Allergic Food Sensitization and Disease Manifestation in the Fetus and Infant: A Perspective
Abstract
1. Introduction
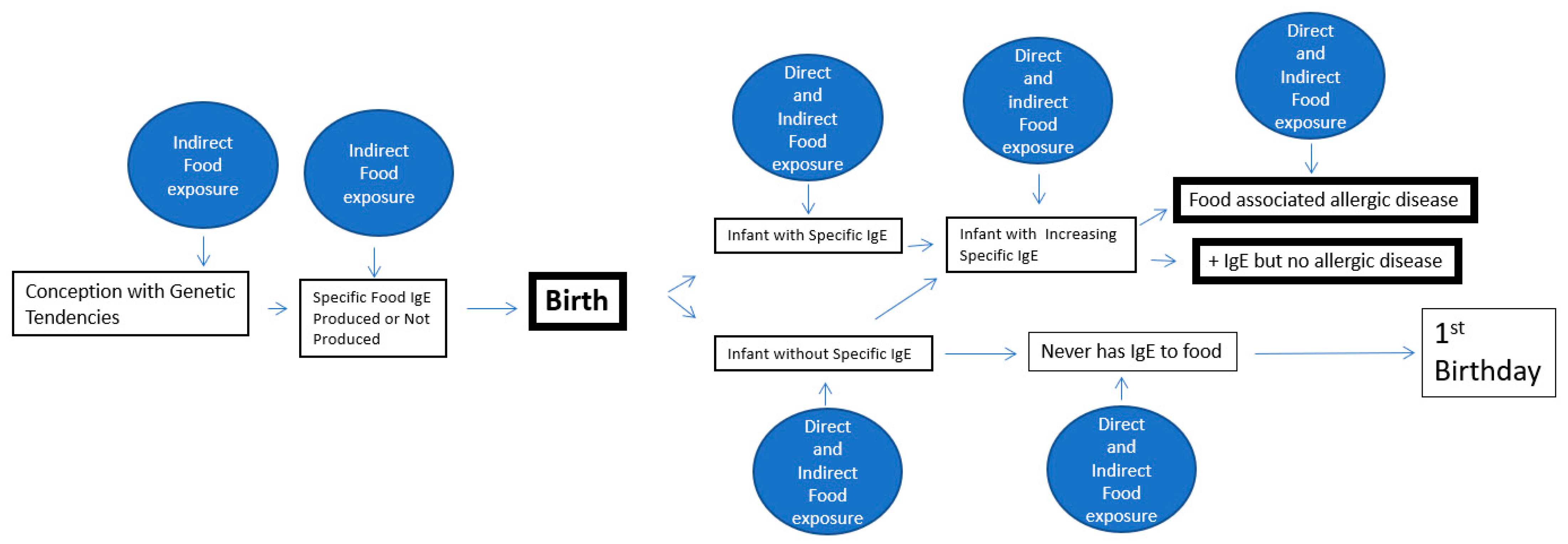
2. Genetic and Epigenetic Potentials
3. Fetal Immunity Development and the Production of IgE
4. Birth and Immediate Post-Birth Allergenic Experiences
5. Advancing Post-Uterine IgE Sensitization
6. Food-Associated IgE Mediated Allergic Diseases in Young Infants
7. Illustrative Case
8. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsuang, A.; Chan, E.S.; Wang, J. Food-induced anaphylaxis in infants: Can new evidence assist with implementation of food allergy prevention and treatment? J. Allergy Clin. Immunol. Pract. 2021, 9, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Steinke, J.W.; Borish, L.; Rosenwasser, L.J. 5. Genetics of hypersensitivity. J. Allergy Clin. Immunol. 2003, 111, S495–S501. [Google Scholar] [CrossRef]
- Hallas, H.W.; Chawes, B.L.; Arianto, L.; Rasmussen, M.A.; Kunøe, A.; Stokholm, J.; Bønnelykke, K.; Bisgaard, H. Children with asthma have fixed airway obstruction through childhood unaffected by exacerbations. J. Allergy Clin. Immunol. Pract. 2020, 8, 1263–1271.e3. [Google Scholar] [CrossRef]
- Hallas, H.W.; Chawes, B.L.; Rasmussen, M.A.; Arianto, L.; Stokholm, J.; Bønnelykke, K.; Bisgaard, H. Airway obstruction and bronchial reactivity from age 1 month until 13 years in children with asthma: A prospective birth cohort study. PLoS Med. 2019, 16, e1002722. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-C.; Chen, R.-F.; Kuo, H.-C. Different implications of paternal and maternal atopy for perinatal IgE production and asthma development. Clin. Dev. Immunol. 2012, 2012. [Google Scholar] [CrossRef]
- Noakes, P.S.; Holt, P.G.; Prescott, S.L. Maternal smoking in pregnancy alters neonatal cytokine responses. Allergy 2003, 58, 1053–1058. [Google Scholar] [CrossRef]
- Guerra, S.; Lombardi, E.; Stern, D.A.; Sherrill, D.L.; Gilbertson-Dahdal, D.; Wheatley-Guy, C.M.; Snyder, E.M.; Wright, A.L.; Martinez, F.D.; Morgan, W.J. Fetal origins of asthma: A longitudinal study from birth to age 36 years. Am. J. Respir. Crit. Care Med. 2020, 202, 1646–1655. [Google Scholar] [CrossRef] [PubMed]
- Ravn, N.H.; Halling, A.S.; Berkowitz, A.G.; Rinnov, M.R.; Silverberg, J.I.; Egeberg, A.; Thyssen, J.P. How does parental history of atopic disease predict the risk of atopic dermatitis in a child? A systematic review and meta-analysis. J. Allergy Clin. Immunol. 2020, 145, 1182–1193. [Google Scholar] [CrossRef]
- Steinke, J.W. Genetics of Hypersensitivity. In Allergy Frontiers: Epigenetics, Allergens and Risk Factors; Springer: Berlin/Heidelberg, Germany, 2009; pp. 227–238. [Google Scholar]
- Thomsen, S.F. Atopic dermatitis: Natural history, diagnosis, and treatment. Int. Sch. Res. Notices 2014, 2014. [Google Scholar] [CrossRef]
- Pfefferle, P.I.; Sel, S.; Ege, M.J.; Büchele, G.; Blümer, N.; Krauss-Etschmann, S.; Herzum, I.; Albers, C.E.; Lauener, R.P.; Roponen, M.; et al. Cord blood allergen-specific IgE is associated with reduced IFN-γ production by cord blood cells: The Protection against Allergy—Study in Rural Environments (PASTURE) Study. J. Allergy Clin. Immunol. 2008, 122, 711–716. [Google Scholar] [CrossRef] [PubMed]
- Brunner, P.M.; Israel, A.; Zhang, N.; Leonard, A.; Wen, H.C.; Huynh, T.; Tran, G.; Lyon, S.; Rodriguez, G.; Immaneni, S.; et al. Early-onset pediatric atopic dermatitis is characterized by TH2/TH17/TH22-centered inflammation and lipid alterations. J. Allergy Clin. Immunol. 2018, 141, 2094–2106. [Google Scholar] [CrossRef]
- Peng, C.; Cardenas, A.; Rifas-Shiman, S.L.; Hivert, M.F.; Gold, D.R.; Platts-Mills, T.A.; Lin, X.; Oken, E.; Baccarelli, A.A.; Litonjua, A.A.; et al. Epigenome-wide association study of total serum immunoglobulin E in children: A life course approach. Clin. Epigenetics 2018, 10, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lima, J.O.; Zhang, L.; Atkinson, T.P.; Philips, J.; Dasanayake, A.P.; Schroeder, H.W., Jr. Early expression of Iϵ, CD23 (FcϵRII), IL-4Rα, and IgE in the human fetus. J. Allergy Clin. Immunol. 2000, 106, 911–917. [Google Scholar] [CrossRef]
- Ekström, E.S.; Nilsson, C.; Holmlund, U.; Ploeg, I.V.; Sandstedt, B.; Lilja, G.; Scheynius, A. IgE is expressed on, but not produced by, fetal cells in the human placenta irrespective of maternal atopy. Clin. Exp. Immunol. 2002, 127, 274–282. [Google Scholar] [CrossRef]
- Sybilski, A.J.; Doboszynska, A.; Samolinski, B. Total and antigen-specific IGE levels in umbilical cord blood. Eur. J. Med Res. 2009, 14, 1–4. [Google Scholar] [CrossRef]
- Park, J.-E.; Jardine, L.; Gottgens, B.; Teichmann, S.A.; Haniffa, M. Prenatal development of human immunity. Science 2020, 368, 600–603. [Google Scholar] [CrossRef]
- Hopp, R.J. Hypersensitivity reactions: An everyday occurrence in pediatric allergy clinics. Pediatric Allergy Immunol. Pulmonol. 2020, 33, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Mimoun, A.; Delignat, S.; Peyron, I.; Daventure, V.; Lecerf, M.; Dimitrov, J.D.; Kaveri, S.V.; Bayry, J.; Lacroix-Desmazes, S. Relevance of the Materno-Fetal Interface for the Induction of Antigen-Specific Immune Tolerance. Front. Immunol. 2020, 11, 810. [Google Scholar] [CrossRef]
- McGovern, N.; Shin, A.; Low, G.; Low, D.; Duan, K.; Yao, L.J.; Msallam, R.; Low, I.; Shadan, N.B.; Sumatoh, H.R.; et al. Human fetal dendritic cells promote prenatal T-cell immune suppression through arginase-2. Nature 2017, 546, 662–666. [Google Scholar] [CrossRef] [PubMed]
- Arshad, S.H. Primary prevention of asthma and allergy. J. Allergy Clin. Immunol. 2005, 116, 3–14. [Google Scholar] [CrossRef]
- Chen, C.H. Predictors of Cord Blood Immunoglobulin (IgE) Levels. 2009. Available online: Clinicaltrials.gov (accessed on 3 January 2021).
- Szépfalusi, Z.; Loibichler, C.; Pichler, J.; Reisenberger, K.; Ebner, C.; Urbanek, R.; Sz, Z. Direct evidence for transplacental allergen transfer. Pediatric Res. 2000, 48, 404–407. [Google Scholar] [CrossRef] [PubMed]
- Msallam, R.; Balla, J.; Rathore, A.P.; Kared, H.; Malleret, B.; Saron, W.A.; Liu, Z.; Hang, J.W.; Dutertre, C.A.; Larbi, A.; et al. Fetal mast cells mediate postnatal allergic responses dependent on maternal IgE. Science 2020, 370, 941–950. [Google Scholar] [CrossRef] [PubMed]
- Fan, B. Nutrition during Pregnancy. Part 1: Weight Gain. Part 2: Nutrient Supplements; National Academy of Sciences, Institute of Medicine: Washington, DC, USA, 1990. [Google Scholar]
- Larqué, E.; Ruiz-Palacios, M.; Koletzko, B. Placental regulation of fetal nutrient supply. Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Vichyanond, P. Localized abdominal urticaria: A distinct clinical phenotype of wheat allergy in young children. J. Allergy Clin. Immunol. Pract. 2020, 8, 3650–3652.e1. [Google Scholar] [CrossRef]
- Renz-Polster, H.; David, M.R.; Buist, A.S.; Vollmer, W.M.; O’connor, E.A.; Frazier, E.A.; Wall, M.A. Caesarean section delivery and the risk of allergic disorders in childhood. Clin. Exp. Allergy 2005, 35, 1466–1472. [Google Scholar] [CrossRef]
- Samady, W.; Trainor, J.; Smith, B.; Gupta, R. Food-induced anaphylaxis in infants and children. Ann. Allergy Asthma Immunol. 2018, 121, 360–365. [Google Scholar] [CrossRef]
- Pouessel, G.; Beaudouin, E.; Tanno, L.K.; Drouet, M.; Deschildre, A.; Labreuche, J.; Renaudin, J.M. Network AV.Food-related anaphylaxis fatalities: Analysis of the Allergy Vigilance Network® database. Allergy 2019, 74, 1193–1196. [Google Scholar] [CrossRef]
- Rajani, P.S.; Martin, H.; Groetch, M.; Järvinen, K.M. Presentation and management of food allergy in breastfed infants and risks of maternal elimination diets. J. Allergy Clin. Immunol. Pract. 2020, 8, 52–67. [Google Scholar] [CrossRef]
- Arima, T.; Campos-Alberto, E.; Funakoshi, H.; Inoue, Y.; Tomiita, M.; Kohno, Y.; Shimojo, N. Immediate systemic allergic reaction in an infant to fish allergen ingested through breast milk. Asia Pac. Allergy 2016, 6, 257. [Google Scholar] [CrossRef][Green Version]
- Monti, G.; Marinaro, L.; Libanore, V.; Peltran, A.; Muratore, M.C.; Silvestro, L. Anaphylaxis Due to Fish Hypersensitivity in an Exclusively Breastfed Infant; Università degli Studi di Torino: Torino, Italy, 2006. [Google Scholar]
- Fleischer, D.M.; Conover-Walker, M.K.; Christie, L.; Burks, A.W.; Wood, R.A. Peanut allergy: Recurrence and its management. J. Allergy Clin. Immunol. 2004, 114, 1195–1201. [Google Scholar] [CrossRef]
- Tan, B.M.; Sher, M.R.; Good, R.A.; Bahna, S.L. Severe food allergies by skin contact. Ann. Allergy Asthma Immunol. 2001, 86, 583–586. [Google Scholar] [CrossRef]
- Bawany, F.; Beck, L.A.; Järvinen, K.M. Halting the march: Primary prevention of atopic dermatitis and food allergies. J. Allergy Clin. Immunol. Pract. 2020, 8, 860–875. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, A.; Kakourou, T.; Orfanou, I.; Xaidara, A.; Chrousos, G. Retrospective analysis of the relationship between infantile seborrheic dermatitis and atopic dermatitis. Pediatric Dermatol. 2014, 31, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Elias, P.M.; Schmuth, M. Abnormal skin barrier in the etiopathogenesis of atopic dermatitis. Curr. Allergy Asthma Rep. 2009, 9, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Satitsuksanoa, P.; van de Veen, W.; Akdis, M. B cells in food allergy. J. Allergy Clin. Immunol. 2021, 147, 49–51. [Google Scholar] [CrossRef]
- Brough, H.A.; Makinson, K.; Penagos, M.; Maleki, S.J.; Cheng, H.; Douiri, A.; Stephens, A.C.; Turcanu, V.; Lack, G. Distribution of peanut protein in the home environment. J. Allergy Clin. Immunol. 2013, 132, 623–629. [Google Scholar] [CrossRef]
- Irahara, M.; Shinahara, W.; Sugimoto, M.; Ogawa, Y.; Shitsukawa, K.; Kubota, K.; Yang, L.; Ohya, Y.; Saito, H.; Kagami, S.; et al. Trajectories of class–switching-related egg and cow’s milk allergen-specific immunoglobulin isotype formation and its modification by eczema with low-and high-affinity immunoglobulin E during early infancy. Immun. Inflamm. Dis. 2019, 7, 74–85. [Google Scholar] [CrossRef]
- Brunner, P.M. Early immunologic changes during the onset of atopic dermatitis. Ann. Allergy Asthma Immunol. 2019, 123, 152–157. [Google Scholar] [CrossRef]
- Silverberg, N.B. A practical overview of pediatric atopic dermatitis, part 1: Epidemiology and pathogenesis. Cutis 2016, 97, 267–271. [Google Scholar] [PubMed]
- Siegfried, E.C.; Hebert, A.A. Diagnosis of atopic dermatitis: Mimics, overlaps, and complications. J. Clin. Med. 2015, 4, 884–917. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.-E.; Chehade, M. Development of IgE-mediated immediate hypersensitivity to a previously tolerated food following its avoidance for eosinophilic gastrointestinal diseases. J. Allergy Clin. Immunology. Pract. 2018, 6, 649–650. [Google Scholar] [CrossRef] [PubMed]
- Pensabene, L.; Salvatore, S.; D’Auria, E.; Parisi, F.; Concolino, D.; Borrelli, O.; Thapar, N.; Staiano, A.; Vandenplas, Y.; Saps, M. Cow’s milk protein allergy in infancy: A risk factor for functional gastrointestinal disorders in children? Nutrients 2018, 10, 1716. [Google Scholar] [CrossRef]
- Caubet, J.C.; Szajewska, H.; Shamir, R.; Nowak-Węgrzyn, A. Non-IgE-mediated gastrointestinal food allergies in children. Pediatric Allergy Immunol. 2017, 28, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Venter, C.; Brown, T.; Meyer, R.; Walsh, J.; Shah, N.; Nowak-Węgrzyn, A.; Chen, T.X.; Fleischer, D.M.; Heine, R.G.; Levin, M.; et al. Better recognition, diagnosis and management of non-IgE-mediated cow’s milk allergy in infancy: iMAP—an international interpretation of the MAP (Milk Allergy in Primary Care) guideline. Clin. Transl. Allergy 2018, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Maciag, M.C.; Bartnikas, L.M.; Sicherer, S.H.; Herbert, L.J.; Young, M.C.; Matney, F.; Westcott-Chavez, A.A.; Petty, C.R.; Phipatanakul, W.; Bingemann, T.A. A Slice of Food Protein–Induced Enterocolitis Syndrome (FPIES): Insights from 441 Children with FPIES as Provided by Caregivers in the International FPIES Association. J. Allergy Clin. Immunol. Pract. 2020, 8, 1702–1709. [Google Scholar] [CrossRef] [PubMed]
- Martin, V.M.; Virkud, Y.V.; Seay, H.; Hickey, A.; Ndahayo, R.; Rosow, R.; Southwick, C.; Elkort, M.; Gupta, B.; Kramer, E.; et al. Prospective Assessment of Pediatrician-Diagnosed Food Protein–Induced Allergic Proctocolitis by Gross or Occult Blood. J. Allergy Clin. Immunol. Pract. 2020, 8, 1692–1699.e1. [Google Scholar] [CrossRef] [PubMed]
- Martin, V.M.; Virkud, Y.V.; Phadke, N.A.; Su, K.W.; Seay, H.; Atkins, M.R.; Keet, C.; Shreffler, W.G.; Yuan, Q. Increased IgE-Mediated Food Allergy With Food Protein-Induced Allergic Proctocolitis. Pediatrics 2020, 146. [Google Scholar] [CrossRef]
- Erwin, E.A.; James, H.R.; Gutekunst, H.M.; Russo, J.M.; Kelleher, K.J.; Platts-Mills, T.A. Serum IgE measurement and detection of food allergy in pediatric patients with eosinophilic esophagitis. Ann. Allergy Asthma Immunol. 2010, 104, 496–502. [Google Scholar] [CrossRef]
- Huang, S.W. Follow-up of children with rhinitis and cough associated with milk allergy. Pediatric Allergy Immunol. 2007, 18, 81–85. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hopp, R.J.; Salazar, P.; Pasha, M.A. Allergic Food Sensitization and Disease Manifestation in the Fetus and Infant: A Perspective. Allergies 2021, 1, 115-122. https://doi.org/10.3390/allergies1020009
Hopp RJ, Salazar P, Pasha MA. Allergic Food Sensitization and Disease Manifestation in the Fetus and Infant: A Perspective. Allergies. 2021; 1(2):115-122. https://doi.org/10.3390/allergies1020009
Chicago/Turabian StyleHopp, Russell J., Peggy Salazar, and Muhammad Asghar Pasha. 2021. "Allergic Food Sensitization and Disease Manifestation in the Fetus and Infant: A Perspective" Allergies 1, no. 2: 115-122. https://doi.org/10.3390/allergies1020009
APA StyleHopp, R. J., Salazar, P., & Pasha, M. A. (2021). Allergic Food Sensitization and Disease Manifestation in the Fetus and Infant: A Perspective. Allergies, 1(2), 115-122. https://doi.org/10.3390/allergies1020009





