Clinical Outcomes and Return-to-Sport Rates following Fragment Fixation Using Hydroxyapatite/Poly-L-Lactate Acid Threaded Pins for Knee Osteochondritis Dissecans: A Case Series
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
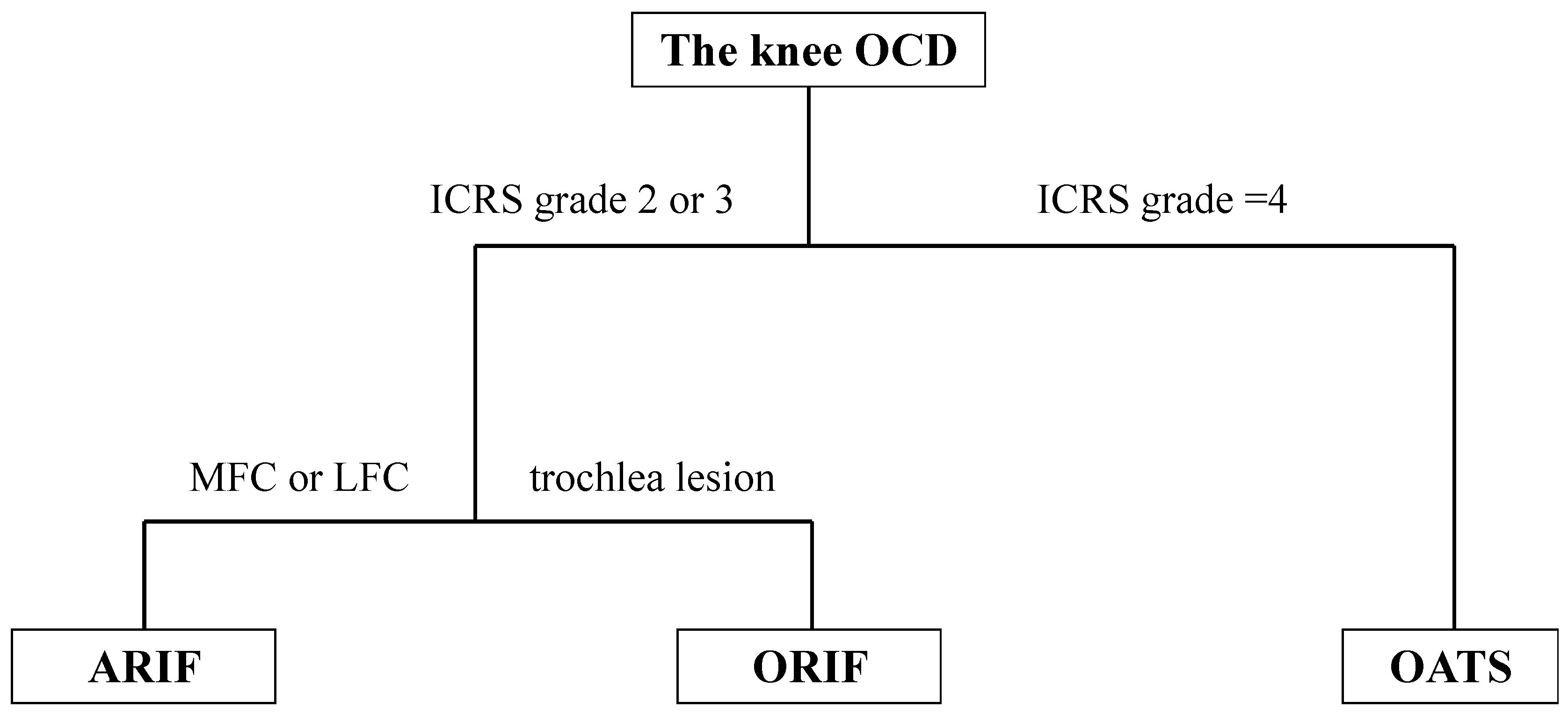
2.3. Surgical Technique
2.4. Postoperative Rehabilitation
2.5. Surgical Findings and Clinical Outcomes
2.6. Return to Sport
2.7. Postoperative Radiographs and MRIs
2.8. Statistical Analysis
3. Results
3.1. Patient Demographic Data and Surgical Records
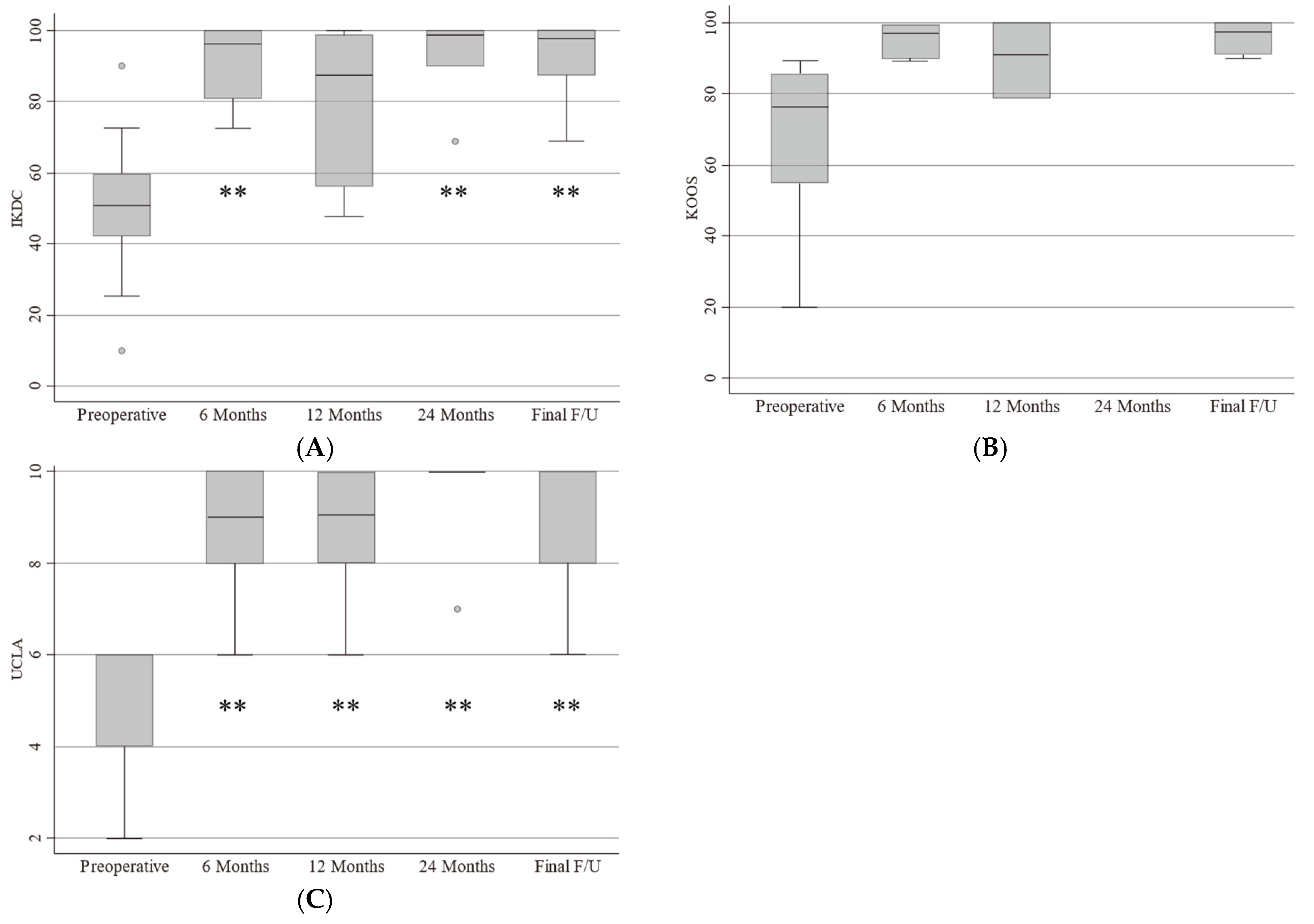
3.2. Clinical Outcomes
3.3. Return-to-Sports Rate
3.4. Postoperative Imaging Analysis
3.5. Case Presentation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andriolo, L.; Di Martino, A.; Altamura, S.A.; Boffa, A.; Poggi, A.; Busacca, M.; Zaffagnini, S.; Filardo, G. Matrix-assisted chondrocyte transplantation with bone grafting for knee osteochondritis dissecans: Stable results at 12 years. Knee Surg. Sports Traumatol. Arthrosc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Accadbled, F.; Vial, J.; Sales de Gauzy, J. Osteochondritis dissecans of the knee. Orthop. Traumatol. Surg. Res. 2018, 104, S97–S105. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Waterman, B.; Dean, R.; Redondo, M.; Cotter, E.; Manning, B.; Yanke, A.; Cole, B. The Influence of Physeal Status on Rate of Reoperation After Arthroscopic Screw Fixation for Symptomatic Osteochondritis Dissecans of the Knee. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. North. Am. Int. Arthrosc. Assoc. 2020, 36, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Hevesi, M.; Sanders, T.L.; Pareek, A.; Milbrandt, T.A.; Levy, B.A.; Stuart, M.J.; Saris, D.B.F.; Krych, A.J. Osteochondritis Dissecans in the Knee of Skeletally Immature Patients: Rates of Persistent Pain, Osteoarthritis, and Arthroplasty at Mean 14-Years’ Follow-Up. Cartilage 2020, 11, 291–299. [Google Scholar] [CrossRef]
- Keyhani, S.; Soleymanha, M.; Verdonk, R.; Abbasian, M. Autogenous Osteochondral Grafting for Treatment of Knee Osteochondritis Dissecans: A Case Series Study. Arch. Bone Jt. Surg. 2020, 8, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Gowd, A.K.; Beck, E.C.; Nabor, D.; Waterman, B.R. A Staged Arthroscopic Approach to Fixation of Unstable Osteochondritis Dissecans in the Medial Femoral Condyle of the Knee Using Nonabsorbable Fixation Screws. Arthrosc. Tech. 2020, 9, e477–e481. [Google Scholar] [CrossRef] [PubMed]
- Camathias, C.; Festring, J.D.; Gaston, M.S. Bioabsorbable lag screw fixation of knee osteochondritis dissecans in the skeletally immature. J. Pediatr. Orthop. B 2011, 20, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Kramer, D.E.; Yen, Y.M.; Simoni, M.K.; Miller, P.E.; Micheli, L.J.; Kocher, M.S.; Heyworth, B.E. Surgical management of osteochondritis dissecans lesions of the patella and trochlea in the pediatric and adolescent population. Am. J. Sports Med. 2015, 43, 654–662. [Google Scholar] [CrossRef]
- Schlechter, J.A.; Nguyen, S.V.; Fletcher, K.L. Utility of Bioabsorbable Fixation of Osteochondral Lesions in the Adolescent Knee: Outcomes Analysis With Minimum 2-Year Follow-up. Orthop. J. Sports Med. 2019, 7, 2325967119876896. [Google Scholar] [CrossRef] [PubMed]
- Tabaddor, R.R.; Banffy, M.B.; Andersen, J.S.; McFeely, E.; Ogunwole, O.; Micheli, L.J.; Kocher, M.S. Fixation of juvenile osteochondritis dissecans lesions of the knee using poly 96L/4D-lactide copolymer bioabsorbable implants. J. Pediatr. Orthop. 2010, 30, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Wiktor, Ł.; Tomaszewski, R. Evaluation of Osteochondritis Dissecans Treatment with Bioabsorbable Implants in Children and Adolescents. J. Clin. Med. 2022, 11, 5395. [Google Scholar] [CrossRef] [PubMed]
- Takayama, T.; Todo, M. Improvement of mechanical properties of hydroxyapatite particle-filled poly (l-lactide) biocomposites using lysine tri-isocyanate. J. Mater. Sci. 2009, 44, 5017–5020. [Google Scholar] [CrossRef]
- Morizane, K.; Shikinami, Y.; Fujibayashi, S.; Goto, K.; Otsuki, B.; Kawai, T.; Shimizu, T.; Matsuda, S. Implantable composite devices of unsintered hydroxyapatite and poly-l-lactide with dispersive marbling morphology to enhance in vivo bioactivity and bioresorbability. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 97, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Golan, O.; Shalom, H.; Kaplan-Ashiri, I.; Cohen, S.R.; Feldman, Y.; Pinkas, I.; Ofek Almog, R.; Zak, A.; Tenne, R. Poly(L-lactic acid) Reinforced with Hydroxyapatite and Tungsten Disulfide Nanotubes. Polymers 2021, 13, 3851. [Google Scholar] [CrossRef] [PubMed]
- Hiramatsu, K.; Yonetani, Y.; Tanaka, Y.; Kita, K.; Amano, H.; Kanamoto, T.; Tachibana, Y.; Kinugasa, K.; Horibe, S. Association of Stability and Size of Unhealed Area With Failure After Internal Fixation for Osteochondritis Dissecans Lesions of the Knee: Radiological Evaluation Using Computed Tomography. Am. J. Sports Med. 2024, 52, 352–361. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, M.; Nakamae, A.; Nakasa, T.; Ikuta, Y.; Hayashi, S.; Ochi, M.; Deie, M.; Adachi, N. Limitation of in-situ arthroscopic fixation for stable juvenile osteochondritis dissecans in the knee. J. Pediatr. Orthop. B 2018, 27, 516–521. [Google Scholar] [CrossRef]
- Uchida, S.; Utsunomiya, H.; Taketa, T.; Sakoda, S.; Hatakeyama, A.; Nakamura, T.; Sakai, A. Arthroscopic fragment fixation using hydroxyapatite/poly-L-lactate Acid thread pins for treating elbow osteochondritis dissecans. Am. J. Sports Med. 2015, 43, 1057–1065. [Google Scholar] [CrossRef]
- Cotter, E.J.; Frank, R.M.; Wang, K.C.; Totlis, T.; Poland, S.; Meyer, M.A.; Cole, B.J. Clinical Outcomes of Osteochondral Allograft Transplantation for Secondary Treatment of Osteochondritis Dissecans of the Knee in Skeletally Mature Patients. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. North. Am. Int. Arthrosc. Assoc. 2018, 34, 1105–1112. [Google Scholar] [CrossRef]
- Scott, C.E.H.; Turnbull, G.S.; MacDonald, D.; Breusch, S.J. Activity levels and return to work following total knee arthroplasty in patients under 65 years of age. Bone Jt. J. 2017, 99-B, 1037–1046. [Google Scholar] [CrossRef]
- Werner, B.C.; Chang, B.; Nguyen, J.T.; Dines, D.M.; Gulotta, L.V. What Change in American Shoulder and Elbow Surgeons Score Represents a Clinically Important Change After Shoulder Arthroplasty? Clin. Orthop. Relat. Res. 2016, 474, 2672–2681. [Google Scholar] [CrossRef]
- Albrecht, C.; Tichy, B.; Zak, L.; Aldrian, S.; Nürnberger, S.; Marlovits, S. Influence of Cell Differentiation and IL-1β Expression on Clinical Outcomes After Matrix-Associated Chondrocyte Transplantation. Am. J. Sports Med. 2014, 42, 59–69. [Google Scholar] [CrossRef]
- Lintz, F.; Pujol, N.; Pandeirada, C.; Boisrenoult, P.; Beaufils, P. Hybrid fixation: Evaluation of a novel technique in adult osteochondritis dissecans of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 568–571. [Google Scholar] [CrossRef] [PubMed]
- Shikinami, Y.; Okuno, M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly-L-lactide (PLLA): Part I. Basic characteristics. Biomaterials 1999, 20, 859–877. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, Y.; Sakano, S.; Iwase, T.; Warashina, H. The long-term behavior of poly-L-lactide screws in a minipig fracture model: Preliminary report. J. Biomed. Mater. Res. 2002, 63, 679–685. [Google Scholar] [CrossRef]
- Yasunaga, T.; Matsusue, Y.; Furukawa, T.; Shikinami, Y.; Okuno, M.; Nakamura, T. Bonding behavior of ultrahigh strength unsintered hydroxyapatite particles/poly(L-lactide) composites to surface of tibial cortex in rabbits. J. Biomed. Mater. Res. 1999, 47, 412–419. [Google Scholar] [CrossRef]
- Fukunaga, N.; Sato, H.; Wakami, T.; Shimoji, A.; Mori, O.; Yoshizawa, K.; Tamura, N. Fixation devices made of poly-L-lactide composite for rib reconstruction after thoracotomy. J. Cardiothorac. Surg. 2024, 19, 130. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.S.; Czarnecki, J.J.; Andersen, J.S.; Micheli, L.J. Internal fixation of juvenile osteochondritis dissecans lesions of the knee. Am. J. Sports Med. 2007, 35, 712–718. [Google Scholar] [CrossRef] [PubMed]
- Webb, J.E.; Lewallen, L.W.; Christophersen, C.; Krych, A.J.; McIntosh, A.L. Clinical outcome of internal fixation of unstable juvenile osteochondritis dissecans lesions of the knee. Orthopedics 2013, 36, e1444–e1449. [Google Scholar] [CrossRef]
- Millington, K.L.; Shah, J.P.; Dahm, D.L.; Levy, B.A.; Stuart, M.J. Bioabsorbable fixation of unstable osteochondritis dissecans lesions. Am. J. Sports Med. 2010, 38, 2065–2070. [Google Scholar] [CrossRef]
- Nakayama, H.; Yoshiya, S. Bone peg fixation of a large chondral fragment in the weight-bearing portion of the lateral femoral condyle in an adolescent: A case report. J. Med. Case Rep. 2014, 8, 316. [Google Scholar] [CrossRef] [PubMed]
- Slough, J.A.; Noto, A.M.; Schmidt, T.L. Tibial cortical bone peg fixation in osteochondritis dissecans of the knee. Clin. Orthop. Relat. Res. 1991, 122–127. [Google Scholar] [CrossRef]
- Ogura, T.; Sakai, H.; Asai, S.; Fukuda, H.; Takahashi, T.; Kanisawa, I.; Yamaura, I.; Tsuchiya, A.; Forney, M.; Winalski, C.S.; et al. Clinical and Radiographic Outcomes After Fixation of Chondral Fragments of the Knee in 6 Adolescents Using Autologous Bone Pegs. Orthop. J. Sports Med. 2020, 8, 2325967120963050. [Google Scholar] [CrossRef] [PubMed]
- Blackman, A.J.; Smith, M.V.; Flanigan, D.C.; Matava, M.J.; Wright, R.W.; Brophy, R.H. Correlation between magnetic resonance imaging and clinical outcomes after cartilage repair surgery in the knee: A systematic review and meta-analysis. Am. J. Sports Med. 2013, 41, 1426–1434. [Google Scholar] [CrossRef] [PubMed]
- Nissen, C.W.; Albright, J.C.; Anderson, C.N.; Busch, M.T.; Carlson, C.; Carsen, S.; Chambers, H.G.; Edmonds, E.W.; Ellermann, J.M.; Ellis, H.B., Jr.; et al. Descriptive Epidemiology From the Research in Osteochondritis Dissecans of the Knee (ROCK) Prospective Cohort. Am. J. Sports Med. 2022, 50, 118–127. [Google Scholar] [CrossRef] [PubMed]




| Number | Age | Sex | BMI (kg/m2) | Sport | OCD Legion |
|---|---|---|---|---|---|
| 1 | 14 | male | 24.2 | baseball | MFC |
| 2 | 12 | male | 18.7 | soccer | MFC |
| 3 | 16 | male | 19.5 | basketball | MFC |
| 4 | 16 | male | 17.1 | basketball | MFC |
| 5 | 13 | male | 18.6 | baseball | MFC |
| 6 | 14 | male | 19.2 | basketball | MFC |
| 7 | 12 | male | 15.9 | soccer | LFC |
| 8 | 13 | male | 19.5 | hand ball | LFC |
| 9 | 16 | male | 21.5 | soccer | LFC |
| 10 | 16 | male | 20.3 | volleyball | LFC |
| 11 | 17 | male | 22.6 | soccer | LFC |
| 12 | 13 | male | 16.7 | volleyball | LFC |
| 13 | 13 | male | 18.9 | basketball | trochlea |
| 14 | 16 | male | 21.8 | soccer | trochlea |
| Number | Size of OCD (mm) | ICRS Grade | Procedure | Number of Pins |
|---|---|---|---|---|
| 1 | 17 × 9 × 2.7 | 1 | ARIF | 3 |
| 2 | 30 × 15 × 3.0 | 2 | ARIF | 6 |
| 3 | 18 × 15 × 4.6 | 2 | ARIF | 5 |
| 4 | 20 × 13 × 6.3 | 2 | ARIF | 6 |
| 5 | 22 × 16 × 4.3 | 3 | ARIF | 5 |
| 6 | 20 × 20 × 2.9 | 3 | ORIF | 9 |
| 7 | 17 × 10 × 3.2 | 1 | ARIF | 2 |
| 8 | 16 × 14 × 5.6 | 2 | ARIF | 5 |
| 9 | 30 × 25 × 8.3 | 3 | ARIF | 9 |
| 10 | 15 × 13 × 6.7 | 3 | ORIF | 6 |
| 11 | 28 × 21 × 4.3 | 3 | ARIF | 6 |
| 12 | 25 × 15 × 3.7 | 3 | ORIF | 7 |
| 13 | 29 × 28 × 4.2 | 3 | ORIF | 10 |
| 14 | 26 × 19 × 3.9 | 3 | ORIF | 9 |
| Number | RTS | Duration from Surgery to RTS (Month) |
|---|---|---|
| 1 | higher | 4 |
| 2 | same | 8 |
| 3 | higher | 6 |
| 4 | same | 6 |
| 5 | same | 9 |
| 6 | same | 6 |
| 7 | higher | 5 |
| 8 | same | 11 |
| 9 | same | 10 |
| 10 | higher | 7 |
| 11 | higher | 8 |
| 12 | higher | 5 |
| 13 | same | 5 |
| 14 | higher | 6 |
| Number | Time to Union (Month) | MOCART Score | M1 | M2 | M3 | M4 | M5 1 | M5 2 | M6 | M7 | M8 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 4 | - | |||||||||
| 2 | 3 | 100 | 20 | 15 | 10 | 5 | 15 | 15 | 5 | 5 | 5 |
| 3 | 3 | 75 | 20 | 15 | 10 | 5 | 5 | 5 | 5 | 5 | 5 |
| 4 | 6 | 75 | 20 | 15 | 10 | 5 | 5 | 5 | 5 | 5 | 5 |
| 5 | 4 | 75 | 20 | 15 | 10 | 5 | 5 | 5 | 5 | 5 | 5 |
| 6 | 4 | 70 | 20 | 15 | 10 | 5 | 5 | 5 | 0 | 0 | 5 |
| 7 | 5 | 100 | 20 | 15 | 10 | 5 | 15 | 15 | 5 | 5 | 5 |
| 8 | 6 | 75 | 20 | 15 | 10 | 5 | 5 | 5 | 5 | 5 | 5 |
| 9 | - | 55 | 20 | 15 | 10 | 5 | 0 | 0 | 0 | 0 | 5 |
| 10 | 4 | 100 | 20 | 15 | 10 | 5 | 15 | 15 | 5 | 5 | 5 |
| 11 | 7 | 55 | 20 | 15 | 10 | 0 | 0 | 0 | 0 | 0 | 5 |
| 12 | 3 | 100 | 20 | 15 | 10 | 5 | 15 | 15 | 5 | 5 | 5 |
| 13 | 4 | 100 | 20 | 15 | 10 | 5 | 15 | 15 | 5 | 5 | 5 |
| 14 | 7 | 100 | 20 | 15 | 10 | 5 | 15 | 15 | 5 | 5 | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shimizu, T.; Murata, Y.; Nakashima, H.; Nishimura, H.; Suzuki, H.; Kawasaki, M.; Tsukamoto, M.; Sakai, A.; Uchida, S. Clinical Outcomes and Return-to-Sport Rates following Fragment Fixation Using Hydroxyapatite/Poly-L-Lactate Acid Threaded Pins for Knee Osteochondritis Dissecans: A Case Series. Biomimetics 2024, 9, 232. https://doi.org/10.3390/biomimetics9040232
Shimizu T, Murata Y, Nakashima H, Nishimura H, Suzuki H, Kawasaki M, Tsukamoto M, Sakai A, Uchida S. Clinical Outcomes and Return-to-Sport Rates following Fragment Fixation Using Hydroxyapatite/Poly-L-Lactate Acid Threaded Pins for Knee Osteochondritis Dissecans: A Case Series. Biomimetics. 2024; 9(4):232. https://doi.org/10.3390/biomimetics9040232
Chicago/Turabian StyleShimizu, Taichi, Yoichi Murata, Hirotaka Nakashima, Haruki Nishimura, Hitoshi Suzuki, Makoto Kawasaki, Manabu Tsukamoto, Akinori Sakai, and Soshi Uchida. 2024. "Clinical Outcomes and Return-to-Sport Rates following Fragment Fixation Using Hydroxyapatite/Poly-L-Lactate Acid Threaded Pins for Knee Osteochondritis Dissecans: A Case Series" Biomimetics 9, no. 4: 232. https://doi.org/10.3390/biomimetics9040232
APA StyleShimizu, T., Murata, Y., Nakashima, H., Nishimura, H., Suzuki, H., Kawasaki, M., Tsukamoto, M., Sakai, A., & Uchida, S. (2024). Clinical Outcomes and Return-to-Sport Rates following Fragment Fixation Using Hydroxyapatite/Poly-L-Lactate Acid Threaded Pins for Knee Osteochondritis Dissecans: A Case Series. Biomimetics, 9(4), 232. https://doi.org/10.3390/biomimetics9040232






