Using Community Detection Analysis to Elucidate Caregivers’ Mental Models of Pediatric Concussion Symptoms
Abstract
1. Introduction
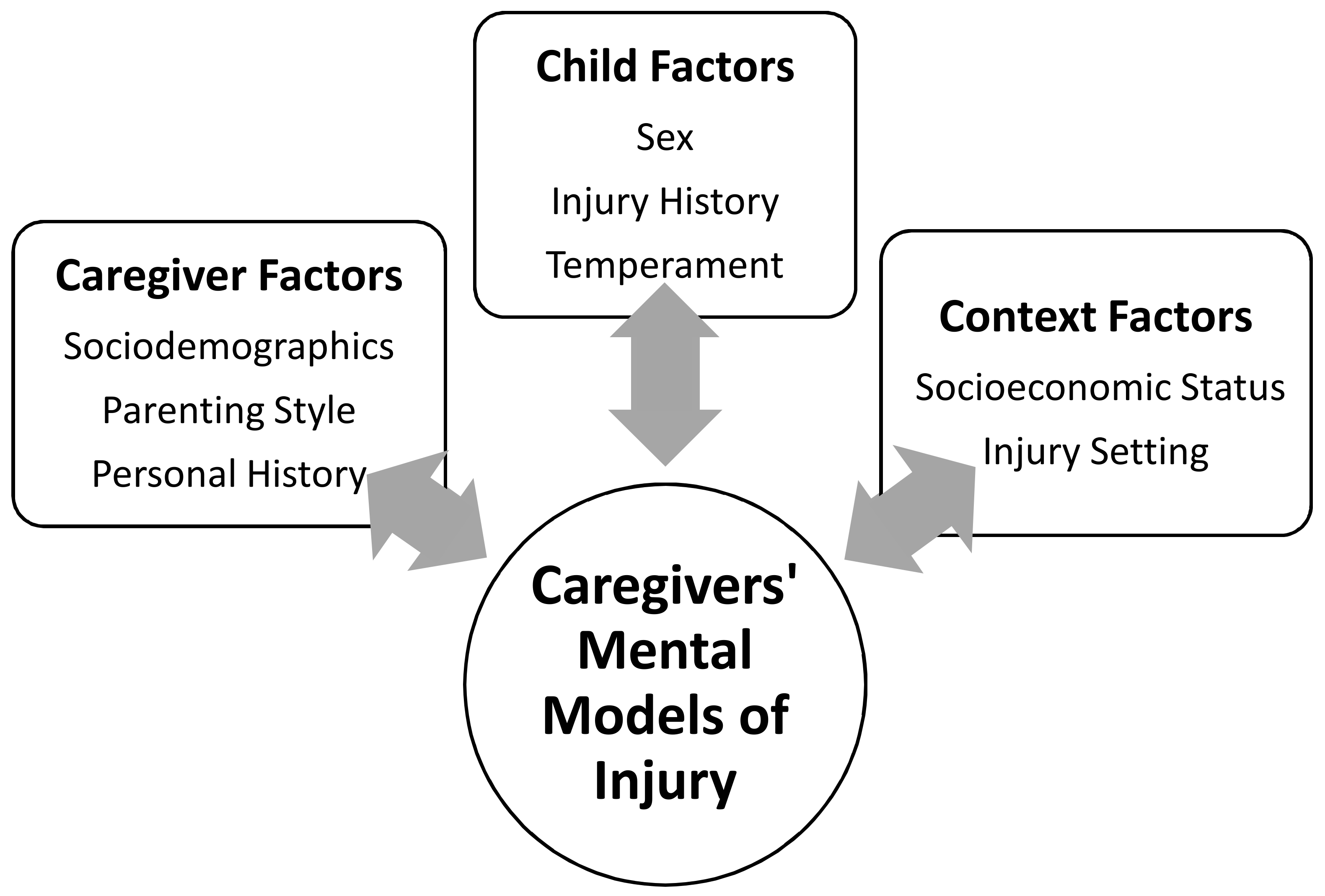
1.1. Theoretical Frameworks of Injury Prevention
1.1.1. Factors Associated with Childhood Injury Risk
1.1.2. Applying these Factors to Understand Caregivers’ Mental Models
1.2. The Current Study
2. Materials and Methods
2.1. Participants
2.2. Survey
2.3. Analytic Approach
2.3.1. Community Detection Analysis
2.3.2. Comparing Clusters Across Sociodemographics, Injury History, and Play Preference
3. Results
3.1. Community Detection Analysis Results
3.2. Logistic Regression Results
4. Discussion
4.1. Practical Applications
4.2. Limitations and Future Directions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Baillargeon, A.; Lassonde, M.; Leclerc, S.; Ellemberg, D. Neuropsychological and neurophysiological assessment of sport concussion in children, adolescents and adults. Brain Inj. 2012, 26, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Toledo, E.; Lebel, A.; Becerra, L.; Minster, A.; Linnman, C.; Maleki, N.; Dodick, D.W.; Borsook, D. The young brain and concussion: Imaging as a biomarker for diagnosis and prognosis. Neurosci. Biobehav. Rev. 2012, 36, 1510–1531. [Google Scholar] [CrossRef] [PubMed]
- Bakhos, L.L.; Lockhart, G.R.; Myers, R.; Linakis, J.G. Emergency Department Visits for Concussion in Young Child Athletes. Pediatrics 2010, 126. [Google Scholar] [CrossRef] [PubMed]
- Stewart, T.C.; Gilliland, J.; Fraser, D. An epidemiologic profile of pediatric concussions: Identifying urban and rural differences. J. Trauma Acute Care Surg. 2014, 76, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Shi, J.; Stanley, R.M.; Sribnick, E.A.; Groner, J.I.; Xiang, H. U.S. trends of ED visits for pediatric traumatic brain injuries: Implications for clinical trials. Int. J. Environ. Res. Public Health 2017, 14, 414. [Google Scholar] [CrossRef] [PubMed]
- Register-Mihalik, J.K.; Guskiewicz, K.M.; McLeod, T.C.V.; Linnan, L.A.; Mueller, F.O.; Marshall, S.W. Knowledge, attitude, and concussion-reporting behaviors among high school athletes: A preliminary study. J. Athl. Train. 2013, 48, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Williamson, I.J.S.; Goodman, D. Converging evidence for the under-reporting of concussions in youth ice hockey. Br. J. Sports Med. 2006, 40, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Sye, G.; Sullivan, S.J.; McCrory, P. High school rugby players’ understanding of concussion and return to play guidelines. Br. J. Sports Med. 2006, 40, 1003–1005. [Google Scholar] [CrossRef] [PubMed]
- McCrea, M.; Hammeke, T.; Olsen, G.; Leo, P.; Guskiewicz, K.M. Unreported concussion in high school football players: Implications for prevention. Clin. J. Sport Med. 2004, 14, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Graham, R.; Rivara, F.P.; Ford, M.A.; Spicer, C.M. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture; National Academies Press: Washington, DC, USA, 2014. [Google Scholar]
- Hassen, G.W.; Tinnesz, N.; Popkin, M.; Pingle, A.; Umandap, C.; Sethuraman, V.; Warren, R.; Villa, J.A.C.; Kalantari, H. Concussion awareness among children and their care givers. Am. J. Emerg. Med. 2018, in press. [Google Scholar] [CrossRef] [PubMed]
- Kerr, Z.Y.; Register-Mihalik, J.K.; Marshall, S.W.; Evenson, K.R.; Mihalik, J.P.; Guskiewicz, K.M. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: Review and application of the socio-ecological framework. Brain Inj. 2014, 28, 1009–1021. [Google Scholar] [CrossRef] [PubMed]
- Austin, L.C.; Fischhoff, B. Injury prevention and risk communication: A mental models approach. Inj. Prev. 2012, 18, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Doyle, J.K.; Ford, D.N. Mental models concepts for system dynamics research. Syst. Dyn. Rev. 1998, 14, 3–29. [Google Scholar] [CrossRef]
- Schwebel, D.; Gaines, J. Pediatric unintentional injury: Behavioral risk factors and implications for prevention. J. Dev. Behav. Pediatr. 2007, 28, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Rosen, B.N.; Peterson, L. Gender differences in children’s outdoor injuries: A review and an integration. Clin. Psychol. Rev. 1990, 10, 187–205. [Google Scholar] [CrossRef]
- Collins, M.W.; Grindel, S.H.; Lovell, M.R.; Dede, D.E.; Moser, D.J.; Phalin, B.R.; Nogle, S.; Wasik, M.; Cordry, D.; Daugherty, M.K.; et al. Relationship between concussion and neuropsychological performance in college football players. Jama 1999, 282, 946–970. [Google Scholar] [CrossRef]
- Alosco, M.L.; Fedor, A.F.; Gunstad, J. Attention deficit hyperactivity disorder as a risk factor for concussions in NCAA division-I athletes. Brain Inj. 2014, 28, 472–474. [Google Scholar] [CrossRef] [PubMed]
- Kerr, Z.Y.; Evenson, K.R.; Rosamond, W.D.; Mihalik, J.P.; Guskiewicz, K.M.; Marshall, S.W. Association between concussion and mental health in former collegiate athletes. Inj. Epidemiol. 2014, 1, 28. [Google Scholar] [CrossRef] [PubMed]
- DiScala, C.; Lescohier, I.; Barthel, M.; Li, G. Injuries to children with Attention Deficit Hyperactivity Disorder. Pediatrics 1998, 102, 1415–1421. [Google Scholar] [CrossRef] [PubMed]
- Merrill, R.M.; Lyon, J.L.; Baker, R.K.; Gren, L.H. Attention deficit hyperactivity disorder and increased risk of injury. Adv. Med. Sci. 2009, 54, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Brehaut, J.C.; Miller, A.; Raina, P.; McGrail, K.M. Childhood Behavior Disorders and injuries among children and youth: A population-based study. Pediatrics 2003, 111, 262. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, A.M.; Arnett, P.A. The development of a survey to examine knowledge about and attitudes towards concussion in high-school students. J. Clin. Exp. Neuropsychol. 2010, 32, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Abrahams, S.; Mc Fie, S.; Patricios, J.; Posthumus, M.; September, A.V. Risk factors for sports concussion: An evidence-based systematic review. Br. J. Sports Med. 2013, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Nordström, A.; Nordström, P.; Ekstrand, J. Sports-related concussion increases the risk of subsequent injury by about 50% in elite male football players. Br. J. Sports Med. 2014, 48, 1447–1450. [Google Scholar] [CrossRef] [PubMed]
- Schulz, M.R.; Marshall, S.W.; Mueller, F.O.; Yang, J.; Weaver, N.L.; Kalsbeek, W.D.; Bowling, J.M. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996–1999. Am. J. Epidemiol. 2004, 160, 937–944. [Google Scholar] [CrossRef] [PubMed]
- Nocera, M.; Gjelsvik, A.; Wing, R.; Amanullah, S. The Association of Parental Coping and Childhood Injury. Matern. Child. Health J. 2016, 20, 2357–2366. [Google Scholar] [CrossRef] [PubMed]
- Morrongiello, B.A.; House, K. Measuring parent attributes and supervision behaviors relevant to child injury risk: Examining the usefulness of questionnaire measures. Inj. Prev. 2004, 10, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Morrongiello, B.A.; Corbett, M.; Lasenby, J.; Johnston, N.; McCourt, M. Factors influencing young children’s risk of unintentional injury: Parenting style and strategies for teaching about home safety. J. Appl. Dev. Psychol. 2006, 27, 560–570. [Google Scholar] [CrossRef]
- Field, T. Postpartum depression effects on early interactions, parenting, and safety practices: A Review. Infant Behav. Dev. 2010, 33, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Morrongiello, B.A.; Corbett, M.; McCourt, M.; Johnston, N. Understanding unintentional injury-risk in young children I. The nature and scope of caregiver supervision of children at home. J. Pediatr. Psychol. 2006, 31, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, K.V.; Iwashyna, T.J. Child injury risks are close to home: Parent psychosocial factors associated with child safety. Matern. Child Health J. 2007, 11, 269–275. [Google Scholar] [CrossRef] [PubMed]
- McKinlay, A.; Kyonka, E.G.; Grace, R.C.; Horwood, L.J.; Fergusson, D.M.; MacFarlane, M.R. An investigation of the pre-injury risk factors associated with children who experience traumatic brain injury. Inj. Prev. 2010, 16, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Schwebel, D.C.; Brezausek, C.M.; Ramey, S.L.; Ramey, C.T. Interactions between child behavior patterns and parenting: Implications for children’s unintentional injury risk. J. Pediatr. Pychol. 2004, 29, 93–109. [Google Scholar] [CrossRef]
- Faelker, T.; Pickett, W.; Brison, R.J. Socioeconomic differences in childhood injury: A population based epidemiologic study in Ontario, Canada. Inj. Prev. 2000, 6, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Schwebel, D.C.; Roth, D.L.; Elliott, M.N.; Windle, M.; Grunbaum, J.A.; Low, B.; Cooper, S.P.; Schuster, M.A. The association of activity level, parent mental distress, and parental involvement and monitoring with unintentional injury risk in fifth graders. Accid. Anal. Prev. 2011, 43, 848–852. [Google Scholar] [CrossRef] [PubMed]
- Morrongiello, B.A.; Walpole, B.; Lasenby, J. Understanding children’s injury-risk behavior: Wearing safety gear can lead to increased risk taking. Accid. Anal. Prev. 2007, 39, 618–623. [Google Scholar] [CrossRef] [PubMed]
- Morrongiello, B.A.; Hogg, K. Mothers’ reactions to children misbehaving in ways that can lead to injury: Implications for gender differences in children’s risk taking and injuries. Sex Roles 2004, 50, 103–118. [Google Scholar] [CrossRef]
- Kroshus, E.; Babkes Stellino, M.; Chrisman, S.P.D.; Rivara, F.P. Threat, pressure, and communication about concussion safety: Implications for parent concussion education. Health Educ. Behav. 2017, 45, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.C.; Salzman, G.A.; Bachman, S.L.; Burke, R.V.; Zaslow, T.; Piasek, C.Z.; Edison, B.R.; Hamilton, A.; Upperman, J.S. Assessment of parental knowledge and attitudes toward pediatric sports-related concussions. Sports Health 2015, 7, 124–129. [Google Scholar] [CrossRef] [PubMed]
- McNally, K.A.; Bangert, B.; Dietrich, A.; Nuss, K.; Rusin, J.; Wright, M.; Taylor, H.G.; Yeates, K.O. Injury versus noninjury factors as predictors of postconcussive symptoms following mild traumatic brain injury in children. Neuropsychology 2013, 27, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Dick, R.W. Is there a gender difference in concussion incidence and outcomes? Br. J. Sports Med. 2009, 43, i46–i50. [Google Scholar] [CrossRef] [PubMed]
- Covassin, T.; Elbin, R.J. The female athlete: The role of gender in the assessment and management of sport-related concussion. Clin. Sports Med. 2011, 30, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Haarbauer-Krupa, J.; Arbogast, K.B.; Metzger, K.B.; Greenspan, A.I.; Kessler, R.; Curry, A.E.; Bell, J.M.; DePadilla, L.; Pfeiffer, M.R.; Zonfrillo, M.R.; et al. Variations in mechanisms of injury for children with concussion. J. Pediatr. 2018, 197, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Barnes, B.C.; Cooper, L.; Kirkendall, D.T.; McDermott, T.P.; Jordan, B.D.; Garrett, W.E. Concussion history in elite male and female soccer players. Am. J. Sports Med. 1998, 26, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Pardini, D.; Stump, J.; Lovell, M.; Collins, M.; Moritz, K.; Fu, F. The Post-concussion Symptom Scale (pcss): A Factor Analysis. Br. J. Sports Med. 2004, 38, 661–662. [Google Scholar]
- Kontos, A.P.; Elbin, R.J.; Schatz, P.; Covassin, T.; Henry, L.; Pardini, J.; Collins, M.W. A revised factor structure for the post-concussion symptom scale: Baseline and postconcussion factors. Am. J. Sports Med. 2012, 40, 2375–2384. [Google Scholar] [CrossRef] [PubMed]
- Kay, M.C.; Register-Mihalik, J.K.; Ford, C.B.; Williams, R.M.; McLeod, T.C.V. Parents’ and child’s concussion history as predictors of parental attitudes and knowledge of concussion recognition and response. Orthop. J. Sport. Med. 2017, 5, 12. [Google Scholar] [CrossRef] [PubMed]
- Kaut, K.P.; DePompei, R.; Kerr, J.; Congeni, J. Reports of head injury and symptom knowledge among college athletes: Implications for assessment and educational intervention. Clin. J. Sport Med. 2003, 13, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Kroshus, E.; Baugh, C.M.; Daneshvar, D.H.; Viswanath, K. Understanding concussion reporting using a model based on the theory of planned behavior. J. Adolesc. Health 2014, 54, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.L.; Sheeran, P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol. Bull. 2006, 132, 249. [Google Scholar] [CrossRef] [PubMed]
- Armitage, C.J.; Conner, M. Efficacy of the theory of planned behaviour: A meta-analytic review. Br. J. Soc. Psychol. 2001, 40, 471–499. [Google Scholar] [CrossRef] [PubMed]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B 1995, 289–300. [Google Scholar] [CrossRef]
- Breslow, N. A generalized Kruskal-Wallis test for comparing K samples subject to unequal patterns of censorship. Biometrika 1970, 57, 579–594. [Google Scholar] [CrossRef]
- Newman, M.E.J. Detecting community structure in networks. Eur. Phys. J. B 2004, 32, 321–330. [Google Scholar] [CrossRef]
- Girvan, M.; Newman, M.E.J. Community structure in social and biological networks. Proc. Natl. Acad. Sci. USA 2002, 99, 7821–7826. [Google Scholar] [CrossRef] [PubMed]
- Fair, D.A.; Bathula, D.; Nikolas, M.A.; Nigg, J.T. Distinct neuropsychological subgroups in typically developing youth inform heterogeneity in children with ADHD. Proc. Natl. Acad. Sci. USA 2012, 109, 6769–6774. [Google Scholar] [CrossRef] [PubMed]
- Karalunas, S.L.; Fair, D.; Musser, E.D.; Aykes, K.; Iyer, S.P.; Nigg, J.T. Subtyping attention-deficit/hyperactivity disorder using temperament dimensions. JAMA Psychiatry 2014, 71, 1015. [Google Scholar] [CrossRef] [PubMed]
- Meunier, D.; Achard, S.; Morcom, A.; Bullmore, E. Age-related changes in modular organization of human brain functional networks. Neuroimage 2009, 44, 715–723. [Google Scholar] [CrossRef] [PubMed]
- Team, R.C. R: A language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2014. Available online: http://softlibre.unizar.es/manuales/aplicaciones/r/fullrefman.pdf (accessed on 5 July 2018).
- Stevens, P.K.; Penprase, B.; Kepros, J.P.; Dunneback, J. Parental recognition of postconcussive symptoms in children. J. Trauma Nurs. 2010, 17, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Coghlin, C.J.; Myles, B.D.; Howitt, S.D. The ability of parents to accurately report concussion occurrence in their bantam-aged minor hockey league children. J. Can. Chiropr. Assoc. 2009, 53, 233–250. [Google Scholar] [PubMed]
- Topolovec-Vranic, J.; Zhang, S.; Wong, H.; Lam, E.; Jing, R.; Russell, K.; Cusimano, M.D. Recognizing the symptoms of mental illness following concussions in the sports community: A need for improvement. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [PubMed]
- Mannings, C.; Kalynych, C.; Joseph, M.M.; Smotherman, C.; Kraemer, D.F. Knowledge assessment of sports-related concussion among parents of children aged 5 years to 15 years enrolled in recreational tackle football. J. Trauma Acute Care Surg. 2014, 77, S18–S22. [Google Scholar] [CrossRef] [PubMed]
- Chrisman, S.P.; Quitiquit, C.; Rivara, F.P. Qualitative study of barriers to concussive symptom reporting in high school athletics. J. Adolesc. Health 2013, 52, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Rowhani-Rahbar, A.; Chrisman, S.P.D.; Drescher, S.; Schiff, M.A.; Rivara, F.P. Agreement between high school athletes and their parents on reporting athletic events and concussion symptoms. J. Neurotrauma 2016, 33, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Porter, S.; Smith-Forrester, J.; Alhajri, N.; Kusch, C.; Sun, J.; Barrable, B.; Paneka, W.J.; Virji-Babul, N. The Child Sport Concussion Assessment Tool (Child SCAT3): Normative values and correspondence between child and parent symptom scores in male child athletes. BMJ Open Sport Exerc. Med. 2015, 1. [Google Scholar] [CrossRef] [PubMed]
- Turner, R.W.; Lucas, J.W.; Margolis, L.H.; Corwell, B.N. A preliminary study of youth sport concussions: Parents’ health literacy and knowledge of return-to-play protocol criteria. Brain Inj. 2017, 31, 1124–1130. [Google Scholar] [CrossRef] [PubMed]

| Variable | Levels of Variable | Total | % |
|---|---|---|---|
| Child Gender | Male | 43 | 57 |
| Female | 33 | 43 | |
| Child Age (years) | 10 | 6 | 7 |
| 11 | 15 | 20 | |
| 12 | 16 | 21 | |
| 13 | 9 | 12 | |
| 14 | 15 | 20 | |
| 15 | 15 | 20 | |
| Caregiver Gender | Male | 20 | 26 |
| Female | 53 | 70 | |
| Unknown | 3 | 4 | |
| Caregiver Age | 26–30 | 4 | 5 |
| 31–35 | 6 | 8 | |
| 36–40 | 12 | 16 | |
| 41–45 | 21 | 28 | |
| 46–50 | 25 | 33 | |
| 51–55 | 5 | 7 | |
| 56–60 | 3 | 4 | |
| Ethnicity (Caregiver) | White | 60 | 79 |
| African American | 13 | 17 | |
| Native American | 1 | 1 | |
| Other | 2 | 3 | |
| Marital Status | Never Married | 6 | 8 |
| Divorced | 8 | 11 | |
| Widow | 3 | 4 | |
| Married | 57 | 75 | |
| Domestic Partnership | 1 | 1 | |
| Refused | 1 | 1 | |
| Caregiver’s Education Level | Some High School | 1 | 1 |
| High School | 10 | 13 | |
| GED | 1 | 1 | |
| Some College | 6 | 8 | |
| Associates | 14 | 18 | |
| 4-year Degree | 27 | 36 | |
| Masters/Doctorate | 17 | 22 | |
| Insurance | CHIP * | 1 | 1 |
| Medicaid | 12 | 16 | |
| Private/Employer Provided | 60 | 79 | |
| Other | 3 | 4 |
| Symptom | Sport Mean (SD) | Fight Mean (SD) | Fall Mean (SD) | Across Context Mean (SD) | p |
|---|---|---|---|---|---|
| Headache | 2.75 (0.90) | 2.83 (0.95) | 3.16 (0.82) | 2.91 (0.70) | 0.01 |
| Neck Pain | 3.07 (0.85) | 2.95 (0.86) | 3.21 (0.72) | 3.10 (0.72) | 0.14 |
| Blurred Vision | 3.79 (0.44) | 3.78 (0.45) | 3.82 (0.42) | 3.80 (0.40) | 0.85 |
| Bruise, Bump, Laceration | 2.84 (0.97) | 2.95 (0.90) | 2.95 (0.93) | 2.90 (0.88) | 0.72 |
| Sensitivity to Light and Noise | 3.56 (0.66) | 3.63 (0.59) | 3.55 (0.68) | 3.60 (0.59) | 0.71 |
| Difficulty Concentrating | 3.42 (0.70) | 3.36 (0.72) | 3.48 (0.67) | 3.43 (0.65) | 0.58 |
| Feeling Sleepier | 3.35 (0.81) | 3.36 (0.83) | 3.42 (0.81) | 3.37 (0.80) | 0.87 |
| Difficulty Falling/Staying Asleep | 2.92 (0.96) | 2.86 (0.97) | 2.95 (0.92) | 2.91 (0.93) | 0.83 |
| Increased Irritability/More Emotional | 2.62 (0.86) | 2.62 (0.91) | 2.68 (0.91) | 2.62 (0.87) | 0.87 |
| Dizziness | 3.64 (0.65) | 3.60 (0.66) | 3.65 (0.60) | 3.64 (0.54) | 0.87 |
| Vomiting | 3.53 (0.66) | 3.49 (0.68) | 3.54 (0.68) | 3.53 (0.60) | 0.97 |
| Loss of Consciousness | 3.92 (0.39) | 3.94 (0.38) | 3.94 (0.38) | 3.96 (0.17) | 0.90 |
| Symptom | Cluster Assignment | Median | IQR (50%) |
|---|---|---|---|
| Increased Irritability/More Emotional | 1 | 2.0 | 2.0–3.3 |
| Trouble Falling/Staying Asleep | 1 | 3.0 | 2.0–4.0 |
| Bruise, Bump, Cut | 2 | 3.0 | 2.0–4.0 |
| Headache | 3 | 3.0 | 2.3–3.5 |
| Neck Pain | 3 | 3.0 | 2.3–3.6 |
| Difficulty Concentrating | 4 | 3.7 | 3.0–4.0 |
| Feeling Sleepier | 4 | 4.0 | 3.0–4.0 |
| Vomiting | 4 | 4.0 | 3.0–4.0 |
| Sensitivity to Light/Noise | 4 | 4.0 | 3.0–4.0 |
| Feeling Dizzy | 4 | 4.0 | 3.0–4.0 |
| Blurred Vision | 4 | 4.0 | 4.0–4.0 |
| Loss of Consciousness | 4 | 4.0 | 4.0–4.0 |
| Variables Included in Each Model | aOR (Adjusted Odds Ratio) | 95% CI | p |
|---|---|---|---|
| Model: All symptoms | |||
| Higher Education | 0.90 | 0.42, 1.96 | 0.79 |
| Male Child | 2.10 | 0.51, 8.68 | 0.31 |
| Previous Treatment for Sprain/Broken Bone | 0.43 | 0.13, 1.38 | 0.16 |
| Child Liking Rough and Tumble Play | 1.48 | 0.71, 3.11 | 0.30 |
| Model: Higher Risk-Nonspecific Cognitive Symptoms | |||
| Higher Education | 0.92 | 0.47, 1.78 | 0.80 |
| Male Child | 1.46 | 0.38, 5.52 | 0.58 |
| Previous Treatment for Sprain/Broken Bone | 0.25 | 0.08, 0.77 | 0.02 * |
| Child Liking Rough and Tumble Play | 1.28 | 0.66, 2.48 | 0.46 |
| Model: Higher Risk-Nonspecific Physical Symptoms | |||
| Higher Education | 0.61 | 0.30, 1.25 | 0.18 |
| Male Child | 1.44 | 0.38, 5.40 | 0.59 |
| Previous Treatment for Sprain/Broken Bone | 0.16 | 0.05, 0.53 | 0.00* |
| Child Liking Rough and Tumble Play | 0.97 | 0.50, 1.88 | 0.94 |
| Model: Lower Risk-Cognitive Perceptual Symptoms | |||
| Higher Education | 0.40 | 0.07, 2.15 | 0.29 |
| Male Child | 0.19 | 0.01, 3.79 | 0.27 |
| Previous Treatment for Sprain/Broken Bone | 0.40 | 0.03, 4.97 | 0.48 |
| Child Liking Rough and Tumble Play | 2.18 | 0.49, 9.65 | 0.30 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goodman, E.; Boe, L.; Thye, M.; Mirman, J. Using Community Detection Analysis to Elucidate Caregivers’ Mental Models of Pediatric Concussion Symptoms. Safety 2018, 4, 35. https://doi.org/10.3390/safety4030035
Goodman E, Boe L, Thye M, Mirman J. Using Community Detection Analysis to Elucidate Caregivers’ Mental Models of Pediatric Concussion Symptoms. Safety. 2018; 4(3):35. https://doi.org/10.3390/safety4030035
Chicago/Turabian StyleGoodman, Emma, Logan Boe, Melissa Thye, and Jessica Mirman. 2018. "Using Community Detection Analysis to Elucidate Caregivers’ Mental Models of Pediatric Concussion Symptoms" Safety 4, no. 3: 35. https://doi.org/10.3390/safety4030035
APA StyleGoodman, E., Boe, L., Thye, M., & Mirman, J. (2018). Using Community Detection Analysis to Elucidate Caregivers’ Mental Models of Pediatric Concussion Symptoms. Safety, 4(3), 35. https://doi.org/10.3390/safety4030035





