Abstract
Documented penicillin allergies are associated with an increased risk of surgical site infections (SSIs), and first-line antibiotics (e.g., cefazolin) are associated with a lower risk of SSIs. The goal of this study was to evaluate the effect of a pharmacist-driven penicillin allergy de-labeling pilot program on the use of preoperative cefazolin in selected surgery patients with documented penicillin allergies. This single-center, quasi-experimental study included adult patients with a charted penicillin allergy who underwent CT or spine surgery in 2021 (control group) or during the 6-month intervention pilot (October 2022–March 2023). In the intervention group, qualifying patients were interviewed via phone to assess allergy history. Qualified patients were de-labeled or referred to an allergist for outpatient skin testing and/or oral challenge. The primary outcome was the rate of cefazolin use preoperatively. Secondary outcomes included 30-day SSIs, Clostridioides difficile infection, acute kidney injury, readmission, and hospital length of stay. Of the intervention group, 57 (79.2%) patients completed the interview. Cefazolin was used preoperatively in 71.0% (152) of the control group versus 88.9% (64) of the intervention group (p < 0.002). There were no clinically significant differences in secondary outcomes. The pharmacist-driven penicillin allergy de-labeling pilot program in CT and spine surgery patients was associated with increased cefazolin use.
1. Introduction
Approximately 10% of the US population have a penicillin (PCN) allergy listed in their medical record; however, true hypersensitivity is uncommon. Some studies suggest that up to 95% of patients who report penicillin allergies can still tolerate this class of medication [1]. The inappropriate reporting of these allergies leads to providers selecting alternative antibiotics associated with higher complication rates. Studies show that documented penicillin allergies are associated with an increased risk of methicillin-resistant Staphylococcus aureus (MRSA) infections, Clostridioides difficile infections (CDIs), and risk of surgical site infections (SSIs) as a result of patients not receiving recommended first-line preoperative antibiotics [2,3]. SSIs have been associated with negative patient outcomes, including rehospitalization, prolongment of hospital length of stay (LOS), reduced quality of life, infection-related complications, and increased costs [4,5]. The literature supports the use of penicillin antibiotics if the patient’s history suggests non-immune mediated intolerance [3] or the allergy reaction is considered low-risk [1]. De-labeling inappropriately documented allergies and clarifying true allergies can decrease the use of unnecessary broad-spectrum antibiotics and potentially prevent these negative patient outcomes [6].
Validated algorithms and questionnaires have been developed to aid in the process of de-labeling patients with inaccurate penicillin allergies [6,7,8,9]. In a study by Devchand et al., 13% of patients who were screened for de-labeling were able to have their penicillin allergy label removed without any direct challenge or skin testing [5]. Several algorithms used by different health systems across the US have been published, and many recommend skin testing, direct oral challenges, or explicit recommendations for alternative cephalosporins [7]. A study published by Kwiatkowski et al. in 2021 evaluated a pharmacist-led intervention to help optimize preoperative antibiotics [8]. Pharmacists assessed penicillin allergies via telephone and then made antibiotic recommendations to providers to increase first-line preoperative antibiotic use. The study found that cefazolin use significantly increased from 28% to 65% after the implementation of this intervention (p = 0.001) [8]. The above study demonstrates that pharmacists are able to assess patients’ allergy history and assist providers in appropriate antibiotic selection in patients with documented penicillin allergies.
Hesitancy to use cephalosporins in patients with documented penicillin allergies stems from early studies estimating that approximately 10% of cephalosporins exhibit cross-reactivity with penicillins [10]. However, these studies overestimated the true cross-reactivity rate in large part due to historical contamination of penicillin in cephalosporin products during the manufacturing process [9]. Further studies have revealed that general cross-reactivity with cephalosporins in patients with reported penicillin allergy is low (~1%), and even in patients with a confirmed penicillin allergy, the rate was significantly lower than previously reported (~2.5%) [11]. Most recent studies have determined that the key factor in determining cross-reactivity between penicillins and cephalosporins is their similarities in R1 side chains. In general, many first- and second-generation cephalosporins possess similar side chains to penicillins [9]. Notably, cefazolin, a first-generation cephalosporin that is the preoperative antibiotic recommended for most surgery types [12], shares no similarity in side chains to any other penicillin or cephalosporin. This provides a unique benefit, in that cross reactivity is not expected in patients with penicillin or cephalosporin allergies, which makes it a safe preoperative choice for the vast majority of patients. Despite the lack of cross-reactivity of cefazolin in penicillin-allergic patients, many providers and institution-specific protocols still recommend alternative antibiotics for patients with penicillin allergies. Thus, education on this topic is often necessary. Furthermore, as in this study, the de-labeling and/or clarifications of these allergy labels can help avoid the issue altogether.
The goal of this study was to evaluate the effect of a pharmacist-driven penicillin allergy de-labeling program on cefazolin use preoperatively in cardiothoracic (CT) and spine surgery patients who had documented penicillin allergies.
2. Materials and Methods
2.1. Study Design and Sample
This was a single-center, quasi-experimental study. A de-labeling pilot program was planned and conducted between October 2022 and March 2023. The study site was a 996-bed quaternary, community teaching hospital located in Minneapolis, Minnesota. Patients ≥18 years of age at hospital admission, charted as having a penicillin allergy, and admitted for CT or spine surgery in 2021 (control group) or October 2022 to March 2023 during the six-month pilot (intervention group) were included. Procedures included coronary artery bypass graft (CABG), laminectomy, spinal fusion, aortic valve replacement, mitral valve replacement, tricuspid valve replacement, and sternotomy. These specific surgical populations were chosen based on provider willingness to participate in the pilot program. Patients were excluded if they had an active infection present at the time of surgery. All activities within the pilot program fell under current pharmacist scope of practice. Therefore, this study was determined to be quality improvement and exempt from IRB review by the Allina Health Institutional Review Board according to federal regulation 45 CFR 46.104(d).
2.2. De-Labeling Pilot Program Description
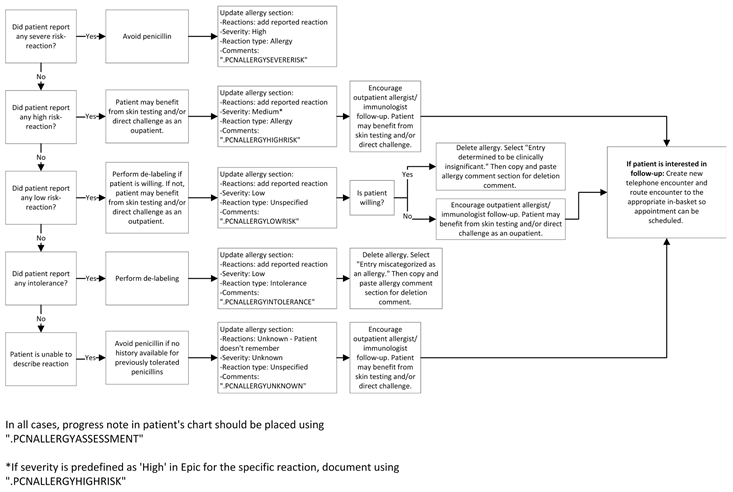
Patients meeting the eligibility criteria for the intervention were identified based on a daily informatics report. Data on patients with new surgeries scheduled during the intervention period with a documented penicillin allergy were entered into a REDCap database for the interviewing pharmacist to confirm eligibility and contact. Pharmacist-led interviews were conducted by pharmacy residents, who were trained on the study protocol and educated about penicillin allergies in order to accurately complete the allergy screenings. After screening to confirm eligibility, pharmacy residents attempted to contact patients via phone. The interviewing pharmacist attempted to contact the patient a maximum of 3 times and left a voicemail if able with each attempt. During the interview, the patient’s allergy history was assessed utilizing the checklist in Appendix A. The checklist was adapted from the Penicillin Allergy History Toolkit published in 2019 by Shenoy et al. in JAMA [9]. Other allergy-related information collected from the patient included what penicillin antibiotic they had a reaction to, the reaction, when this reaction occurred, if the patient took medications or sought medical care to treat the reaction, the timing of symptom onset after taking the medication, and other penicillin and/or cephalosporins the patient had tolerated in the past (both before and after the reaction). The interviewing pharmacist then took the appropriate actions based on the algorithm shown in Appendix B. This algorithm was adapted from a publication by Ramsey et al. [6]. Afterwards, the interviewing pharmacist could de-label the allergy or refer the patient to an outpatient allergist for skin testing and/or oral challenge as appropriate. De-labeled patients were educated about the removal of their allergy and that they should alert other healthcare providers outside of the study institution that their penicillin allergy had been de-labeled. The allergy alert in the medical record was updated, and a progress note was placed in the chart to document information gathered in the interview for surgeons and other providers to access when making antibiotic therapy decisions in the future.
In addition to the de-labeling pilot program and as part of broader efforts to increase cefazolin utilization, CT and spine surgeons also received education about beta-lactam cross reactivity in 2022, prior to the de-labeling pilot program. Surgeons were also provided with an updated surgical prophylaxis guideline with the goal of increasing cefazolin use. This guideline included the images shown in Appendix C and Appendix D. Despite this education in 2022 prior to the pilot program, overall cefazolin utilization across all surgery types between January and September 2022 remained below the health system’s goal in the months prior to the pilot program, and the cefazolin utilization rate was only stable-to-slightly higher in 2022 in October compared with 2021 (81.0% vs. 77.8%, respectively, not delineated by specialty or surgery type). CT and spine surgeons supported the additional interventions included in the pilot program to supplement the disseminated education.
2.3. Data Collection and Measures
Data were collected as a combination of data extracts from the electronic data warehouse and chart reviews as needed. Intervention process measures were collected by the pharmacy team in a REDCap database, documenting confirmation of eligibility, calls to patients, and outcomes of the interview. Infection measures were collected from the Infection Prevention Department.
The primary endpoint of the study was the rate of cefazolin use preoperatively, defined as administered within the 2 h window prior to surgery. Secondary endpoints included SSIs, CDI, and 30-day readmission. SSIs were defined according to the National Healthcare Safety Network (NHSN) definitions [13]. Secondary measures also included acute kidney injury (AKI) (as defined by an increase in serum creatinine (SCr) of ≥0.3 mg/dL within 48 h or ≥50% within 7 days, with baseline SCr being defined as the most recent value prior to surgery up to 365 days prior) [14,15] and hospital LOS.
Patient characteristics collected included age, body mass index (BMI), sex, race, Hispanic ethnicity, diabetes, history of CDI, American Society of Anesthesiologists physical status classification, prior MRSA colonization, and immunosuppressant use. Immunosuppressants included corticosteroids, antirejection therapies, monoclonal antibodies, and DMARDs. Documentation of the reported drug allergy included specific allergy type and previously reported drug reactions. Type of surgery was also documented.
2.4. Statistical Analysis
Patient characteristics and outcomes were compared by group (control vs. intervention). Intervention patients were only included in outcome analysis if the pharmacy staff attempted to contact them. Statistical significance was assessed using Fisher’s exact tests for categorical measures and t-tests for continuous measures. All analyses were conducted using Stata version 17.0 (StataCorp College Station, TX, USA).
3. Results
We identified 214 and 102 patients who met the inclusion criteria for the control and intervention groups, respectively. Of the 102 patients who met inclusion in the intervention group, pharmacists attempted to contact 72. The final analysis was conducted on this subset of patients whom the team attempted to contact. The remaining 30 patients that met inclusion criteria were not contacted due to the urgent nature of their procedure (n = 12), because the penicillin allergy had been previously deleted (n = 2), because they were a duplicate patient (n = 1), or because they were missed by staff due to scheduling or time constraints (n = 15), as shown in Figure 1. The demographic and baseline characteristics for both groups are shown in Table 1. There were several baseline characteristics that were statistically different between the groups, including a higher percentage of females in the intervention group. The groups also differed with regard to ASA classification, reported drug allergy, and surgery type, with significantly fewer CT surgeries in the intervention group. Of the patients who were contacted in the intervention group, 57 (79.2%) completed the interview. The average time to complete the patient interview and related documentation was 13.47 min.

Figure 1.
Intervention group.

Table 1.
Demographic and baseline characteristics.
Of the patients with attempted contacts by pharmacy staff (n = 72), 8 (11.1%) were de-labeled, of which 5 were de-labeled after pharmacist interview alone and 3 after referral to an outpatient allergist. A total of 19 (26.4%) patients were referred to outpatient allergists for skin testing and/or oral challenge. At the time of writing, six (31.6%) patients have made a follow-up allergist appointment. Three of these patients have not yet been seen, and the other three were seen, tested, and de-labeled.
The primary outcome of cefazolin use preoperatively occurred in 152 (71.0%) patients in the control group compared with 64 (88.9%) patients in the intervention group (p = 0.002). This includes patients who received cefazolin alone and patients who received multiple antibiotics, including cefazolin, as shown in Table 2. Cefazolin was used as monotherapy in 94 (43.9%) patients in the control group compared with 56 (77.8%) patients in the intervention group.

Table 2.
Antibiotics administered and outcomes.
No clinically significant differences in secondary outcomes that were associated with the intervention were identified. Surgical site infections occurred in five (2.3%) patients in the control group and three (4.2%) patients in the intervention group (p = 0.420). No patients in either group were found to have CDI. Readmission within 30 days occurred in 12 (5.6%) patients in the control group and 5 (6.9%) patients in the intervention group (p = 0.680). AKI occurred in 13 (6.1%) patients in the control group and no patients in the intervention group (p = 0.135), though SCr data were not available for 59.3% of the control group and 81.9% of the intervention group. There was a statistically significant difference in hospital LOS, with a mean of 3.89 days in the control group compared with 2.34 days in the intervention group (p = 0.015). However, given a very low proportion of CT surgeries in the intervention group, the comparison of the LOS is not appropriate given the variability of the surgery type. LOS data were stratified by surgery type to account for this, and patients who had received spine surgery had a statistically significantly longer LOS in the intervention group (2.21 days) compared with the control group (1.02 days). In the intervention group, data were also collected on new allergies added to the patient’s medical record during their surgical admission in order to assess the safety of the intervention. No patients had a new cefazolin allergy added after receiving cefazolin preoperatively.
4. Discussion
The pharmacist-driven penicillin allergy de-labeling pilot program in CT and spine surgery patients was associated with increased first-line preoperative antibiotic (cefazolin) use. There was no significant difference in surgical site infections, CDI, or acute kidney injury; however, the study was underpowered to detect a difference due to very few events occurring in either group. The decreased LOS in the intervention group was primarily driven by a lack of CT surgery in the intervention group and was not intervention-related. Due to the urgent nature of these procedures, many were not scheduled in advance, so pharmacists were unable to complete an allergy clarification interview. To address this, we compared the mean LOS for spine surgery patients only and found a significant increase. According to a discussion with spine surgeons at the study institution, spinal fusion procedures consistently have a longer length of stay compared with laminectomies. Spinal fusion procedures made up a larger portion of the intervention group (58.3% of the intervention group vs. 16.8% of the control group), likely accounting for this increase. To better assess the effect of a penicillin allergy de-labeling intervention on the LOS, future studies would need to match or stratify analyses by specific surgery type, which we did not have sufficient sample size to do in this study.
The results of this study add evidence to the increasing literature that demonstrates the positive impact of penicillin allergy de-labeling interventions. Several previous studies have also shown an increase in first-line antibiotic use following pharmacist-led penicillin allergy efforts [6,8,16]. Our study was similar to the study by Kwiatkowski et al. in terms of study design and endpoints but differed in key aspects of methodology, including the patient population included, the identification of appropriate patients, the timing of interviews, and making formal antibiotic therapy recommendations to providers. Despite these differences, their study found similar results to our study—increased preoperative cefazolin use after pharmacist penicillin allergy de-labeling and allergy clarification efforts. It is of note that though these studies have shown that pharmacists are capable of performing this work, it can be difficult to implement these programs into pharmacists’ workflow and procure dedicated time for these efforts. In this study, 14.7% of eligible patients in the intervention group were not able to be interviewed due to staff time constraints, making these results more applicable to actual practice. Another concern with penicillin allergy de-labeling efforts is that patients may have the allergy re-labeled or that they will still have penicillin listed as an allergy in the electronic medical record within other health systems. Proper documentation of allergy removal and patient education to share the removal of their allergy when receiving care at other health systems is important to ensure full benefit from the de-labeling process. This study involved both documentation and patient education efforts in order to prevent re-labeling. No de-labeled patients had been re-labeled within the study institution at the time of data analysis, although allergy labels at other healthcare systems could not be assessed.
Limitations include small sample size, resulting in insufficient power to detect a difference in secondary outcomes. There were also a large portion of patients who did not have SCr data available. Given the urgent nature of most cardiothoracic procedures, the intervention was unsuccessful in these patients. Preoperative penicillin de-labeling programs would likely be more successful targeting surgical types that are planned in advance, so interviewers have sufficient time to complete the patient interview. The patients for which unsuccessful contact attempts were made were included in the intervention group, as documentation was updated according to protocol, but this may have introduced bias into the results, as these patients did not complete an interview. Further study is needed to assess association with key secondary outcomes. Another limitation to this study was the low rate of allergist follow-up. Of 19 patients referred to an allergist, only 6 (31.6%) made follow-up appointments despite this intervention being successful in de-labeling inappropriate penicillin allergies. The reasons cited most often by patients who declined allergist referral or failed to schedule follow-up included that the patient lived far away from participating outpatient clinics, wanted to recover from surgery prior to making other appointments, or did not see value in scheduling an appointment. Data on cefazolin utilization post-education alone in the surgery types included in the pilot program could not be collected, as education was also incorporated into the pilot program.
Though the patient interview process was the main intervention in this study, provider education was also a key aspect of the pilot program. Surgeons received the updated surgical prophylaxis guideline and education about beta-lactam cross-reactivity in patients with documented penicillin allergies both prior to and within the pilot program. This education is necessary to reduce long-standing false beliefs about beta-lactam cross-reactivity, which lead to avoidance of the class in general; however, education alone is often ineffective in changing practice [17].
The full implications of this study for patient outcomes are difficult to measure, as patients in the intervention group will continue to receive benefit from the allergy clarification interview each time antibiotic therapy is considered for them in the future. The clarification interview and documentation in the medical record will optimize all future antibiotic selection for these patients. Additionally, based on the successful results of this pilot and positive feedback from providers and the pharmacy residents involved with this pilot program, a system-wide protocol is under development at the study institution. There is also potential to expand this service to other patient populations, including inpatient and outpatient care. This would help to catch patients who would typically not be able to be interviewed prior to urgent surgery when it is not feasible to complete an interview. A practice parameter update published in December 2022 in the Journal of Allergy and Clinical Immunology gives new recommendations for antibiotic allergies [18]. The authors recommend that patients with a non-anaphylactic penicillin allergy can receive cephalosporins regardless of the side chain similarities between penicillin and the cephalosporin agent. This recommendation may be of interest in future adaptations or implementation of de-labeling services at the study institution or other institutions.
5. Conclusions
The pharmacist-driven penicillin allergy de-labeling pilot program in CT and spine surgery patients was associated with increased cefazolin use. Further study is necessary to determine the full impact of pharmacist-driven penicillin allergy de-labelling on CT and spine surgery patients or other surgery types.
Author Contributions
All authors contributed substantially to the work reported. Conceptualization, K.G. and A.T.; methodology, K.G., A.S. and A.T.; formal analysis, A.S. and M.V.; investigation, H.C., B.G., A.S. and K.G.; data curation, H.C., B.G. and A.S.; writing—original draft preparation, H.C., B.G., K.G. and A.T.; writing—review and editing, H.C., B.G., K.G., A.T., A.S. and M.V.; visualization, A.T.; supervision, K.G.; project administration, K.G., H.C. and B.G.; funding acquisition, K.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Allina Health Foundation, grant number 21-0039.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, was approved by the Institutional Review Board of Allina Health, study number 1810409, and was determined to be exempt on 13 January 2022.
Informed Consent Statement
Patient consent was waived due to the following reasons: The use or disclosure of the protected health information involves no more than minimal risk to the privacy of individuals. This research could not have practicably been conducted without the waiver or alteration or without access to and use of the protected health information. This study was determined to be quality improvement and exempt from IRB review by the Allina Health Institutional Review Board according to federal regulation 45 CFR 46.104(d).
Data Availability Statement
The data used in this study are not publicly available due to health system data privacy restrictions.
Acknowledgments
Natalie Ha, Asha Farah, JoAn Hall, Annie Nguyen, Youchan Song, Cedrik Krouch, Michael Wankum, Justin Kirven, and William Hicks.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
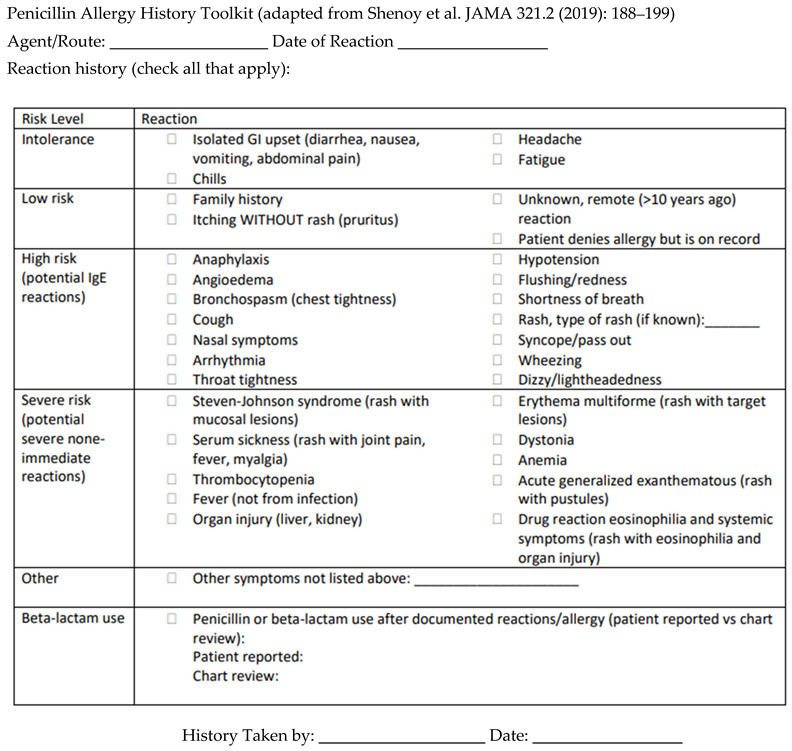
Appendix B
Algorithm for pharmacist-driven penicillin allergy de-labeling.
Appendix C
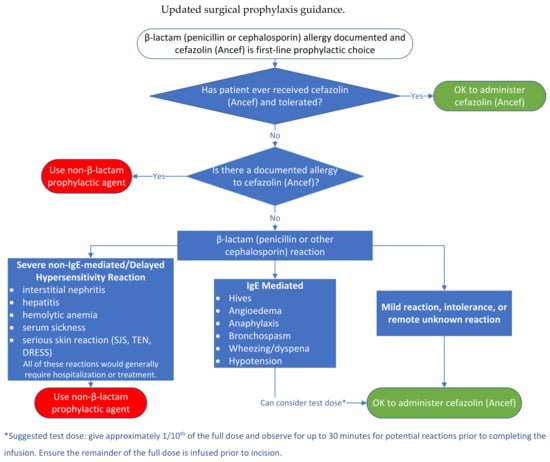
Figure A1.
A decision algorithm for the preoperative assessment and perioperative management of the patient reporting a β-lactam allergy and requiring cefazolin (Ancef®) antimicrobial prophylaxis. It should also be noted that the potential exists for patients to have separate, independent hypersensitivity reactions to two β-lactam antibiotics that are structurally unrelated [19]. SJS, Stevens Johnson Syndrome; TEN, toxic epidermal necrolysis, DRESS, drug rash eosinophilia and systemic symptoms.
Figure A1.
A decision algorithm for the preoperative assessment and perioperative management of the patient reporting a β-lactam allergy and requiring cefazolin (Ancef®) antimicrobial prophylaxis. It should also be noted that the potential exists for patients to have separate, independent hypersensitivity reactions to two β-lactam antibiotics that are structurally unrelated [19]. SJS, Stevens Johnson Syndrome; TEN, toxic epidermal necrolysis, DRESS, drug rash eosinophilia and systemic symptoms.

Appendix D
Beta-lactam cross-reactivity guidance in surgical prophylaxis guidelines.
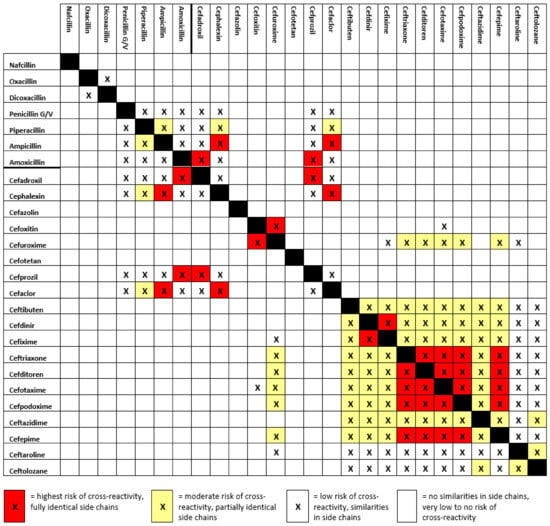
Figure A2.
Blank boxes imply no side chain similarities. Red colored boxes indicate β-lactams that share a fully identical R1 or R2 side chain structure. Yellow colored boxes indicate β-lactams with a partially identical (shared ring or branch chain structure) side chain(s) structure (either R1, R2 or both). Boxes with an “X” and no coloring indicate β-lactams with a similar R1 or R2 sidechain. Adapted from Zagursky R, et al. Cross-Reactivity in β-Lactam Allergy (2018) [19] to reflect products available in the United States and for ease of use. Carbapenems (imipenem, meropenem, ertapenem) are broad spectrum β-lactams, and through difference in parent structure and side chains are considered extremely low risk of cross reactivity with other β-lactams. Monobactams (aztreonam) are technically not β-lactams and carry an extremely low risk of cross reactivity with β-lactams outside of reported ceftazidime and cefiderocol allergies.
Figure A2.
Blank boxes imply no side chain similarities. Red colored boxes indicate β-lactams that share a fully identical R1 or R2 side chain structure. Yellow colored boxes indicate β-lactams with a partially identical (shared ring or branch chain structure) side chain(s) structure (either R1, R2 or both). Boxes with an “X” and no coloring indicate β-lactams with a similar R1 or R2 sidechain. Adapted from Zagursky R, et al. Cross-Reactivity in β-Lactam Allergy (2018) [19] to reflect products available in the United States and for ease of use. Carbapenems (imipenem, meropenem, ertapenem) are broad spectrum β-lactams, and through difference in parent structure and side chains are considered extremely low risk of cross reactivity with other β-lactams. Monobactams (aztreonam) are technically not β-lactams and carry an extremely low risk of cross reactivity with β-lactams outside of reported ceftazidime and cefiderocol allergies.

References
- Sacco, K.A.; Bates, A.; Brigham, T.J.; Imam, J.S.; Burton, M.C. Clinical outcomes following inpatient penicillin allergy testing: A systematic review and meta-analysis. Allergy 2017, 72, 1288–1296. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, K.G.; Lu, N.; Zhang, Y.; Li, Y.; Walensky, R.P.; Choi, H.K. Risk of meticillin resistant Staphylococcus aureus and Clostridium difficile in patients with a documented penicillin allergy: Population based matched cohort study. BMJ 2018, 361, k2400. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, K.G.; Ryan, E.E.; Li, Y.; Lee, H.; Kuhlen, J.L.; Shenoy, E.S. The Impact of a Reported Penicillin Allergy on Surgical Site Infection Risk. Clin. Infect. Dis. 2018, 66, 329–336. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, W.J.; Gupta, K.; Itani, K.M.F. Association of Postoperative Infection With Risk of Long-term Infection and Mortality. JAMA Surg. 2020, 155, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Badia, J.M.; Casey, A.L.; Petrosillo, N.; Hudson, P.M.; Mitchell, S.A.; Crosby, C. Impact of surgical site infection on healthcare costs and patient outcomes: A systematic review in six European countries. J. Hosp. Infect. 2017, 96, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Devchand, M.; Kirkpatrick, C.M.J.; Stevenson, W.; Garrett, K.; Perera, D.; Khumra, S.; Urbancic, K.; Grayson, M.L.; Trubiano, J.A. Evaluation of a pharmacist-led penicillin allergy de-labelling ward round: A novel antimicrobial stewardship intervention. J. Antimicrob. Chemother. 2019, 74, 1725–1730. [Google Scholar] [CrossRef] [PubMed]
- Graf, K.; Ott, E.; Vonberg, R.P.; Kuehn, C.; Haverich, A.; Chaberny, I.F. Economic aspects of deep sternal wound infections. Eur. J. Cardiothorac. Surg. 2010, 37, 893–896. [Google Scholar] [CrossRef] [PubMed]
- Kwiatkowski, S.; Mulugeta, S.; Davis, S.; Kenney, R.; Kalus, J.; Walton, L.; Patel, N. Optimizing preoperative antibiotics in patients with beta-lactam allergies: A role for pharmacy. Am. J. Health Syst. Pharm. 2021, 78, S76–S82. [Google Scholar] [CrossRef] [PubMed]
- Shenoy, E.S.; Macy, E.; Rowe, T.; Blumenthal, K.G. Evaluation and Management of Penicillin Allergy: A Review. JAMA 2019, 321, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Kalakoti, P.; Missios, S.; Maiti, T.; Konar, S.; Bir, S.; Bollam, P.; Nanda, A. Inpatient Outcomes and Postoperative Complications After Primary Versus Revision Lumbar Spinal Fusion Surgeries for Degenerative Lumbar Disc Disease: A National (Nationwide) Inpatient Sample Analysis, 2002–2011. World Neurosurg. 2016, 85, 114–124. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, A.; Staicu, M.L. Use of a Penicillin Allergy Screening Algorithm and Penicillin Skin Testing for Transitioning Hospitalized Patients to First-Line Antibiotic Therapy. J. Allergy Clin. Immunol. Pract. 2018, 6, 1349–1355. [Google Scholar] [CrossRef] [PubMed]
- Bratzler, D.W.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.G.; Slain, D.; et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg. Infect. 2013, 14, 73–156. [Google Scholar] [CrossRef] [PubMed]
- National Healthcare Safety Network. Surgical Site Infection Event (SSI). 2023. Available online: https://www.cdc.gov/nhsn/psc/ssi/index.html (accessed on 15 May 2023).
- Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Off. J. Int. Soc. Nephrol. 2012, 2, 1–138. [Google Scholar]
- Bouchard, J. Estimating Baseline Serum Creatinine for Assessing Acute Kidney Injury: Not a One Size Fits All Approach. Kidney Int. Rep. 2021, 6, 562–564. [Google Scholar] [CrossRef] [PubMed]
- Wade, S.; Marshall, E. A pharmacist-led penicillin allergy de-labelling project within a preoperative assessment clinic: The low-hanging fruit is within reach. J. Hosp. Infect. 2023, 139, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Satterfield, J.; Miesner, A.R.; Percival, K.M. The role of education in antimicrobial stewardship. J. Hosp. Infect. 2020, 105, 130–141. [Google Scholar] [CrossRef] [PubMed]
- Khan, D.A.; Banerji, A.; Blumenthal, K.G.; Phillips, E.J.; Solensky, R.; White, A.A.; Bernstein, J.A.; Chu, D.K.; Ellis, A.K.; Golden, D.B.K.; et al. Drug allergy: A 2022 practice parameter update. J. Allergy Clin. Immunol. 2022, 150, 1333–1393. [Google Scholar] [CrossRef] [PubMed]
- Zagursky, R.; Pichichero, M. Cross-Reactivity in β-Lactam Allergy. J. Allergy Clin. Immunol. Pract. 2018, 6, 72–81. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).

