Pilot Evaluation of Silicone Surrogates for Oral Mucosa Simulation in Craniofacial Surgical Training
Abstract
1. Introduction
1.1. A History of Surgical Education
1.2. Teaching for Rare Surgical Methods
1.3. 3D Modeling for Educational Insight
1.4. Functional 3D Models Enable On-Demand Practice
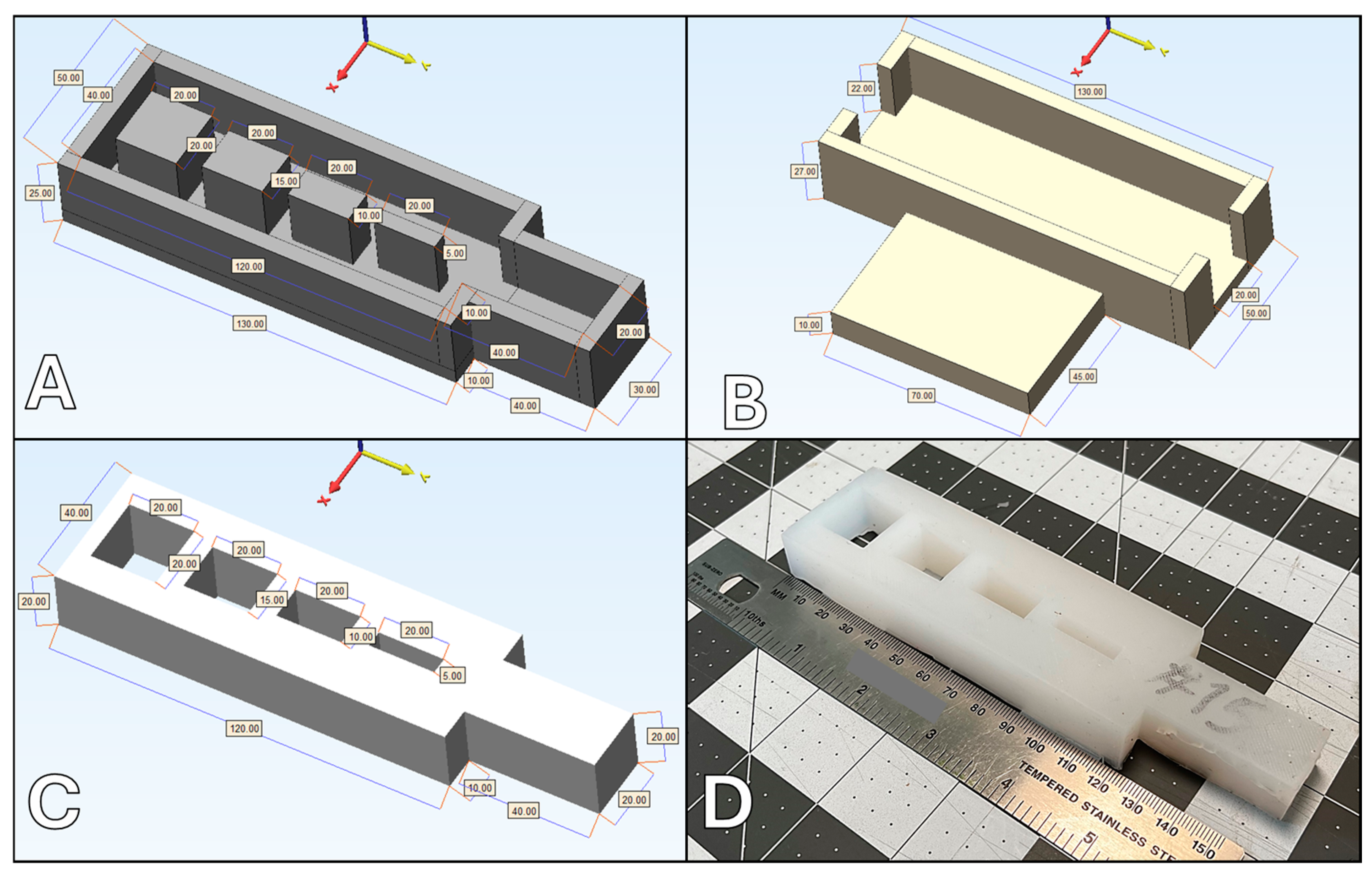
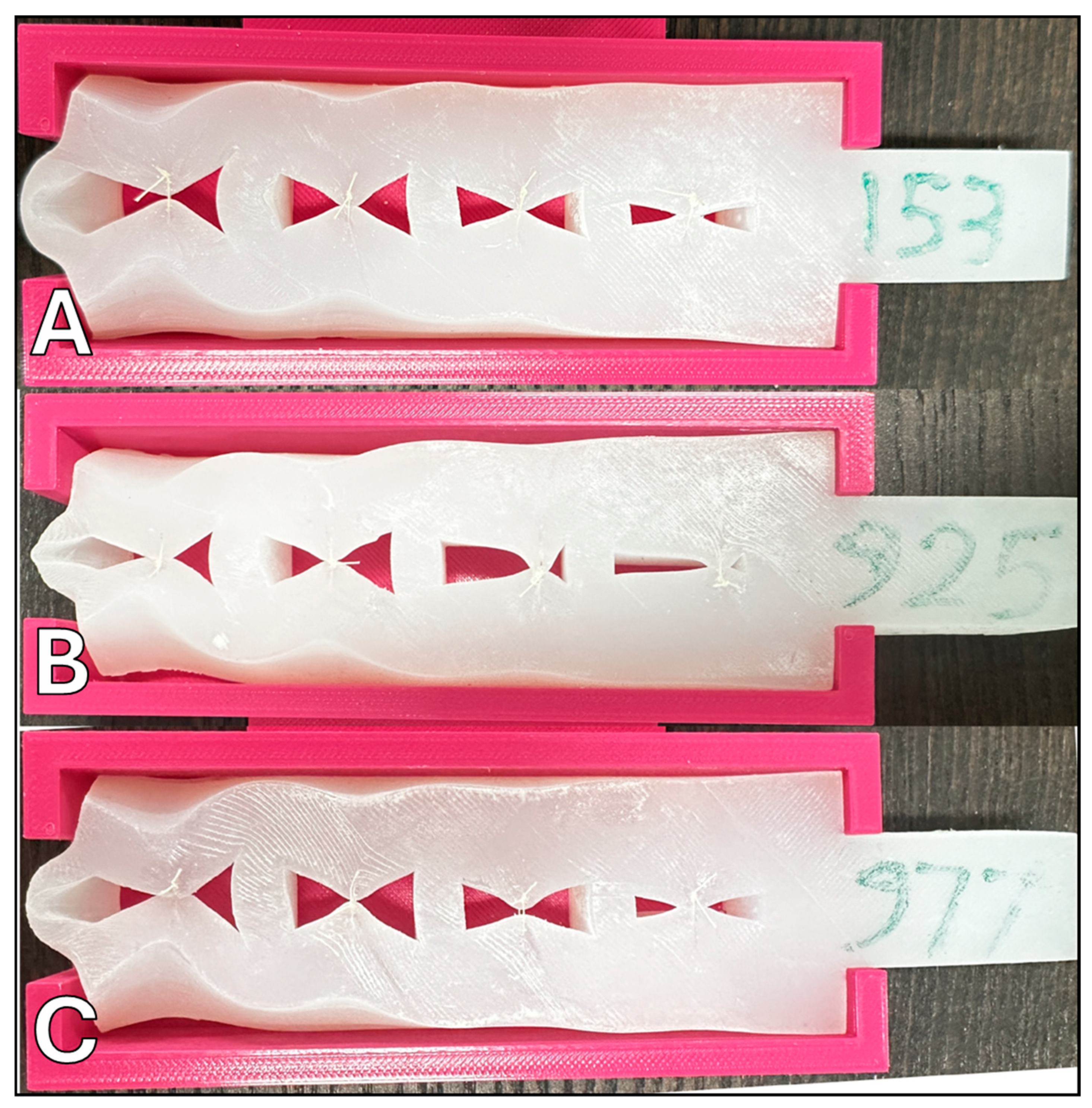
2. Materials and Methods
3. Results
4. Discussion
4.1. Current Challenges & Future Directions
4.2. Biomimicry of Surrogate Materials
4.3. Local Production, Customization, and Training for Enhanced Accessibility
4.4. Anticipated Challenges and Strategies for Refinement
4.5. Accessible & Equitable Practice
4.6. Global Implications in Surgical Education
4.7. Impact on Patient Care Outcomes
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Appuhamillage, G.A.; Ambagaspitiya, S.S.; Dassanayake, R.S.; Wijenayake, A. 3D and 4D printing of biomedical materials: Current trends, challenges, and future outlook. Explor. Med. 2024, 5, 17–47. [Google Scholar] [CrossRef]
- Michaels, R.; A Witsberger, C.; Powell, A.R.; Koka, K.; Cohen, K.; Nourmohammadi, Z.; E Green, G.; A Zopf, D. 3D printing in surgical simulation: Emphasized importance in the COVID-19 pandemic era. J. 3D Print. Med. 2021, 5, 5–9. [Google Scholar] [CrossRef]
- Michaels, R.E.; Witsberger, C.; Cin, M.D.; Zugris, N.V.; Jaksic, D.; Wen, K.; Nourmohammadi, Z.; Zopf, D. Development of a High-Fidelity, 3D-Printed Veau Class II Cleft Palate Simulator with Patient-Specific Capabilities. J. 3D Print. Med. 2022, 6, 69–75. [Google Scholar] [CrossRef]
- Choi, J.J.E.; Zwirner, J.; Ramani, R.S.; Ma, S.; Hussaini, H.M.; Waddell, J.N.; Hammer, N. Mechanical properties of human oral mucosa tissues are site dependent: A combined biomechanical, histological and ultrastructural approach. Clin. Exp. Dent. Res. 2020, 6, 602–611. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Lee, E.J.; Jang, W.B.; Kwon, S.-M. Development of Biocompatible 3D-Printed Artificial Blood Vessels through Multidimensional Approaches. J. Funct. Biomater. 2023, 14, 497. [Google Scholar] [CrossRef] [PubMed]
- Camison, L.; Brooker, J.E.; Naran, S.; Potts, J.R.; Losee, J.E. The History of Surgical Education in the United States: Past, Present, and Future. Ann. Surg. Open 2022, 3, e148. [Google Scholar] [CrossRef] [PubMed]
- Kotsis, S.V.; Chung, K.C. Application of the ‘See One, Do One, Teach One’ Concept in Surgical Training. Plast. Reconstr. Surg. 2013, 131, 1194–1201. [Google Scholar] [CrossRef] [PubMed]
- Shebrain, S.; Ferrin, N.; Cookenmaster, C.; Norman, E.; Sawyer, R. History of surgical training in Kalamazoo. Ann. Med. Surg. 2022, 73, 103175. [Google Scholar] [CrossRef] [PubMed]
- Nikkhah, D.; Rawlins, J. Training and mentorship in plastic surgery. J. Plast. Reconstr. Aesthet. Surg. 2019, 72, 1576–1606. [Google Scholar] [CrossRef]
- Chen, G.; Jin, S.; Xia, Q.; Wang, Z.; Shi, Z.; Chen, G.; Hong, Y.; Fan, X.; Lin, H. Insight into the history and trends of surgical simulation training in education: A bibliometric analysis. Int. J. Surg. 2023, 109, 2204–2213. [Google Scholar] [CrossRef]
- Lauer, C.I.; Shabahang, M.M.; Restivo, B.; Lane, S.; Hayek, S.; Dove, J.; Ellison, H.B.; Pica, E.; Ryer, E.J. The Value of Surgical Graduate Medical Education (GME) Programs Within An Integrated Health Care System. J. Surg. Educ. 2019, 76, e173–e181. [Google Scholar] [CrossRef] [PubMed]
- Ryan, M.S.; Holmboe, E.S.; Chandra, S. Competency-Based Medical Education: Considering Its Past, Present, and a Post–COVID-19 Era. Acad. Med. 2022, 97, S90–S97. [Google Scholar] [CrossRef]
- Kaban, L.B.; Hale, R.; Perrott, D.H. Oral and Maxillofacial Surgery Training in the United States. Oral Maxillofac. Surg. Clin. N. Am. 2022, 34, 495–503. [Google Scholar] [CrossRef]
- Liu, K.; Fang, B.; Wu, Y.; Li, Y.; Jin, J.; Tan, L.; Zhang, S. Anatomical education and surgical simulation based on the Chinese Visible Human: A three-dimensional virtual model of the larynx region. Anat. Sci. Int. 2013, 88, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Alemayehu, D.G.; Zhang, Z.; Tahir, E.; Gateau, D.; Zhang, D.-F.; Ma, X. Preoperative Planning Using 3D Printing Technology in Orthopedic Surgery. BioMed Res. Int. 2021, 2021, 7940242. [Google Scholar] [CrossRef]
- Sud, R.; Khanduja, S. Implementing competency-based medical education in post-graduate ophthalmology training: Understanding key concepts and methodologies and overcoming challenges. Indian J. Ophthalmol. 2022, 70, 3701. [Google Scholar] [CrossRef] [PubMed]
- Meling, T.R.; Meling, T.R. The impact of surgical simulation on patient outcomes: A systematic review and meta-analysis. Neurosurg. Rev. 2021, 44, 843–854. [Google Scholar] [CrossRef]
- Heskin, L.; Simms, C.; Traynor, O.; Galvin, R. Designing a synthetic simulator to teach open surgical skills for limb exploration in trauma: A qualitative study exploring the experiences and perspectives of educators and surgical trainees. BMC Surg. 2021, 21, 417. [Google Scholar] [CrossRef]
- Oxford, K.; Walsh, G.; Bungay, J.; Quigley, S.; Dubrowski, A. Development, manufacture and initial assessment of validity of a 3-dimensional-printed bowel anastomosis simulation training model. Can. J. Surg. 2021, 64, E484–E490. [Google Scholar] [CrossRef]
- Saba, P.; Belfast, E.; Melnyk, R.; Patel, A.; Kashyap, R.; Ghazi, A. Development of a High-Fidelity Robot-Assisted Kidney Transplant Simulation Platform Using Three-Dimensional Printing and Hydrogel Casting Technologies. J. Endourol. 2020, 34, 1088–1094. [Google Scholar] [CrossRef]
- Muelleman, T.; Peterson, J.; Chowdhury, N.; Gorup, J.; Camarata, P.; Lin, J. Individualized Surgical Approach Planning for Petroclival Tumors Using a 3D Printer. J. Neurol. Surg. Part B Skull Base 2015, 77, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Mobbs, R.J.; Coughlan, M.; Thompson, R.; Sutterlin, C.E.; Phan, K. The utility of 3D printing for surgical planning and patient-specific implant design for complex spinal pathologies: Case report. J. Neurosurg. Spine 2017, 26, 513–518. [Google Scholar] [CrossRef]
- Foresti, R.; Fornasari, A.; Massoni, C.B.; Mersanne, A.; Martini, C.; Cabrini, E.; Freyrie, A.; Perini, P. Surgical Medical Education via 3D Bioprinting: Modular System for Endovascular Training. Bioengineering 2024, 11, 197. [Google Scholar] [CrossRef]
- Qiu, K.; Haghiashtiani, G.; McAlpine, M.C. 3D Printed Organ Models for Surgical Applications. Annu. Rev. Anal. Chem. 2018, 11, 287–306. [Google Scholar] [CrossRef]
- Huang, X.; Wang, P.; Chen, J.; Huang, Y.; Liao, Q.; Huang, Y.; Liu, Z.; Peng, D. An intelligent grasper to provide real-time force feedback to shorten the learning curve in laparoscopic training. BMC Med. Educ. 2024, 24, 161. [Google Scholar] [CrossRef]
- Xu, J.; Anastasiou, D.; Booker, J.; Burton, O.E.; Horsfall, H.L.; Fernandez, C.S.; Xue, Y.; Stoyanov, D.; Tiwari, M.K.; Marcus, H.J.; et al. A Deep Learning Approach to Classify Surgical Skill in Microsurgery Using Force Data from a Novel Sensorised Surgical Glove. Sensors 2023, 23, 8947. [Google Scholar] [CrossRef] [PubMed]
- Talanki, V.R.; Peng, Q.; Shamir, S.B.; Baete, S.H.; Duong, T.Q.; Wake, N. Three-Dimensional Printed Anatomic Models Derived From Magnetic Resonance Imaging Data: Current State and Image Acquisition Recommendations for Appropriate Clinical Scenarios. J. Magn. Reson. Imaging 2022, 55, 1060–1081. [Google Scholar] [CrossRef] [PubMed]
- Maloney, S.; Haines, T. Issues of cost-benefit and cost-effectiveness for simulation in health professions education. Adv. Simul. 2016, 1, 13. [Google Scholar] [CrossRef]
- Tjønnås, M.S.; Muller, S.; Våpenstad, C.; Tjønnås, J.; Ose, S.O.; Das, A.; Sandsund, M. Stress responses in surgical trainees during simulation-based training courses in laparoscopy. BMC Med. Educ. 2024, 24, 407. [Google Scholar] [CrossRef] [PubMed]
- Tjønnås, M.S.; Das, A.; Våpenstad, C.; Ose, S.O. Simulation-based skills training: A qualitative interview study exploring surgical trainees’ experience of stress. Adv. Simul. 2022, 7, 33. [Google Scholar] [CrossRef]
- Ye, Z.; Dun, A.; Jiang, H.; Nie, C.; Zhao, S.; Wang, T.; Zhai, J. The role of 3D printed models in the teaching of human anatomy: A systematic review and meta-analysis. BMC Med. Educ. 2020, 20, 335. [Google Scholar] [CrossRef] [PubMed]
- Şenel, S. An Overview of Physical, Microbiological and Immune Barriers of Oral Mucosa. Int. J. Mol. Sci. 2021, 22, 7821. [Google Scholar] [CrossRef]
- Waasdorp, M.; Krom, B.P.; Bikker, F.J.; Van Zuijlen, P.P.M.; Niessen, F.B.; Gibbs, S. The Bigger Picture: Why Oral Mucosa Heals Better Than Skin. Biomolecules 2021, 11, 1165. [Google Scholar] [CrossRef]
- Carnevale, M.L.; Phair, J.; Indes, J.E.; Koleilat, I. Digital Footprint of Vascular Surgery Training Programs in the United States and Canada. Ann. Vasc. Surg. 2020, 67, 115–122. [Google Scholar] [CrossRef]
- Nagassa, R.G.; McMenamin, P.G.; Adams, J.W.; Quayle, M.R.; Rosenfeld, J.V. Advanced 3D printed model of middle cerebral artery aneurysms for neurosurgery simulation. 3D Print. Med. 2019, 5, 11. [Google Scholar] [CrossRef]
- Tenewitz, C.; Le, R.T.; Hernandez, M.; Baig, S.; Meyer, T.E. Systematic review of three-dimensional printing for simulation training of interventional radiology trainees. 3D Print. Med. 2021, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Gao, Q.; Wang, Q.; Li, M.; Lu, C. Feasibility and impact of three-dimensional (3D) printing technology in simulated teaching of congenital malformations. BMC Med. Educ. 2024, 24, 499. [Google Scholar] [CrossRef]
- Simkovich, S.M.; Underhill, L.J.; Kirby, M.A.; Crocker, M.E.; Goodman, D.; McCracken, J.P.; Thompson, L.M.; Diaz-Artiga, A.; Castañaza-Gonzalez, A.; Garg, S.S.; et al. Resources and Geographic Access to Care for Severe Pediatric Pneumonia in Four Resource-limited Settings. Am. J. Respir. Crit. Care Med. 2022, 205, 183–197. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Lee, Y.-C.; Kim, S.-G.; Garagiola, U. Advancements in Oral Maxillofacial Surgery: A Comprehensive Review on 3D Printing and Virtual Surgical Planning. Appl. Sci. 2023, 13, 9907. [Google Scholar] [CrossRef]
- García-Robles, P.; Cortés-Pérez, I.; Nieto-Escámez, F.A.; García-López, H.; Obrero-Gaitán, E.; Osuna-Pérez, M.C. Immersive virtual reality and augmented reality in anatomy education: A systematic review and meta-analysis. Anat. Sci. Educ. 2024, 17, 514–528. [Google Scholar] [CrossRef]
- von Bechtolsheim, F.; Franz, A.; Schmidt, S.; Schneider, A.; La Rosée, F.; Radulova-Mauersberger, O.; Krause-Jüttler, G.; Hümpel, A.; Bodenstedt, S.; Speidel, S.; et al. The development of tissue handling skills is sufficient and comparable after training in virtual reality or on a surgical robotic system: A prospective randomized trial. Surg. Endosc. 2024, 38, 2900–2910. [Google Scholar] [CrossRef] [PubMed]

| Sample # | Silicone 10A | Silicone 00-45 | Silicone Additive |
|---|---|---|---|
| 810 | 100 g | 0 g | 10 g (10%) |
| 456 | 100 g | 0 g | 20 g (20%) |
| 925 | 100 g | 0 g | 30 g (30%) |
| 926 | 75 g | 25 g | 10 g (10%) |
| 153 | 75 g | 25 g | 20 g (20%) |
| 370 | 75 g | 25 g | 30 g (30%) |
| 977 | 50 g | 50 g | 10 g (10%) |
| 445 | 50 g | 50 g | 20 g (20%) |
| 642 | 50 g | 50 g | 30 g (30%) |
| 966 | 25 g | 75 g | 10 g (10%) |
| 876 | 25 g | 75 g | 20 g (20%) |
| 864 | 25 g | 75 g | 30 g (30%) |
| 643 | 0 g | 100 g | 10 g (10%) |
| 498 | 0 g | 100 g | 20 g (20%) |
| 745 | 0 g | 100 g | 30 g (30%) |
| Domain | Sample 153 | Sample 925 | Sample 977 |
| Tactile Sensation | 4.0 | 3.0 | 5.0 |
| Tactile Hardness | 3.5 | 3.0 | 5.0 |
| Needle Puncture Performance | 4.0 | 4.5 | 3.5 |
| Cut Performance | 3.5 | 3.5 | 3.5 |
| Defect Repair Performance | 5.0 | 5.0 | 5.0 |
| Suture Retention to Manual Pull-out | 4.0 | 4.5 | 4.5 |
| Strain at Suture Pull-out | 3.0 | 3.5 | 4.5 |
| Strain with Finger Pinch | 3.0 | 4.0 | 4.0 |
| Average | 3.75 | 3.88 | 4.38 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cin, M.D.; Koka, K.; Darragh, J.; Nourmohammadi, Z.; Hamdan, U.; Zopf, D.A. Pilot Evaluation of Silicone Surrogates for Oral Mucosa Simulation in Craniofacial Surgical Training. Biomimetics 2024, 9, 464. https://doi.org/10.3390/biomimetics9080464
Cin MD, Koka K, Darragh J, Nourmohammadi Z, Hamdan U, Zopf DA. Pilot Evaluation of Silicone Surrogates for Oral Mucosa Simulation in Craniofacial Surgical Training. Biomimetics. 2024; 9(8):464. https://doi.org/10.3390/biomimetics9080464
Chicago/Turabian StyleCin, Mitchell D., Krishna Koka, Justin Darragh, Zahra Nourmohammadi, Usama Hamdan, and David A. Zopf. 2024. "Pilot Evaluation of Silicone Surrogates for Oral Mucosa Simulation in Craniofacial Surgical Training" Biomimetics 9, no. 8: 464. https://doi.org/10.3390/biomimetics9080464
APA StyleCin, M. D., Koka, K., Darragh, J., Nourmohammadi, Z., Hamdan, U., & Zopf, D. A. (2024). Pilot Evaluation of Silicone Surrogates for Oral Mucosa Simulation in Craniofacial Surgical Training. Biomimetics, 9(8), 464. https://doi.org/10.3390/biomimetics9080464










