Recent Developments of Silk-Based Scaffolds for Tissue Engineering and Regenerative Medicine Applications: A Special Focus on the Advancement of 3D Printing
Abstract
1. Introduction
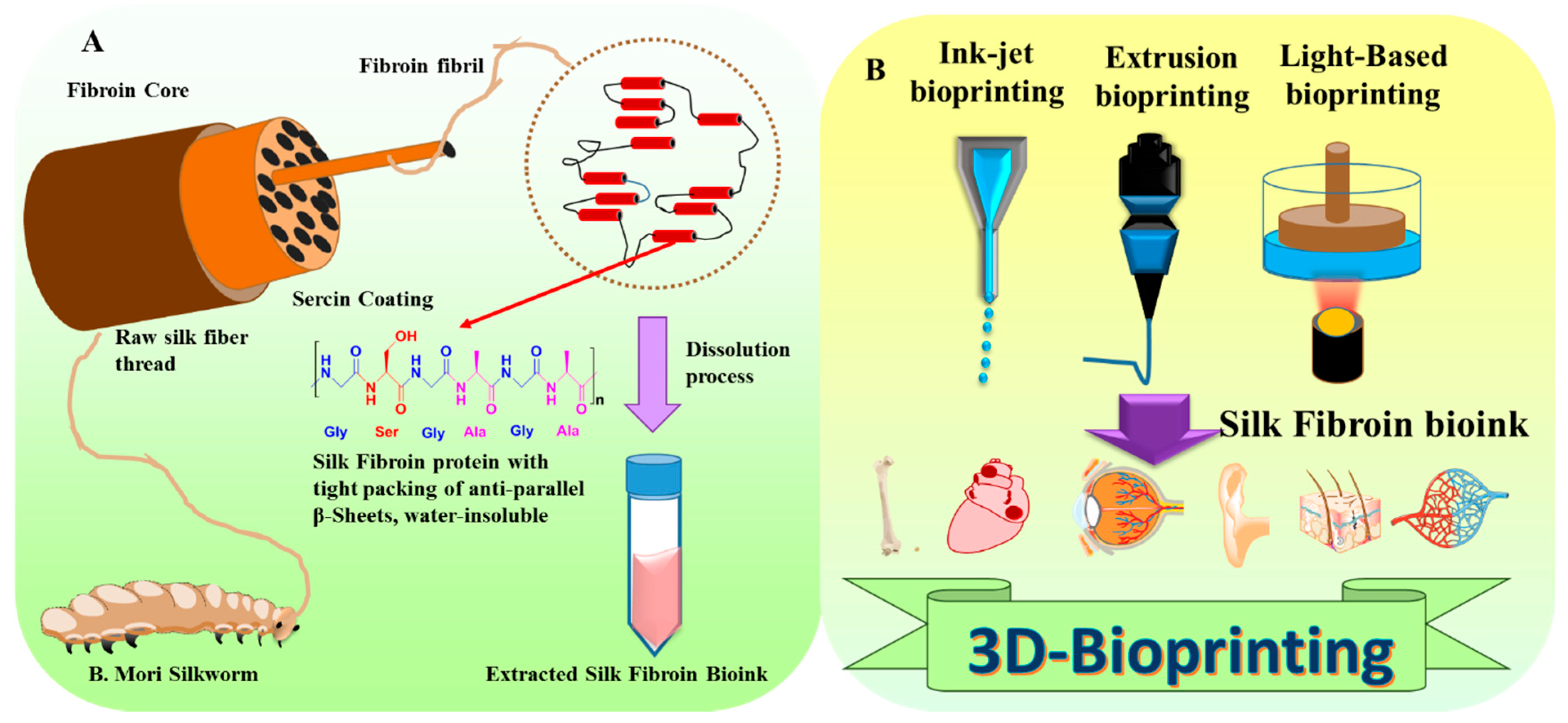
2. Sources, Structure, and Chemistry of Silks Derived from the Silkworms
3. Features of Silk Fibroin as a Biomaterial
3.1. Physical Properties
3.2. Biodegradability
3.3. Biological Competency
3.4. Modifying the Qualities of Silk by Altering the Structure
4. Structural Diversification of Silk Biomaterials
4.1. Innate Silk Structures
4.2. Silk Films
4.3. Wet-Spun and Electro-Spun Fibers
4.4. Silk Hydrogels
4.5. 3D Porous Silk Scaffolds
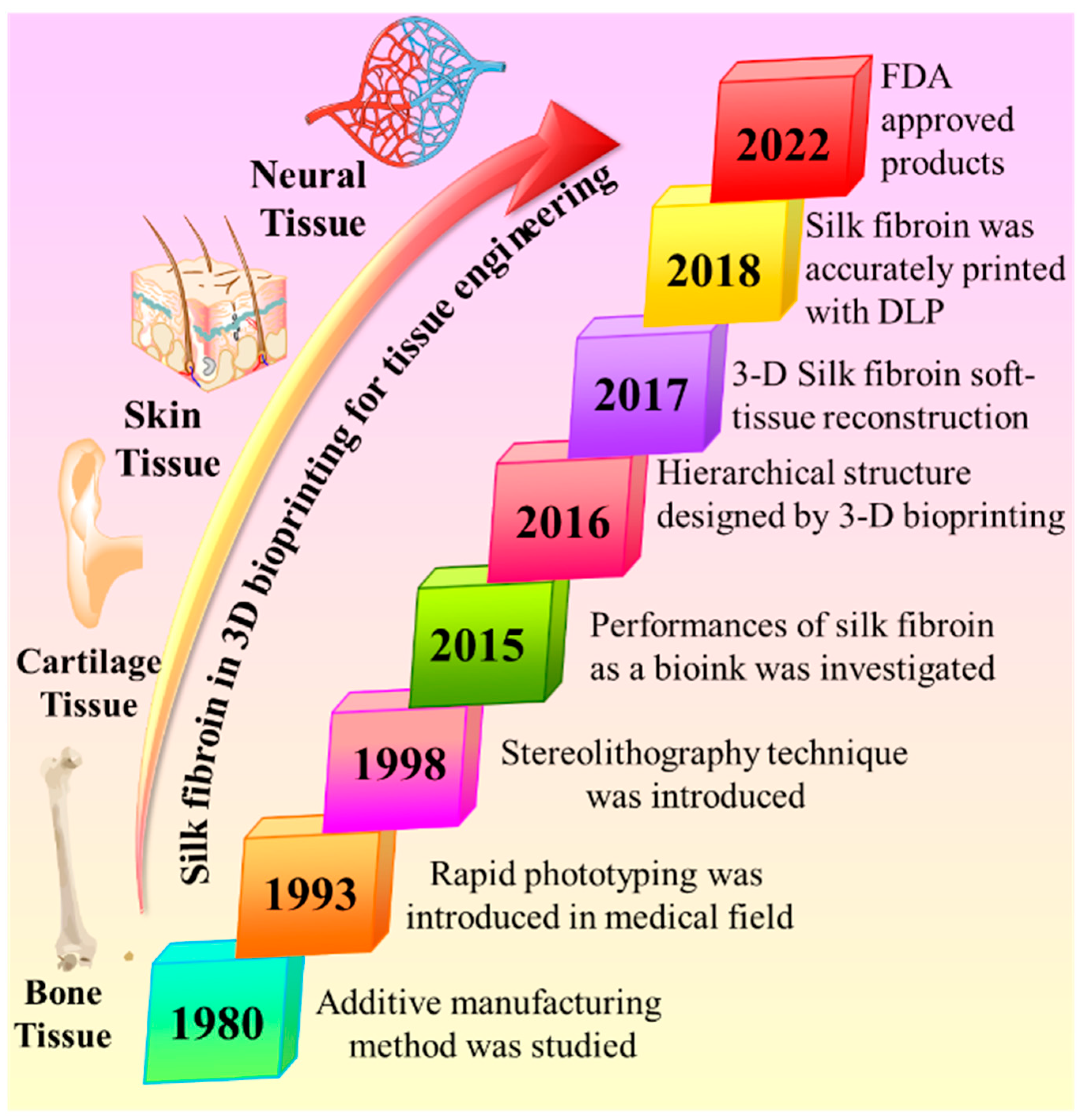
5. 3D Bioprinting in the Tissue Engineering Field
6. 3D Bioprinting Technology for Silk Fibroin Bioinks
6.1. Inkjet Bioprinting
6.2. Extrusion Bioprinting
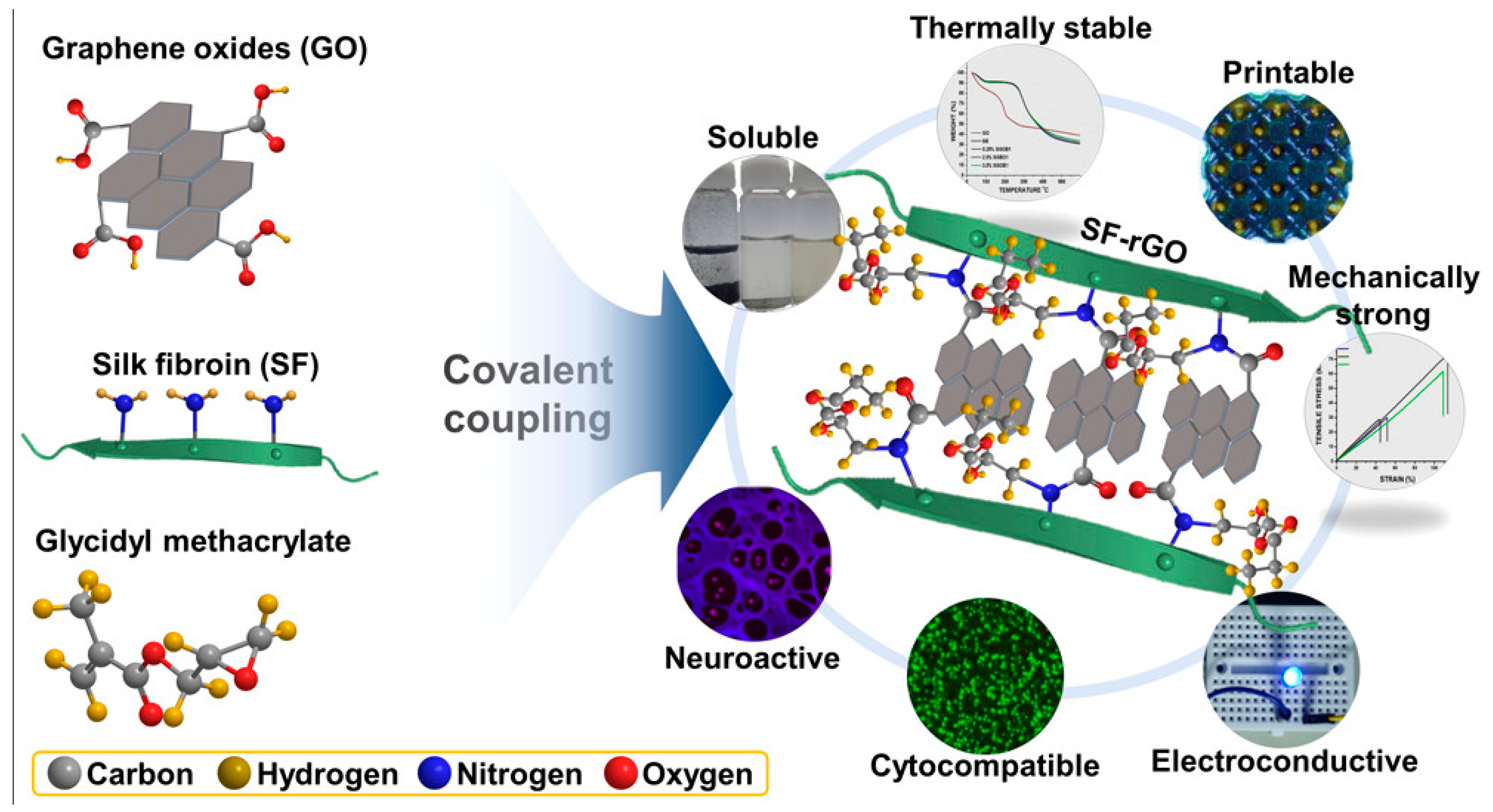
6.3. Light-Based Bioprinting
7. Applications of 3D Bioprinting Based on Silk Fibroin
7.1. 3D Bone Tissue Engineering
7.2. 3D Cartilage Tissue Engineering
7.3. 3D Neural Tissue Engineering
7.4. 3D Skin Tissue Engineering
8. Challenges in Translating Silk Fibroin into the Medical Market
9. Clinical Trials and Commercial Medical Products
10. Future Perspectives
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Jain, P.; Kathuria, H.; Dubey, N. Advances in 3D bioprinting of tissues/organs for regenerative medicine and in-vitro models. Biomaterials 2022, 287, 121639. [Google Scholar] [CrossRef]
- Paul, K.; Darzi, S.; McPhee, G.; Del Borgo, M.P.; Werkmeister, J.A.; Gargett, C.E.; Mukherjee, S. 3D bioprinted endometrial stem cells on melt electrospun poly ε-caprolactone mesh for pelvic floor application promote anti-inflammatory responses in mice. Acta Biomater. 2019, 97, 162–176. [Google Scholar] [CrossRef] [PubMed]
- Filippi, M.; Preziosa, P.; Rocca, M.A. Brain mapping in multiple sclerosis: Lessons learned about the human brain. Neuroimage 2019, 190, 32–45. [Google Scholar] [CrossRef] [PubMed]
- Lui, Y.S.; Sow, W.T.; Tan, L.P.; Wu, Y.; Lai, Y.; Li, H. 4D printing and stimuli-responsive materials in biomedical aspects. Acta Biomater. 2019, 92, 19–36. [Google Scholar] [CrossRef] [PubMed]
- Salaris, F.; Rosa, A. Construction of 3D in vitro models by bioprinting human pluripotent stem cells: Challenges and opportunities. Brain Res. 2019, 1723, 146393. [Google Scholar] [CrossRef] [PubMed]
- Su, X.; Wang, T.; Guo, S. Applications of 3D printed bone tissue engineering scaffolds in the stem cell field. Regen. Ther. 2021, 16, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Alonzo, M.; AnilKumar, S.; Roman, B.; Tasnim, N.; Joddar, B. 3D Bioprinting of cardiac tissue and cardiac stem cell therapy. Transl. Res. 2019, 211, 64–83. [Google Scholar] [CrossRef] [PubMed]
- Gu, Z.; Fu, J.; Lin, H.; He, Y. Development of 3D bioprinting: From printing methods to biomedical applications. Asian J. Pharm. Sci. 2020, 15, 529–557. [Google Scholar] [CrossRef]
- Bhattacharjee, P.; Naskar, D.; Maiti, T.K.; Bhattacharya, D.; Kundu, S.C. Non-mulberry silk fibroin grafted poly (Є-caprolactone)/nano hydroxyapatite nanofibrous scaffold for dual growth factor delivery to promote bone regeneration. J. Colloid Interface Sci. 2016, 472, 16–33. [Google Scholar] [CrossRef] [PubMed]
- Kundu, B.; Rajkhowa, R.; Kundu, S.C.; Wang, X. Silk fibroin biomaterials for tissue regenerations. Adv. Drug Deliv. Rev. 2013, 65, 457–470. [Google Scholar] [CrossRef]
- Simionescu, B.C.; Ivanov, D. Natural and synthetic polymers for designing composite materials. In Handbook of Bioceramics and Biocomposites; Springer: Berlin/Heidelberg, Germany, 2016; pp. 233–286. [Google Scholar]
- Chen, G.; Xiao, X.; Zhao, X.; Tat, T.; Bick, M.; Chen, J. Electronic textiles for wearable point-of-care systems. Chem. Rev. 2021, 122, 3259–3291. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Huang, Y.; Bai, H.; Wang, G.; Hu, X.; Kumar, S.; Min, R. Biocompatible and biodegradable polymer optical fiber for biomedical application: A review. Biosensors 2021, 11, 472. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Hu, F.; Wu, R.; Xu, Z.; Shao, G.; Yu, R.; Liu, X.Y. New Silk Road: From Mesoscopic Reconstruction/Functionalization to Flexible Meso-Electronics/Photonics Based on Cocoon Silk Materials. Adv. Mater. 2021, 33, 2005910. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zhang, S.; Cao, Y.; Marelli, B.; Xia, X.; Tao, T.H. Engineering the future of silk materials through advanced manufacturing. Adv. Mater. 2018, 30, 1706983. [Google Scholar] [CrossRef]
- Babu, K.M. Silk: Processing, Properties and Applications; Woodhead Publishing; Elsevier imprints: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Colomban, P.; Jauzein, V. Silk: Fibers, films, and composites—Types, processing, structure, and mechanics. In Handbook of Properties of Textile and Technical Fibres; Elsevier: Amsterdam, The Netherlands, 2018; pp. 137–183. [Google Scholar]
- Srivastava, S.; Bhargava, A. Biological Synthesis of Nanoparticles: Animal Systems. In Green Nanoparticles: The Future of Nanobiotechnology; Springer: Berlin/Heidelberg, Germany, 2022; pp. 261–284. [Google Scholar]
- Tang, G.; Liu, Z.; Liu, Y.; Yu, J.; Wang, X.; Tan, Z.; Ye, X. Recent trends in the development of bone regenerative biomaterials. Front. Cell Dev. Biol. 2021, 9, 665813. [Google Scholar] [CrossRef] [PubMed]
- Meyer, H.-P.; Werbitzky, O. Development of Swiss Biotechnology Beyond the Biopharmaceutical Sector In memoriam Prof. Dr. Oreste Ghisalba (1946–2018). Chimia 2020, 74, 345. [Google Scholar] [CrossRef]
- Xu, H.-L.; Chen, P.-P.; Wang, L.-F.; Xue, W.; Fu, T.-L. Hair regenerative effect of silk fibroin hydrogel with incorporation of FGF-2-liposome and its potential mechanism in mice with testosterone-induced alopecia areata. J. Drug Deliv. Sci. Technol. 2018, 48, 128–136. [Google Scholar] [CrossRef]
- Bojedla, S.S.R.; Chameettachal, S.; Yeleswarapu, S.; Nikzad, M.; Masood, S.H.; Pati, F. Silk fibroin microfiber-reinforced polycaprolactone composites with enhanced biodegradation and biological characteristics. J. Biomed. Mater. Res. Part A 2022, 110, 1386–1400. [Google Scholar] [CrossRef]
- Zhang, Z.; Ai, S.; Yang, Z.; Li, X. Peptide-based supramolecular hydrogels for local drug delivery. Adv. Drug Deliv. Rev. 2021, 174, 482–503. [Google Scholar] [CrossRef]
- Hao, Z.; Long, D.; Zhang, Y.; Umuhoza, D.; Dai, J.; Xu, Z.; Zhang, G.; Meng, W.; Xiang, Z.; Zhao, A. New insight into the mechanism of in vivo fibroin self-assembly and secretion in the silkworm, Bombyx mori. Int. J. Biol. Macromol. 2021, 169, 473–479. [Google Scholar] [CrossRef]
- Song, K.; Wang, Y.; Dong, W.; Li, Z.; He, H.; Zhu, P.; Xia, Q. Silkworm spinning: The programmed self-assembly from natural silk fibroin to superfibre. bioRxiv 2021. [Google Scholar] [CrossRef]
- Carlson, M.; Hansen, A.; Levin, T.; Rick, M.; Tallqvist, F.; Tiefensee, M. Streamlining the manufacturing of biotherapeutics: SPPS vs. Recombinant protein production. 2021. Available online: https://www.diva-portal.org/smash/record.jsf?pid=diva2%3A1560723&dswid=2356 (accessed on 20 October 2022).
- Yang, Y.; Yao, X.; Li, X.; Guo, C.; Li, C.; Liu, L.; Zhou, Z. Non-mulberry silk fiber-based scaffolds reinforced by PLLA porous microspheres for auricular cartilage: An in vitro study. Int. J. Biol. Macromol. 2021, 182, 1704–1712. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.P.; Nguyen, Q.V.; Nguyen, V.-H.; Le, T.-H.; Huynh, V.Q.N.; Vo, D.-V.N.; Trinh, Q.T.; Kim, S.Y.; Le, Q.V. Silk fibroin-based biomaterials for biomedical applications: A review. Polymers 2019, 11, 1933. [Google Scholar] [CrossRef] [PubMed]
- McGill, M.; Holland, G.P.; Kaplan, D.L. Experimental methods for characterizing the secondary structure and thermal properties of silk proteins. Macromol. Rapid Commun. 2019, 40, 1800390. [Google Scholar] [CrossRef] [PubMed]
- Kiseleva, A.P.; Krivoshapkin, P.V.; Krivoshapkina, E.F. Recent advances in development of functional spider silk-based hybrid materials. Front. Chem. 2020, 8, 554. [Google Scholar] [CrossRef]
- Fu, C.; Wang, Y.; Guan, J.; Chen, X.; Vollrath, F.; Shao, Z. Cryogenic toughness of natural silk and a proposed structure–function relationship. Mater. Chem. Front. 2019, 3, 2507–2513. [Google Scholar] [CrossRef]
- Yousef, M.; Hassabo, A.G. Puncture resistance properties of natural and synthetic fabrics. J. Text. Color. Polym. Sci. 2021, 18, 211–228. [Google Scholar] [CrossRef]
- Li, G.; Li, Y.; Chen, G.; He, J.; Han, Y.; Wang, X.; Kaplan, D.L. Silk-based biomaterials in biomedical textiles and fiber-based implants. Adv. Healthc. Mater. 2015, 4, 1134–1151. [Google Scholar] [CrossRef]
- Belbéoch, C.; Lejeune, J.; Vroman, P.; Salaün, F. Silkworm and spider silk electrospinning: A review. Environ. Chem. Lett. 2021, 19, 1737–1763. [Google Scholar] [CrossRef]
- Craig, H.C. Unravelling the Secrets of Silk: An In-Depth Biochemical Analysis of Spider and Silkworm Silk. Ph.D. Thesis, UNSW Sydney, Sydney, NSW, Australia, 2019. [Google Scholar]
- Kaur, M.; Singh, K. Review on titanium and titanium based alloys as biomaterials for orthopaedic applications. Mater. Sci. Eng. C 2019, 102, 844–862. [Google Scholar] [CrossRef]
- Jin, D.; Hu, J.; Xia, D.; Kuang, H.; Du, J.; Mo, X.; Yin, M. Evaluation of a simple off-the-shelf bi-layered vascular scaffold based on poly (L-lactide-co-ε-caprolactone)/silk fibroin in vitro and in vivo. Int. J. Nanomed. 2019, 14, 4261. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Xiao, L.; Ding, Z.; Lu, Q.; Kaplan, D.L. Fragile-Tough Mechanical Reversion of Silk Materials via Tuning Supramolecular Assembly. ACS Biomater. Sci. Eng. 2021, 7, 2337–2345. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhang, W.; Hu, Y.; Fei, Y.; Liu, H.; Huang, Z.; Wang, C.; Ruan, D.; Heng, B.C.; Chen, W. Systematic review of silk scaffolds in musculoskeletal tissue engineering applications in the recent decade. ACS Biomater. Sci. Eng. 2021, 7, 817–840. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhou, S.; Wang, L.; You, R.; Yan, S.; Zhang, Q.; Li, M. Bioactive silk fibroin scaffold with nanoarchitecture for wound healing. Compos. Part B Eng. 2021, 224, 109165. [Google Scholar] [CrossRef]
- Zhang, F.; King, M.W. Biodegradable polymers as the pivotal player in the design of tissue engineering scaffolds. Adv. Healthc. Mater. 2020, 9, 1901358. [Google Scholar] [CrossRef]
- Elgarahy, A.; Elwakeel, K.; Mohammad, S.; Elshoubaky, G. A critical review of biosorption of dyes, heavy metals and metalloids from wastewater as an efficient and green process. Clean. Eng. Technol. 2021, 4, 100209. [Google Scholar] [CrossRef]
- Falcucci, T.; Presley, K.F.; Choi, J.; Fizpatrick, V.; Barry, J.; Kishore Sahoo, J.; Ly, J.T.; Grusenmeyer, T.A.; Dalton, M.J.; Kaplan, D.L. Degradable Silk-Based Subcutaneous Oxygen Sensors. Adv. Funct. Mater. 2022, 2202020. [Google Scholar] [CrossRef]
- Muley, A.B.; Shingote, P.R.; Patil, A.P.; Dalvi, S.G.; Suprasanna, P. Gamma radiation degradation of chitosan for application in growth promotion and induction of stress tolerance in potato (Solanum tuberosum L.). Carbohydr. Polym. 2019, 210, 289–301. [Google Scholar] [CrossRef]
- Owen, R.; Reilly, G.C. In vitro models of bone remodelling and associated disorders. Front. Bioeng. Biotechnol. 2018, 6, 134. [Google Scholar] [CrossRef]
- Huang, G.; Li, F.; Zhao, X.; Ma, Y.; Li, Y.; Lin, M.; Jin, G.; Lu, T.J.; Genin, G.M.; Xu, F. Functional and biomimetic materials for engineering of the three-dimensional cell microenvironment. Chem. Rev. 2017, 117, 12764–12850. [Google Scholar] [PubMed]
- Reddy, M.S.B.; Ponnamma, D.; Choudhary, R.; Sadasivuni, K.K. A comparative review of natural and synthetic biopolymer composite scaffolds. Polymers 2021, 13, 1105. [Google Scholar] [CrossRef] [PubMed]
- Chouhan, D.; Mandal, B.B. Silk biomaterials in wound healing and skin regeneration therapeutics: From bench to bedside. Acta Biomater. 2020, 103, 24–51. [Google Scholar] [CrossRef]
- Holland, C.; Numata, K.; Rnjak-Kovacina, J.; Seib, F.P. The biomedical use of silk: Past, present, future. Adv. Healthc. Mater. 2019, 8, 1800465. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Hu, D.A.; Wu, D.; He, F.; Wang, H.; Huang, L.; Shi, D.; Liu, Q.; Ni, N.; Pakvasa, M. Applications of biocompatible scaffold materials in stem cell-based cartilage tissue engineering. Front. Bioeng. Biotechnol. 2021, 9, 603444. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, S.; Sakiragaoglu, O.; Chirila, T.V. Study of the Antioxidative Effects of Bombyx mori Silk Sericin in Cultures of Murine Retinal Photoreceptor Cells. Molecules 2022, 27, 4635. [Google Scholar] [CrossRef] [PubMed]
- Ma, D.; Wang, Y.; Dai, W. Silk fibroin-based biomaterials for musculoskeletal tissue engineering. Mater. Sci. Eng. C 2018, 89, 456–469. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.P. Developing Translational Tissue Engineering Solutions for Regenerative Medicine. Ph.D. Thesis, The University of Sydney, Sydney, NSW, Australia, 2018. [Google Scholar]
- Zhao, T.; Chu, Z.; Ma, J.; Ouyang, L. Immunomodulation effect of biomaterials on bone formation. J. Funct. Biomater. 2022, 13, 103. [Google Scholar] [CrossRef]
- Janani, G.; Kumar, M.; Chouhan, D.; Moses, J.C.; Gangrade, A.; Bhattacharjee, S.; Mandal, B.B. Insight into silk-based biomaterials: From physicochemical attributes to recent biomedical applications. ACS Appl. Bio Mater. 2019, 2, 5460–5491. [Google Scholar] [CrossRef]
- Bucciarelli, A.; Motta, A. Use of Bombyx mori silk fibroin in tissue engineering: From cocoons to medical devices, challenges, and future perspectives. Biomater. Adv. 2022, 139, 212982. [Google Scholar] [CrossRef]
- Williams, D.F. Challenges with the development of biomaterials for sustainable tissue engineering. Front. Bioeng. Biotechnol. 2019, 7, 127. [Google Scholar] [CrossRef]
- Yang, D.; Xiao, J.; Wang, B.; Li, L.; Kong, X.; Liao, J. The immune reaction and degradation fate of scaffold in cartilage/bone tissue engineering. Mater. Sci. Eng. C 2019, 104, 109927. [Google Scholar] [CrossRef] [PubMed]
- Akintayo, O.; Olajide, J.; Betiku, O.; Egoh, A.; Adegbesan, O.; Daramola, O.; Sadiku, E.; Desai, D. Poly (lactic acid)-silkworm silk fibre/fibroin bio-composites: A review of their processing, properties, and nascent applications. Express Polym. Lett. 2020, 14, 924–951. [Google Scholar] [CrossRef]
- Shang, L.; Yu, Y.; Liu, Y.; Chen, Z.; Kong, T.; Zhao, Y. Spinning and applications of bioinspired fiber systems. ACS Nano 2019, 13, 2749–2772. [Google Scholar] [CrossRef]
- Chakraborty, T.; Sarma, A.; Das, M.K. Silk fibroin: A smart biomaterial for long term and targeted nanotherapeutics. Curr. Trends 2016, 3, 45–82. [Google Scholar]
- Low, J.T.; Yusoff, N.I.S.M.; Othman, N.; Wong, T.W.; Wahit, M.U. Silk fibroin-based films in food packaging applications: A review. Compr. Rev. Food Sci. Food Saf. 2022, 21, 2253–2273. [Google Scholar] [CrossRef]
- Tandon, S.; Kandasubramanian, B.; Ibrahim, S.M. Silk-based composite scaffolds for tissue engineering applications. Ind. Eng. Chem. Res. 2020, 59, 17593–17611. [Google Scholar] [CrossRef]
- Fonseca, A.C.; Melchels, F.P.; Ferreira, M.J.; Moxon, S.R.; Potjewyd, G.; Dargaville, T.R.; Kimber, S.J.; Domingos, M. Emulating human tissues and organs: A bioprinting perspective toward personalized medicine. Chem. Rev. 2020, 120, 11093–11139. [Google Scholar] [CrossRef]
- Tomeh, M.A.; Hadianamrei, R.; Zhao, X. Silk fibroin as a functional biomaterial for drug and gene delivery. Pharmaceutics 2019, 11, 494. [Google Scholar] [CrossRef]
- Babu, K.M. Silk from silkworms and spiders as high-performance fibers. In Structure and Properties of High-Performance Fibers; Elsevier: Amsterdam, The Netherlands, 2017; pp. 327–366. [Google Scholar]
- Kostag, M.; Jedvert, K.; El Seoud, O.A. Engineering of sustainable biomaterial composites from cellulose and silk fibroin: Fundamentals and applications. Int. J. Biol. Macromol. 2021, 167, 687–718. [Google Scholar] [CrossRef]
- Chen, W.; Li, F.; Chen, L.; Zhang, Y.; Zhang, T.; Wang, T. Fast self-assembly of microporous silk fibroin membranes on liquid surface. Int. J. Biol. Macromol. 2020, 156, 633–639. [Google Scholar] [CrossRef]
- Yao, X.; Zou, S.; Fan, S.; Niu, Q.; Zhang, Y. Bioinspired silk fibroin materials: From silk building blocks extraction and reconstruction to advanced biomedical applications. Mater. Today Bio 2022, 16, 100381. [Google Scholar] [CrossRef]
- Tudureanu, R.; Handrea-Dragan, I.M.; Boca, S.; Botiz, I. Insight and Recent Advances into the Role of Topography on the Cell Differentiation and Proliferation on Biopolymeric Surfaces. Int. J. Mol. Sci. 2022, 23, 7731. [Google Scholar] [CrossRef]
- Han, S.; Nie, K.; Li, J.; Sun, Q.; Wang, X.; Li, X.; Li, Q. 3D Electrospun Nanofiber-Based Scaffolds: From Preparations and Properties to Tissue Regeneration Applications. Stem Cells Int. 2021, 2021, 8790143. [Google Scholar] [CrossRef]
- Wani, S.U.D.; Gautam, S.P.; Qadrie, Z.L.; Gangadharappa, H.V. Silk fibroin as a natural polymeric based bio-material for tissue engineering and drug delivery systems-A review. Int. J. Biol. Macromol. 2020, 163, 2145–2161. [Google Scholar] [CrossRef] [PubMed]
- Horne, J.; McLoughlin, L.; Bridgers, B.; Wujcik, E.K. Recent developments in nanofiber-based sensors for disease detection, immunosensing, and monitoring. Sens. Actuators Rep. 2020, 2, 100005. [Google Scholar] [CrossRef]
- Mozafari, M.; Rajadas, J.; Kaplan, D. Nanoengineered Biomaterials for Regenerative Medicine; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Zhao, Y.; Zhu, Z.S.; Guan, J.; Wu, S.J. Processing, mechanical properties and bio-applications of silk fibroin-based high-strength hydrogels. Acta Biomater. 2021, 125, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.; Qiao, K.; Wang, Y.; Zheng, Y.; He, W.; Xie, Y.; Yang, H. Injectable and biodegradable double-network nanocomposite hydrogel with regulable sol-gel transition process and mechanical properties. Polym. Test. 2022, 106, 107452. [Google Scholar] [CrossRef]
- Zhang, W.; Zhang, Y.; Zhang, A.; Ling, C.; Sheng, R.; Li, X.; Yao, Q.; Chen, J. Enzymatically crosslinked silk-nanosilicate reinforced hydrogel with dual-lineage bioactivity for osteochondral tissue engineering. Mater. Sci. Eng. C 2021, 127, 112215. [Google Scholar] [CrossRef]
- Haider, A.; Haider, S.; Rao Kummara, M.; Kamal, T.; Alghyamah, A.-A.A.; Jan Iftikhar, F.; Bano, B.; Khan, N.; Amjid Afridi, M.; Soo Han, S.; et al. Advances in the scaffolds fabrication techniques using biocompatible polymers and their biomedical application: A technical and statistical review. J. Saudi Chem. Soc. 2020, 24, 186–215. [Google Scholar] [CrossRef]
- Shahbazi, M.-A.; Ghalkhani, M.; Maleki, H. Directional Freeze-Casting: A Bioinspired Method to Assemble Multifunctional Aligned Porous Structures for Advanced Applications. Adv. Eng. Mater. 2020, 22, 2000033. [Google Scholar] [CrossRef]
- Lemos, R.; Maia, F.R.; Ribeiro, V.P.; Costa, J.B.; Coutinho, P.J.G.; Reis, R.L.; Oliveira, J.M. Carbon nanotube-reinforced cell-derived matrix-silk fibroin hierarchical scaffolds for bone tissue engineering applications. J. Mater. Chem. B 2021, 9, 9561–9574. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Mei, L.; Wang, F.; Pei, B.; Li, X. The Potential Matrix and Reinforcement Materials for the Preparation of the Scaffolds Reinforced by Fibers or Tubes for Tissue Repair. In Tissue Repair: Reinforced Scaffolds; Li, X., Ed.; Springer Singapore: Singapore, 2017; pp. 25–77. [Google Scholar] [CrossRef]
- Utech, S.; Boccaccini, A.R. A review of hydrogel-based composites for biomedical applications: Enhancement of hydrogel properties by addition of rigid inorganic fillers. J. Mater. Sci. 2016, 51, 271–310. [Google Scholar] [CrossRef]
- Xu, T.; Yang, H.; Yang, D.; Yu, Z.-Z. Polylactic Acid Nanofiber Scaffold Decorated with Chitosan Islandlike Topography for Bone Tissue Engineering. ACS Appl. Mater. Interfaces 2017, 9, 21094–21104. [Google Scholar] [CrossRef]
- Hamidi, Y.K.; Yalcinkaya, M.A.; Guloglu, G.E.; Pishvar, M.; Amirkhosravi, M.; Altan, M.C. Silk as a Natural Reinforcement: Processing and Properties of Silk/Epoxy Composite Laminates. Materials 2018, 11, 2135. [Google Scholar] [CrossRef] [PubMed]
- Turnbull, G.; Clarke, J.; Picard, F.; Riches, P.; Jia, L.; Han, F.; Li, B.; Shu, W. 3D bioactive composite scaffolds for bone tissue engineering. Bioact. Mater. 2018, 3, 278–314. [Google Scholar] [CrossRef]
- Park, S.-H.; Jung, C.S.; Min, B.-H. Advances in three-dimensional bioprinting for hard tissue engineering. Tissue Eng. Regen. Med. 2016, 13, 622–635. [Google Scholar] [CrossRef]
- Guvendiren, M.; Molde, J.; Soares, R.M.D.; Kohn, J. Designing Biomaterials for 3D Printing. ACS Biomater. Sci. Eng. 2016, 2, 1679–1693. [Google Scholar] [CrossRef]
- Yang, Y.; Song, X.; Li, X.; Chen, Z.; Zhou, C.; Zhou, Q.; Chen, Y. Recent Progress in Biomimetic Additive Manufacturing Technology: From Materials to Functional Structures. Adv. Mater. 2018, 30, 1706539. [Google Scholar] [CrossRef]
- DeSimone, E.; Schacht, K.; Pellert, A.; Scheibel, T. Recombinant spider silk-based bioinks. Biofabrication 2017, 9, 044104. [Google Scholar] [CrossRef]
- Moon, B.M.; Choi, M.-J.; Sultan, M.T.; Yang, J.W.; Ju, H.W.; Lee, J.M.; Park, H.J.; Park, Y.R.; Kim, S.H.; Kim, D.W.; et al. Novel fabrication method of the peritoneal dialysis filter using silk fibroin with urease fixation system. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017, 105, 2136–2144. [Google Scholar] [CrossRef]
- Vasconcelos, A.; Gomes, A.C.; Cavaco-Paulo, A. Novel silk fibroin/elastin wound dressings. Acta Biomater. 2012, 8, 3049–3060. [Google Scholar] [CrossRef]
- Gao, F.; Xu, Z.; Liang, Q.; Liu, B.; Li, H.; Wu, Y.; Zhang, Y.; Lin, Z.; Wu, M.; Ruan, C.; et al. Direct 3D Printing of High Strength Biohybrid Gradient Hydrogel Scaffolds for Efficient Repair of Osteochondral Defect. Adv. Funct. Mater. 2018, 28, 1706644. [Google Scholar] [CrossRef]
- Garcia-Fuentes, M.; Meinel, A.J.; Hilbe, M.; Meinel, L.; Merkle, H.P. Silk fibroin/hyaluronan scaffolds for human mesenchymal stem cell culture in tissue engineering. Biomaterials 2009, 30, 5068–5076. [Google Scholar] [CrossRef] [PubMed]
- Porter, D.; Vollrath, F. Silk as a Biomimetic Ideal for Structural Polymers. Adv. Mater. 2009, 21, 487–492. [Google Scholar] [CrossRef]
- Brenckle, M.A.; Tao, H.; Kim, S.; Paquette, M.; Kaplan, D.L.; Omenetto, F.G. Protein-Protein Nanoimprinting of Silk Fibroin Films. Adv. Mater. 2013, 25, 2409–2414. [Google Scholar] [CrossRef] [PubMed]
- Guo, N.; Leu, M.C. Additive manufacturing: Technology, applications and research needs. Front. Mech. Eng. 2013, 8, 215–243. [Google Scholar] [CrossRef]
- Kruth, J.P.; Leu, M.C.; Nakagawa, T. Progress in Additive Manufacturing and Rapid Prototyping. CIRP Ann. 1998, 47, 525–540. [Google Scholar] [CrossRef]
- Webb, P.A. A review of rapid prototyping (RP) techniques in the medical and biomedical sector. J. Med. Eng. Technol. 2000, 24, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Jose, R.R.; Brown, J.E.; Polido, K.E.; Omenetto, F.G.; Kaplan, D.L. Polyol-Silk Bioink Formulations as Two-Part Room-Temperature Curable Materials for 3D Printing. ACS Biomater. Sci. Eng. 2015, 1, 780–788. [Google Scholar] [CrossRef] [PubMed]
- Sommer, M.R.; Schaffner, M.; Carnelli, D.; Studart, A.R. 3D Printing of Hierarchical Silk Fibroin Structures. ACS Appl. Mater. Interfaces 2016, 8, 34677–34685. [Google Scholar] [CrossRef]
- Rodriguez, M.J.; Brown, J.; Giordano, J.; Lin, S.J.; Omenetto, F.G.; Kaplan, D.L. Silk based bioinks for soft tissue reconstruction using 3-dimensional (3D) printing with in vitro and in vivo assessments. Biomaterials 2017, 117, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Yeon, Y.K.; Lee, J.M.; Chao, J.R.; Lee, Y.J.; Seo, Y.B.; Sultan, M.T.; Lee, O.J.; Lee, J.S.; Yoon, S.-I.; et al. Precisely printable and biocompatible silk fibroin bioink for digital light processing 3D printing. Nat. Commun. 2018, 9, 1620. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Abdulla, R.; Parker, B.; Samanipour, R.; Ghosh, S.; Kim, K. A simple and high-resolution stereolithography-based 3D bioprinting system using visible light crosslinkable bioinks. Biofabrication 2015, 7, 045009. [Google Scholar] [CrossRef]
- Ozbolat, I.T.; Yu, Y. Bioprinting Toward Organ Fabrication: Challenges and Future Trends. IEEE Trans. Biomed. Eng. 2013, 60, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Hopp, B.; Smausz, T.; Szabó, G.; Kolozsvari, L.; Nogradi, A.; Kafetzopoulos, D.; Fotakis, C. Femtosecond laser printing of living cells using absorbing film-assisted laser-induced forward transfer. Opt. Eng. 2012, 51, 014302. [Google Scholar] [CrossRef]
- Hölzl, K.; Lin, S.; Tytgat, L.; Van Vlierberghe, S.; Gu, L.; Ovsianikov, A. Bioink properties before, during and after 3D bioprinting. Biofabrication 2016, 8, 032002. [Google Scholar] [CrossRef]
- Xu, T.; Baicu, C.; Aho, M.; Zile, M.; Boland, T. Fabrication and characterization of bio-engineered cardiac pseudo tissues. Biofabrication 2009, 1, 035001. [Google Scholar] [CrossRef]
- Billiet, T.; Vandenhaute, M.; Schelfhout, J.; Van Vlierberghe, S.; Dubruel, P. A review of trends and limitations in hydrogel-rapid prototyping for tissue engineering. Biomaterials 2012, 33, 6020–6041. [Google Scholar] [CrossRef]
- Dai, X.; Liu, L.; Ouyang, J.; Li, X.; Zhang, X.; Lan, Q.; Xu, T. Coaxial 3D bioprinting of self-assembled multicellular heterogeneous tumor fibers. Sci. Rep. 2017, 7, 1457. [Google Scholar] [CrossRef]
- Saunders, R.E.; Derby, B. Inkjet printing biomaterials for tissue engineering: Bioprinting. Int. Mater. Rev. 2014, 59, 430–448. [Google Scholar] [CrossRef]
- Murphy, S.V.; Atala, A. 3D bioprinting of tissues and organs. Nat. Biotechnol. 2014, 32, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Guillotin, B.; Catros, S.; Guillemot, F. Laser Assisted Bio-printing (LAB) of Cells and Bio-materials Based on Laser Induced Forward Transfer (LIFT). In Laser Technology in Biomimetics: Basics and Applications; Schmidt, V., Belegratis, M.R., Eds.; Springer: Berlin, Heidelberg, Germany, 2013; pp. 193–209. [Google Scholar] [CrossRef]
- Karzyński, K.; Kosowska, K.; Ambrożkiewicz, F.; Berman, A.; Cichoń, J.; Klak, M.; Serwańska-Świętek, M.; Wszoła, M. Use of 3D bioprinting in biomedical engineering for clinical application. Med. Stud. Stud. Med. 2018, 34, 93–97. [Google Scholar] [CrossRef]
- Tao, H.; Marelli, B.; Yang, M.; An, B.; Onses, M.S.; Rogers, J.A.; Kaplan, D.L.; Omenetto, F.G. Inkjet Printing of Regenerated Silk Fibroin: From Printable Forms to Printable Functions. Adv. Mater. 2015, 27, 4273–4279. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liu, B.; Pei, B.; Chen, J.; Zhou, D.; Peng, J.; Zhang, X.; Jia, W.; Xu, T. Inkjet Bioprinting of Biomaterials. Chem. Rev. 2020, 120, 10793–10833. [Google Scholar] [CrossRef]
- Pereira, F.; Parfenov, V.; Khesuani, Y.; Ovsianikov, A.; Mironov, V. 3D Printing and Biofabrication; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Bishop, E.S.; Mostafa, S.; Pakvasa, M.; Luu, H.H.; Lee, M.J.; Wolf, J.M.; Ameer, G.A.; He, T.-C.; Reid, R.R. 3-D bioprinting technologies in tissue engineering and regenerative medicine: Current and future trends. Genes Dis. 2017, 4, 185–195. [Google Scholar] [CrossRef]
- Rider, P.M.; Brook, I.M.; Smith, P.J.; Miller, C.A. Reactive Inkjet Printing of Regenerated Silk Fibroin Films for Use as Dental Barrier Membranes. Micromachines 2018, 9, 46. [Google Scholar] [CrossRef]
- Compaan, A.M.; Christensen, K.; Huang, Y. Inkjet Bioprinting of 3D Silk Fibroin Cellular Constructs Using Sacrificial Alginate. ACS Biomater. Sci. Eng. 2017, 3, 1519–1526. [Google Scholar] [CrossRef]
- Suntivich, R.; Drachuk, I.; Calabrese, R.; Kaplan, D.L.; Tsukruk, V.V. Inkjet Printing of Silk Nest Arrays for Cell Hosting. Biomacromolecules 2014, 15, 1428–1435. [Google Scholar] [CrossRef]
- He, Y.; Gu, Z.; Xie, M.; Fu, J.; Lin, H. Why choose 3D bioprinting? Part II: Methods and bioprinters. Bio-Des. Manuf. 2020, 3, 1–4. [Google Scholar] [CrossRef]
- Jiang, T.; Munguia-Lopez, J.G.; Flores-Torres, S.; Kort-Mascort, J.; Kinsella, J.M. Extrusion bioprinting of soft materials: An emerging technique for biological model fabrication. Appl. Phys. Rev. 2019, 6, 011310. [Google Scholar] [CrossRef]
- Ozbolat, I.T.; Moncal, K.K.; Gudapati, H. Evaluation of bioprinter technologies. Addit. Manuf. 2017, 13, 179–200. [Google Scholar] [CrossRef]
- Zheng, Z.; Wu, J.; Liu, M.; Wang, H.; Li, C.; Rodriguez, M.J.; Li, G.; Wang, X.; Kaplan, D.L. 3D Bioprinting of Self-Standing Silk-Based Bioink. Adv. Healthc. Mater. 2018, 7, 1701026. [Google Scholar] [CrossRef]
- Wang, H.-Y.; Zhang, Y.-Q.; Wei, Z.-G. Characterization of undegraded and degraded silk fibroin and its significant impact on the properties of the resulting silk biomaterials. Int. J. Biol. Macromol. 2021, 176, 578–588. [Google Scholar] [CrossRef] [PubMed]
- Sakai, S.; Yoshii, A.; Sakurai, S.; Horii, K.; Nagasuna, O. Silk fibroin nanofibers: A promising ink additive for extrusion three-dimensional bioprinting. Mater. Today Bio 2020, 8, 100078. [Google Scholar] [CrossRef] [PubMed]
- Yusupov, V.; Churbanov, S.; Churbanova, E.; Bardakova, K.; Antoshin, A.; Evlashin, S.; Timashev, P.; Minaev, N. Laser-induced forward transfer hydrogel printing: A defined route for highly controlled process. Int. J. Bioprinting 2020, 6, 271. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Kim, D.Y.; Lim, T.H.; Park, C.H. Silk Fibroin Bioinks for Digital Light Processing (DLP) 3D Bioprinting. In Bioinspired Biomaterials: Advances in Tissue Engineering and Regenerative Medicine; Chun, H.J., Reis, R.L., Motta, A., Khang, G., Eds.; Springer: Singapore, 2020; pp. 53–66. [Google Scholar] [CrossRef]
- Lee, H.; Kwak, H.; Na, K.; Shin, S.; Shin, D.; Hyun, J. Noncytotoxic biocomposite hydrogel fabricated by digital light processing 3D printing. In Proceedings of the ECCM 2018–18th European Conference on Composite Materials, Athens, Greece, 24–28th June 2018. [Google Scholar]
- Ajiteru, O.; Sultan, M.T.; Lee, Y.J.; Seo, Y.B.; Hong, H.; Lee, J.S.; Lee, H.; Suh, Y.J.; Ju, H.W.; Lee, O.J.; et al. A 3D Printable Electroconductive Biocomposite Bioink Based on Silk Fibroin-Conjugated Graphene Oxide. Nano Lett. 2020, 20, 6873–6883. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Eglin, D.; Alini, M.; Richards, G.R.; Qin, L.; Lai, Y. Visible Light-Induced 3D Bioprinting Technologies and Corresponding Bioink Materials for Tissue Engineering: A Review. Engineering 2021, 7, 966–978. [Google Scholar] [CrossRef]
- Nieto, D.; Corrales, J.A.M.; Mora, A.J.d.; Moroni, L. Fundamentals of light-cell–polymer interactions in photo-cross-linking based bioprinting. APL Bioeng. 2020, 4, 041502. [Google Scholar] [CrossRef]
- Florencio-Silva, R.; Sasso, G.R.d.S.; Sasso-Cerri, E.; Simões, M.J.; Cerri, P.S. Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. BioMed. Res. Int. 2015, 2015, 421746. [Google Scholar] [CrossRef]
- Buckwalter, J.; Glimcher, M.; Cooper, R.; Recker, R. Bone biology. I: Structure, blood supply, cells, matrix, and mineralization. Instr. Course Lect. 1996, 45, 371–386. [Google Scholar]
- Roach, H.I. Why does bone matrix contain non-collagenous proteins? The possible roles of osteocalcin, osteonectin, osteopontin and bone sialoprotein in bone mineralisation and resorption. Cell Biol. Int. 1994, 18, 617–628. [Google Scholar] [CrossRef] [PubMed]
- Olszta, M.J.; Cheng, X.; Jee, S.S.; Kumar, R.; Kim, Y.-Y.; Kaufman, M.J.; Douglas, E.P.; Gower, L.B. Bone structure and formation: A new perspective. Mater. Sci. Eng. R Rep. 2007, 58, 77–116. [Google Scholar] [CrossRef]
- Frantz, C.; Stewart, K.M.; Weaver, V.M. The extracellular matrix at a glance. J. Cell Sci. 2010, 123, 4195–4200. [Google Scholar] [CrossRef] [PubMed]
- Amini, A.R.; Laurencin, C.T.; Nukavarapu, S.P. Bone Tissue Engineering: Recent Advances and Challenges. Crit. Rev. Biomed. Eng. 2012, 40, 363–408. [Google Scholar] [CrossRef]
- Melke, J.; Midha, S.; Ghosh, S.; Ito, K.; Hofmann, S. Silk fibroin as biomaterial for bone tissue engineering. Acta Biomater. 2016, 31, 1–16. [Google Scholar] [CrossRef]
- Chawla, S.; Midha, S.; Sharma, A.; Ghosh, S. Silk-Based Bioinks for 3D Bioprinting. Adv. Healthc. Mater. 2018, 7, 1701204. [Google Scholar] [CrossRef]
- Das, S.; Pati, F.; Choi, Y.-J.; Rijal, G.; Shim, J.-H.; Kim, S.W.; Ray, A.R.; Cho, D.-W.; Ghosh, S. Bioprintable, cell-laden silk fibroin–gelatin hydrogel supporting multilineage differentiation of stem cells for fabrication of three-dimensional tissue constructs. Acta Biomater. 2015, 11, 233–246. [Google Scholar] [CrossRef]
- Chawla, S.; Sharma, A.; Bandyopadhyay, A.; Ghosh, S. Developmental Biology-Inspired Strategies To Engineer 3D Bioprinted Bone Construct. ACS Biomater. Sci. Eng. 2018, 4, 3545–3560. [Google Scholar] [CrossRef]
- Wei, L.; Wu, S.; Kuss, M.; Jiang, X.; Sun, R.; Reid, P.; Qin, X.; Duan, B. 3D printing of silk fibroin-based hybrid scaffold treated with platelet rich plasma for bone tissue engineering. Bioact. Mater. 2019, 4, 256–260. [Google Scholar] [CrossRef]
- Huang, T.; Fan, C.; Zhu, M.; Zhu, Y.; Zhang, W.; Li, L. 3D-printed scaffolds of biomineralized hydroxyapatite nanocomposite on silk fibroin for improving bone regeneration. Appl. Surf. Sci. 2019, 467–468, 345–353. [Google Scholar] [CrossRef]
- Yang, J.; Deng, C.; Shafiq, M.; Li, Z.; Zhang, Q.; Du, H.; Li, S.; Zhou, X.; He, C. Localized delivery of FTY-720 from 3D printed cell-laden gelatin/silk fibroin composite scaffolds for enhanced vascularized bone regeneration. Smart Mater. Med. 2022, 3, 217–229. [Google Scholar] [CrossRef]
- Sophia Fox, A.J.; Bedi, A.; Rodeo, S.A. The Basic Science of Articular Cartilage: Structure, Composition, and Function. Sport. Health 2009, 1, 461–468. [Google Scholar] [CrossRef]
- Ai, C.; Lee, Y.H.D.; Tan, X.H.; Tan, S.H.S.; Hui, J.H.P.; Goh, J.C.-H. Osteochondral tissue engineering: Perspectives for clinical application and preclinical development. J. Orthop. Transl. 2021, 30, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhou, G.; Cao, Y. Recent Progress in Cartilage Tissue Engineering—Our Experience and Future Directions. Engineering 2017, 3, 28–35. [Google Scholar] [CrossRef]
- Lu, Q.; Hu, X.; Wang, X.; Kluge, J.A.; Lu, S.; Cebe, P.; Kaplan, D.L. Water-insoluble silk films with silk I structure. Acta Biomater. 2010, 6, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Cheng, G.; Davoudi, Z.; Xing, X.; Yu, X.; Cheng, X.; Li, Z.; Deng, H.; Wang, Q. Advanced Silk Fibroin Biomaterials for Cartilage Regeneration. ACS Biomater. Sci. Eng. 2018, 4, 2704–2715. [Google Scholar] [CrossRef]
- Marelli, B.; Patel, N.; Duggan, T.; Perotto, G.; Shirman, E.; Li, C.; Kaplan, D.L.; Omenetto, F.G. Programming function into mechanical forms by directed assembly of silk bulk materials. Proc. Natl. Acad. Sci. USA 2017, 114, 451–456. [Google Scholar] [CrossRef]
- Chameettachal, S.; Midha, S.; Ghosh, S. Regulation of Chondrogenesis and Hypertrophy in Silk Fibroin-Gelatin-Based 3D Bioprinted Constructs. ACS Biomater. Sci. Eng. 2016, 2, 1450–1463. [Google Scholar] [CrossRef]
- Shi, W.; Sun, M.; Hu, X.; Ren, B.; Cheng, J.; Li, C.; Duan, X.; Fu, X.; Zhang, J.; Chen, H.; et al. Structurally and Functionally Optimized Silk-Fibroin–Gelatin Scaffold Using 3D Printing to Repair Cartilage Injury In Vitro and In Vivo. Adv. Mater. 2017, 29, 1701089. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, Y.; Zuo, Q.; Wang, Q.; Li, Z.; Yan, K.; Yuan, T.; Zhang, Y.; Shen, K.; Xie, R. 3D bioprinting of biomimetic bilayered scaffold consisting of decellularized extracellular matrix and silk fibroin for osteochondral repair. Int. J. Bioprinting 2021, 7, 401. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, Y.; Luo, C.; Zhai, C.; Li, Z.; Zhang, Y.; Yuan, T.; Dong, S.; Zhang, J.; Fan, W. Crosslinker-free silk/decellularized extracellular matrix porous bioink for 3D bioprinting-based cartilage tissue engineering. Mater. Sci. Eng. C 2021, 118, 111388. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.M.; VanDusen, K.W.; Kostrominova, T.Y.; Mertens, J.P.; Larkin, L.M. Scaffoldless tissue-engineered nerve conduit promotes peripheral nerve regeneration and functional recovery after tibial nerve injury in rats. Neural Regen. Res. 2017, 12, 1529. [Google Scholar] [PubMed]
- Ray, W.Z.; Mahan, M.A.; Guo, D.; Guo, D.; Kliot, M. An update on addressing important peripheral nerve problems: Challenges and potential solutions. Acta Neurochir. 2017, 159, 1765–1773. [Google Scholar] [CrossRef]
- Grinsell, D.; Keating, C.P. Peripheral Nerve Reconstruction after Injury: A Review of Clinical and Experimental Therapies. BioMed Res. Int. 2014, 2014, 698256. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, Y.; Gong, J.; Yang, L.; Niu, C.; Ni, X.; Wang, Y.; Peng, S.; Gu, X.; Sun, C.; et al. Chitosan degradation products facilitate peripheral nerve regeneration by improving macrophage-constructed microenvironments. Biomaterials 2017, 134, 64–77. [Google Scholar] [CrossRef]
- Trappmann, B.; Gautrot, J.E.; Connelly, J.T.; Strange, D.G.T.; Li, Y.; Oyen, M.L.; Cohen Stuart, M.A.; Boehm, H.; Li, B.; Vogel, V.; et al. Extracellular-matrix tethering regulates stem-cell fate. Nat. Mater. 2012, 11, 642–649. [Google Scholar] [CrossRef]
- Di Cio, S.; Gautrot, J.E. Cell sensing of physical properties at the nanoscale: Mechanisms and control of cell adhesion and phenotype. Acta Biomater. 2016, 30, 26–48. [Google Scholar] [CrossRef]
- Boni, R.; Ali, A.; Shavandi, A.; Clarkson, A.N. Current and novel polymeric biomaterials for neural tissue engineering. J. Biomed. Sci. 2018, 25, 90. [Google Scholar] [CrossRef]
- Knowlton, S.; Anand, S.; Shah, T.; Tasoglu, S. Bioprinting for Neural Tissue Engineering. Trends Neurosci. 2018, 41, 31–46. [Google Scholar] [CrossRef]
- Madhusudanan, P.; Raju, G.; Shankarappa, S. Hydrogel systems and their role in neural tissue engineering. J. R. Soc. Interface 2020, 17, 20190505. [Google Scholar] [CrossRef]
- Zhao, Y.-H.; Niu, C.-M.; Shi, J.-Q.; Wang, Y.-Y.; Yang, Y.-M.; Wang, H.-B. Novel conductive polypyrrole/silk fibroin scaffold for neural tissue repair. Neural Regen. Res. 2018, 13, 1455. [Google Scholar] [PubMed]
- Li, G.; Chen, K.; You, D.; Xia, M.; Li, W.; Fan, S.; Chai, R.; Zhang, Y.; Li, H.; Sun, S. Laminin-Coated Electrospun Regenerated Silk Fibroin Mats Promote Neural Progenitor Cell Proliferation, Differentiation, and Survival in vitro. Front. Bioeng. Biotechnol. 2019, 7, 190. [Google Scholar] [CrossRef]
- Liang, Y.; Goh, J.C.-H. Polypyrrole-incorporated conducting constructs for tissue engineering applications: A review. Bioelectricity 2020, 2, 101–119. [Google Scholar] [CrossRef]
- Sun, W.; Taylor, C.S.; Zhang, Y.; Gregory, D.A.; Tomeh, M.A.; Haycock, J.W.; Smith, P.J.; Wang, F.; Xia, Q.; Zhao, X. Cell guidance on peptide micropatterned silk fibroin scaffolds. J. Colloid Interface Sci. 2021, 603, 380–390. [Google Scholar] [CrossRef]
- Bouwstra, J.A.; Honeywell-Nguyen, P.L. Skin structure and mode of action of vesicles. Adv. Drug Deliv. Rev. 2002, 54, S41–S55. [Google Scholar] [CrossRef] [PubMed]
- Khalili, S.; Khorasani, S.N.; Razavi, S.M.; Hashemibeni, B.; Tamayol, A. Nanofibrous Scaffolds with Biomimetic Composition for Skin Regeneration. Appl. Biochem. Biotechnol. 2019, 187, 1193–1203. [Google Scholar] [CrossRef]
- Kwak, H.; Shin, S.; Lee, H.; Hyun, J. Formation of a keratin layer with silk fibroin-polyethylene glycol composite hydrogel fabricated by digital light processing 3D printing. J. Ind. Eng. Chem. 2019, 72, 232–240. [Google Scholar] [CrossRef]
- Xiong, S.; Zhang, X.; Lu, P.; Wu, Y.; Wang, Q.; Sun, H.; Heng, B.C.; Bunpetch, V.; Zhang, S.; Ouyang, H. A Gelatin-sulfonated Silk Composite Scaffold based on 3D Printing Technology Enhances Skin Regeneration by Stimulating Epidermal Growth and Dermal Neovascularization. Sci. Rep. 2017, 7, 4288. [Google Scholar] [CrossRef]
- Na, K.; Shin, S.; Lee, H.; Shin, D.; Baek, J.; Kwak, H.; Park, M.; Shin, J.; Hyun, J. Effect of solution viscosity on retardation of cell sedimentation in DLP 3D printing of gelatin methacrylate/silk fibroin bioink. J. Ind. Eng. Chem. 2018, 61, 340–347. [Google Scholar] [CrossRef]
- Highley, C.B.; Rodell, C.B.; Burdick, J.A. Direct 3D Printing of Shear-Thinning Hydrogels into Self-Healing Hydrogels. Adv. Mater. 2015, 27, 5075–5079. [Google Scholar] [CrossRef]
- Costa, J.B.; Silva-Correia, J.; Oliveira, J.M.; Reis, R.L. Fast Setting Silk Fibroin Bioink for Bioprinting of Patient-Specific Memory-Shape Implants. Adv. Healthc. Mater. 2017, 6, 1701021. [Google Scholar] [CrossRef]
- Costa, J.B.; Silva-Correia, J.; Ribeiro, V.P.; da Silva Morais, A.; Oliveira, J.M.; Reis, R.L. Engineering patient-specific bioprinted constructs for treatment of degenerated intervertebral disc. Mater. Today Commun. 2019, 19, 506–512. [Google Scholar] [CrossRef]
- Hong, N.; Yang, G.-H.; Lee, J.; Kim, G. 3D bioprinting and its in vivo applications. J. Biomed. Mater. Res. Part B Appl. Biomater. 2018, 106, 444–459. [Google Scholar] [CrossRef]
- Montaseri, Z.; Abolmaali, S.S.; Tamaddon, A.M.; Farvadi, F. Composite silk fibroin hydrogel scaffolds for cartilage tissue regeneration. J. Drug Deliv. Sci. Technol. 2023, 79, 104018. [Google Scholar] [CrossRef]
- Li, Z.; Jia, S.; Xiong, Z.; Long, Q.; Yan, S.; Hao, F.; Liu, J.; Yuan, Z. 3D-printed scaffolds with calcified layer for osteochondral tissue engineering. J. Biosci. Bioeng. 2018, 126, 389–396. [Google Scholar] [CrossRef]
- Jiang, J.P.; Liu, X.Y.; Zhao, F.; Zhu, X.; Li, X.Y.; Niu, X.G.; Yao, Z.T.; Dai, C.; Xu, H.Y.; Ma, K.; et al. Three-dimensional bioprinting collagen/silk fibroin scaffold combined with neural stem cells promotes nerve regeneration after spinal cord injury. Neural Regen Res. 2020, 15, 959–968. [Google Scholar] [CrossRef]
- Singh, Y.P.; Bandyopadhyay, A.; Mandal, B.B. 3D Bioprinting Using Cross-Linker-Free Silk–Gelatin Bioink for Cartilage Tissue Engineering. ACS Appl. Mater. Interfaces 2019, 11, 33684–33696. [Google Scholar] [CrossRef]
- Addition of Platelet-Rich Plasma to Silk Fibroin Hydrogel Bioprinting for Cartilage Regeneration. Tissue Eng. Part A 2020, 26, 886–895. [CrossRef]
- Nguyễn, T.T.; Ratanavaraporn, J.; Yodmuang, S. Alginate-silk fibroin Bioink: A printable hydrogel for tissue engineering. In Proceedings of the 2019 12th Biomedical Engineering International Conference (BMEiCON), Ubon Ratchathani, Thailand, 19–22 November 2019; pp. 1–4. [Google Scholar]
- Sharma, A.; Desando, G.; Petretta, M.; Chawla, S.; Bartolotti, I.; Manferdini, C.; Paolella, F.; Gabusi, E.; Trucco, D.; Ghosh, S.; et al. Investigating the Role of Sustained Calcium Release in Silk-Gelatin-Based Three-Dimensional Bioprinted Constructs for Enhancing the Osteogenic Differentiation of Human Bone Marrow Derived Mesenchymal Stromal Cells. ACS Biomater. Sci. Eng. 2019, 5, 1518–1533. [Google Scholar] [CrossRef]
- Kim, H.H.; Song, D.W.; Kim, M.J.; Ryu, S.J.; Um, I.C.; Ki, C.S.; Park, Y.H. Effect of silk fibroin molecular weight on physical property of silk hydrogel. Polymer 2016, 90, 26–33. [Google Scholar] [CrossRef]
- Cho, H.J.; Yoo, Y.J.; Kim, J.W.; Park, Y.H.; Bae, D.G.; Um, I.C. Effect of molecular weight and storage time on the wet- and electro-spinning of regenerated silk fibroin. Polym. Degrad. Stab. 2012, 97, 1060–1066. [Google Scholar] [CrossRef]
- Zhao, M.; Qi, Z.; Tao, X.; Newkirk, C.; Hu, X.; Lu, S. Chemical, Thermal, Time, and Enzymatic Stability of Silk Materials with Silk I Structure. Int. J. Mol. Sci. 2021, 22, 4136. [Google Scholar] [CrossRef]
- Xie, F.; Shao, H.; Hu, X. Effect of storage time and concentration on structure of regenerated silk fibroin solution. Int. J. Mod. Phys. B 2006, 20, 3878–3883. [Google Scholar] [CrossRef]
- Lu, Q.; Zhang, B.; Li, M.; Zuo, B.; Kaplan, D.L.; Huang, Y.; Zhu, H. Degradation Mechanism and Control of Silk Fibroin. Biomacromolecules 2011, 12, 1080–1086. [Google Scholar] [CrossRef]



| Patent No | Patent Title | Name of Inventor | Date of Publication | Main Features |
|---|---|---|---|---|
| CN-109667059-B | Method for preparing silk fibroin biological tissue engineering scaffold by solvent spraying | RogerZhang, YaopengLin, JiadongXie, Xiaofeng Zhang, Min Yu, Mingguang, Miao Lei | 7 January 2022 |
|
| CN-113926000-A | Preparation method of silk fibroin drug delivery tissue engineering scaffold | Chen Ying, Cui Xin, Wang Rong, Zhang Peipei | 14 January 2022 |
|
| WO-2022180565-A1 | Silk fibroin and related use for 3d bioprinting | Alessandra Baldwin, Christian Andrea di Buduo, Pierre-Alexandre Laurent, Erik Gatenholm, Hector MartinezItedale Redwan-Namro, Volodymyr Kuzmenko | 1 September 2022 |
|
| CN-109096501-B | Silk fibroin three-dimensional porous scaffold and preparation method thereof | Zhang Qiang, Cong Han, Yan Shuqin, Biography of You Ren, Li Xiufang, Luo Zuwei | 1 November 2022 |
|
| CN-115227871-A | Silk fibroin biomaterial ink and preparation method and application thereof | Chen Mingxue, Li Yangyang, Fang Yongcong, new Monday, Yang Dejin, Shao Hongyi, Zhang Songyang | 25 October 2022 |
|
| AU-2017359330-B2 | 3D vascularized human ocular tissue for cell therapy and drug discovery | Kapil Bharti, Russell Louis Quinn, Min Jae Song | 10 March 2022 |
|
| CN-113651974-A | Preparation method of photoinduced silk fibroin/gelatin co-crosslinked hydrogel suitable for 3D printing | Huang Yiyi, Lu Lingling, Yao Juming, Li Yongqiang, Shao Jianzhong, Sun Guangdong, Pan Xiaopeng | 16 November 2021 |
|
| CN-113527709-A | Modified tussah silk protein and 3D printing ink based on modified tussah silk protein | Gou Ma Ling, Yellow Magnolia, Yang Xiong | 22 October 2021 |
|
| CN-112843337-A | Silk bionic bioink and preparation method and application thereof | Li Fengyu, Yao Yingkai, Tang Yongtao, Liu Jing, Guan Diqin | 28 May 2021 |
|
| CN-106267370-B | Silk fibroin/cellulose 3D printing ink | Zhang Yaopeng, Huang Li, Zhu Yufang, Shao Huili, Hu Xuechao | 3 January 2020 |
|
| 3D Bioprinting Techniques | Speed/Cost | Resolution/Viscosity | Vertical Printing Ability | Cell Viability/Density | Advantages | Disadvantages | Ref |
|---|---|---|---|---|---|---|---|
| Ink-jet | Fast/Economic | 50 μm/10 m Pa s | Low | ~95%; Low | Capable of bioprinting materials, poor viscosity | Lack of continuous flow | [103,104,105,106,107,108,109,110,111,112] |
| Extrusion | Slow/Budget friendly | 100 μm/30 × 107 m Pa s | Good | ~89%; High | Capable to embed rich cell densities | Viscous liquids only | |
| Light-based | Moderate/Expensive | 10 μm/300 m Pa s | Moderate | ~85%; Medium | Both solid and liquid-phase biomaterials are used for deposition | Thermal damage due to laser irritation |
| Types of Crosslinking | Combination of Bioinks | 3D Bioprinting | In Vitro Models | Cell Density | Compressive Modulus | Printing Mode | Ref |
|---|---|---|---|---|---|---|---|
| Photo crosslinking | SF-GMA | Bone TE | NIH/3T3 | 1 × 106 mL−1 | 75–94 kPa | DLP | [173,167] |
| SF-GelMA | TE | NIH/3T3 | 1.5 × 106 mL−1 | - | DLP | [168,171] | |
| SF-PEG4A | Skin TE | NIH/3T3 | 1.5 × 106 mL−1 | 15.5 kPa | DLP | [102,169] | |
| Enzymatic crosslinking | SF-CAM | Cartilage TE | rBM-MSCs | Seeding 65% | Extrusion | [170,174] | |
| SF-G | Cartilage TE | hMSCs | 1.5 × 104 mL−1 | 18 kPa | Extrusion | [152,165] | |
| SF | TE | hASCs | 1.5 × 104 mL−1 | - | - | [175] | |
| SF/elastin | Intervertebral disc TE | hASCs | 2 × 105 mL−1 | 440 kPa | - | [176] | |
| 3DG-SF-SO3 | Skin TE | CFFs | 1 × 106 mL−1 | - | - | [172] | |
| SF-G | Cartilages TE | BMSCs | - | Extrusion | [153] | ||
| Physical/Chemical crosslinking | SF-Collagen | Knee cartilage TE | BMSCs | 2 × 107 mL−1 | - | Extrusion | [177] |
| SF-Chitosan | Cartilages TE | BMSCs | 2 × 107 mL−1 | - | Extrusion | [178] | |
| SF-Alginate | Vascular tissue engineering | NIH/3T3 | 1 × 106 mL−1 | 6.6 kPa | Inkjet | [119] | |
| SF-PEG | Cartilages TE | hMSCs | 2.5 × 106 mL−1 | - | - | [179] | |
| SF-PEG | Cartilages TE | hMSCs | 2 ×106 mL−1 | 258 kPa | Stereolithography | [124] | |
| SF- collagen | Nerve TE | - | - | - | - | [180] | |
| silk-gelatin | Cartilages TE | Chondrocytes | - | 0.1 mPa | Extrusion | [181] | |
| SF-PEG | Cartilages TE | PRP | - | 110 kPa | - | [182] | |
| Ionic crosslinking | SF-Alginate | Cartilages TE | NIH 3T3 | 1.5 × 106 mL−1 | - | Inkjet | [183] |
| SF-G | Bone TE | hMSCs | 2 × 106 mL−1 | - | - | [184] |
| Types of Classes | Details | Applications | US Regulator Path |
|---|---|---|---|
| Class I | Minimal harm to the patient | Endoscopic instruments | 5% 510 k (or) PMN approval |
| Class II (a) and (b) | (a) Moderate harm with limited period of device usage; (b) moderate harm only | Catheters, Ear-hearing tools, | 510 k (or) PMN approval with clinical proofs |
| Class III | It has 10% substantial risks | Organ implants | Approval in some special cases only |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shabbirahmed, A.M.; Sekar, R.; Gomez, L.A.; Sekhar, M.R.; Hiruthyaswamy, S.P.; Basavegowda, N.; Somu, P. Recent Developments of Silk-Based Scaffolds for Tissue Engineering and Regenerative Medicine Applications: A Special Focus on the Advancement of 3D Printing. Biomimetics 2023, 8, 16. https://doi.org/10.3390/biomimetics8010016
Shabbirahmed AM, Sekar R, Gomez LA, Sekhar MR, Hiruthyaswamy SP, Basavegowda N, Somu P. Recent Developments of Silk-Based Scaffolds for Tissue Engineering and Regenerative Medicine Applications: A Special Focus on the Advancement of 3D Printing. Biomimetics. 2023; 8(1):16. https://doi.org/10.3390/biomimetics8010016
Chicago/Turabian StyleShabbirahmed, Asma Musfira, Rajkumar Sekar, Levin Anbu Gomez, Medidi Raja Sekhar, Samson Prince Hiruthyaswamy, Nagaraj Basavegowda, and Prathap Somu. 2023. "Recent Developments of Silk-Based Scaffolds for Tissue Engineering and Regenerative Medicine Applications: A Special Focus on the Advancement of 3D Printing" Biomimetics 8, no. 1: 16. https://doi.org/10.3390/biomimetics8010016
APA StyleShabbirahmed, A. M., Sekar, R., Gomez, L. A., Sekhar, M. R., Hiruthyaswamy, S. P., Basavegowda, N., & Somu, P. (2023). Recent Developments of Silk-Based Scaffolds for Tissue Engineering and Regenerative Medicine Applications: A Special Focus on the Advancement of 3D Printing. Biomimetics, 8(1), 16. https://doi.org/10.3390/biomimetics8010016









