The Moment Criterion of Anthropomorphicity of Prosthetic Feet as a Potential Predictor of Their Functionality for Transtibial Amputees
Abstract
:1. Introduction
1.1. Problem of Overloading the Residuum
1.2. Current Regulatory Status of Prosthetic Feet
1.3. Motivation for the Current Study
2. Materials and Methods
2.1. Normal Ballistic Synergy and Compensatory Prosthetic Synergy
2.1.1. Ballistic Synergy in the Norm
2.1.2. Compensatory Synergy in Prosthetic Gait
2.2. Anthropomorphicity of Prosthetic Feet and Evolution of Its Criteria
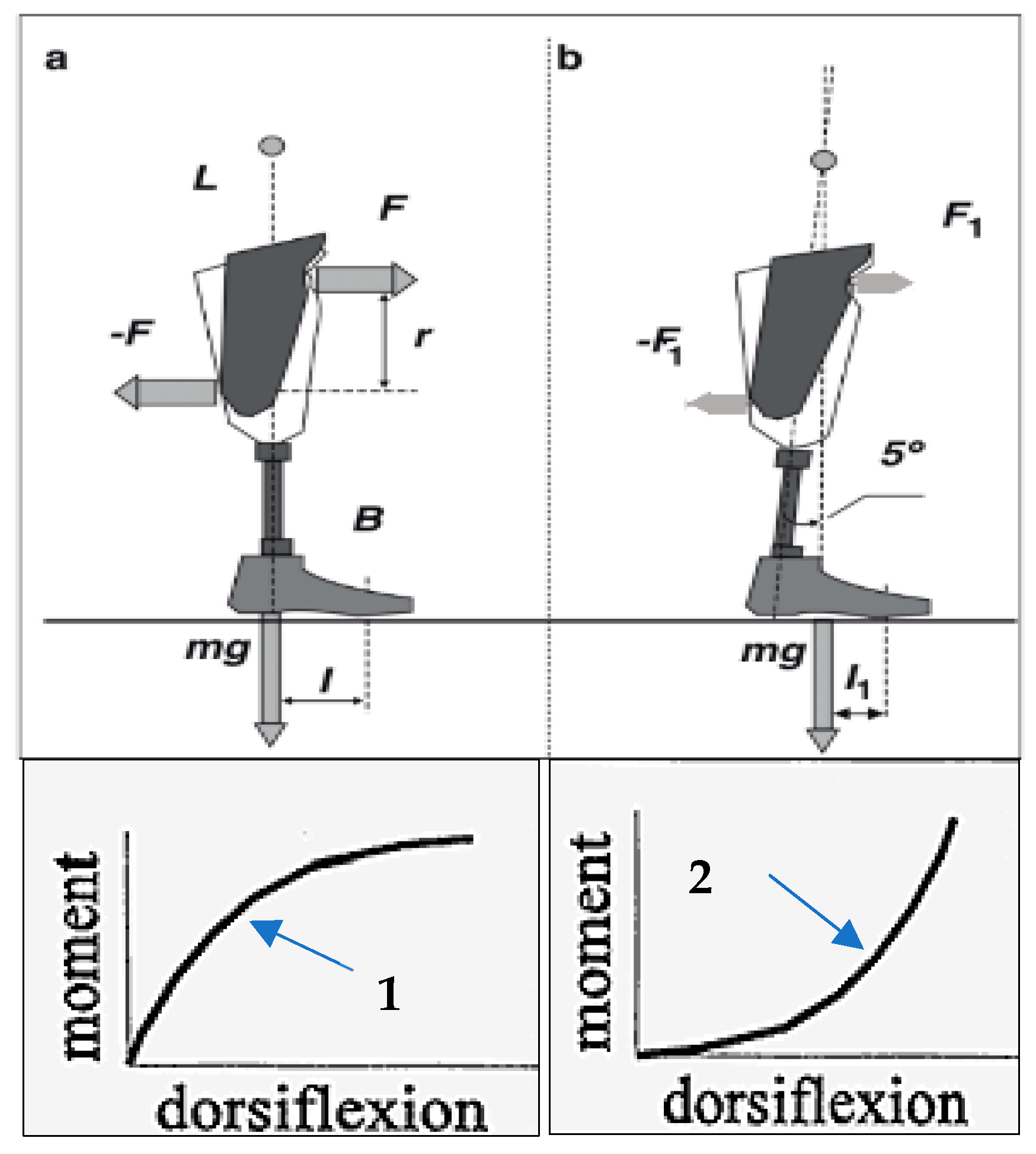
2.2.1. Index of Anthropomorphicity and Its Relation to Bending Moments
2.2.2. Automated Procedure to Compute the Index of Anthropomorphicity
2.2.3. Outcomes of the Observational Study
3. Discussion
4. Conclusions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Pohjolainen, T. A clinical evaluation of stumps in lower limb amputees. Prosthet. Orthot. Int. 1991, 15, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Koc, E.; Tunca, M.; Akar, A.; Erbil, A.H.; Demiralp, B.; Arca, E. Skin problems in amputees: A descriptive study. Int. J. Dermatol. 2008, 47, 463–466. [Google Scholar] [CrossRef] [PubMed]
- Meulenbelt, H.E.; Geertzen, J.H.; Jonkman, M.F.; Dijkstra, P.U. Skin problems of the stump in lower limb amputees: 1. A clinical study. Acta Derm.-Venereol. 2011, 91, 173–177. [Google Scholar] [CrossRef]
- Buikema, K.E.; Meyerle, J.H. Amputation stump: Privileged harbor for infections, tumors, and immune disorders. Clin. Dermatol. 2014, 32, 670–677. [Google Scholar] [CrossRef] [PubMed]
- Colgecen, E.; Korkmaz, M.; Ozyurt, K.; Mermerkaya, U.; Kader, C. A clinical evaluation of skin disorders of lower limb amputation sites. Int. J. Dermatol. 2016, 55, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Bennett, L. Transferring load to flesh. Bull. Prosthet. Res. 1974, Fall, 133–143. [Google Scholar]
- Sinha, R.; Van Den Heuvel, W.J.; Arokiasamy, P. Factors affecting quality of life in lower limb amputees. Prosthet. Orthot. Int. 2011, 35, 90–96. [Google Scholar] [CrossRef]
- Calabrese, L.; Maffoni, M.; Torlaschi, V.; Pierobon, A. What Is Hidden behind Amputation? Quanti-Qualitative Systematic Review on Psychological Adjustment and Quality of Life in Lower Limb Amputees for Non-Traumatic Reasons. Healthcare 2023, 11, 1661. [Google Scholar] [CrossRef]
- Sankaran, S.; Murugan, P.R.; Johnson, J.C.; Abdullah, H.J.S.; Raj, C.M.N.; Ashokan, D. Prevention of Skin Problems in Patients using Prosthetic Limb: A Review of Current Technologies and Limitations. In Proceedings of the 2019 International Conference on Communication and Signal Processing (ICCSP), Melmaruvathur, India, 4–6 April 2019; pp. 0077–0081. [Google Scholar]
- Quintero-Quiroz, C.; Pérez, V.Z. Materials for lower limb prosthetic and orthotic interfaces and sockets: Evolution and associated skin problems. Rev. Fac. Med. 2019, 67, 117–125. [Google Scholar] [CrossRef]
- Branemark, R.P.; Hagberg, K.; Kulbacka-Ortiz, K.; Berlin, O.; Rydevik, B. Osseointegrated Percutaneous Prosthetic System for the Treatment of Patients With Transfemoral Amputation: A Prospective Five-year Follow-up of Patient-reported Outcomes and Complications. J. Am. Acad. Orthop. Surg. 2019, 27, e743–e751. [Google Scholar] [CrossRef] [PubMed]
- Thesleff, A.; Branemark, R.; Hakansson, B.; Ortiz-Catalan, M. Biomechanical Characterisation of Bone-anchored Implant Systems for Amputation Limb Prostheses: A Systematic Review. Ann. Biomed. Eng. 2018, 46, 377–391. [Google Scholar] [CrossRef]
- Branemark, R.; Berlin, O.; Hagberg, K.; Bergh, P.; Gunterberg, B.; Rydevik, B. A novel osseointegrated percutaneous prosthetic system for the treatment of patients with transfemoral amputation: A prospective study of 51 patients. Bone Jt. J. 2014, 96-B, 106–113. [Google Scholar] [CrossRef]
- Fitzpatrick, N.; Smith, T.J.; Pendegrass, C.J.; Yeadon, R.; Ring, M.; Goodship, A.E.; Blunn, G.W. Intraosseous transcutaneous amputation prosthesis (ITAP) for limb salvage in 4 dogs. Vet. Surg. 2011, 40, 909–925. [Google Scholar] [CrossRef] [PubMed]
- Farina, D.; Vujaklija, I.; Brånemark, R.; Bull, A.M.J.; Dietl, H.; Graimann, B.; Hargrove, L.J.; Hoffmann, K.-P.; Huang, H.; Ingvarsson, T.; et al. Toward higher-performance bionic limbs for wider clinical use. Nat. Biomed. Eng. 2021, 7, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Black, G.G.; Vaeth, A.M.; Chen, Y.; Truong, A.Y.; Reif, T.J.; Rozbruch, S.R.; Otterburn, D.M. Osseointegration for Lower Limb Amputation: Understanding the Risk Factors and Time Courses of Soft Tissue Complications. Ann. Plast. Surg. 2023, 90, S452–S456. [Google Scholar] [CrossRef] [PubMed]
- Bowker, J.H. The Art of Prosthesis Prescription. In Atlas of Amputations and Limb Deficiencies: Surgical, Prosthetic, and Rehabilitation Principles; Smith, D., Michael, J., Bowker, J., Eds.; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2004; Chapter 582004. [Google Scholar]
- Stevens, P.M.; Rheinstein, J.; Wurdeman, S.R. Prosthetic Foot Selection for Individuals with Lower-Limb Amputation: A Clinical Practice Guideline. JPO J. Prosthet. Orthot. 2018, 30, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, E.J.; Riddick, W. Reliability, Validity, and Responsiveness of Clinical Performance-Based Outcome Measures of Walking for Individuals With Lower Limb Amputations: A Systematic Review. Phys. Ther. 2018, 98, 1037–1045. [Google Scholar] [CrossRef]
- Koehler-McNicholas, S.R.; Nickel, E.A.; Barrons, K.; Blaharski, K.E.; Dellamano, C.A.; Ray, S.F.; Schnall, B.L.; Hendershot, B.D.; Hansen, A.H. Mechanical and dynamic characterization of prosthetic feet for high activity users during weighted and unweighted walking. PLoS ONE 2018, 13, e0202884. [Google Scholar] [CrossRef]
- Webber, C.M.; Kaufman, K. Instantaneous stiffness and hysteresis of dynamic elastic response prosthetic feet. Prosthet. Orthot. Int. 2017, 41, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Czerniecki, J.M. Research and clinical selection of foot-ankle systems. JPO J. Prosthet. Orthot. 2005, 17, S35–S37. [Google Scholar] [CrossRef]
- Linde, H.; Geurts, A.; Hofstad, C.; Postema, K.; Geertzen, J.; Limbeek, J.v. A systematic literature review of the effect of different prosthetic components on human functioning with a lower limb prosthesis. J. Rehabil. Res. Dev. 2004, 41, 555–570. [Google Scholar] [CrossRef] [PubMed]
- Raschke, S.U.; Orendurff, M.S.; Mattie, J.L.; Kenyon, D.E.; Jones, O.Y.; Moe, D.; Winder, L.; Wong, A.S.; Moreno-Hernández, A.; Highsmith, M.J. Biomechanical characteristics, patient preference and activity level with different prosthetic feet: A randomized double blind trial with laboratory and community testing. J. Biomech. 2015, 48, 146–152. [Google Scholar] [CrossRef] [PubMed]
- AOPA. American Orthotic Prosthetics Association’S Prosthetic Foot Project: What It Is Not, and What Patient Care Facility Providers/Practitioners Need to Know; American Orthotic and Prosthetic Association (AOPA): Alexandria, VA, USA, 2010; pp. 1–44. [Google Scholar]
- Perry, J. Gait Analysis: Normal and Pathological Function; Slack, Inc.: Thorofare, NJ, USA, 1992. [Google Scholar]
- Valmassy, R.L. Clinical Biomechanics of the Lower Extremities; Mosby: St. Louis, MO, USA, 1996; p. vxiii. 510p. [Google Scholar]
- FDA. 21CFR890.3420. In Code of Federal Regulations Title 21/H—Medical Devices/Part 890—Physical Medicine Devices/Subpart D—Physical Medicine Prosthetic Devices/Sec. 890.3420 External Limb Prosthetic Component; Food and Drug Administration: Silver Spring, MD, USA, 2018. [Google Scholar]
- ISO 22675:2016; Prosthetics—Testing of Ankle-Foot Devices and Foot Units—Requirements and Test Methods. International Organization for Standardization: Geneva, Switzerland, 2016.
- ISO 22523:2006; External Limb Prostheses and External Orthoses—Requirements and Test Methods. International Organization for Standardization: Geneva, Switzerland, 2006.
- ISO/TS 16955:2016(en); Prosthetics—Quantification of Physical Parameters of Ankle Foot Devices and Foot Units. International Organization for Standardization: Geneva, Switzerland, 2016.
- ISO 10328:2016; Prosthetics—Structural Testing of Lower-Limb Prosthetics—Requirements and Test Methods. International Organization for Standardization: Geneva, Switzerland, 2016. Available online: https://www.iso.org/standard/36413.html (accessed on 20 November 2023).
- Suryawan, D.; Khafidh, M.; Kistriyani, L.; Ismail, R. A systematic review and comparison of international standards for prosthetic feet. In AIP Conference Proceedings; AIP Publishing LLC: Melville, NY, USA, 2023; Volume 2568. [Google Scholar]
- Pitkin, M.R. Mechanical Outcomes of a Rolling-Joint Prosthetic Foot and Its Performance in the Dorsiflexion Phase of Transtibial Amputee Gait. J. Prosthet. Orthot. 1995, 7, 114–123. [Google Scholar] [CrossRef]
- Pitkin, M. What can normal gait biomechanics teach a designer of lower limb prostheses? Acta Bioeng. Biomech. 2013, 15, 3–10. [Google Scholar] [PubMed]
- Quesada, P.M.; Pitkin, M.; Colvin, J. Biomechanical evaluation of a prototype foot/ankle prosthesis. IEEE Trans. Rehabil. Eng. 2000, 8, 156–159. [Google Scholar] [CrossRef]
- Quesada, P.; Pitkin, M.; Hays, J.; Colvin, J. Rotational stiffness adjustability of a prototype foot/ankle prosthesis. In Proceedings of the ASME International Mechanical Engineering Congress and Exposition, Nashville, TN, USA, 14–19 November 1999; p. 159. [Google Scholar]
- Pitkin, M.; Frossard, L. Loading Effect of Prosthetic Feet’s Anthropomorphicity on Transtibial Osseointegrated Implant. Mil. Med. 2021, 186 (Suppl. S1), 681–687. [Google Scholar] [CrossRef] [PubMed]
- Pitkin, M. Mechanics of the Mobility of the Human Foot. Mechanics of Solids (Mechanica Tverdogo Tela (in Russian), Izvestia of the Academy of Sciences of the USSR, Moscow). Mechnica Solids 1975, 10, 40–45. [Google Scholar]
- Frossard, L.; Leech, B.; Pitkin, M. Automated characterization of anthropomorphicity of prosthetic feet fitted to bone-anchored transtibial prosthesis. IEEE Trans. Biomed. Eng. 2019, 66, 3402–3410. [Google Scholar] [CrossRef]
- Pitkin, M. Theory of Designing the Anthropomorphic Lower Limb Prostheses. In Biomechanics of Lower Limb Prosthetics; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Winter, D.A. Biomechanics of Human Movement; John Willey & Sons, Inc.: New York, NY, USA, 1979. [Google Scholar]
- Saunders, J.B.; Inman, V.T.; Eberhart, H.D. The major determinants in normal and pathological gait. J. Bone Jt. Surg. Am. 1953, 35-A, 543–558. [Google Scholar] [CrossRef]
- Scott, S.H.; Winter, D.A. Talocrural and talocalcaneal joint kinematics and kinetics during the stance phase of walking. J. Biomech. 1991, 24, 743–752. [Google Scholar] [CrossRef]
- Pitkin, M. Effects of Design Variants in Lower Limb Prostheses on Gait Synergy. J. Prosthet. Orthot. 1997, 9, 113–122. [Google Scholar] [CrossRef]
- Breakey, J. Gait of unilateral below-knee amputees. Orthot. Prosthet. 1976, 30, 17–24. [Google Scholar]
- Lloyd, C.H.; Stanhope, S.J.; Davis, I.S.; Royer, T.D. Strength asymmetry and osteoarthritis risk factors in unilateral trans-tibial, amputee gait. Gait Posture 2010, 32, 296–300. [Google Scholar] [CrossRef] [PubMed]
- Norvell, D.C.; Czerniecki, J.M.; Reiber, G.E.; Maynard, C.; Pecoraro, J.A.; Weiss, N.S. The prevalence of knee pain and symptomatic knee osteoarthritis among veteran traumatic amputees and nonamputees. Arch. Phys. Med. Rehabil. 2005, 86, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Jasni, F.; Hamzaid, N.A.; Mohd Syah, N.E.; Chung, T.Y.; Abu Osman, N.A. Analysis of interrelationships among voluntary and prosthetic leg joint parameters using cyclograms. Front. Neurosci. 2017, 11, 230. [Google Scholar] [CrossRef] [PubMed]
- Olesnavage, K.M.; Prost, V.; Johnson, W.B.; Major, M.J.; Winter, A.G. Experimental Demonstration of the Lower Leg Trajectory Error Framework Using Physiological Data as Inputs. J. Biomech. Eng. 2021, 143, 031003. [Google Scholar] [CrossRef] [PubMed]
- Kadhim, F.M.; Chiad, J.S.; Takhakh, A.M. Design and manufacturing knee joint for smart transfemoral prosthetic. In IOP Conference Series: Materials Science and Engineering; IOP Publishing: Bristol, UK, 2018; Volume 454, p. 012078. [Google Scholar]
- Bai, X.; Ewins, D.; Crocombe, A.D.; Xu, W. Kinematic and biomimetic assessment of a hydraulic ankle/foot in level ground and camber walking. PLoS ONE 2017, 12, e0180836. [Google Scholar] [CrossRef]
- Cavaco, A.; Ramalho, A.; Pais, S.; Durães, L. Mechanical and structural characterization of tibial prosthetic interfaces before and after aging under simulated service conditions. J. Mech. Behav. Biomed. Mater. 2015, 43, 78–90. [Google Scholar] [CrossRef]
- LaPrè, A.; Sup, F. A.; Sup, F. A control strategy for an active alignment transtibial prosthesis. In Dynamic Systems and Control Conference; American Society of Mechanical Engineers: New York, NY, USA, 2015; Volume 57243. [Google Scholar]
- Powelson, T.; Yang, J. Literature review of prosthetics for transtibial amputees. Int. J. Biomechatron. Biomed. Robot. 2012, 2, 50–64. [Google Scholar] [CrossRef]
- Chen, C.W.J.; Heim, W.; Fairley, K.; Clement, R.J.; Biddiss, E.; Torres-Moreno, R.; Andrysek, J. Evaluation of an instrument-assisted dynamic prosthetic alignment technique for individuals with transtibial amputation. Prosthet. Orthot. Int. 2016, 40, 475–483. [Google Scholar] [CrossRef]
- Klute, G.K.; Kallfelz, C.F.; Czerniecki, J.M. Mechanical properties of prosthetic limbs: Adapting to the patient. J. Rehabil. Res. Dev. 2001, 38, 299–307. [Google Scholar]
- Prinsen, E.C.; Nederhand, M.J.; Rietman, J.S. Adaptation strategies of the lower extremities of patients with a transtibial or transfemoral amputation during level walking: A systematic review. Arch. Phys. Med. Rehabil. 2011, 92, 1311–1325. [Google Scholar] [CrossRef]
- Crenna, P.; Frigo, C. Dynamics of the ankle joint analyzed through moment–angle loops during human walking: Gender and age effects. Hum. Mov. Sci. 2011, 30, 1185–1198. [Google Scholar] [CrossRef] [PubMed]
- Major, M.J.; Twiste, M.; Kenney, L.P.; Howard, D. The effects of prosthetic ankle stiffness on stability of gait in people with transtibial amputation. J. Rehabil. Res. Dev. 2016, 53, 839–852. [Google Scholar] [CrossRef] [PubMed]
- Gard, S.A.; Su, P.F.; Lipschutz, R.D.; Hansen, A.H. Effect of prosthetic ankle units on roll-over shape characteristics during walking in persons with bilateral transtibial amputations. J. Rehabil. Res. Dev. 2011, 48, 1037–1048. [Google Scholar] [CrossRef] [PubMed]
- Drevelle, X.; Villa, C.; Bonnet, X.; Bascou, J.; Loiret, I.; Pillet, H. Analysis of ankle stiffness for asymptomatic subjects and transfemoral amputees in daily living situations. Comput. Methods Biomech. Biomed. Eng. 2014, 17 (Suppl. S1), 80–81. [Google Scholar] [CrossRef]
- Wright, D.G.; Rennels, D.C. A Study of the Elastic Properties of Plantar Fascia. J. Bone Jt. Surg. Am. 1964, 46, 482–492. [Google Scholar] [CrossRef]
- Pitkin, M.; Hays, J.; Srinivasan, S.; Colvin, J. Artificial foot and ankle. US Patent 6290730, 2001. Available online: https://patents.google.com/patent/US6290730B1/en (accessed on 20 November 2023).
- Pitkin, M.R. Synthesis of a cycloidal mechanism of the prosthetic ankle. Prosthet. Orthot. Int. 1996, 20, 159–171. [Google Scholar] [CrossRef]
- Pitkin, M. Lowering the forces and pressures on amputee stump with Rolling Joint Foot. Biomechanics 1999, 6, 315–318. [Google Scholar]
- Pitkin, M.; Colvin, J.; Quesada, P.; Hayes, J. Gait Analysis of Twenty Unilateral Transtibial Amputees; Report, NIH/NIAMS/NCMRR Grant2R44AR4 3290-02 “Prosthetic Rolling Joint Foot and Ankle”; Ohio Willow Wood Company: Mt. Sterling, OH, USA, 1999. [Google Scholar]
- Pillet, H.; Drevelle, X.; Bonnet, X.; Villa, C.; Martinet, N.; Sauret, C.; Bascou, J.; Loiret, I.; Djian, F.; Rapin, N. APSIC: Training and fitting amputees during situations of daily living. IRBM 2014, 35, 60–65. [Google Scholar] [CrossRef]
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Kr, M.; Shree, V.; Swetha, P. Understanding the etiologies and methods to assess the need for lower limb amputation. J. Cardiovasc. Dis. Res. 2023, 14, 589–600. [Google Scholar]
- McDonald, C.L.; Westcott-McCoy, S.; Weaver, M.R.; Haagsma, J.; Kartin, D. Global prevalence of traumatic non-fatal limb amputation. Prosthet. Orthot. Int. 2021, 45, 105–114. [Google Scholar] [CrossRef]
- Røikjer, J.; Jensen, M.H.; Vestergaard, P.; Sørensen, A.M.; Laursen, H.V.B.; Ejskjær, N. Twenty years with diabetes and amputations: A retrospective population-based cohort study. Diabet. Med. 2020, 37, 2098–2108. [Google Scholar] [CrossRef]
- MacKenzie, E.J.; Castillo, R.C.; Jones, A.S.; Bosse, M.J.; Kellam, J.F.; Pollak, A.N.; Webb, L.X.; Swiontkowski, M.F.; Smith, D.G.; Sanders, R.W. Health-care costs associated with amputation or reconstruction of a limb-threatening injury. J. Bone Jt. Surg. 2007, 89, 1685–1692. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, A.T.; Pallangyo, A.J.; Herman, A.M.; Schaumeier, M.J.; Smith, A.D.; Hevelone, N.D.; Crandell, D.M.; Nguyen, L.L. The effect of social integration on outcomes after major lower extremity amputation. J. Vasc. Surg. 2016, 63, 154–162. [Google Scholar] [CrossRef]
- Dillingham, T.R.; Pezzin, L.E.; MacKenzie, E.J. Limb amputation and limb deficiency: Epidemiology and recent trends in the United States. South. Med. J. 2002, 95, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Schober, T.-L.; Abrahamsen, C. Patient perspectives on major lower limb amputation–A qualitative systematic review. Int. J. Orthop. Trauma Nurs. 2022, 46, 100958. [Google Scholar] [CrossRef]
- Suckow, B.D.; Goodney, P.P.; Nolan, B.W.; Veeraswamy, R.K.; Gallagher, P.; Cronenwett, J.L.; Kraiss, L.W. Domains that determine quality of life in vascular amputees. Ann. Vasc. Surg. 2015, 29, 722–730. [Google Scholar] [CrossRef]
- Jensen, P.S.; Petersen, J.; Kirketerp-Møller, K.; Poulsen, I.; Andersen, O. Progression of disease preceding lower extremity amputation in Denmark: A longitudinal registry study of diagnoses, use of medication and healthcare services 14 years prior to amputation. BMJ Open 2017, 7, e016030. [Google Scholar] [CrossRef]
- Prost, V.; Johnson, W.B.; Kent, J.A.; Major, M.J.; Winter, A.G. Systematic Assessment of Prosthesis Stiffness on User Biomechanics Using the Lower Leg Trajectory Error Framework and Its Implication for the Design and Evaluation of Ankle-Foot Prostheses. J. Biomech. Eng. 2023, 145, 041002. [Google Scholar] [CrossRef]
- Clites, T.R.; Shepherd, M.K.; Ingraham, K.A.; Wontorcik, L.; Rouse, E.J. Understanding patient preference in prosthetic ankle stiffness. J. Neuroeng. Rehabil. 2022, 18, 128. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, M.K.; Azocar, A.F.; Major, M.J.; Rouse, E.J. Amputee perception of prosthetic ankle stiffness during locomotion. J. Neuroeng. Rehabil. 2018, 15, 99. [Google Scholar] [CrossRef] [PubMed]
- Prost, V.; Olesnavage, K.M.; Johnson, W.B.; Major, M.J.; Winter, A.G. Design and Testing of a Prosthetic Foot With Interchangeable Custom Springs for Evaluating Lower Leg Trajectory Error, an Optimization Metric for Prosthetic Feet. J. Mech. Robot. 2018, 10, 021010. [Google Scholar] [CrossRef]
- Glowinski, S.; Blazejewski, A.; Krzyzynski, T. Inertial Sensors and Wavelets Analysis as a Tool for Pathological Gait Identification. In Innovations in Biomedical Engineering; Advances in Intelligent Systems and Computing; Springer International Publishing: Cham, Switzerland, 2017; pp. 106–114. [Google Scholar]
- Zhu, R.; Zhou, Z. A real-time articulated human motion tracking using tri-axis inertial/magnetic sensors package. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 295–302. [Google Scholar] [PubMed]
- Seth, A.; Hicks, J.L.; Uchida, T.K.; Habib, A.; Dembia, C.L.; Dunne, J.J.; Ong, C.F.; DeMers, M.S.; Rajagopal, A.; Millard, M.; et al. OpenSim: Simulating musculoskeletal dynamics and neuromuscular control to study human and animal movement. PLoS Comput. Biol. 2018, 14, e1006223. [Google Scholar] [CrossRef]






| Gait with the Subjects’ Own Prosthetic Feet | Gait of the Subjects’ with Free-Flow Foot | Able-Bodied Subjects | |
|---|---|---|---|
| K1 | 3.053 | ||
| K2 | 5.299 | 8.936 | |
| IA | 5.883 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pitkin, M. The Moment Criterion of Anthropomorphicity of Prosthetic Feet as a Potential Predictor of Their Functionality for Transtibial Amputees. Biomimetics 2023, 8, 572. https://doi.org/10.3390/biomimetics8080572
Pitkin M. The Moment Criterion of Anthropomorphicity of Prosthetic Feet as a Potential Predictor of Their Functionality for Transtibial Amputees. Biomimetics. 2023; 8(8):572. https://doi.org/10.3390/biomimetics8080572
Chicago/Turabian StylePitkin, Mark. 2023. "The Moment Criterion of Anthropomorphicity of Prosthetic Feet as a Potential Predictor of Their Functionality for Transtibial Amputees" Biomimetics 8, no. 8: 572. https://doi.org/10.3390/biomimetics8080572
APA StylePitkin, M. (2023). The Moment Criterion of Anthropomorphicity of Prosthetic Feet as a Potential Predictor of Their Functionality for Transtibial Amputees. Biomimetics, 8(8), 572. https://doi.org/10.3390/biomimetics8080572







