; Dawkins, D.M. Intraorbital wooden foreign body (IOFB): Mimicking air on CT. Emerg. Radiol. 2007, 14, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Hilbert-Carius, P.; Wurmb, T.; Lier, H.; Fischer, M.; Helm, M.; Lott, C.; Böttiger, B.W.; Bernhard, M. Versorgung von Schwerverletzten: Update der S3-Leitlinie Polytrauma/Schwerverletzten-Behandlung 2016 [Care for severely injured persons: Update of the 2016 S3 guideline for the treatment of polytrauma and the severely injured]. Anaesthesist 2017, 66, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Lendemans, S.; Ruchholtz, S.; German Society of Trauma Surgery (DGU). S3-Leitlinie Polytrauma/Schwerverletzten-Behandlung. Schockraumversorgung [S3 guideline on treatment of polytrauma/severe injuries. Trauma room care]. Unfallchirurg 2012, 115, 14–21. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE-Initiative. Das Strengthening the Reporting of Observational Studies in Epidemiology (STROBE-) Statement [The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting of observational studies]. Internist 2008, 49, 688–693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yaniv, G.; Portnoy, O.; Simon, D.; Bader, S.; Konen, E.; Guranda, L. Revised protocol for whole-body CT for multi-trauma patients applying triphasic injection followed by a single-pass scan on a 64-MDCT. Clin. Radiol. 2013, 68, 668–675. [Google Scholar] [CrossRef] [PubMed]
- Reyes, J.M.; Garciía Vargas, M.F.; Rosenvasser, J.; Arocena, M.A.; Medina, A.J.; Funes, J. Classification and epidemiology of orbital fractures diagnosed by computed tomography. Rev. Argent. Radiol. 2013, 7, 139–146. [Google Scholar]
- Salonen, E.M.; Koivikko, M.P.; Koskinen, S.K. Multidetector computed tomography imaging of facial trauma in accidental falls from heights. Acta Radiol. 2007, 48, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.; Reid, R.R.; Poon, C.S. Multidetector computed tomography of maxillofacial fractures: The key to high-impact radiological reporting. Semin. Ultrasound CT MRI 2012, 33, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Hopper, R.A.; Salemy, S.; Sze, R.W. Diagnosis of midface fractures with CT: What the surgeon needs to know. Radiographics 2006, 26, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Winegar, B.A.; Murillo, H.; Tantiwongkosi, B. Spectrum of critical imaging findings in complex facial skeletal trauma. Radiographics 2013, 33, 3–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chapman, V.M.; Fenton, L.Z.; Gao, D.; Strain, J.D. Facial fractures in children: Unique patterns of injury observed by computed tomography. J. Comput. Assist. Tomogr. 2009, 3, 70–72. [Google Scholar] [CrossRef] [PubMed]
- Yuan, W.H.; Hsu, H.C.; Cheng, H.C.; Guo, W.Y.; Teng, M.M.; Chen, S.J.; Lin, T.C. CT of globe rupture: Analysis and frequency of findings. AJR Am. J. Roentgenol. 2014, 202, 1100–1107, Erratum in AJR Am. J. Roentgenol. 2014, 202, 1396. [Google Scholar] [CrossRef] [PubMed]
- Murali, S.; Davis, C.; McCrea, M.J.; Plewa, M.C. Orbital compartment syndrome: Pearls and pitfalls for the emergency physician. J. Am. Coll. Emerg. Physicians Open 2021, 6, e12372. [Google Scholar] [CrossRef] [PubMed]
- Hrach, C.J.; Quint, D.J. Globe tenting as a result of head trauma. AJNR Am. J. Neuroradiol. 1997, 18, 980–982. [Google Scholar] [CrossRef] [PubMed]
- Dalley, R.W.; Robertson, W.D.; Rootman, J. Globe tenting: A sign of increased orbital tension. AJNR Am. J. Neuroradiol. 1989, 10, 181–186. [Google Scholar] [PubMed]
- Zhu, L.; Liu, B.; Zhong, J. Post-traumatic right carotid-cavernous fistula resulting in symptoms in the contralateral eye: A case report and literature review. BMC Ophthalmol. 2018, 25, 183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cellaigh, P.O.; Ekanaykaee, K.; Beirne, C.J.; Patton, D.W. Diagnosis and management of common maxillofacial injuries in the emergency department. Part 4: Orbital floor and midface fractures. Emerg. Med. J. 2007, 24, 292–293. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | n (%) | |
|---|---|---|
| Sex | male | 806 (76) |
| female | 255 (24) | |
| Age in Years | 0–9 | 6 (0.6) |
| 10–19 | 93 (8.8) | |
| 20–29 | 219 (20.6) | |
| 30–39 | 140 (13.2) | |
| 40–49 | 174 (16.4) | |
| 50–59 | 187 (17.6) | |
| 60–69 | 93 (8.8) | |
| 70–79 | 85 (8.0) | |
| 80–89 | 59 (5.6) | |
| 90–99 | 5 (0.5) | |
| Trauma Mechanism | Road traffic accidents | 581 (54.7) |
| - car (driver/passenger) | 280 (26.4) | |
| - bicyclist | 110 (10.4) | |
| - motorcyclist | 95 (8.9) | |
| - pedestrian | 96 (9.0) | |
| Fall from heights > 3 m | 305 (28.8) | |
| Assault | 40 (3.8) | |
| Miscellaneous | 135 (12.7) |
| n | Included Patients (n = 1061) | Confirmed Orbital Trauma (n = 250) | ||
|---|---|---|---|---|
| % | % | |||
| All orbital injuries | total | 250 | 23.6 | 100.0 |
| Osseous injuries | ||||
| total | 247 | 23.3 | 98.8 | |
| isolated | 149 | 14.0 | 59.6 | |
| Soft tissue injuries | ||||
| total | 101 | 9.5 | 40.4 | |
| isolated | 3 | 0.3 | 1.2 | |
| Combined injuries | total | 98 | 9.2 | 39.2 |
| Type of Fracture | Right Orbit n (%) | Left Orbit n (%) | Total n (%) |
|---|---|---|---|
| single wall | 51 (58.0) | 40 (49.4) | 91 (36.8) |
| two walls | 21 (23.9) | 22 (27.2) | 43 (17.4) |
| three walls | 13 (14.8) | 12 (14.8) | 25 (10.1) |
| four walls | 2 (2.2) | 6 (7.4) | 8 (3.2) |
| four walls and orbital apex | 1 (1.1) | 1 (1.2) | 2 (0.8) |
| bilateral fractures | 78 (31.6) | ||
| total | 88 (35.6) | 81 (32.8) | 247 (100) |
| Location of Soft Tissue Injury | Type of Lesion | n (%) |
|---|---|---|
| Extraocular muscles | 54 (53.5) | |
| dislocation | 45 (44.6) | |
| pierced by bone fragment | 8 (7.9) | |
| intramuscular foreign body | 1 (1.0) | |
| Ocular globe and lens | 38 (37.6) | |
| Deformed globe or vitreous body | 24 (23.8) | |
| rupture of ocular globe | 7 (6.9) | |
| dislocated lens | 6 (5.9) | |
| intraconal foreign body | 1 (1.0) | |
| Optic nerve | 24 (23.8) | |
| elongation | 13 (12.9) | |
| otherwise altered morphology | 10 (9.9) | |
| pierced by foreign body | 1 (1.0) | |
| Orbital vessels | 16 (15.8) | |
| dilated superior ophthalmic vein | 10 (9.9) | |
| direct carotid cavernous fistula | 6 (5.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goelz, L.; Syperek, A.; Heske, S.; Mutze, S.; Hosten, N.; Kirsch, M. Retrospective Cohort Study of Frequency and Patterns of Orbital Injuries on Whole-Body CT with Maxillofacial Multi-Slice CT. Tomography 2021, 7, 373-386. https://doi.org/10.3390/tomography7030033
Goelz L, Syperek A, Heske S, Mutze S, Hosten N, Kirsch M. Retrospective Cohort Study of Frequency and Patterns of Orbital Injuries on Whole-Body CT with Maxillofacial Multi-Slice CT. Tomography. 2021; 7(3):373-386. https://doi.org/10.3390/tomography7030033
Chicago/Turabian StyleGoelz, Leonie, Annika Syperek, Stephanie Heske, Sven Mutze, Norbert Hosten, and Michael Kirsch. 2021. "Retrospective Cohort Study of Frequency and Patterns of Orbital Injuries on Whole-Body CT with Maxillofacial Multi-Slice CT" Tomography 7, no. 3: 373-386. https://doi.org/10.3390/tomography7030033
APA StyleGoelz, L., Syperek, A., Heske, S., Mutze, S., Hosten, N., & Kirsch, M. (2021). Retrospective Cohort Study of Frequency and Patterns of Orbital Injuries on Whole-Body CT with Maxillofacial Multi-Slice CT. Tomography, 7(3), 373-386. https://doi.org/10.3390/tomography7030033







