Incidence and Outcome of Unexpected Non-Cardiac Abnormality on Cardiac Magnetic Resonance Imaging: A Report from Northeastern Thailand
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Cardiovascular Magnetic Resonance (CMR) Scanning Protocol
2.3. CMR Imaging Analysis and Follow-Up Protocol
2.4. Statistical Analysis
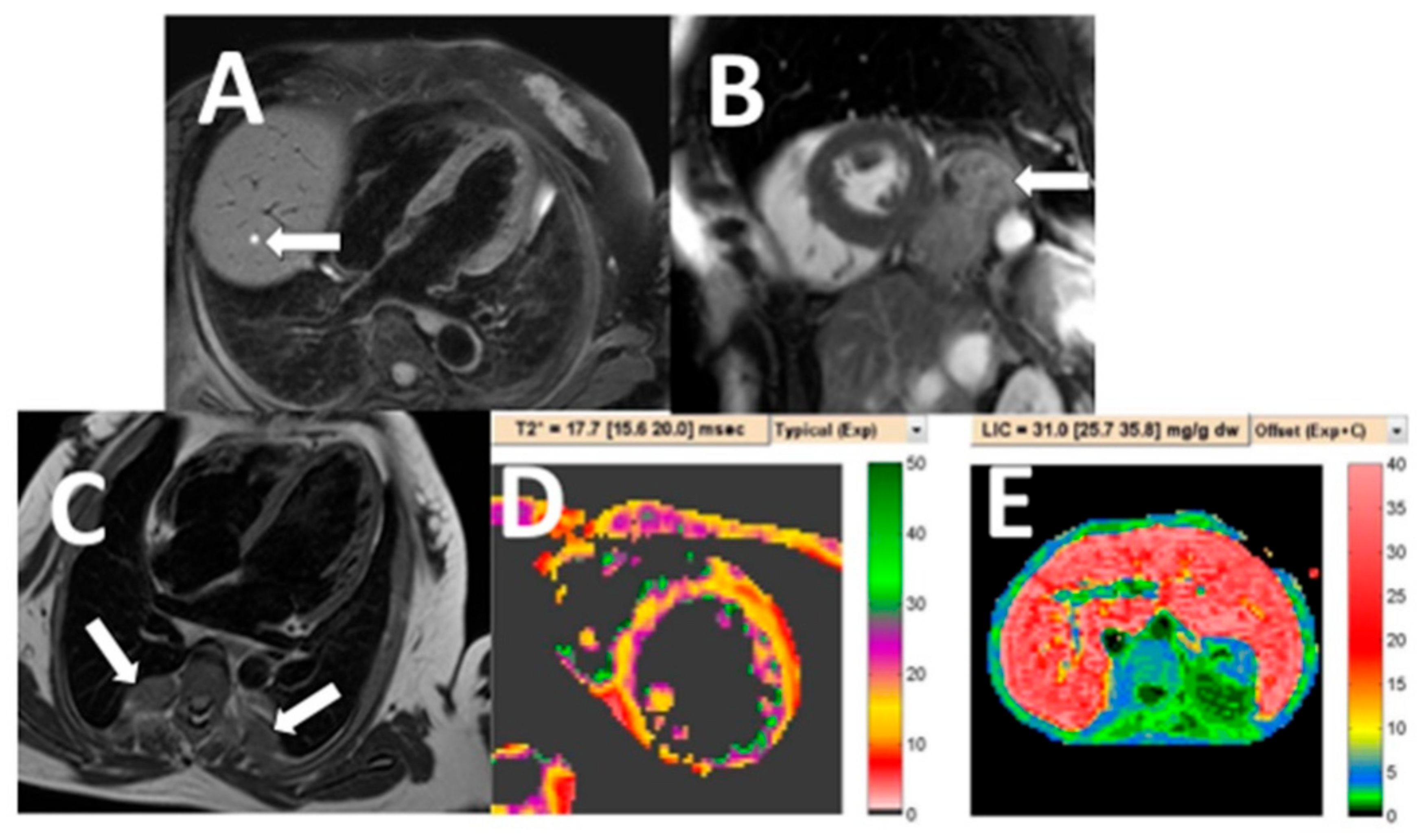
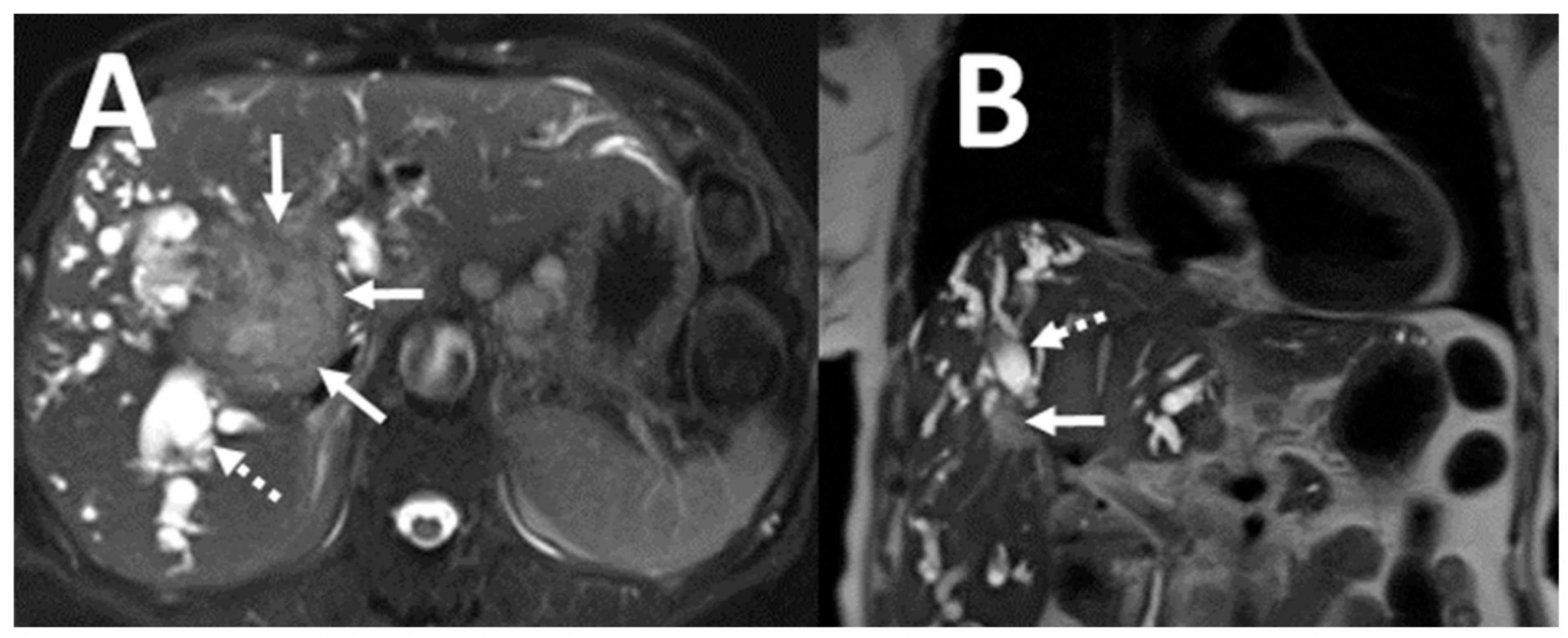
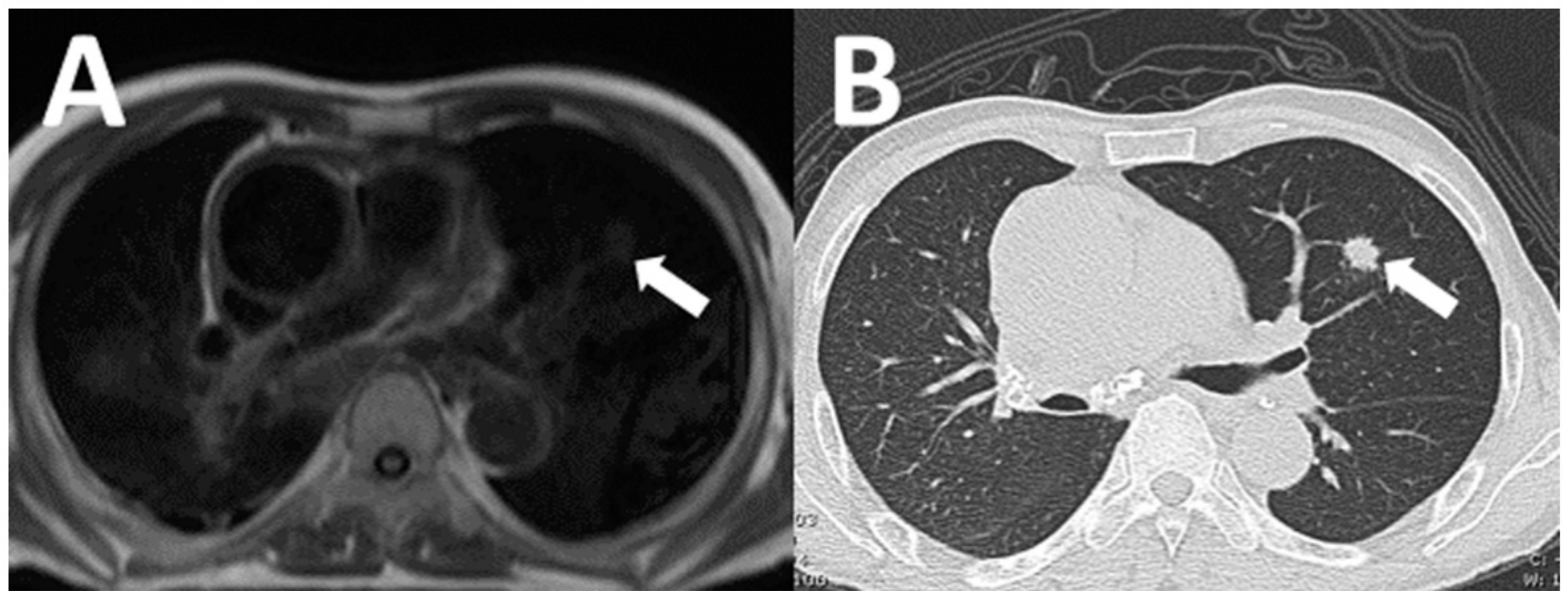
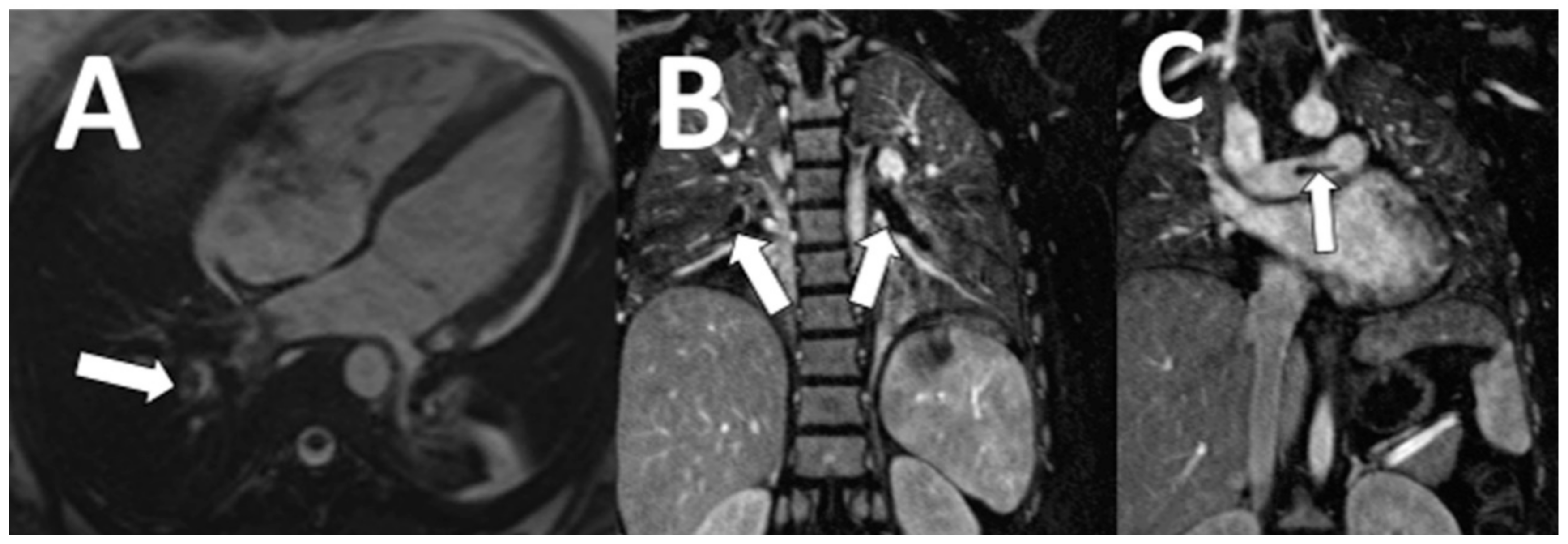
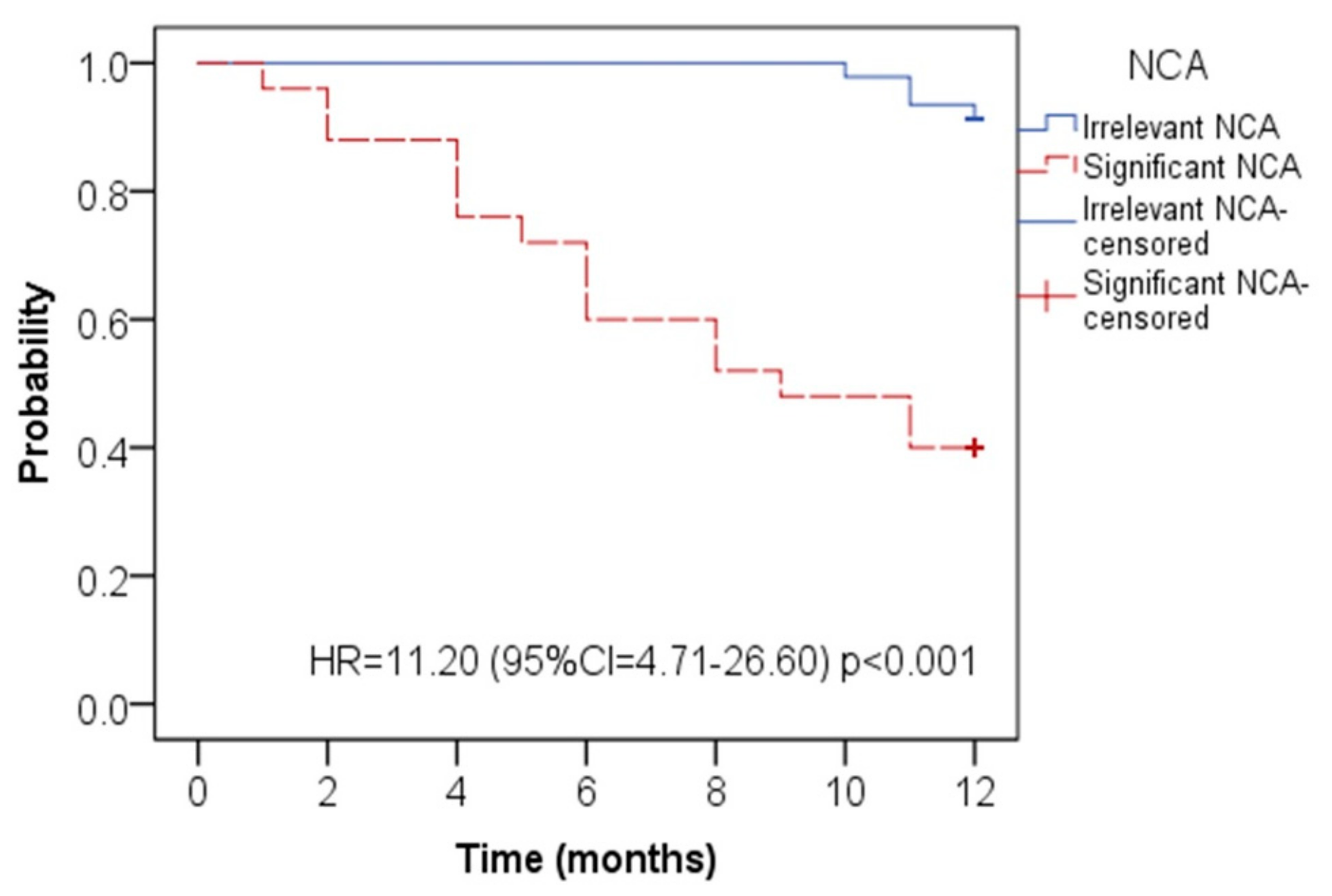
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leiner, T.; Bogaert, J.; Friedrich, M.G.; Mohiaddin, R.; Muthurangu, V.; Myerson, S.; Powell, A.J.; Raman, S.V.; Pennell, D.J. SCMR Position Paper (2020) on clinical indications for cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2020, 22, 76. [Google Scholar] [CrossRef] [PubMed]
- Kramer, C.M.; Barkhausen, J.; Flamm, S.D.; Kim, R.J.; Nagel, E. Society for cardiovascular magnetic resonance board of trustee’s task force on standardized protocols. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J. Cardiovasc. Magn. Reson. 2013, 15, 91. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, J.C.; Lyen, S.M.; Loughborough, W.; Amadu, A.M.; Baritussio, A.; Dastidar, A.G.; Manghat, N.E.; Bucciarelli-Ducci, C. Extracardiac findings in cardiovascular magnetic resonance: What the imaging cardiologist needs to know. J. Cardiovasc. Magn. Reson. 2016, 18, 26. [Google Scholar] [CrossRef] [PubMed]
- Schulz-Menger, J.; Bluemke, D.A.; Bremerich, J.; Flamm, S.D.; Fogel, M.A.; Friedrich, M.G. Standardized image interpretation and post-processing in cardiovascular magnetic resonance: Society of Cardiovascular Magnetic Resonance (SCMR) Board of trustees task force on standardized post procession. J. Cardiovasc. Magn. Reson. 2013, 15, 35. [Google Scholar] [CrossRef] [PubMed]
- Horton, K.M.; Post, W.S.; Blumenthal, R.S.; Fishman, E.K. Prevalence of significant non-cardiac findings on electron-beam computed tomography coronary artery calcium screening examinations. Circulation 2002, 106, 532–534. [Google Scholar] [CrossRef] [PubMed]
- Karkhanis, S.; Patil, S.; Hoey, E.T.; Ganeshan, A. The prevalence and significance of thoracic findings in patients undergoing extended coverage computed tomography for assessment of abdominal aortic aneurysms. Br. J. Radiol. 2016, 89, 1062. [Google Scholar] [CrossRef] [PubMed]
- Mora-Encinas, J.P.; Martin, B.; Montero, J.N.; Monago, R.M.; Romero, A. Prevalence and significance of extracardiac findings in cardiac magnetic resonance imaging. Rev. Argen. Radiol. 2016, 80, 171–177. [Google Scholar]
- Irwin, R.B.; Newton, T.; Peebles, C.; Borg, A.; Clark, D.; Miller, C.; Abidin, N.; Greaves, M.; Schmitt, M. Incidental extracardiac findings on clinical CMR. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Saensa-Ard, S.; Leuangwattanawanit, S.; Senggunprai, L.; Namwat, N.; Kongpeth, S.; Chamgramol, Y.; Loilome, W.; Khansaard, W.; Jusakul, A.; Prawan, A.; et al. Establishment of cholangiocarcinoma cell lines from patients in the endemic area of liver fluke infection in Thailand. Tumor Biol. 2017, 39, 101042311772592. [Google Scholar] [CrossRef] [PubMed]
- Koene, R.J.; Prizment, A.E.; Blaes, A.; Konete, S.H. Shared risk factors in cardiovascular disease and cancer. Circulation 2016, 133, 1104–1114. [Google Scholar] [CrossRef] [PubMed]
- Sripa, B.; Kaewkes, S.; Sithithaworn, P.; Mairiang, E.; Laha, T.; Smout, M.; Pairojkul, C.; Bhudhisawasdi, V.; Tesana, S.; Thinkamrop, B.; et al. Liver fluke induces cholangiocarcinoma. PLoS Med. 2007, 4, e201. [Google Scholar] [CrossRef] [PubMed]
- Uttaravichien, T.; Bhudhisawasdi, V.; Pairojkul, C.; Pungkhem, A. Intrahepatic cholangiocarcinoma in Thailand. J. Hepatobiliary Pancreat. Surg. 1999, 6, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Greulich, S.; Backes, M.; Schumm, J.; Grün, S.; Steubing, H.; Sechtem, U.; Geissler, A.; Mahrholdt, H. Extracardiac findings in cardiovascular MR: Why cardiologists and radiologists should read together. Int. J. Cardiovasc. Imaging 2014, 30, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Dunet, V.; Schwitter, J.; Meuli, R.; Beigelman-Aubry, C. Incidental extracardiac findings on cardiac MR: Systematic review and meta-analysis. J. Magn. Reson. Imaging 2016, 43, 929–939. [Google Scholar] [CrossRef] [PubMed]
- Dunet, V.; Barras, H.; Boulanger, X.; Monney, P.; Qanadli, S.D.; Meuli, R.; Schwitter, J.; Beigelman-Aubry, C. Impact of extracardiac findings during cardiac MR on patient management and outcome. Med. Sci. Monit. 2015, 21, 1288–1296. [Google Scholar] [PubMed]
- Sokolowski, F.C.; Karius, P.; Rodriguez, A.; Lembcke, A.; Wagner, M.; Hamm, B. Extracardiac findings at cardiac MR imaging: a single-centre retrospective study over 14 years. Eur Radiol. 2018, 28, 4102–4110. [Google Scholar] [CrossRef] [PubMed]
| Variable | Patients with NCA (n = 118) | Patients without NCA (n = 264) | p-Value |
|---|---|---|---|
| Age; years (mean ± SD) | 55.6 ± 11.2 | 57.1 ± 14.3 | 0.34 |
| Female | 56 (47.5) | 134 (50.8) | 0.55 |
| Obesity * | 11 (9.3) | 28 (10.6) | 0.77 |
| Diabetes | 30 (25.4) | 65 (24.6) | 0.87 |
| Hypertension | 58 (23.7) | 78 (29.5) | 0.24 |
| Dyslipidemia | 42 (35.6) | 73 (27.7) | 0.12 |
| Smoking history | 10 (8.5) | 24 (9.1) | 0.85 |
| Previous cardiac surgery | 44 (37.3) | 101((38.3) | 0.85 |
| Cardiac MRI indications | |||
| Cardiomyopathy | 40 (33.9) | 92 (34.8) | 0.86 |
| Ischemic heart disease | 38 (32.2) | 80 (30.3) | 0.71 |
| Congenital heart disease | 33 (27.9) | 78 (29.5) | 0.75 |
| Cardiac mass | 4 (3.4) | 8 (3.0) | 0.83 |
| Pericardial disease | 3 (2.6) | 7 (2.4) | 0.91 |
| Non-Cardiac Abnormality (NCA) | n (%) |
|---|---|
| Clinically significant NCA (n = 25) | |
| Malignancy | 18 (72) |
| Cholangiocarcinoma | 7 (28) |
| Lung cancer | 4 (16) |
| Hepatocellular carcinoma | 3 (12) |
| Breast cancer | 1 (4) |
| Renal cell carcinoma | 2 (8) |
| Bone metastasis | 1 (4) |
| Pulmonary thromboembolism | 2 (8) |
| Aortic dissection | 2 (8) |
| Aortic aneurysm | 3 (12) |
| Irrelevant NCA (n = 93) | |
| Simple renal cortical cyst | 36 (38.7) |
| Simple liver cyst | 11 (11.7) |
| Hepatic hemangioma | 2 (2.2) |
| Ascites | 10 (10.7) |
| Splenic cyst | 1 (1.1) |
| Splenomegaly | 4 (4.3) |
| Esophageal dilatation | 6 (6.5) |
| Pleural effusion | 8 (8.6) |
| Pleural plaque | 2 (2.2) |
| Hiatal hernia | 3 (3.2) |
| Thyroid goiter | 4 (4.3) |
| Extramedullary hematopoiesis | 5 (5.4) |
| Thoracic spine hemangioma | 1 (1.1) |
| One-Year Mortality | Clinically Significant NCA | Irrelevant NCA | p-Value |
|---|---|---|---|
| Death | 15 (60) | 8 (9.4) | 0.02 * |
| Survived | 10 (40) | 85 (90.6) | 0.0017 * |
| One-Year Mortality | Patient without NCA | Patient with NCA | p-Value |
| Death | 24 (9.1) | 23 (19.5) | 0.31 |
| Survived | 240 (90.9) | 95 (80.5) | 0.0085 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chaosuwannakit, N.; Makarawate, P. Incidence and Outcome of Unexpected Non-Cardiac Abnormality on Cardiac Magnetic Resonance Imaging: A Report from Northeastern Thailand. Tomography 2021, 7, 202-209. https://doi.org/10.3390/tomography7020018
Chaosuwannakit N, Makarawate P. Incidence and Outcome of Unexpected Non-Cardiac Abnormality on Cardiac Magnetic Resonance Imaging: A Report from Northeastern Thailand. Tomography. 2021; 7(2):202-209. https://doi.org/10.3390/tomography7020018
Chicago/Turabian StyleChaosuwannakit, Narumol, and Pattarapong Makarawate. 2021. "Incidence and Outcome of Unexpected Non-Cardiac Abnormality on Cardiac Magnetic Resonance Imaging: A Report from Northeastern Thailand" Tomography 7, no. 2: 202-209. https://doi.org/10.3390/tomography7020018
APA StyleChaosuwannakit, N., & Makarawate, P. (2021). Incidence and Outcome of Unexpected Non-Cardiac Abnormality on Cardiac Magnetic Resonance Imaging: A Report from Northeastern Thailand. Tomography, 7(2), 202-209. https://doi.org/10.3390/tomography7020018





