Morphometric Analysis of Subaxial Cervical Vertebra Pedicles in the Turkish Population
Abstract
1. Introduction
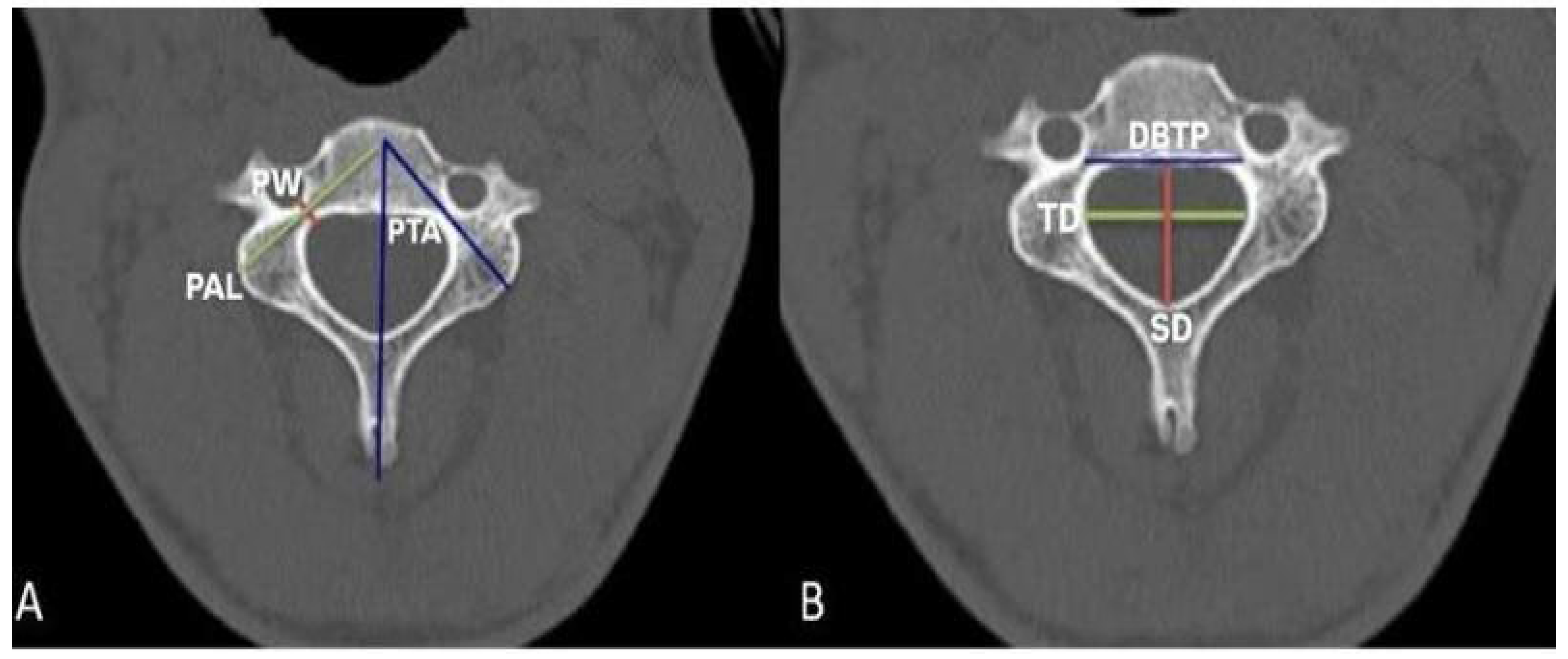
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Acer, N. Basic Anatomy for Health Sciences, 2nd ed.; Istanbul Medical Bookstore: Istanbul, Turkey, 2022. [Google Scholar]
- Arıncı, K.; Elhan, A. Anatomy, 7th ed.; Güneş Medical Bookstores: Ankara, Turkey, 2020. [Google Scholar]
- Şahin, B. Illustrated Basic Anatomy for Health Sciences; Istanbul Medical Bookstores: Istanbul, Turkey, 2019. [Google Scholar]
- Saluja, S.; Patil, S.; Vasudeva, N. Morphometric Analysis of Sub-axial Cervical Vertebrae and Its Surgical Implications. J. Clin. Diagn. Res. 2015, 9, AC01–AC04. [Google Scholar] [CrossRef]
- Sureka, B.; Mittal, A.; Mittal, M.K.; Agarwal, K.; Sinha, M.; Thukral, B.B. Morphometric analysis of cervical spinal canal diameter, transverse foramen, and pedicle width using computed tomography in Indian population. Neurol. India 2018, 66, 454–458. [Google Scholar] [CrossRef]
- Özbağ, D. Human Anatomy; İstanbul Medical Bookstores: Istanbul, Turkey, 2020. [Google Scholar]
- Rao, R.D.; Marawar, S.V.; Stemper, B.D.; Yoganandan, N.; Shender, B.S. Computerized tomographic morphometric analysis of subaxial cervical spine pedicles in young asymptomatic volunteers. J. Bone Jt. Surg. Am. 2008, 90, 1914–1921. [Google Scholar] [CrossRef]
- Tomasino, A.; Parikh, K.; Koller, H.; Zink, W.; Tsiouris, A.J.; Steinberger, J.; Härtl, R. The vertebral artery and the cervical pedicle: Morphometric analysis of a critical neighborhood. J. Neurosurg. Spine 2010, 13, 52–60. [Google Scholar] [CrossRef]
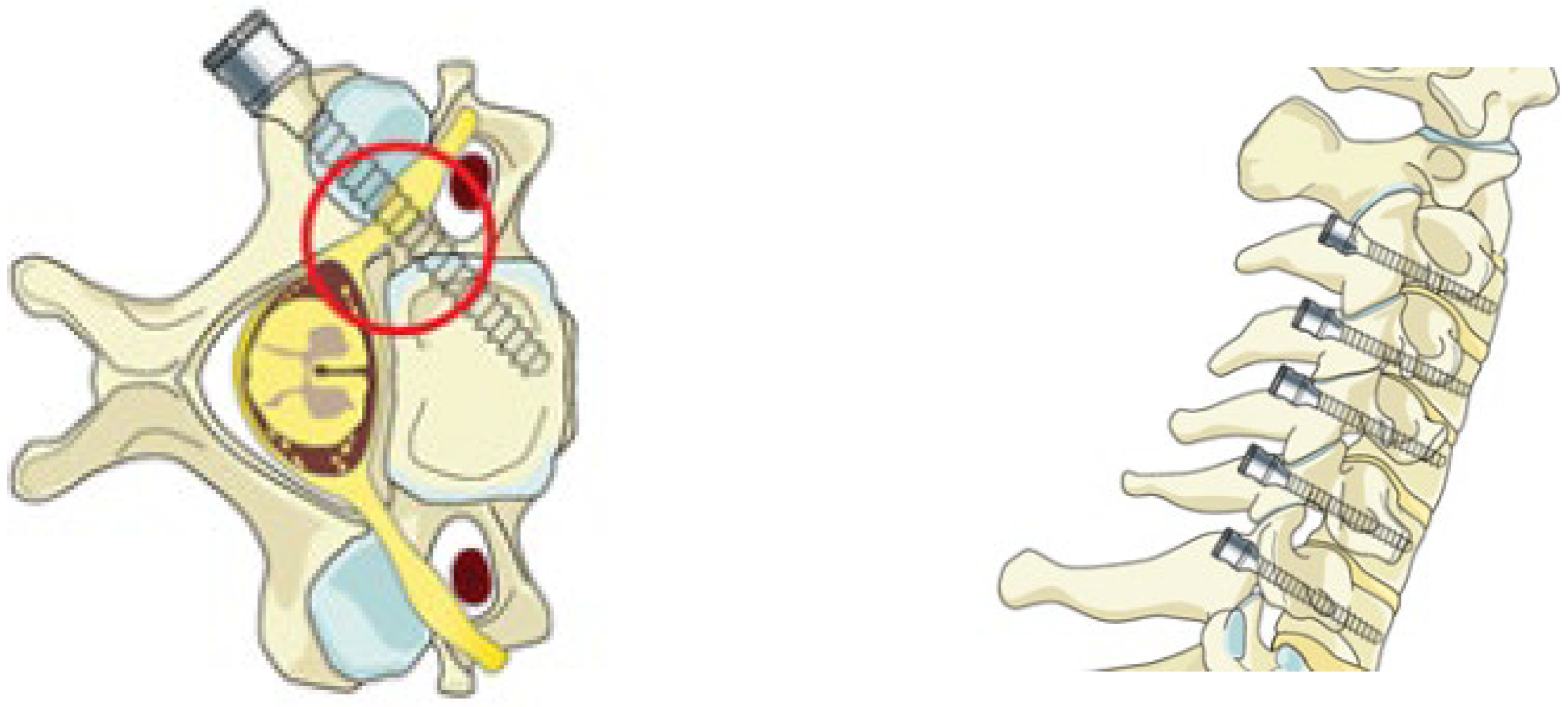
- Surgery Reference. Pedicle Screw Insertion in the Cervical Spine. Available online: https://images.app.goo.gl/Az46ESsrPwdE9gDH8 (accessed on 23 June 2023).
- Alsaleh, K.; Essbaiheen, F.; Aldosari, K.; Alsubei, B.; Alabdulkareeem, M. Morphometric Analysis of Subaxial Cervical Spine Pedicles in a Middle Eastern Population. Int. J. Spine Surg. 2021, 15, 413–417. [Google Scholar] [CrossRef]
- Srivastava, A.; Nanda, G.; Mahajan, R.; Nanda, A.; Batra, S.; Mishra, N.; Pandita, N.; Chhabra, H.S. Feasibility of Sub-Axial Cervical Laminar Screws, Including C7, in the Indian Population: A Study on 50 Patients Using Computed Tomography-Based Morphometry Measurements. Asian Spine J. 2019, 13, 7–12. [Google Scholar] [CrossRef]
- Güler, H.; Esen, E.E.; Balcıoğlu, E.; Göktepe, Ö.; Yılmaz, H.; Yay, A.H.; Nisari, M.; Al, Ö.; Uçar, S.; Ekinci, H.K.G.; et al. Bone development in offspring of pregnant rats treated with carbamazepine: Evaluation by three different methods. Epilepsia 2022, 63, 3066–3077. [Google Scholar] [CrossRef]
- Abumi, K.; Itoh, H.; Taneichi, H.; Kaneda, K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: Description of the techniques and preliminary report. J. Spinal Disord. 1994, 7, 19–28. [Google Scholar] [CrossRef]
- Patwardhan, A.R.; Nemade, P.S.; Bhosale, S.K.; Srivastava, S.K. Computed tomography-based morphometric analysis of cervical pedicles in Indian population: A pilot study to assess feasibility of transpedicular screw fixation. J. Postgrad. Med. 2012, 58, 119–122. [Google Scholar] [CrossRef]
- Munusamy, T.; Thien, A.; Anthony, M.G.; Bakthavachalam, R.; Dinesh, S.K. Computed tomographic morphometric analysis of cervical pedicles in a multi-ethnic Asian population and relevance to subaxial cervical pedicle screw fixation. Eur. Spine J. 2015, 24, 120–126. [Google Scholar] [CrossRef]
- Canberk, İ. Morphometric Measurements Made by Computerized Tomography on Lower Cervical Vertebral Pedicles; Afyon Kocatepe University: Afyonkarahisar, Turkey, 2017; pp. 17–19. [Google Scholar]
- Farooque, K.; Yadav, R.; Chowdhury, B.; Gamanagatti, S.; Kumar, A.; Meena, P.K. Computerized Tomography-Based Morphometric Analysis of Subaxial Cervical Spine Pedicle in Asymptomatic Indian Population. Int. J. Spine Surg. 2018, 12, 112–120. [Google Scholar] [CrossRef]
- Westermann, L.; Spemes, C.; Eysel, P.; Simons, M.; Scheyerer, M.J.; Siewe, J.; Baschera, D. Computer tomography-based morphometric analysis of the cervical spine pedicles C3–C7. Acta Neurochir. 2018, 160, 863–871. [Google Scholar] [CrossRef]
- Atalar, K. Evaluation of Cervical Vertebrae Pedicle and Surrounding Structure Morphologies to Guide Transpedicular Screwing Technique Using 3-Dimensional Reconstruction Method; Gazi University Institute of Health Sciences: Ankara, Turkey, 2018; pp. 33–35. [Google Scholar]
| Levels | G | PWR | PWL | PTAR | PTAL | PALR | PALL | TD | SD | DBTP |
|---|---|---|---|---|---|---|---|---|---|---|
| C3 | M | 4.76 ± 0.72 | 4.61 ± 0.70 | 48.35 ± 5.31 | 47.71 ± 3.48 | 30.74 ± 2.14 | 30.86 ± 1.94 | 24.63 ± 1.44 | 15.10 ± 1.76 | 25.85 ± 1.10 |
| F | 4.11 ± 0.63 | 3.91 ± 0.58 | 46.40 ± 4.11 | 47.08 ± 3.59 | 29.70 ± 2.16 | 27.79 ± 1.49 | 22.73 ± 1.19 | 13.99 ± 1.48 | 24.13 ± 0.84 | |
| GN | 4.44 ± 0.74 | 4.26 ± 0.73 | 47.38 ± 4.81 | 47.39 ± 3.52 | 30.22 ± 2.19 | 29.83 ± 20.01 | 23.68 ± 1.62 | 14.55 ± 1.70 | 24.99 ± 1.30 | |
| p | 0.001 | <0.001 | 0.117 | 0.491 | 0.065 | <0.001 | <0.001 | 0.010 | <0.001 | |
| C4 | M | 4.85 ± 0.71 | 4.80 ± 0.80 | 50.61 ± 4.42 | 50.81 ± 3.69 | 30.78 ± 1.96 | 30.88 ± 2.05 | 25.79 ± 1.33 | 14.19 ± 1.50 | 26.69 ± 1.26 |
| F | 4.29 ± 0.80 | 4.13 ± 0.73 | 48.74 ± 3.99 | 49.65 ± 3.37 | 29.35 ± 2.09 | 24.79 ± 1.33 | 24.25 ± 1.19 | 13.55 ± 1.63 | 25.26 ± 1.25 | |
| GN | 4.57 ± 0.80 | 4.46 ± 0.83 | 49.68 ± 4.28 | 50.23 ± 3.55 | 30.06 ± 2.13 | 29.80 ± 2.07 | 25.02 ± 1.47 | 13.87 ± 1.58 | 25.97 ± 1.44 | |
| p | 0.005 | 0.001 | 0.091 | 0.209 | 0.009 | <0.001 | <0.001 | 0.115 | <0.001 | |
| C5 | M | 5.25 ± 0.77 | 5.18 ± 0.77 | 49.04 ± 3.96 | 50.31 ± 4.14 | 32.54 ± 1.90 | 32.49 ± 1.95 | 27.25 ± 1.79 | 14.98 ± 1.69 | 27.84 ± 1.35 |
| F | 4.61 ± 0.67 | 4.44 ± 0.72 | 48.93 ± 4.32 | 50.60 ± 4.25 | 30.31 ± 1.95 | 29.29 ± 1.62 | 25.39 ± 1.57 | 13.73 ± 1.72 | 25.82 ± 1.16 | |
| GN | 4.93 ± 0.78 | 4.81 ± 0.83 | 48.99 ± 4.11 | 50.45 ± 4.16 | 31.42 ± 2.21 | 30.89 ± 2.40 | 26.32 ± 1.91 | 14.36 ± 1.81 | 26.83 ± 1.61 | |
| p | 0.001 | <0.001 | 0.920 | 0.794 | <0.001 | <0.001 | <0.001 | 0.006 | <0.001 | |
| C6 | M | 5.59 ± 0.77 | 5.36 ± 0.73 | 46.77 ± 5.53 | 46.38 ± 5.30 | 33.78 ± 2.39 | 33.52 ± 2.54 | 27.54 ± 1.83 | 15.96 ± 2.00 | 29.24 ± 1.77 |
| F | 4.65 ± 0.90 | 4.50 ± 0.65 | 44.24 ± 4.60 | 45.88 ± 3.64 | 31.24 ± 2.25 | 30.77 ± 2.41 | 25.55 ± 1.77 | 14.47 ± 1.86 | 26.69 ± 1.46 | |
| GN | 5.12 ± 0.96 | 4.93 ± 0.81 | 45.01 ± 5.10 | 46.13 ± 4.51 | 32.51 ± 2.63 | 32.15 ± 2.82 | 26.54 ± 2.05 | 15.21 ± 2.06 | 27.97 ± 2.06 | |
| p | <0.001 | <0.001 | 0.251 | 0.671 | <0.001 | <0.001 | <0.001 | 0.004 | <0.001 | |
| C7 | M | 6.31 ± 10.89 | 6.22 ± 0.93 | 40.74 ± 4.56 | 41.29 ± 5.37 | 35.35 ± 3.03 | 34.92 ± 2.72 | 2.85 ± 1.90 | 16.65 ± 2.35 | 30.35 ± 1.60 |
| F | 5.39 ± 0.83 | 5.45 ± 0.65 | 34.97 ± 4.37 | 38.74 ± 2.91 | 31.97 ± 3.34 | 31.66 ± 3.13 | 24.65 ± 1.81 | 14.37 ± 1.87 | 28.44 ± 1.35 | |
| GN | 5.85 ± 0.97 | 5.84 ± 0.89 | 37.85 ± 5.30 | 40.02 ± 4.47 | 33.66 ± 3.59 | 33.83 ± 3.35 | 25.75 ± 2.15 | 15.51 ± 2.40 | 29.39 ± 1.76 | |
| p | <0.001 | <0.001 | <0.001 | 0.025 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| ETHNICITY | AGE/ GENDER | PW | PTA | PAL | TD | SD | |
|---|---|---|---|---|---|---|---|
| ABUMI, 1994 [13] | 15–80/ 12M-1F | 30–40 | |||||
| RAO, 2008 [7] | North American | average 25/ 63M-35F | M-F C3 5.8–4.8 C4 6.0–5.0 C5 6.3–5.2 C6 6.5–5.7 C7 7.6–6.5 | M-F C3 47.4–46.6 C4 47.8–47.8 C5 45.9–46.9 C6 41.8–42.5 C7 33.8–33.0 | M-F C3 34.3–30.9 C4 33.7–30.3 C5 34.2–30.9 C6 34.1–30.6 C7 32.6–28.9 | ||
| PATWARDHAN, 2012 [14] | Indian | -/27M,F | M-F C3 5.3–4.6 C4 5.3–4.7 C5 5.6–4.7 C6 5.6–5.3 C7 6.1–5.6 | ||||
| MUNUSAMY, 2015 [15] | Multiracial Asia (33 Chinese, 11 Malay, 6 Indian) | average 38.5 (21–70)/ 31M-19F | M-F C3 5.74–4.75 C4 5.70–4.77 C5 6.07–5.18 C6 6.42–5.45 C7 7.07–6.29 | M-F C3 45.7–46.7 C4 48.4–48.8 C5 47.9–47.6 C6 44.0–44.9 C7 38.2–37.8 | |||
| CANBERK, 2017 [16] | Turkish | 18–96/ 54M-46F | RIGHT M-F C3 4.22–3.58 C4 4.11–3.55 C5 4.91–3.92 C6 5.26–4.70 C7 6.03–5.10 LEFT M-F C3 4.31–3.35 C4 4.40–3.39 C5 4.77–4.34 C6 5.37–4.65 C7 5.99–4.75 | RIGHT M-F C3 36.14–39.25 C4 37.74–38.94 C5 35.34–36.31 C6 33.36–33.73 C7 30.99–30.57 LEFT M-F C3 39.44–38.46 C4 41.68–43.63 C5 38.87–38.89 C6 38.91–40.59 C7 33.29–33.51 | M-F C3 23.98–23.06 C4 25.02–24.41 C5 25.56–25.29 C6 26.18–25.35 C7 25.50–23.60 | M-F C3 15.23–12.78 C4 14.40–12.47 C5 14.76–13.05 C6 15.12–14.19 C7 15.02–14.03 | |
| FAROOQUE, 2018 [17] | Indian | E-Average 29.3 F-Average 31.3/ 50M-50F | RIGHT M-F C3 4.72–4.37 C4 5.00–4.60 C5 5.49–4.83 C6 5.79–5.00 C7 6.10–5.47 LEFT M-F C3 4.74–4.30 C4 5.08–4.61 C5 5.44–4.80 C6 5.70–5.08 C7 6.00–5.42 | RIGHT M-F C3 45.01–44.02 C4 43.40–41.92 C5 41.60–40.26 C6 39.80–38.42 C7 37.72–36.58 LEFT M-F C3 44.94–44.00 C4 43.80–41.94 C5 41.55–40.02 C6 39.20–38.28 C7 37.63–36.64 | RIGHT M-F C3 30.29–28.89 C4 30.76–29.46 C5 31.52–30.41 C6 32.61–31.78 C7 34.23–32.33 LEFT M-F C3 30.32–28.90 C4 30.84–29.59 C5 31.67–30.60 C6 32.41–31.81 C7 33.19–32.43 | ||
| WESTERMANN, 2018 [18] | Caucasian | E-Average 58 F-Average 57/ 52M-48F | RIGHT M-F C3 4.99–4.34 C4 5.27–4.38 C5 5.50–4.84 C6 6.12–5.16 C7 6.73–6.00 LEFT M-F C3 4.88–4.08 C4 5.13–4.38 C5 5.59–5.03 C6 5.99–5.18 C7 6.87–6.10 | RIGHT M-F C3 44.54–45.27 C4 48.37–47.64 C5 47.38–47.34 C6 43.55–43.46 C7 35.72–35.43 LEFT M-F C3 44.72–45.26 C4 47.95–47.21 C5 47.41–45.90 C6 43.36–41.77 C7 34.79–34.40 | RIGHT M-F C3 32.47–30.51 C4 31.76–29.72 C5 33.45–31.05 C6 35.26–31.13 C7 34.74–31.17 LEFT M-F C3 32.41–30.07 C4 31.69–29.20 C5 32.72–30.62 C6 34.48–31.31 C7 34.49–30.72 | ||
| ATALAR, 2018 [19] | Turkish | 18–30, 31–50, 51+/ 41M-59F | RIGHT M-F C3 40.80–42.00 C4 44.83–44.90 C5 44.62–42.06 C6 38.13–36.72 C7 28.57–27.40 LEFT M-F C3 43.00–42.87 C4 46.55–44.72 C5 44.45–44.42 C6 39.46–38.31 C7 29.37–30.01 | RIGHT M-F C3 17.8–25.4 C4 17.8–25.7 C5 18.9–25.2 C6 19.1–22.4 C7 17.0–19.9 LEFT M-F C3 17.6–26.2 C4 17.12–27 C5 17.6–25.2 C6 18.2–24.6 C7 17.4–22.6 | |||
| ALSALEH, 2021 [10] | Middle East | average 40 (18–92)/ 154M-116F | C3 4.4 C4 4.4 C5 4.8 C6 5 C7 6.1 | C3 44.1 C4 46.7 C5 47.3 C6 44.2 C7 35.5 | |||
| PRESENT STUDY, 2023 | Turkish | 18–45/ 30M-30F | RIGHT M-F C3 4.76–4.11 C4 4.85–4.29 C5 5.25–4.61 C6 5.59–4.65 C7 6.31–5.39 LEFT M-F C3 4.61–3.91 C4 4.80–4.13 C5 5.18–4.44 C6 5.36–4.50 C7 6.22–5.45 | RIGHT M-F C3 48.35–46.40 C4 50.61–48.74 C5 49.04–48.93 C6 45.77–44.24 C7 40.74–34.98 LEFT M-F C3 47.71–47.08 C4 50.81–49.65 C5 50.31–50.60 C6 46.38–45.88 C7 41.29–38.73 | RIGHT M-F C3 30.74–29.70 C4 30.78–29.35 C5 32.54–30.31 C6 33.78–31.25 C7 35.35–31.98 LEFT M-F C3 30.86–28.79 C4 30.88–28.71 C5 32.49–29.29 C6 33.52–30.78 C7 34.94–31.66 | M-F C3 24.63–22.73 C4 25.79–24.25 C5 27.25–25.39 C6 27.54–25.55 C7 28.85–24.65 | M-F C3 15.10–13.99 C4 14.19–13.55 C5 14.98–13.73 C6 15.96–14.47 C7 16.65–14.37 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batir, H.N.T.; Güler, H.; Arpaçay, B.K.; Ökçesiz, İ.; Dönmez, H.; Kahriman, G. Morphometric Analysis of Subaxial Cervical Vertebra Pedicles in the Turkish Population. Tomography 2025, 11, 79. https://doi.org/10.3390/tomography11070079
Batir HNT, Güler H, Arpaçay BK, Ökçesiz İ, Dönmez H, Kahriman G. Morphometric Analysis of Subaxial Cervical Vertebra Pedicles in the Turkish Population. Tomography. 2025; 11(7):79. https://doi.org/10.3390/tomography11070079
Chicago/Turabian StyleBatir, Hande Nur Taşdemir, Hatice Güler, Burcu Kamaşak Arpaçay, İzzet Ökçesiz, Halil Dönmez, and Güven Kahriman. 2025. "Morphometric Analysis of Subaxial Cervical Vertebra Pedicles in the Turkish Population" Tomography 11, no. 7: 79. https://doi.org/10.3390/tomography11070079
APA StyleBatir, H. N. T., Güler, H., Arpaçay, B. K., Ökçesiz, İ., Dönmez, H., & Kahriman, G. (2025). Morphometric Analysis of Subaxial Cervical Vertebra Pedicles in the Turkish Population. Tomography, 11(7), 79. https://doi.org/10.3390/tomography11070079





