Association by Age Groups Between Retrofitting Home Heating and Insulation and Subsequent Hospitalised Home Fall Rates: A Natural Experiment
Abstract
1. Introduction
2. Materials and Methods
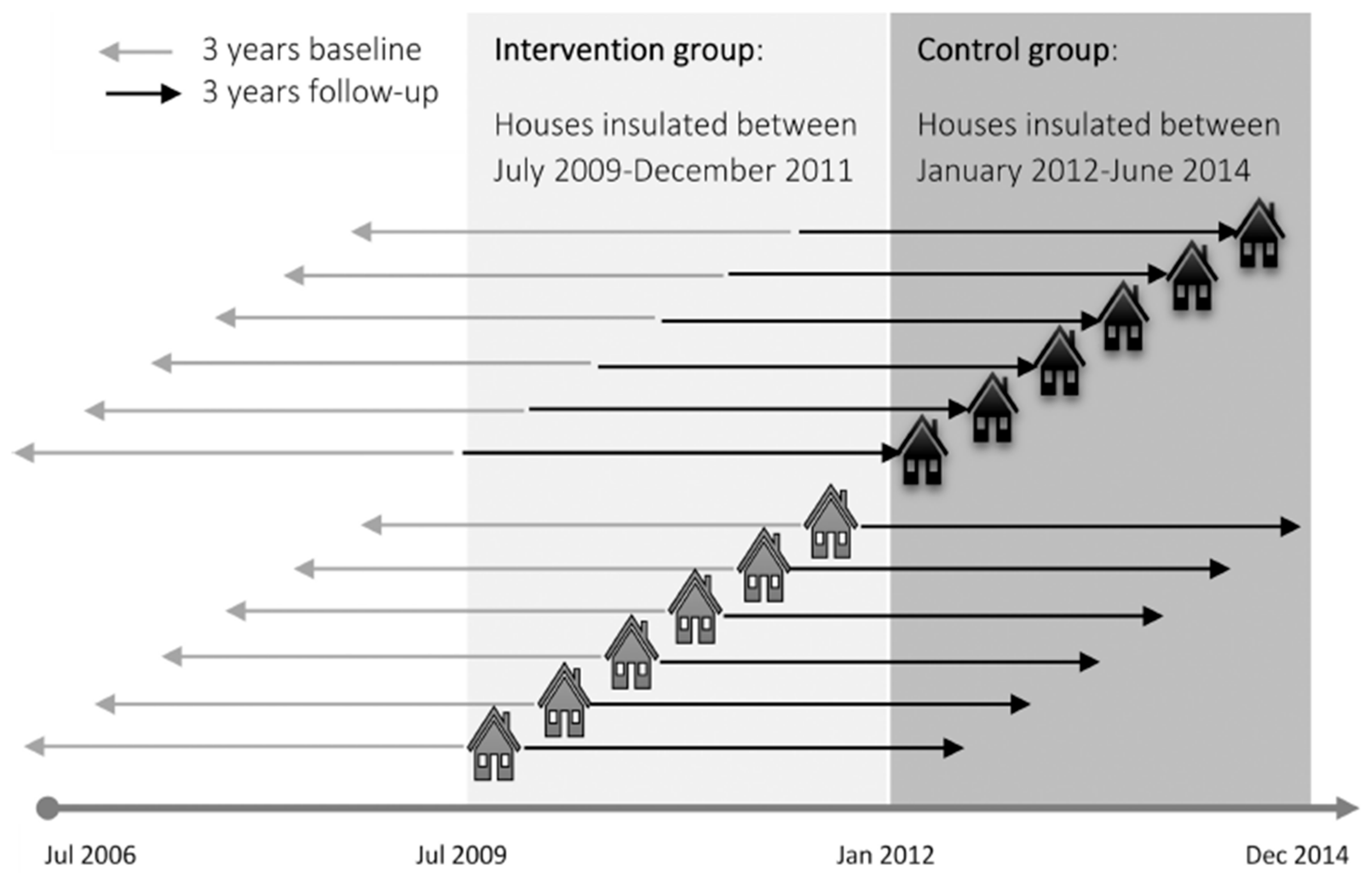
2.1. Study Design
2.2. Injury Outcomes and Duration of Exposure
2.3. Analysis
3. Results
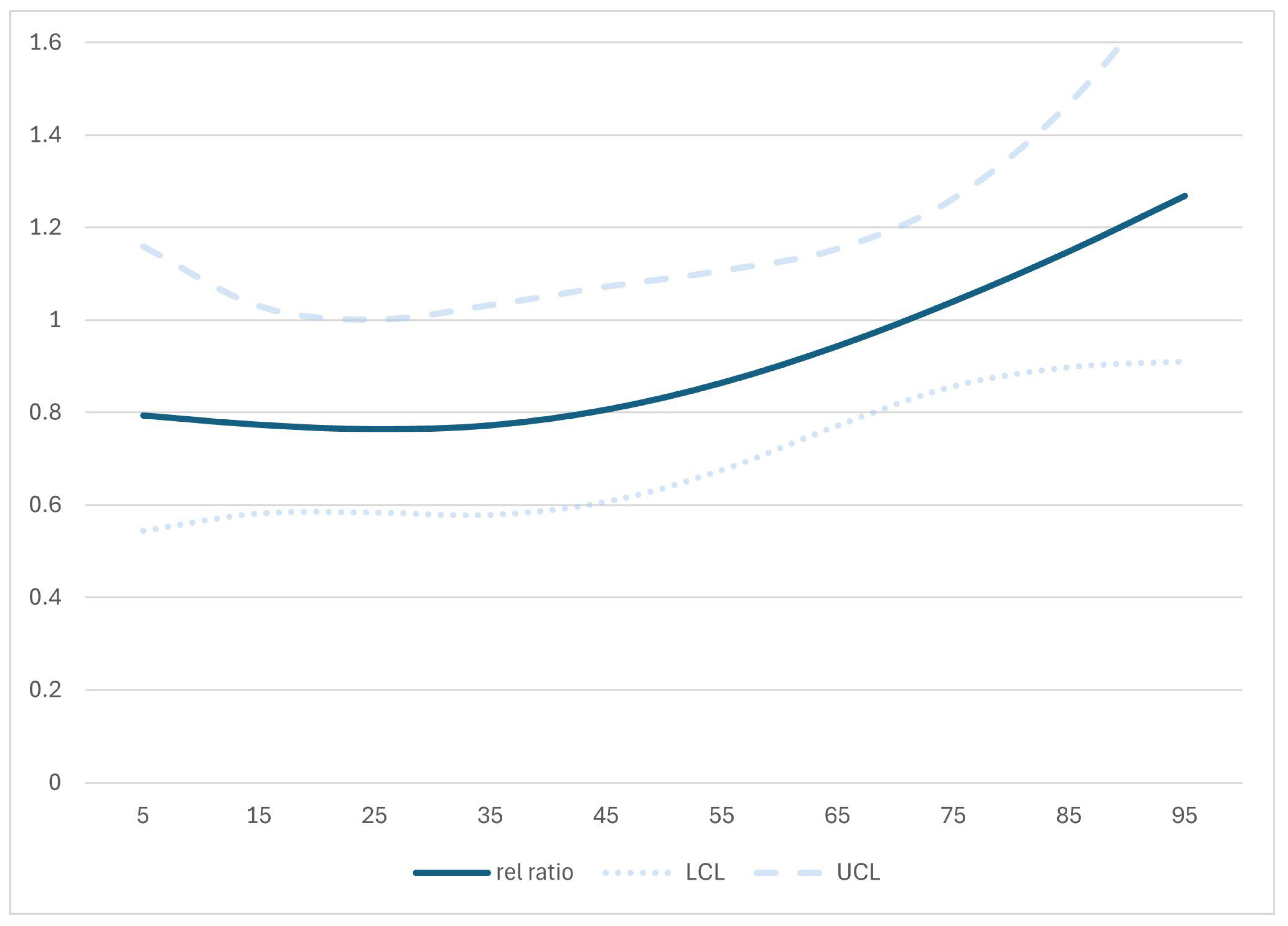
3.1. Crude Relative Rate Ratios
3.2. Adjusted Relative Rate Ratios
3.3. Sensitivity Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| EECA WUNZ | Energy Efficiency and Conservation Authority Warm Up New Zealand scheme |
| PHO | Primary Health Organisation |
| NHI | National Health Index number: a unique identifier assigned to everyone who uses health and disability support services |
| NZ | New Zealand |
References
- World Health Organization. WHO Housing and Health Guidelines; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Statistics New Zealand. Housing in Aotearoa: 2020; Statistics New Zealand: Auckland, New Zealand, 2020. [Google Scholar]
- New Zealand Government. Healthy Homes Guarantee Act 2017; New Zealand Government: Wellington, New Zealand, 2017. [Google Scholar]
- Fyfe, C.; Telfar-Barnard, L.; Howden-Chapman, P.; Douwes, J. Association between home insulation and hospital admission rates: Retrospective cohort study using linked data from a national intervention programme. BMJ 2020, 371, m4571. [Google Scholar] [CrossRef]
- Fyfe, C.; Barnard, L.T.; Douwes, J.; Howden-Chapman, P.; Crane, J. Retrofitting home insulation reduces incidence and severity of chronic respiratory disease. Indoor Air 2022, 32, e13101. [Google Scholar] [CrossRef] [PubMed]
- Howden-Chapman, P.; Matheson, A.; Crane, J.; Viggers, H.; Cunningham, M.; Blakely, T.; Woodward, A.; Saville-Smith, K.; O’Dea, D.; Kennedy, M.; et al. Effect of insulating existing houses on health inequality: Cluster randomised study in the community. Br. Med. J. 2007, 334, 460–464. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, K.C. Gee My Account Is in Credit! Qualitative Component of the Warm Homes Pilot Study. Unpublished Master’s Thesis. 2008. Available online: http://ourarchive.otago.ac.nz/handle/10523/367 (accessed on 15 April 2025).
- Sowden, S.; White, M. High-rise health: A qualitative study of the effect of social housing improvements on the health and wellbeing of residents in high-rise flats. Lancet 2014, 384, S76. [Google Scholar] [CrossRef]
- Thomson, H.; Thomas, S.; Sellstrom, E.; Petticrew, M. Housing improvements for health and associated socio-economic outcomes. Cochrane Database Syst. Rev. 2013, 28, CD008657. [Google Scholar] [CrossRef]
- Sawyer, A.; Sherriff, N.; Bishop, D.; Darking, M.; Huber, J.W. “It’s changed my life not to have the continual worry of being warm”—Health and wellbeing impacts of a local fuel poverty programme: A mixed-methods evaluation. BMC Public Health 2022, 22, 786. [Google Scholar] [CrossRef]
- Clemson, L.; Stark, S.; Pighills, A.C.; Fairhall, N.J.; Lamb, S.E.; Ali, J.; Sherrington, C. Environmental interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2023, 3, CD013258. [Google Scholar] [CrossRef]
- Keall, M.D.; Pierse, N.; Howden-Chapman, P.; Cunningham, C.; Cunningham, M.; Guria, J.; Baker, M.G. Home modifications to reduce injuries from falls in the home injury prevention intervention (HIPI) study: A cluster-randomised controlled trial. Lancet 2015, 385, 231–238. [Google Scholar] [CrossRef]
- Keall, M.D.; Tupara, H.; Pierse, N.; Wilkie, M.; Baker, M.G.; Howden-Chapman, P.; Cunningham, C. Home modifications to prevent home fall injuries in houses with Maori occupants (MHIPI): A randomised controlled trial. Lancet Public Health 2021, 6, e631–e640. [Google Scholar] [CrossRef]
- Turner, R.; Hayen, A.; Dunsmuir, W.; Finch, C.F. Air temperature and the incidence of fall-related hip fracture hospitalisations in older people. Osteoporos. Int. 2011, 22, 1183–1189. [Google Scholar] [CrossRef]
- Du Fay De Lavallaz, J.; Badertscher, P.; Nestelberger, T.; Flores, D.; Miró, Ò.; Salgado, E.; Geigy, N.; Christ, M.; Cullen, L.; Than, M. Circadian, weekly, seasonal, and temperature-dependent patterns of syncope aetiology in patients at increased risk of cardiac syncope. Ep Eur. 2019, 21, 511–521. [Google Scholar] [CrossRef]
- Nakagawa, H.; Niu, K.; Hozawa, A.; Ikeda, Y.; Kaiho, Y.; Ohmori-Matsuda, K.; Nakaya, N.; Kuriyama, S.; Ebihara, S.; Nagatomi, R. Impact of nocturia on bone fracture and mortality in older individuals: A Japanese longitudinal cohort study. J. Urol. 2010, 184, 1413–1418. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, N.; Boer, M.C.; De Santo, T.; Grovale, N.; Aerts, A.J.; Boersma, L.; Wieling, W. Daily, weekly, monthly, and seasonal patterns in the occurrence of vasovagal syncope in an older population. Europace 2007, 9, 823–828. [Google Scholar] [CrossRef] [PubMed]
- Wijlhuizen, G.J.; Chorus, A.M.; Hopman-Rock, M. The FARE: A new way to express FAlls Risk among older persons including physical activity as a measure of exposure. Prev. Med. 2010, 50, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Telfar Barnard, L.F.; Baker, M.G.; Hales, S.; Howden-Chapman, P. Novel use of three administrative datasets to establish a cohort for environmental health research. BMC Public Health 2015, 15, 246. [Google Scholar] [CrossRef]
- Langley, J.; Stephenson, S.; Cryer, C.; Borman, B. Traps for the unwary in estimating person based injury incidence using hospital discharge data. Inj. Prev. 2002, 8, 332–337. [Google Scholar] [CrossRef]
- Gauthier, J.; Wu, Q.V.; Gooley, T.A. Cubic splines to model relationships between continuous variables and outcomes: A guide for clinicians. Bone Marrow Transplant. 2020, 55, 675–680. [Google Scholar] [CrossRef]
- Gardner, W.; Mulvey, E.P.; Shaw, E.C. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol. Bull. 1995, 118, 392. [Google Scholar] [CrossRef]
- Salmond, C.; Crampton, P.; King, P.; Waldegrave, C. NZiDep: A New Zealand index of socioeconomic deprivation for individuals. Soc. Sci. Med. 2006, 62, 1474–1485. [Google Scholar]
- Isaacs, N. Thermal insulation. Build Mag. 2007, 110–111. [Google Scholar]
- Craig, P.; Cooper, C.; Gunnell, D.; Haw, S.; Lawson, K.; Macintyre, S.; Ogilvie, D.; Petticrew, M.; Reeves, B.; Sutton, M. Using natural experiments to evaluate population health interventions: New Medical Research Council guidance. J. Epidemiol. Community Health 2012, 66, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Geller, A.M.; Zenick, H. Aging and the environment: A research framework. Environ. Health Perspect. 2005, 113, 1257–1262. [Google Scholar] [CrossRef] [PubMed]
- Chapman, R.; Howden-Chapman, P.; Viggers, H.; O’Dea, D.; Kennedy, M. Retrofitting houses with insulation: A cost-benefit analysis of a randomised community trial. J. Epidemiol. Community Health 2009, 63, 271–277. [Google Scholar] [CrossRef]
- Mishra, S.R.; Wilson, T.; Andrabi, H.; Ait Ouakrim, D.; Li, A.; Akpan, E.; Bentley, R.; Blakely, T. The total health gains and cost savings of eradicating cold housing in Australia. Soc. Sci. Med. 2023, 334, 115954. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Value | Intervention n (%) | Control n (%) | Intervention Falls Baseline/Follow-Up | Control Falls Baseline/Follow-Up | Relative Rate Ratio (95% CI) |
|---|---|---|---|---|---|---|
| Overall | 236,040 (100) | 233,626 (100) | 1288/2535 | 1075/2115 | 0.99 (0.89, 1.09) | |
| Sex | Female | 126,453 (53.6) | 123,682 (52.9) | 870/1638 | 709/1422 | 0.92 (0.82, 1.04) |
| Male | 109,587 (46.4) | 109,944 (47.1) | 418/897 | 366/693 | 1.12 (0.94, 1.33) | |
| Age at start of study | 0–9 | 41,608 (17.6) | 39,303 (16.8) | 120/99 | 101/93 | 0.83 (0.57, 1.23) |
| 10–19 | 30,721 (13.0) | 33,771 (14.5) | 36/45 | 31/47 | 0.79 (0.42, 1.48) | |
| 20–29 | 27,758 (11.8) | 30,118 (12.9) | 38/34 | 43/53 | 0.77 (0.42, 1.43) | |
| 30–39 | 33,778 (14.3) | 32,141 (13.8) | 58/49 | 43/49 | 0.71 (0.41, 1.24) | |
| 40–49 | 31,176 (13.2) | 31,848 (13.6) | 70/79 | 51/77 | 0.71 (0.44, 1.15) | |
| 50–59 | 24,667 (10.5) | 25,998 (11.1) | 97/136 | 99/135 | 1.04 (0.72, 1.50) | |
| 60–69 | 23,914 (10.1) | 22,223 (9.5) | 177/260 | 119/210 | 0.88 (0.66, 1.18) | |
| 70–79 | 16,404 (6.9) | 13,266 (5.7) | 298/629 | 256/493 | 1.12 (0.92, 1.38) | |
| 80–89 | 5683 (2.4) | 4677 (2.0) | 344/932 | 295/756 | 1.04 (0.87, 1.25) | |
| 90 plus | 331 (0.1) | 281 (0.1) | 50/272 | 37/202 | 0.87 (0.55, 1.37) | |
| Age dichotomised | 0–64 | 200,152 (84.8) | 203,927 (87.3) | 494/529 | 407/528 | 0.81 * (0.68, 0.97) |
| 65 plus | 35,888 (15.2) | 29,699 (12.7) | 794/2006 | 668/1587 | 1.10 (0.97, 1.24) | |
| Ethnicity | European | 159,261 (67.5) | 147,956 (63.3) | 1052/2214 | 876/1779 | 1.01 (0.91, 1.13) |
| Māori | 36,698 (15.5) | 42,675 (18.3) | 134/185 | 109/189 | 0.79 (0.57, 1.09) | |
| Other | 40,081 (17.0) | 42,995 (18.4) | 102/136 | 90/147 | 0.82 (0.57, 1.18) | |
| Deprivation (NZDep) quintile | 1 least deprived | 35,632 (15.1) | 31,911 (13.7) | 180/345 | 148/278 | 1.00 (0.76, 1.31) |
| 2 | 42,570 (18.0) | 37,748 (16.2) | 187/422 | 164/312 | 1.18 (0.91, 1.52) | |
| 3 | 48,633 (20.6) | 45,328 (19.4) | 267/510 | 217/401 | 1.02 (0.82, 1.27) | |
| 4 | 55,909 (23.7) | 55,358 (23.7) | 347/643 | 271/556 | 0.89 (0.73, 1.08) | |
| 5 most deprived | 53,296 (22.6) | 63,281 (27.1) | 307/615 | 275/568 | 0.95 (0.78, 1.16) | |
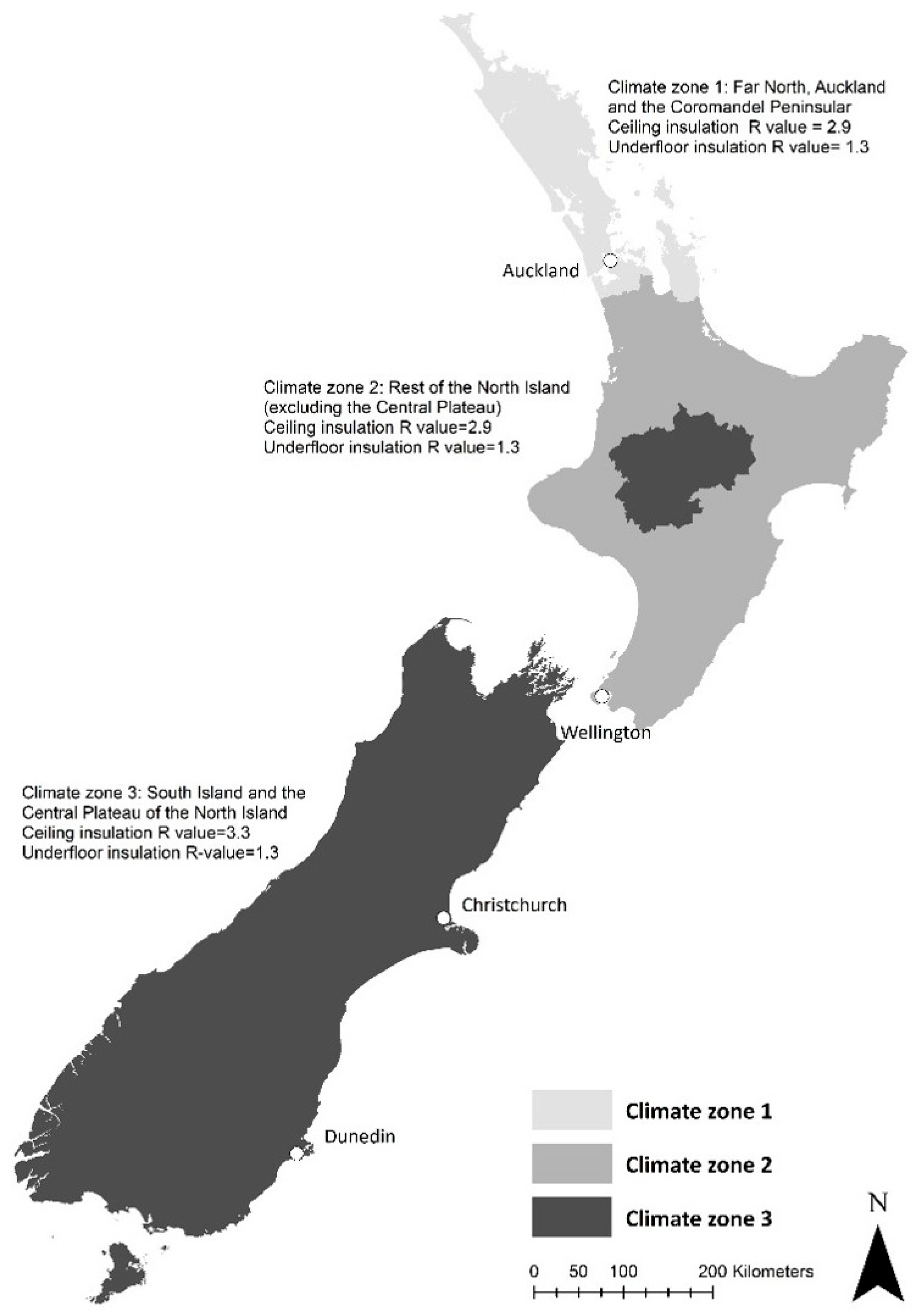
| Climate zone (see Figure 2) | CZ1: Far North, Auckland and Coromandel Peninsula) | 64,335 (27.3) | 71,336 (30.5) | 384/700 | 332/615 | 0.97 (0.80, 1.16) |
| CZ2: rest of North Island (excluding Central Plateau) | 114,293 (48.4) | 121,470 (52.0) | 594/1113 | 524/1046 | 0.93 (0.80, 1.07) | |
| CZ3: South Island and Central Plateau | 57,412 (24.3) | 40,820 (17.5) | 310/722 | 219/454 | 1.10 (0.89, 1.36) |
| Factor | Factor Level | Adjusted Relative Rate (95% CI) | p-Value |
|---|---|---|---|
| age dichotomised | 0–64 | 0.12 (0.11, 0.14) | <0.0001 |
| 65+ | reference | ||
| ethnicity | European | 2.23 (1.97, 2.52) | <0.0001 |
| Māori | 1.74 (1.49, 2.02) | <0.0001 | |
| Other | reference | ||
| sex | F | 1.57 (1.47, 1.68) | <0.0001 |
| M | reference | ||
| deprivation quintile | 1 least deprived | 0.72 (0.65, 0.81) | <0.0001 |
| 2 | 0.71 (0.64, 0.79) | <0.0001 | |
| 3 | 0.80 (0.73, 0.89) | <0.0001 | |
| 4 | 0.90 (0.82, 0.98) | 0.02 | |
| 5 most deprived | reference | ||
| climate zone | CZ1: Far North, Auckland and Coromandel Peninsula) | 1.39 (1.29, 1.50) | <0.0001 |
| CZ2: rest of North Island (excluding Central Plateau) | reference | ||
| CZ3: South Island and Central Plateau | 1.10 (1.01, 1.19) | 0.03 | |
| cohort | Intervention | 0.96 (0.83, 1.10) | 0.54 |
| Control | reference | ||
| period | Follow-up | 1.96 (1.74, 2.21) | <0.0001 |
| Baseline | reference | ||
| cohort × period | Intervention, follow-up | 1.09 (0.93, 1.28) | 0.29 |
| cohort × age | Intervention, age 0–64 | 1.25 (1.02, 1.52) | 0.03 |
| period × age | Follow-up, age 0–64 | 0.65 (0.54, 0.78) | <0.0001 |
| cohort × period × age | Intervention, follow-up, age 0–64 | 0.74 (0.58, 0.96) | 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keall, M.D.; Fyfe, C.; Howden-Chapman, P.; Pierse, N. Association by Age Groups Between Retrofitting Home Heating and Insulation and Subsequent Hospitalised Home Fall Rates: A Natural Experiment. Safety 2025, 11, 81. https://doi.org/10.3390/safety11030081
Keall MD, Fyfe C, Howden-Chapman P, Pierse N. Association by Age Groups Between Retrofitting Home Heating and Insulation and Subsequent Hospitalised Home Fall Rates: A Natural Experiment. Safety. 2025; 11(3):81. https://doi.org/10.3390/safety11030081
Chicago/Turabian StyleKeall, Michael D., Caroline Fyfe, Philippa Howden-Chapman, and Nevil Pierse. 2025. "Association by Age Groups Between Retrofitting Home Heating and Insulation and Subsequent Hospitalised Home Fall Rates: A Natural Experiment" Safety 11, no. 3: 81. https://doi.org/10.3390/safety11030081
APA StyleKeall, M. D., Fyfe, C., Howden-Chapman, P., & Pierse, N. (2025). Association by Age Groups Between Retrofitting Home Heating and Insulation and Subsequent Hospitalised Home Fall Rates: A Natural Experiment. Safety, 11(3), 81. https://doi.org/10.3390/safety11030081






