Association between the Thickness of Lumbar Subcutaneous Fat Tissue and the Presence of Hernias in Adults with Persistent, Non-Traumatic Low Back Pain
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Sample Selection
2.4. Image Mode
2.5. Subcutaneous Fatty Tissue Thickness Measurement
2.6. Statistical Analysis
3. Results
3.1. Age and Subcutaneous Fatty Tissue Thickness of the Participants
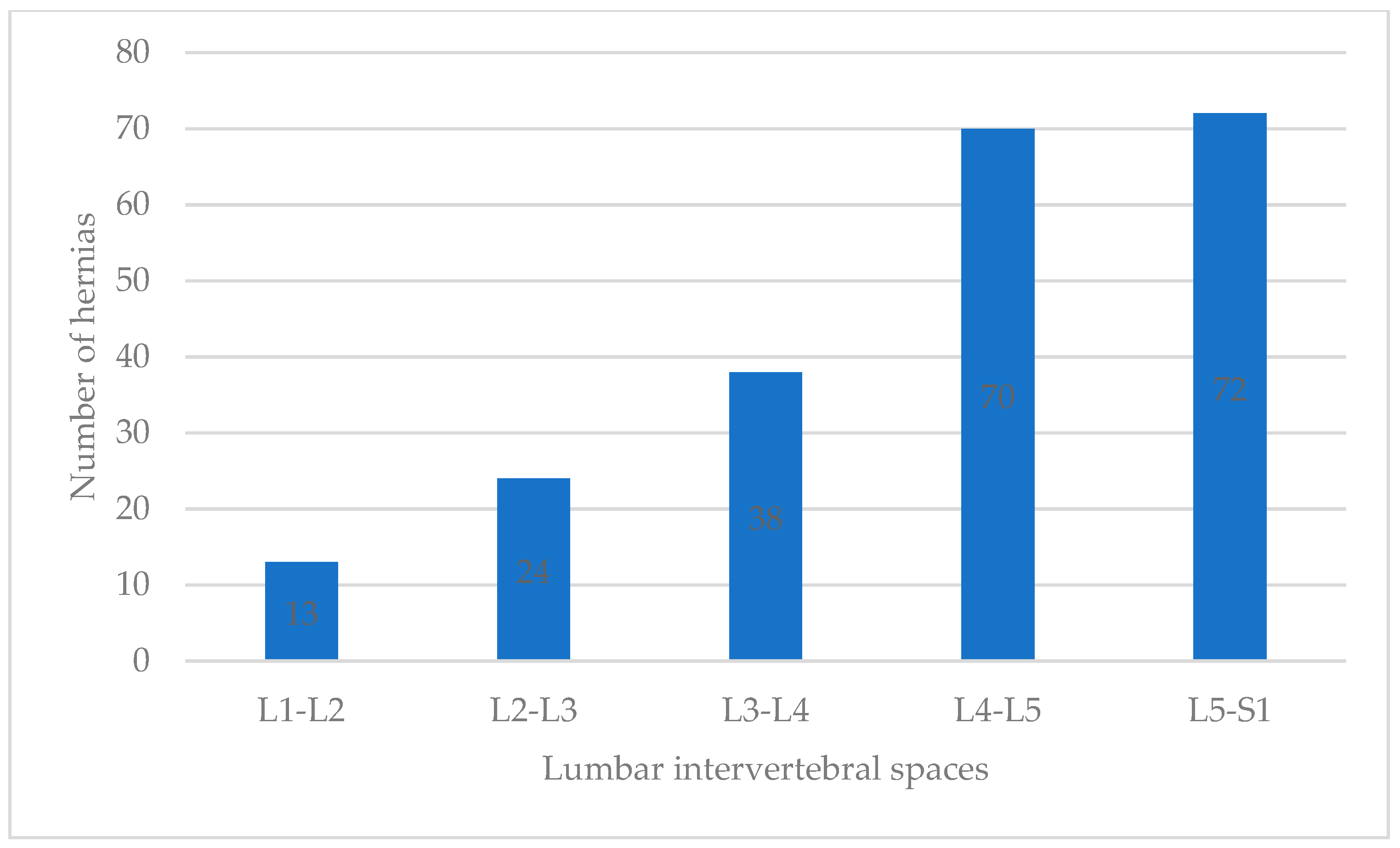
3.2. Number of Hernias in Participants
3.3. Association Analysis
3.4. Specificity and Sensitivity of LSFTT with Hernia Presence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ota, Y.; Connolly, M.; Srinivasan, A.; Kim, J.; Capizzano, A.A.; Moritani, T. Mechanisms and Origins of Spinal Pain: From Molecules to Anatomy, with Diagnostic Clues and Imaging Findings. Radiographics 2020, 40, 1163–1181. [Google Scholar] [CrossRef] [PubMed]
- Hoy, D.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Bain, C.; Williams, G.; Smith, E.; Vos, T.; Barendregt, J.; et al. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014, 73, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Kraychete, D.C.; Sakata, R.K.; Issy, A.M.; Bacellar, O.; Santos-Jesus, R.; Carvalho, E.M. Serum cytokine levels in patients with chronic low back pain due to herniated disc: Analytical cross-sectional study. Sao Paulo Med. J. 2010, 128, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Onyemaechi, N.O.; Anyanwu, G.E.; Obikili, E.N.; Onwuasoigwe, O.; Nwankwo, O.E. Impact of overweight and obesity on the musculoskeletal system using lumbosacral angles. Patient Prefer. Adherence 2016, 10, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Li, X.; Wu, W. Association between Overweight or Obesity and Lumbar Disk Diseases: A Meta-Analysis. J. Spinal Disord. Tech. 2015, 28, 370–376. [Google Scholar] [CrossRef]
- Fotakopoulos, G.; Makris, D.; Kotlia, P.; Tzerefos, C.; Fountas, K. Recurrence Is Associated With Body Mass Index in Patients Undergoing a Single-Level Lumbar Disc Herniation Surgery. J. Clin. Med. Res. 2018, 10, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Kittiskulnam, P.; Johansen, K.L. The obesity paradox: A further consideration in dialysis patients. Semin. Dial. 2019, 32, 485–489. [Google Scholar] [CrossRef]
- Güleç, İ.; Karagöz Güzey, F. The importance of subcutaneous tissue thickness for the occurrence of surgical site infection after lumbar disc surgery. J. Turk. Spinal Surg. 2020, 31, 245–250. [Google Scholar] [CrossRef]
- Özcan-Ekşi, E.E.; Kara, M.; Berikol, G.; Orhun, Ö.; Turgut, V.U.; Ekşi, M.Ş. A new radiological index for the assessment of higher body fat status and lumbar spine degeneration. Skelet. Radiol. 2022, 51, 1261–1271. [Google Scholar] [CrossRef]
- Berikol, G.; Ekşi, M.Ş.; Aydın, L.; Börekci, A.; Özcan-Ekşi, E.E. Subcutaneous fat index: A reliable tool for lumbar spine studies. Eur. Radiol. 2022, 32, 6504–6513. [Google Scholar] [CrossRef]
- Kızılgöz, V. The relationship between dorsal subcutaneous fat tissue thickness and lumbar disc herniation: A magnetic resonance imaging-based study. Curr. Res. MRI 2022, 1, 38–41. [Google Scholar] [CrossRef]
- Barquera, S.; Hernández-Barrera, L.; Trejo-Valdivia, B.; Shamah, T.; Campos-Nonato, I.; Rivera-Dommarco, J. Obesidad en México, prevalencia y tendencias en adultos. Ensanut 2018-19 [Obesity in Mexico, prevalence andtrends in adults. Ensanut 2018-19]. Salud Pública México 2020, 62, 682–692. (In Spanish) [Google Scholar] [CrossRef]
- Dávila-Torres, J.; González-Izquierdo, J.J.; Barrera-Cruz, A. Panorama de la obesidad en México [Obesity in Mexico]. Rev. Med. Inst. Mex. Seguro Soc. 2015, 53, 240–249. (In Spanish) [Google Scholar]
- Kızılgöz, V.; Aydın, S.; Karavaş, E.; Kantarcı, M.; Kahraman, Ş. Are paraspinal muscle quantity, lumbar indentation value, and subcutaneous fat thickness related to disc degeneration? An MRI-based study. Radiography 2023, 29, 428–435. [Google Scholar] [CrossRef]
- Urits, I.; Burshtein, A.; Sharma, M.; Testa, L.; Gold, P.A.; Orhurhu, V.; Viswanath, O.; Jones, M.R.; Sidransky, M.A.; Spektor, B.; et al. Low Back Pain, a Comprehensive Review: Pathophysiology, Diagnosis, and Treatment. Curr. Pain Headache Rep. 2019, 23, 23. [Google Scholar] [CrossRef]
- Yang, H.; Liu, H.; Li, Z.; Zhang, K.; Wang, J.; Wang, H.; Zheng, Z. Low back pain associated with lumbar disc herniation: Role of moderately degenerative disc and annulus fibrous tears. Int. J. Clin. Exp. Med. 2015, 8, 1634–1644. [Google Scholar] [PubMed]
- Takatalo, J.; Karppinen, J.; Taimela, S.; Niinimäki, J.; Laitinen, J.; Sequeiros, R.B.; Samartzis, D.; Korpelainen, R.; Näyhä, S.; Remes, J.; et al. Association of abdominal obesity with lumbar disc degeneration—A magnetic resonance imaging study. PLoS ONE 2013, 8, e56244. [Google Scholar] [CrossRef] [PubMed]
- Frigolet, M.E.; Dong-Hoon, K.; Canizales-Quinteros, S.; Gutiérrez-Aguilar, R. Obesity, adipose tissue, and bariatric surgery. Bol. Med. Hosp. Infant. Mex. 2020, 77, 3–14. [Google Scholar] [CrossRef]
- Sevil, O.K.; Beyhan, M. Relationship between lumbar subcutaneous adipose tissue thickness and spinopelvic parameters. Cukurova Med. J. 2020, 45, 1238–1245. [Google Scholar] [CrossRef]
- Yazici, A.; Yerlikaya, T. The relationship between the degeneration and asymmetry of the lumbar multifidus and erector spinae muscles in patients with lumbar disc herniation with and without root compression. J. Orthop. Surg. Res. 2022, 17, 541. [Google Scholar] [CrossRef] [PubMed]
- Mo, A.Z.; Gjolaj, J.P. Axial Low Back Pain in Elite Athletes. Clin. Sports Med. 2021, 40, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Teichtahl, A.J.; Urquhart, D.M.; Wang, Y.; Wluka, A.E.; Wijethilake, P.; O’Sullivan, R.; Cicuttini, F.M. Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J. 2015, 15, 1593–1601. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.S.; Doan, N.; Shabani, S.; Baisden, J.; Wolfla, C.; Paskoff, G.; Shender, B.; Stemper, B. Upright magnetic resonance imaging of the lumbar spine: Back pain and radiculopathy. J. Craniovertebral Junction Spine 2016, 7, 31–37. [Google Scholar] [CrossRef]


| Variable Description Mean | General | Female | Male | |||
|---|---|---|---|---|---|---|
| Mean | Std. Dev. | Mean | Std. Dev. | Mean | Std. Dev. | |
| Age (years) | 47.05 | 1.55 | 48.77 | 1.50 | 45.31 | 1.58 |
| Thickness (mm) | ||||||
| L1-L2 LSFTT | 26 | 44 | 23 | 42 | 28 | 45 |
| L2-L3 LSFTT | 34 | 48 | 31 | 46 | 38 | 49 |
| L3-L4 LSFTT | 52 | 50 | 49 | 50 | 55 | 50 |
| L4-L5 LSFTT | 77 | 42 | 79 | 41 | 74 | 44 |
| L5-S1 LSFTT | 74 | 44 | 75 | 44 | 73 | 45 |
| Prevalence | Percentage | Std. Dev. | Percentage | Std. Dev. | Percentage | Std. Dev. |
| HerniaL1-L2 | 21.66 | 1.08 | 21.52 | 1.08 | 21.81 | 1.09 |
| Hernia L2-L3 (mm) | 22.76 | 1.15 | 23.20 | 1.15 | 22.31 | 1.14 |
| Hernia L3-L4 (mm) | 26.62 | 1.32 | 27.34 | 1.35 | 25.89 | 1.29 |
| Hernia L4-L5 (mm) | 29.74 | 1.35 | 31.30 | 1.38 | 28.17 | 1.31 |
| Hernia L5-S1 (mm) | 30.46 | 1.22 | 32.27 | 1.25 | 28.64 | 1.17 |
| Two or more Hernias (%) | 36 | 48 | 47 | 50.21 | 25.88 | 44.06 |
| Overall Prevalence (%) | 65 | 48 | 69 | 47 | 61 | 49 |
| Overall Hernia Presence | Odds Ratio | Standard Error | Z | p | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Age | 0.98 | 0.01 | 1.56 | 0.118 | 0.96 | 1.00 |
| Gender | 0.65 | 0.23 | −1.21 | 0.225 | 0.33 | 1.30 |
| L1-L2 LSFTT | 4.46 | 2.80 | 2.38 | 0.017 | 1.30 | 15.24 |
| L2-L3 LSFTT | 5.26 | 3.27 | 2.67 | 0.008 | 1.56 | 17.81 |
| L3-L4 LSFTT | 4.43 | 2.77 | 2.38 | 0.017 | 1.30 | 15.07 |
| L4-L5 LSFTT | 4.62 | 2.89 | 2.45 | 0.014 | 1.35 | 15.73 |
| L5-S1 LSFTT | 4.55 | 2.84 | 2.43 | 0.015 | 1.34 | 15.43 |
| Average LSFTT L1-S1 | 0.22 | 0.13 | −2.47 | 0.140 | 0.64 | 1.73 |
| Post Hoc Hosmer–Lemeshow = 0.27 | ||||||
| Number of hernias per patient | Coefficient | Standard Error | Z | p | 95% Confidence Interval | |
| L5-S1 LSFTT | 0.013 | 0.005 | 2.460 | 0.014 | 0.003 | 0.024 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poot-Franco, J.A.; Mena-Balan, A.; Perez-Navarrete, A.; Huchim, O.; Azcorra-Perez, H.; Mendez-Dominguez, N. Association between the Thickness of Lumbar Subcutaneous Fat Tissue and the Presence of Hernias in Adults with Persistent, Non-Traumatic Low Back Pain. Tomography 2024, 10, 277-285. https://doi.org/10.3390/tomography10020022
Poot-Franco JA, Mena-Balan A, Perez-Navarrete A, Huchim O, Azcorra-Perez H, Mendez-Dominguez N. Association between the Thickness of Lumbar Subcutaneous Fat Tissue and the Presence of Hernias in Adults with Persistent, Non-Traumatic Low Back Pain. Tomography. 2024; 10(2):277-285. https://doi.org/10.3390/tomography10020022
Chicago/Turabian StylePoot-Franco, Jorge Adolfo, Anuar Mena-Balan, Adrian Perez-Navarrete, Osvaldo Huchim, Hugo Azcorra-Perez, and Nina Mendez-Dominguez. 2024. "Association between the Thickness of Lumbar Subcutaneous Fat Tissue and the Presence of Hernias in Adults with Persistent, Non-Traumatic Low Back Pain" Tomography 10, no. 2: 277-285. https://doi.org/10.3390/tomography10020022
APA StylePoot-Franco, J. A., Mena-Balan, A., Perez-Navarrete, A., Huchim, O., Azcorra-Perez, H., & Mendez-Dominguez, N. (2024). Association between the Thickness of Lumbar Subcutaneous Fat Tissue and the Presence of Hernias in Adults with Persistent, Non-Traumatic Low Back Pain. Tomography, 10(2), 277-285. https://doi.org/10.3390/tomography10020022







