Adverse Effects Due to the Use of Upper Limbs Exoskeletons in the Work Environment: A Scoping Review
Abstract
1. Introduction
2. Methodology
2.1. Inclusion Criteria
2.2. Exclusion Criteria
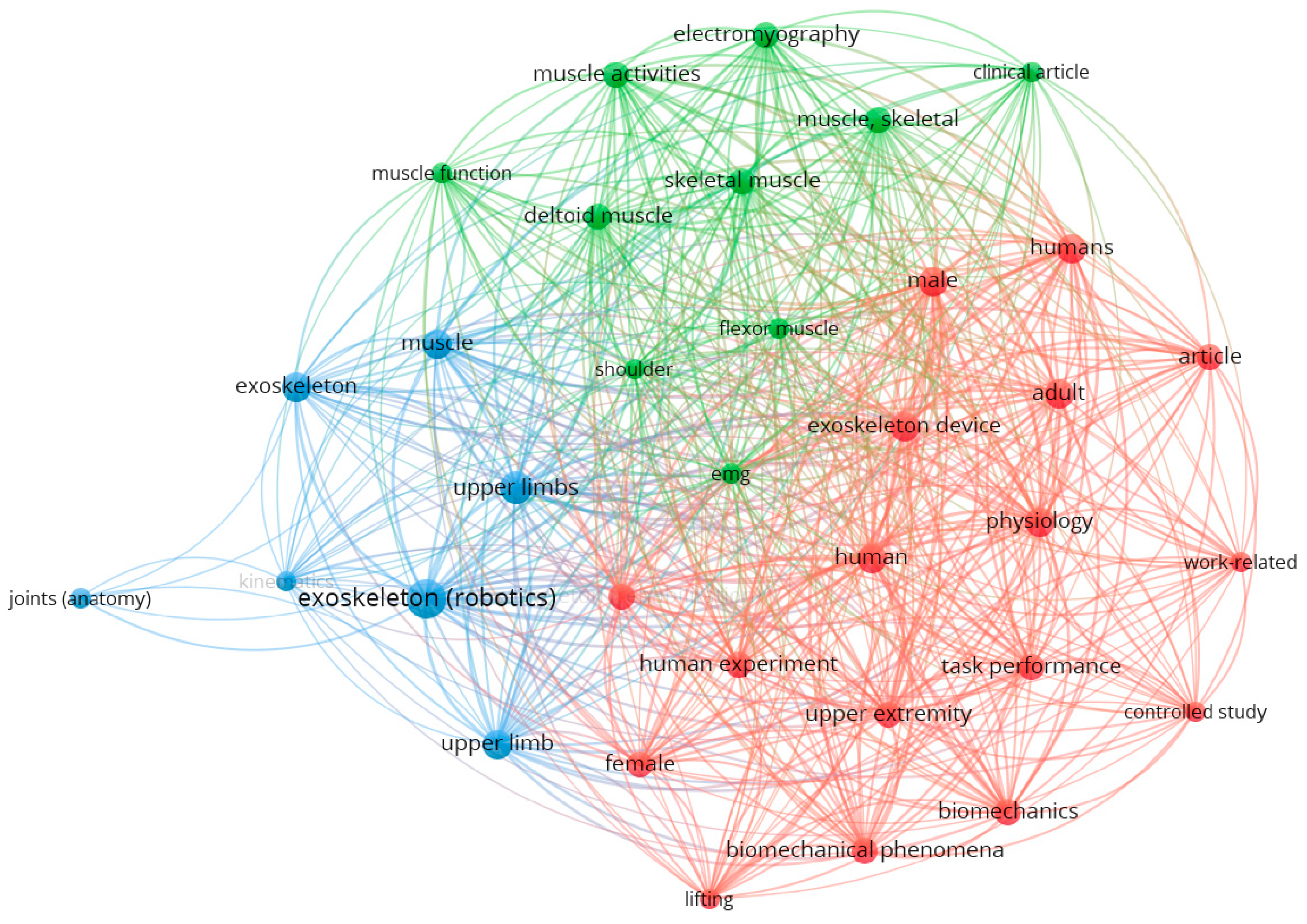
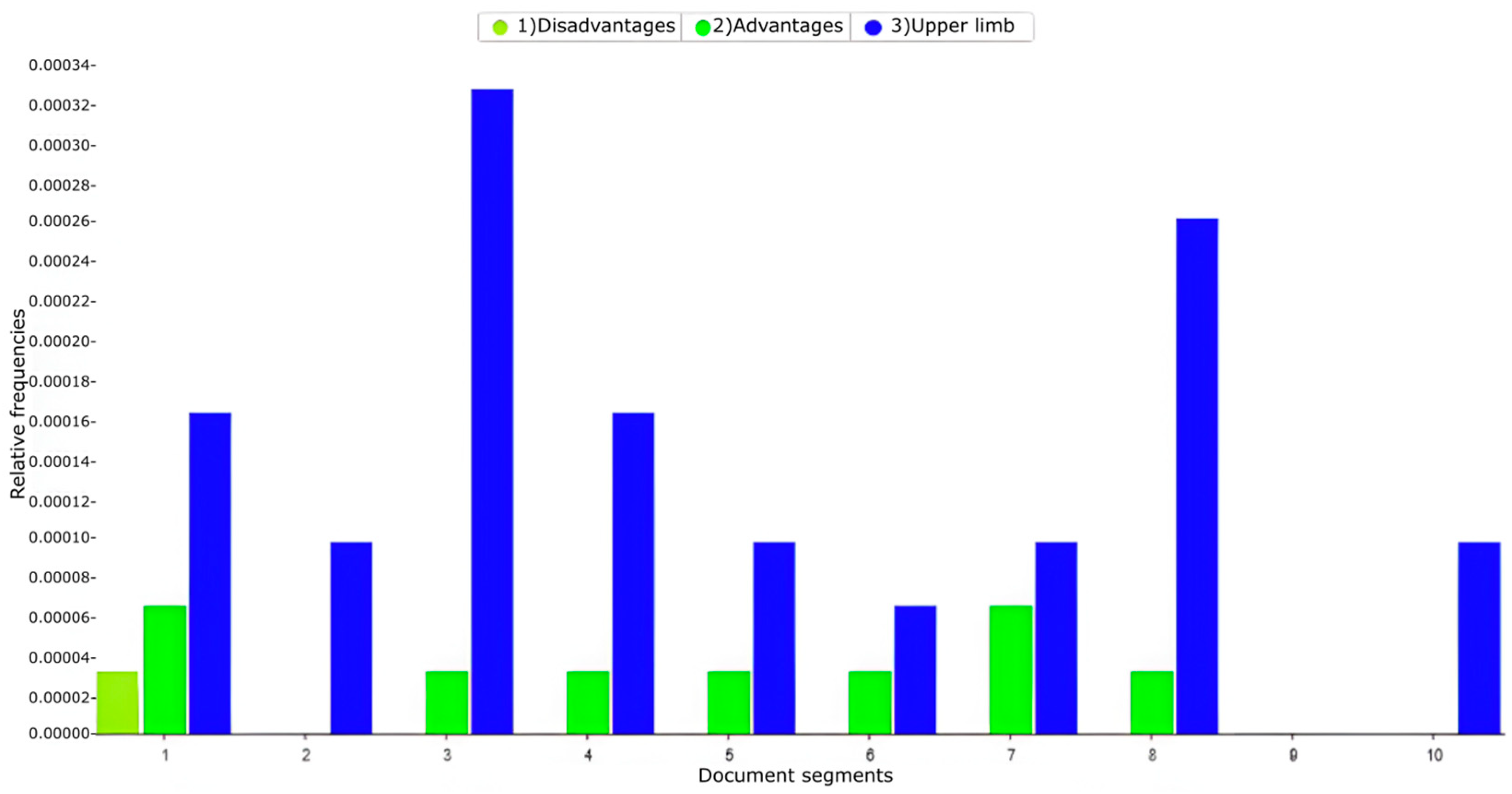
3. Results
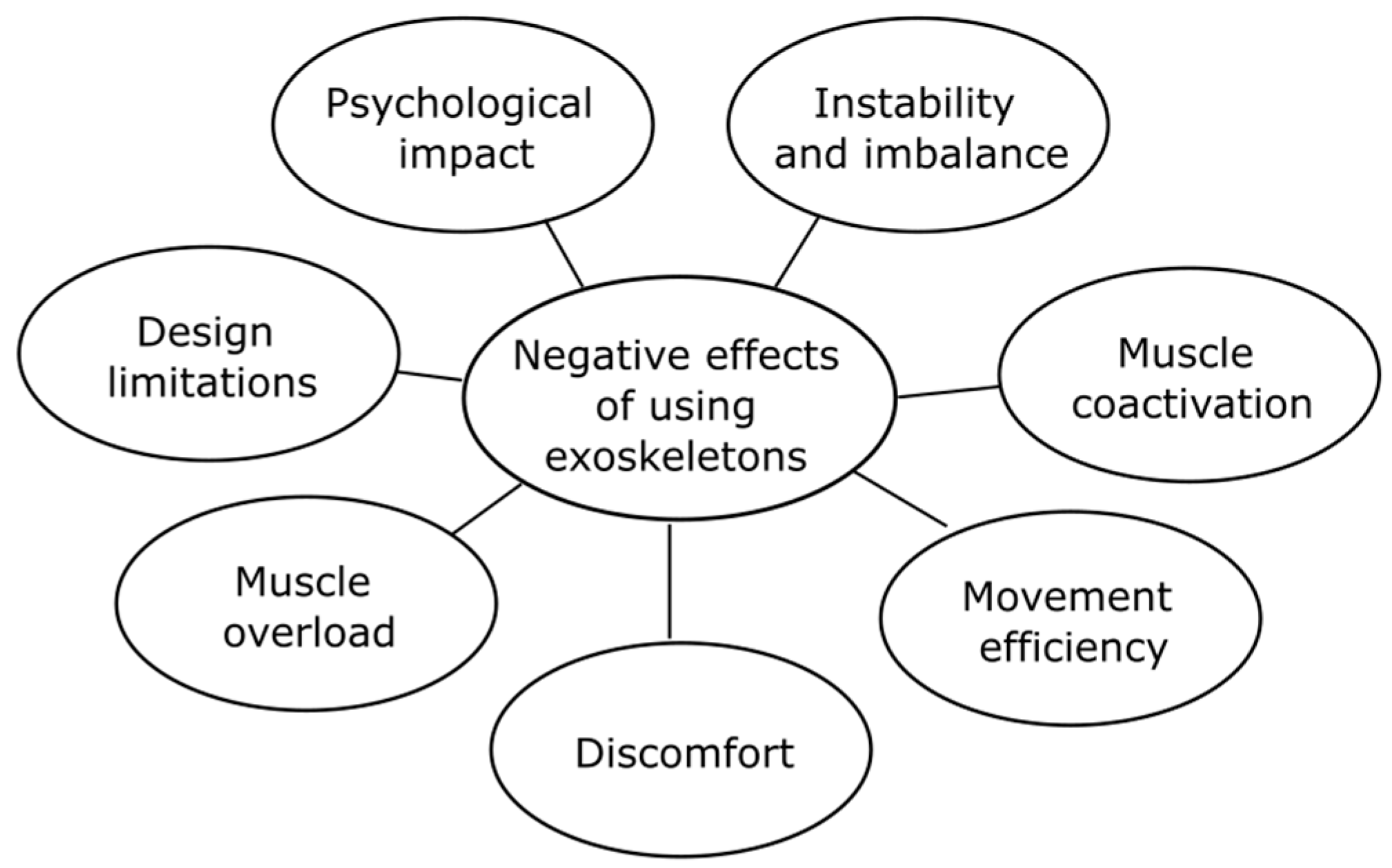
3.1. Negative Effects Due to the Use of Upper-Limb Exoskeletons in the Work Environment
3.2. Potential Risks Associated with Prolonged Use of Exoskeletons in the Workplace
3.3. Impact of Using Exoskeletons During Repetitive Tasks
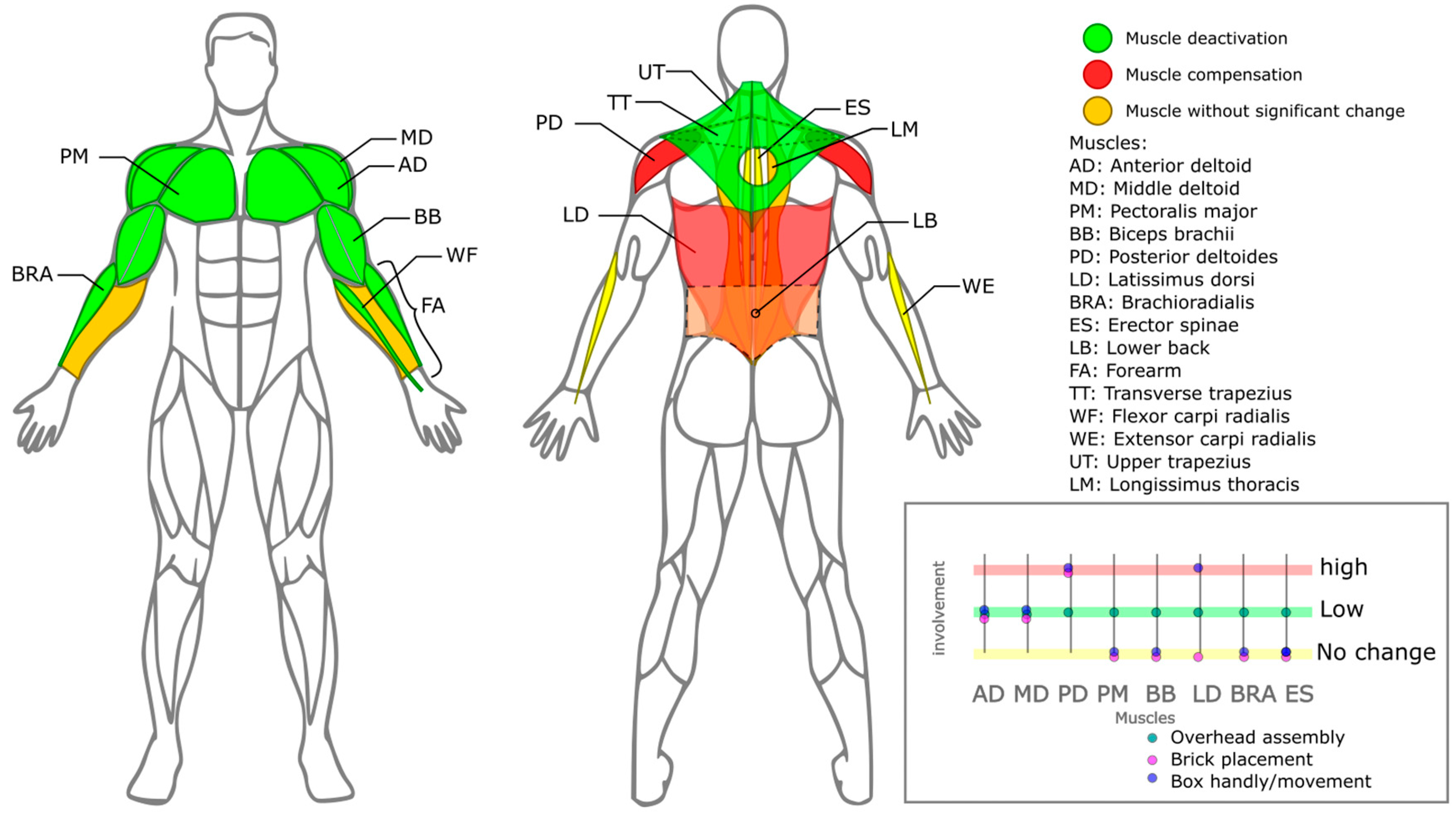
3.3.1. Physiological Effects
3.3.2. Psychological Effects
3.3.3. Adverse Effects on Technology
3.3.4. Adverse Effects on Productivity and Task Completion
3.4. Alternative Solutions to Reduce Adverse Effects on Exoskeletons
3.4.1. Ergonomic Aspects
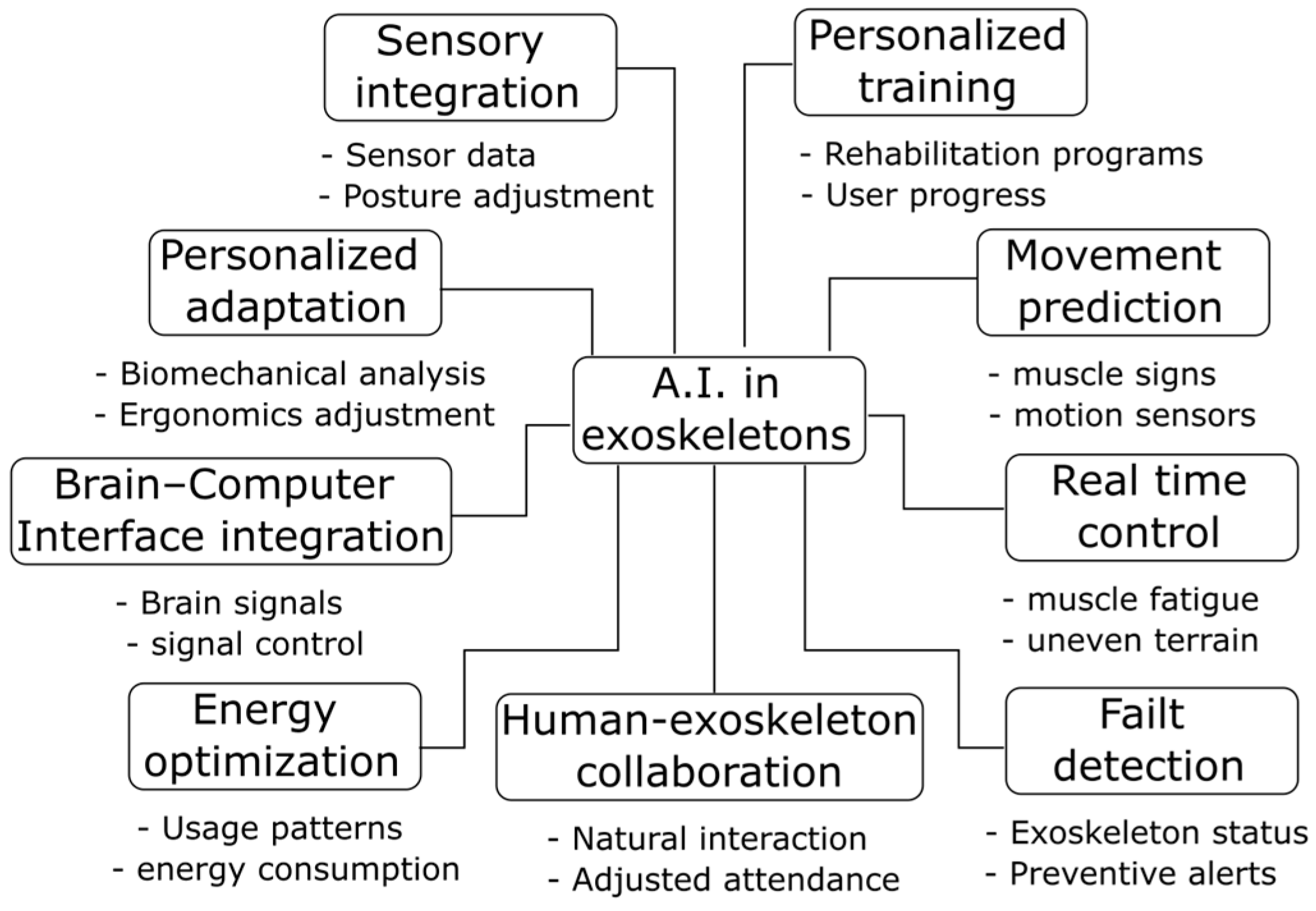
3.4.2. Use of Artificial Intelligence
3.5. Limitations in Implementing Solutions to Reduce the Negative Effects of the Exoskeleton and User Interaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| SECTION | ITEM | PRISMA-ScR CHECKLIST ITEM | REPORTED ON PAGE |
| TITLE | |||
| Title | 1 | Identify the report as a scoping review. | 1 |
| ABSTRACT | |||
| Structured summary | 2 | Provide a structured summary that includes (as applicable): background, objectives, eligibility criteria, sources of evidence, charting methods, results, and conclusions that relate to the review questions and objectives. | 1 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. Explain why the review questions/objectives lend themselves to a scoping review approach. | 1, 2, 3, 4 |
| Objectives | 4 | Provide an explicit statement of the questions and objectives being addressed with reference to their key elements (e.g., population or participants, concepts, and context) or other relevant key elements used to conceptualize the review questions and/or objectives. | 4 |
| METHODS | |||
| Protocol and registration | 5 | Indicate whether a review protocol exists; state if and where it can be accessed (e.g., a Web address); and if available, provide registration information, including the registration number. | 3,4 |
| Eligibility criteria | 6 | Specify characteristics of the sources of evidence used as eligibility criteria (e.g., years considered, language, and publication status), and provide a rationale. | 4.5 |
| Information sources * | 7 | Describe all information sources in the search (e.g., databases with dates of coverage and contact with authors to identify additional sources), as well as the date the most recent search was executed. | 5 |
| Search | 8 | Present the full electronic search strategy for at least 1 database, including any limits used, such that it could be repeated. | 5 |
| Selection of sources of evidence † | 9 | State the process for selecting sources of evidence (i.e., screening and eligibility) included in the scoping review. | 5 |
| Data charting process ‡ | 10 | Describe the methods of charting data from the included sources of evidence (e.g., calibrated forms or forms that have been tested by the team before their use, and whether data charting was done independently or in duplicate) and any processes for obtaining and confirming data from investigators. | 4 |
| Data items | 11 | List and define all variables for which data were sought and any assumptions and simplifications made. | 4 |
| Critical apprA.I.sal of individual sources of evidence § | 12 | If done, provide a rationale for conducting a critical appraisal of included sources of evidence; describe the methods used and how this information was used in any data synthesis (if appropriate). | 4 |
| Synthesis of results | 13 | Describe the methods of handling and summarizing the data that were charted. | 12 |
| RESULTS | |||
| Selection of sources of evidence | 14 | Give numbers of sources of evidence screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally using a flow diagram. | 5–11 |
| Characteristics of sources of evidence | 15 | For each source of evidence, present characteristics for which data were charted and provide the citations. | - |
| Critical appraisal within sources of evidence | 16 | If done, present data on critical appraisal of included sources of evidence (see item 12). | - |
| Results of individual sources of evidence | 17 | For each included source of evidence, present the relevant data that were charted that relate to the review questions and objectives. | - |
| Synthesis of results | 18 | Summarize and/or present the charting results as they relate to the review questions and objectives. | 12, 13 |
| DISCUSSION | |||
| Summary of evidence | 19 | Summarize the main results (including an overview of concepts, themes, and types of evidence available), link to the review questions and objectives, and consider the relevance to key groups. | 12, 13 |
| Limitations | 20 | Discuss the limitations of the scoping review process. | 13 |
| Conclusions | 21 | Provide a general interpretation of the results with respect to the review questions and objectives, as well as potential implications and/or next steps. | 13 |
| FUNDING | |||
| Funding | 22 | Describe sources of funding for the included sources of evidence, as well as sources of funding for the scoping review. Describe the role of the funders of the scoping review. | 13 |
References
- Kim, S.; Nussbaum, M.A.; Smets, M.; Ranganathan, S. Effects of an arm-support exoskeleton on perceived work intensity and musculoskeletal discomfort: An 18-month field study in automotive assembly. Am. J. Ind. Med. 2021, 64, 905–914. [Google Scholar] [CrossRef]
- Ambrosini, E.; Ferrante, S.; Rossini, M.; Molteni, F.; Gföhler, M.; Reichenfelser, W.; Duschau-Wicke, A.; Ferrigno, G.; Pedrocchi, A. Functional and usability assessment of a robotic exoskeleton arm to support activities of daily life. Robotica 2014, 32, 1213–1224. [Google Scholar] [CrossRef]
- De Looze, M.P.; Bosch, T.; Krause, F.; Stadler, K.S.; O’Sullivan, L.W. Exoskeletons for industrial application and their potential effects on physical work load. Ergonomics 2016, 59, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Mänttäri, S.; Rauttola, A.-P.; Halonen, J.; Karkulehto, J.; Säynäjäkangas, P.; Oksa, J. Effects of an exoskeleton on muscle activity in tasks requiring arm elevation: Part I—Experiments in a controlled laboratory setting. Work 2024, 77, 1179–1188. [Google Scholar] [CrossRef]
- Massardi, S.; Rodriguez-Cianca, D.; Pinto-Fernandez, D.; Moreno, J.C.; Lancini, M.; Torricelli, D. Characterization and Evaluation of Human–Exoskeleton Interaction Dynamics: A Review. Sensors 2022, 22, 3993. [Google Scholar] [CrossRef]
- Schalk, M.; Schalk, I.; Holl, M.; Kopp, V.; Bauernhansl, T.; Siegert, J.; Schneider, U. Exoskelette reduzieren die subjektive Belastung/Effect of exoskeletons used in industry on perceived exertion during standardized work tasks. Wt Werkstattstech. Online 2022, 112, 607–612. [Google Scholar] [CrossRef]
- Kranenborg, S.E.; Greve, C.; Reneman, M.F.; Roossien, C.C. Side-effects and adverse events of a shoulder- and back-support exoskeleton in workers: A systematic review. Appl. Ergon. 2023, 111, 104042. [Google Scholar] [CrossRef]
- Liu, Y.; Gautam, Y.; Ojha, A.; Shayesteh, S.; Jebelli, H. Studying the Effects of Back-Support Exoskeletons on Workers’ Cognitive Load during Material Handling Tasks. In Construction Research Congress 2024; American Society of Civil Engineers: Des Moines, IA, USA, 2024; pp. 659–669. [Google Scholar] [CrossRef]
- Tetteh, E.; Hallbeck, M.S.; Mirka, G.A. Effects of passive exoskeleton support on EMG measures of the neck, shoulder and trunk muscles while holding simulated surgical postures and performing a simulated surgical procedure. Appl. Ergon. 2022, 100, 103646. [Google Scholar] [CrossRef]
- Botti, L.; Melloni, R. Occupational Exoskeletons: Understanding the Impact on Workers and Suggesting Guidelines for Practitioners and Future Research Needs. Appl. Sci. 2023, 14, 84. [Google Scholar] [CrossRef]
- Schwerha, D.; McNamara, N.; Kim, S.; Nussbaum, M.A. Exploratory Field Testing of Passive Exoskeletons in Several Manufacturing Environments: Perceived Usability and User Acceptance. IISE Trans. Occup. Ergon. Hum. Factors 2022, 10, 71–82. [Google Scholar] [CrossRef]
- Bär, M.; Steinhilber, B.; Rieger, M.A.; Luger, T. The influence of using exoskeletons during occupational tasks on acute physical stress and strain compared to no exoskeleton—A systematic review and meta-analysis. Appl. Ergon. 2021, 94, 103385. [Google Scholar] [CrossRef] [PubMed]
- Carbonari, L.; Palomba, I.; Solazzi, M.; Visconte, C. eXoft, Innovative Soft-Rigid Exoskeleton for Smart Factory. In Advances in Italian Mechanism Science; Quaglia, G., Boschetti, G., Carbone, Y.G., Eds.; Mechanisms and Machine Science; Springer Nature: Cham, Switzerland, 2024; Volume 164, pp. 126–133. [Google Scholar] [CrossRef]
- Cha, J.S.; Monfared, S.; Stefanidis, D.; Nussbaum, M.A.; Yu, D. Supporting Surgical Teams: Identifying Needs and Barriers for Exoskeleton Implementation in the Operating Room. Hum. Factors 2020, 62, 377–390. [Google Scholar] [CrossRef] [PubMed]
- Glowinski, S.; Pecolt, S.; Błażejewski, A.; Maciejewski, I.; Królikowski, T. Gait Analysis with an Upper Limb Prosthesis in a Child with Thrombocytopenia–Absent Radius Syndrome. J. Clin. Med. 2025, 14, 2245. [Google Scholar] [CrossRef]
- Armstrong, K.; Brinkmann, J.T.; Stine, R.; Gard, S.A.; Major, M.J. Do Upper-Limb Loss and Prosthesis Use Affect Lower-Limb Gait Dynamics? J. Prosthet. Orthot. 2021, 33, 249–254. [Google Scholar] [CrossRef]
- Yancosek, K.E.; Schnall, B.L.; Baum, B.S. Impact of Upper-Limb Prosthesis on Gait: A Case Study. JPO J. Prosthet. Orthot. 2008, 20, 163–166. [Google Scholar] [CrossRef]
- Johnson, M.J.; Keyvanian, S.; Mendonca, R.J. Toward inclusive rehabilitation robots. In Rehabilitation Robots for Neurorehabilitation in High-, Low-, and Middle-Income Countries; Elsevier: Amsterdam, The Netherlands, 2024; pp. 471–498. [Google Scholar] [CrossRef]
- Flor-Unda, O.; Casa, B.; Fuentes, M.; Solorzano, S.; Narvaez-Espinoza, F.; Acosta-Vargas, P. Exoskeletons: Contribution to Occupational Health and Safety. Bioengineering 2023, 10, 1039. [Google Scholar] [CrossRef]
- Fox, S.; Aranko, O.; Heilala, J.; Vahala, P. Exoskeletons: Comprehensive, comparative and critical analyses of their potential to improve manufacturing performance. J. Manuf. Technol. Manag. 2019, 31, 1261–1280. [Google Scholar] [CrossRef]
- Bonello, A.; Francalanza, E.; Refalo, P. Smart and Sustainable Human-Centred Workstations for Operators with Disability in the Age of Industry 5.0: A Systematic Review. Sustainability 2023, 16, 281. [Google Scholar] [CrossRef]
- Huamanchahua, D.; Castaneda-Vasquez, C.; Vasquez-Espinoza, A.; Munoz-Zevallos, A. Robotic Devices Types Exoskeletons for Elbow Rehabilitation: A Technological Review. In Proceedings of the 2021 IEEE 12th Annual Ubiquitous Computing, Electronics & Mobile Communication Conference (UEMCON), New York, NY, USA, 1–4 December 2021; IEEE: New York, NY, USA, 2021; pp. 0791–0796. [Google Scholar] [CrossRef]
- Bulboacă, A.E.; Bolboacă, S.D.; Bulboacă, A.C. Ethical considerations in providing an upper limb exoskeleton device for stroke patients. Med. Hypotheses 2017, 101, 61–64. [Google Scholar] [CrossRef]
- Kotnik, P.; Koprivnik, N. Musculoskeletal Disorders in the Workplace of Physiotherapists: Occupational Risk Factors and Their Role in Prevention and Management: A Systematic Review. Open Access Maced. J. Med. Sci. 2024, 12, 347–355. [Google Scholar] [CrossRef]
- Søraa, R.A.; Fosch-Villaronga, E. Exoskeletons for all: The interplay between exoskeletons, inclusion, gender, and intersectionality. Paladyn J. Behav. Robot. 2020, 11, 217–227. [Google Scholar] [CrossRef]
- Zhou, X.; Zheng, L. Model-Based Comparison of Passive and Active Assistance Designs in an Occupational Upper Limb Exoskeleton for Overhead Lifting. IISE Trans. Occup. Ergon. Hum. Factors 2021, 9, 167–185. [Google Scholar] [CrossRef]
- Jianzhong, W.; Zhenghua, D.; Shouqian, S.; Yichen, Z.; Lang, S.; Junfang, Z.; Dongwei, Z.; Xuequn, Z.; Vänni, K.; Kaiyuan, Z. Evaluation method of usability performance for upper-limb exoskeleton. IET Conf. Proc. 2024, 2023, 342–348. [Google Scholar] [CrossRef]
- Wu, K.; Xiang, P.; Ramon, R.; Aravelli, A.; Lagos, L.; Bai, O. Assessment of a Modular Upper-Limb Exoskeleton with Powered Assistance. In Proceedings of the 2023 2nd International Conference on Automation, Robotics and Computer Engineering (ICARCE), Wuhan, China, 14–16 December 2023; IEEE: New York, NY, USA, 2023; pp. 1–6. [Google Scholar] [CrossRef]
- Lee, S.; Xiang, Y.; Xia, T.; Yang, J. Assessments and Evaluation Methods for Upper Limb Exoskeleton—A Literature Survey. In Volume 2: 42nd Computers and Information in Engineering Conference (CIE); American Society of Mechanical Engineers: St. Louis, MO, USA, 2022; p. V002T02A021. [Google Scholar] [CrossRef]
- Salvadore, G.; Rota, E.; Corsi, E.; Colombina, G. Industrial Wearable Robots: A HUMANufacturing Approach. In XV Mediterranean Conference on Medical and Biological Engineering and Computing–MEDICON 2019; Henriques, J., Neves, N., De Carvalho, P., Eds.; IFMBE Proceedings; Springer International Publishing: Cham, Switzerland, 2020; Volume 76, pp. 1729–1733. ISBN 978-3-030-31634-1. [Google Scholar]
- Blanchet, L.; Achiche, S.; Docquier, Q.; Fisette, P.; Raison, M. A procedure to optimize the geometric and dynamic designs of assistive upper limb exoskeletons. Multibody Syst. Dyn. 2021, 51, 221–245. [Google Scholar] [CrossRef]
- Wang, Z.; Cui, L.; Guo, W.; Zhao, L.; Yuan, X.; Gu, X.; Tang, W.; Bu, L.; Huang, W. A design method for an intelligent manufacturing and service system for rehabilitation assistive devices and special groups. Adv. Eng. Inform. 2022, 51, 101504. [Google Scholar] [CrossRef]
- Gandolla, M.; Antonietti, A.; Longatelli, V.; Gasperina, S.D.; Ambrosini, E.; Pedrocchi, A. Research Technologies for Assistance During Daily Life Activities. In XV Mediterranean Conference on Medical and Biological Engineering and Computing—MEDICON 2019; Henriques, J., Neves, N., De Carvalho, Y.P., Eds.; IFMBE Proceedings; Springer International Publishing: Cham, Switzerland, 2020; Volume 76, pp. 1709–1713. [Google Scholar] [CrossRef]
- Kumar, R.S.; Maurya, K.; Rastogi, M.; Gupta, M. Sensor and Button-Controlled Exoskeleton Arm. In Proceedings of the 2022 IEEE 9th Uttar Pradesh Section International Conference on Electrical, Electronics and Computer Engineering (UPCON), Prayagraj, India, 2–4 December 2022; IEEE: New York, NY, USA, 2022; pp. 1–4. [Google Scholar] [CrossRef]
- Adverse Effects for Use Upper Limb Exoskeletons—Mendeley Data. Available online: https://data.mendeley.com/drafts/zpbv5kw9rv (accessed on 18 April 2025).
- Tounekti, Y.; Cocquerz, T.; Mansour, K.B. The effects of an upper limb exoskeleton on gait performance and stability. J. Biomech. 2024, 169, 112072. [Google Scholar] [CrossRef]
- Zheng, L.; Pan, C.; Wei, L.; Bahreinizad, H.; Chowdhury, S.; Ning, X.; Santos, F. Shoulder-assist exoskeleton effects on balance and muscle activity during a block-laying task on a simulated mast climber. Int. J. Ind. Ergon. 2024, 104, 103652. [Google Scholar] [CrossRef]
- Pinho, J.P.; Forner-Cordero, A. Shoulder muscle activity and perceived comfort of industry workers using a commercial upper limb exoskeleton for simulated tasks. Appl. Ergon. 2022, 101, 103718. [Google Scholar] [CrossRef]
- Fernández Álvarez, L.G.; Núñez Nagy, S.; Cano de la Cuerda, R. Exoesqueletos portables en personas con lesión medular. Revisión sistemática. RIECS 2020, 5, 86–105. [Google Scholar] [CrossRef]
- Yoon, J.; Park, J.; Lee, C.; Bang, Y. Upper limb power-assist wearable robot for handling repetitive medium- to low-weight loads in daily logistics tasks. Robot. Auton. Syst. 2024, 181, 104780. [Google Scholar] [CrossRef]
- Latella, C.; Tirupachuri, Y.; Tagliapietra, L.; Rapetti, L.; Schirrmeister, B.; Bornmann, J.; Gorjan, D.; Čamernik, J.; Maurice, P.; Fritzsche, L.; et al. Analysis of Human Whole-Body Joint Torques During Overhead Work with a Passive Exoskeleton. IEEE Trans. Hum.-Mach. Syst. 2022, 52, 1060–1068. [Google Scholar] [CrossRef]
- Watterworth, M.W.B.; Porto, R.; Cort, J.A.; La Delfa, N.J. Modeling the Effects of Worker and Work Task Height on Upper-Limb Exoskeleton Support. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2023, 67, 847–851. [Google Scholar] [CrossRef]
- De Bock, S.; Ghillebert, J.; Govaerts, R.; Elprama, S.A.; Marusic, U.; Serrien, B.; Jacobs, A.; Geeroms, J.; Meeusen, R.; De Pauw, K. Passive Shoulder Exoskeletons: More Effective in the Lab Than in the Field? IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 173–183. [Google Scholar] [CrossRef]
- Dalbøge, A.; Frost, J.; Grytnes, R.; Roy, J.-S.; Samani, A.; Christiansen, D.H. Effects of a passive shoulder exoskeleton on muscle activity among Danish slaughterhouse workers. Appl. Ergon. 2024, 114, 104111. [Google Scholar] [CrossRef] [PubMed]
- Ramella, G.; Grazi, L.; Giovacchini, F.; Trigili, E.; Vitiello, N.; Crea, S. Evaluation of antigravitational support levels provided by a passive upper-limb occupational exoskeleton in repetitive arm movements. Appl. Ergon. 2024, 117, 104226. [Google Scholar] [CrossRef]
- Arnoux, B.; Farr, A.; Boccara, V.; Vignais, N. Evaluation of a Passive Upper Limb Exoskeleton in Healthcare Workers during a Surgical Instrument Cleaning Task. Int. J. Environ. Res. Public Health 2023, 20, 3153. [Google Scholar] [CrossRef]
- Coccia, A.; Capodaglio, E.M.; Amitrano, F.; Gabba, V.; Panigazzi, M.; Pagano, G.; D’Addio, G. Biomechanical Effects of Using a Passive Exoskeleton for the Upper Limb in Industrial Manufacturing Activities: A Pilot Study. Sensors 2024, 24, 1445. [Google Scholar] [CrossRef] [PubMed]
- Ojelade, A.; Morris, W.; Kim, S.; Kelson, D.; Srinivasan, D.; Smets, M.; Nussbaum, M.A. Three passive arm-support exoskeletons have inconsistent effects on muscle activity, posture, and perceived exertion during diverse simulated pseudo-static overhead nutrunning tasks. Appl. Ergon. 2023, 110, 104015. [Google Scholar] [CrossRef]
- Grazi, L.; Trigili, E.; Fiore, M.; Giovacchini, F.; Sabatini, A.M.; Vitiello, N.; Crea, S. Passive shoulder occupational exoskeleton reduces shoulder muscle coactivation in repetitive arm movements. Sci. Rep. 2024, 14, 27843. [Google Scholar] [CrossRef]
- Pinho, J.P.; Americano, P.P.; Taira, C.; Pereira, W.; Caparroz, E.; Forner-Cordero, A. Shoulder muscles electromyographic responses in automotive workers wearing a commercial exoskeleton. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; IEEE: New York, NY, USA, 2020; pp. 4917–4920. [Google Scholar] [CrossRef]
- Kim, S.; Madinei, S.; Alemi, M.M.; Srinivasan, D.; Nussbaum, M.A. Assessing the potential for “undesired” effects of passive back-support exoskeleton use during a simulated manual assembly task: Muscle activity, posture, balance, discomfort, and usability. Appl. Ergon. 2020, 89, 103194. [Google Scholar] [CrossRef]
- Van Engelhoven, L.; Poon, N.; Kazerooni, H.; Rempel, D.; Barr, A.; Harris-Adamson, C. Experimental Evaluation of a Shoulder-Support Exoskeleton for Overhead Work: Influences of Peak Torque Amplitude, Task, and Tool Mass. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 250–263. [Google Scholar] [CrossRef]
- McFarland, T.; Fischer, S. Considerations for Industrial Use: A Systematic Review of the Impact of Active and Passive Upper Limb Exoskeletons on Physical Exposures. IISE Trans. Occup. Ergon. Hum. Factors 2019, 7, 322–347. [Google Scholar] [CrossRef]
- Musso, M.; Oliveira, A.S.; Bai, S. Influence of an upper limb exoskeleton on muscle activity during various construction and manufacturing tasks. Appl. Ergon. 2024, 114, 104158. [Google Scholar] [CrossRef] [PubMed]
- Barbe, M.F.; Gallagher, S.; Massicotte, V.S.; Tytell, M.; Popoff, S.N.; Barr-Gillespie, A.E. The interaction of force and repetition on musculoskeletal and neural tissue responses and sensorimotor behavior in a rat model of work-related musculoskeletal disorders. BMC Musculoskelet. Disord. 2013, 14, 303. [Google Scholar] [CrossRef]
- Blanco, A.; Catalan, J.M.; Martinez, D.; Garcia-Perez, J.V.; Garcia-Aracil, N. The Effect of an Active Upper-Limb Exoskeleton on Metabolic Parameters and Muscle Activity During a Repetitive Industrial Task. IEEE Access 2022, 10, 16479–16488. [Google Scholar] [CrossRef]
- Mänttäri, S.; Rauttola, A.-P.; Halonen, J.; Karkulehto, J.; Säynäjäkangas, P.; Oksa, J. Effects of upper-limb exoskeleton on muscle activity in tasks requiring arm elevation: Part II—In-field experiments in construction industry settings. Work 2024, 79, 753–763. [Google Scholar] [CrossRef]
- Theurel, J.; Desbrosses, K.; Roux, T.; Savescu, A. Physiological consequences of using an upper limb exoskeleton during manual handling tasks. Appl. Ergon. 2018, 67, 211–217. [Google Scholar] [CrossRef]
- Schwerha, D.J.; McNamara, N.; Nussbaum, M.A.; Kim, S. Adoption potential of occupational exoskeletons in diverse enterprises engaged in manufacturing tasks. Int. J. Ind. Ergon. 2021, 82, 103103. [Google Scholar] [CrossRef]
- Wollesen, B.; Gräf, J.; Hansen, L.; Gurevich, A.; Elprama, S.A.; Argubi-Wollesen, A.; De Pauw, K. Gender differences in the use of an upper-extremity exoskeleton during physically and cognitively demanding tasks—A study protocol for a randomized experimental trial. Front. Neurol. 2024, 15, 1401937. [Google Scholar] [CrossRef]
- Moeller, T.; Krell-Roesch, J.; Woll, A.; Stein, T. Effects of Upper-Limb Exoskeletons Designed for Use in the Working Environment—A Literature Review. Front. Robot. AI 2022, 9, 858893. [Google Scholar] [CrossRef]
- Choi, D.L.Y.H. Individual Differences in Body Mass, Biological Sex, and Physical Fitness Affecting Human-Exoskeleton Interactions. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2023, 67, 1794–1800. [Google Scholar] [CrossRef]
- Weston, E.B.; Alizadeh, M.; Hani, H.; Knapik, G.G.; Souchereau, R.A.; Marras, W.S. A Physiological and Biomechanical Investigation of Three Passive Upper-Extremity Exoskeletons during Simulated Overhead Work. Ergonomics 2021, 65, 105–117. [Google Scholar] [CrossRef]
- Lim, Y.X.; Sharifi, M. A Chain-Based Cable-Driven Upper-Limb Exoskeleton: Design, Mechanical Analysis and Development. In Proceedings of the 2024 International Symposium on Medical Robotics (ISMR), Atlanta, GA, USA, 3–5 June 2024; IEEE: New York, NY, USA, 2024; pp. 1–7. [Google Scholar] [CrossRef]
- Liu, K.-H.; Yi, S.-C.; Lin, Y.-C. How to Select the Force Setting of the Exoskeleton? The Effect of Working Height, Hand Posture on Assisting Force. In Cross-Cultural Design; Rau, P.-L.P., Ed.; Lecture Notes in Computer Science; Springer Nature: Cham, Switzerland, 2023; Volume 14023, pp. 98–107. [Google Scholar] [CrossRef]
- Zhang, Y.; Arakelian, V. Design of a Passive Robotic ExoSuit for Carrying Heavy Loads. In Proceedings of the 2018 IEEE-RAS 18th International Conference on Humanoid Robots (Humanoids) 2018, Beijing, China, 6–9 November 2018. [Google Scholar] [CrossRef]
- Kong, Y.-K.; Kim, J.H.; Shim, H.-H.; Shim, J.-W.; Park, S.-S.; Choi, K.-H. Efficacy of passive upper-limb exoskeletons in reducing musculoskeletal load associated with overhead tasks. Appl. Appl. Ergon. 2023, 109, 103965, ISSN 0003-6870. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Arakelian, V. Design and Experimental Evaluation of a Semi-Passive Upper-Limb Exoskeleton for Workers with Motorized Tuning of Assistance. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 10. [Google Scholar] [CrossRef]
- Pacifico et IPacifico, I.; Parri, A.; Taglione, S.; Sabatini, A.M.; Violante, F.S.; Molteni, F.; Giovacchini, F.; Vitiello, N.; Crea, S. Exoskeletons for workers: A case series study in an enclosures production line. Appl. Ergon. 2022, 101, 103679. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kwon, K.; Soltis, I.; Matthews, J.; Lee, Y.; Kim, H.; Romero, L.; Zavanelli, N.; Kwon, Y.; Kwon, S.; et al. Intelligent upper-limb exoskeleton integrated with soft wearable bioelectronics and deep-learning for human intention-driven strength augmentation based on sensory feedback. arXiv 2023. [Google Scholar] [CrossRef]
- Thakur, N.; Han, C.Y. Exoskeleton-Based Multimodal Action and Movement Recognition: Identifying and Developing the Optimal Boosted Learning Approach. arXiv 2021. [Google Scholar] [CrossRef]
- Li, J.; Chen, C. Machine learning-based energy harvesting for wearable exoskeleton robots. Sustain. Energy Technol. Assess. 2023, 57, 103122. [Google Scholar] [CrossRef]
- Coser, O.; Tamantini, C.; Soda, P.; Zollo, L. AI-based methodologies for exoskeleton-assisted rehabilitation of the lower limb: A review. Front. Robot. AI 2024, 11, 1341580. [Google Scholar] [CrossRef]
- Pinelli, M.; Manetti, S.; Lettieri, E. Assessing the Social and Environmental Impact of Healthcare Technologies: Towards an Extended Social Return on Investment. Int. J. Environ. Res. Public Health 2023, 20, 5224. [Google Scholar] [CrossRef]
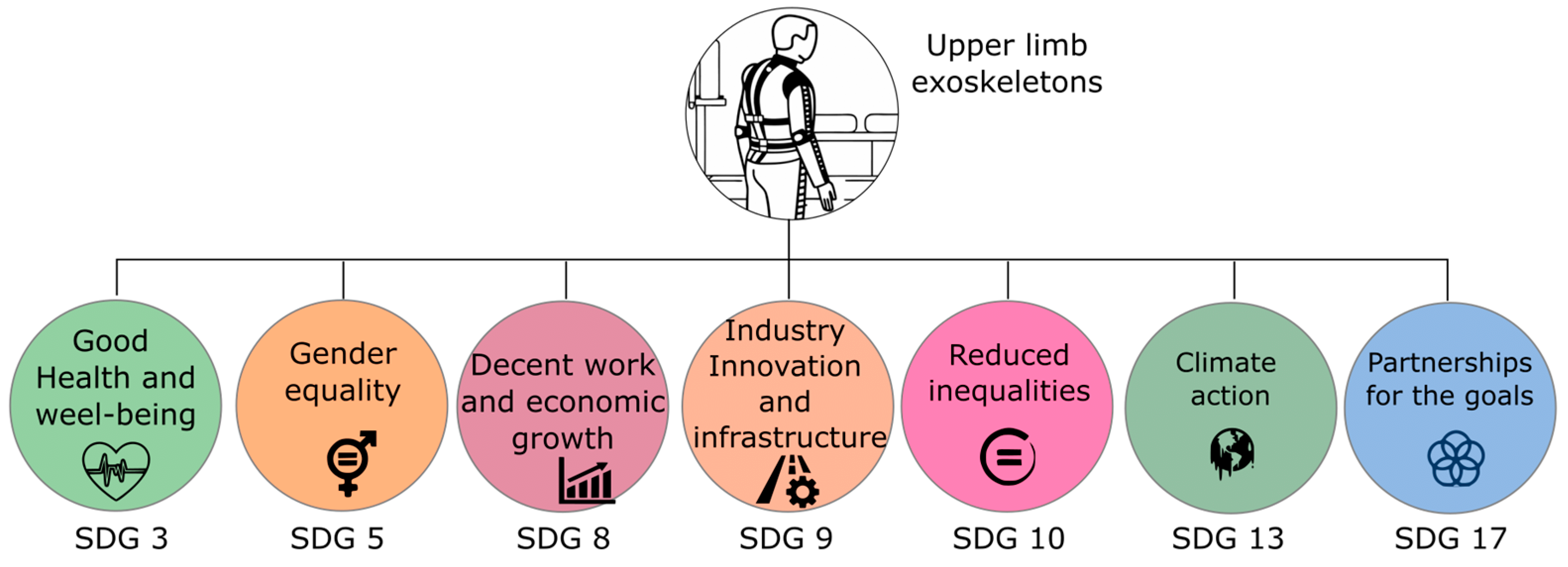


| SDG | Contribution/Issue | References |
|---|---|---|
| SDG 3: Health and Well-being | Rehabilitation technologies and assistive devices enhance quality of life for individuals with motor impairments. | [22,23] |
| SDG 3: Health and Well-being | Mitigates occupational musculoskeletal strain in rehabilitation therapists during patient sessions. | [24] |
| SDG 5: Gender equality | Promotes inclusion, accessibility, empowerment and equity in rehabilitation technologies. | [25] |
| SDG 8: Decent Work and Economic Growth | Supports industrial workers by reducing musculoskeletal risks and improving productivity. | [26,27,28] |
| SDG 8: Decent Work and Economic Growth | Enhances ergonomic safety and occupational health outcomes by reducing work-related injuries and improving job satisfaction. | [26,29,30] |
| SDG 9: Industry, Innovation and Infrastructure | Promotes technological innovation in advanced materials, intelligent control systems, and optimized human-machine interfaces. | [22,31] |
| SDG 9: Industry, Innovation and Infrastructure | Supports smart manufacturing and Industry 4.0 integration. | [30,32] |
| SDG 10: Reduced Inequalities | Enhances accessibility for persons with disabilities, advancing equality. | [33,34] |
| SDG 11: Sustainable Cities and Communities | Enhances mobility and independence, fostering inclusive communities | [23] |
| Quality Assessment Questions Answer | Answer |
|---|---|
| Does the document describe the effects associated with the prolonged use of upper-limb exoskeletons in work activities? | (+1) Yes/(+0) No |
| Does the paper describe the health risks associated with the prolonged use of upper-limb exoskeletons in the work environment? | (+1) Yes/(+0) No |
| Are ergonomic recommendations addressed or given to reduce workers’ health risks due to the use of exoskeletons? | (+1) Yes/(+0) No |
| Is the journal or conference in which the article was published indexed in the JCR? | (+1) if it is ranked Q1, (+0.75) if it is ranked Q2, (+0.50) if it is ranked Q3, (+0.25) if it is ranked Q4, (+0.0) if it is not ranked |
| Database | String Search | Studies Number |
|---|---|---|
| Web of Science | effects upper limb exoskeleton workers (Topic) | 35 |
| Taylor & Francis | Abstract: effects upper limb exoskeleton workers | 7 |
| Science Direct | Title, abstract, keywords: effects upper limb exoskeleton workers | 6 |
| Scopus | TITLE-ABS-KEY (effects AND upper AND limb AND exoskeleton AND workers) | 31 |
| PubMed | search: effects upper limb exoskeleton workers | 37 |
| Total number of studies | 116 |
| Negative Effect | Description | Ref |
|---|---|---|
| Discomfort and pain | Due to muscle weakness, inadequate redistribution of loads, restriction of movements, increase in body temperature, and fatigue due to lack of adaptation. | [52] |
| Increased cognitive load | It occurs because the worker must adapt to new movement patterns, divide their attention between the task and the device, and manage possible discomforts. This increases mental effort and fatigue, affecting efficiency and safety at work. | [36] |
| Task-specific constraints | Due to restrictions in movement, agility is reduced, making tasks that require flexibility or precision difficult, generating muscle fatigue in unassisted areas, and increasing discomfort in prolonged postures. | [42,53] |
| Negative perception and usability | It arises from discomfort, movement restrictions, and fatigue, which makes it difficult to use for a long time and can generate rejection by the worker. | [12] |
| Possibility of increased fatigue | It is due to overload in unassisted muscles, restriction of natural movements, increased cognitive effort, and possible discomfort in adjustment. The weight of the exoskeleton and the need to adapt to its functioning can lead to physical and mental exhaustion. | [42,52] |
| Ergonomic and design challenges | Lack of standardized methodologies for ergonomic analysis and optimization. | [7,48] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flor-Unda, O.; Arcos-Reina, R.; Nunez-Nagy, S.; Alarcos, B. Adverse Effects Due to the Use of Upper Limbs Exoskeletons in the Work Environment: A Scoping Review. Biomimetics 2025, 10, 340. https://doi.org/10.3390/biomimetics10050340
Flor-Unda O, Arcos-Reina R, Nunez-Nagy S, Alarcos B. Adverse Effects Due to the Use of Upper Limbs Exoskeletons in the Work Environment: A Scoping Review. Biomimetics. 2025; 10(5):340. https://doi.org/10.3390/biomimetics10050340
Chicago/Turabian StyleFlor-Unda, Omar, Rafael Arcos-Reina, Susana Nunez-Nagy, and Bernardo Alarcos. 2025. "Adverse Effects Due to the Use of Upper Limbs Exoskeletons in the Work Environment: A Scoping Review" Biomimetics 10, no. 5: 340. https://doi.org/10.3390/biomimetics10050340
APA StyleFlor-Unda, O., Arcos-Reina, R., Nunez-Nagy, S., & Alarcos, B. (2025). Adverse Effects Due to the Use of Upper Limbs Exoskeletons in the Work Environment: A Scoping Review. Biomimetics, 10(5), 340. https://doi.org/10.3390/biomimetics10050340






