Detection Rate and Variability in Measurement of Mandibular Incisive Canal on Cone-Beam Computed Tomography: A Study of 220 Dentate Hemi-Mandibles from Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient and Hemi-Mandible Selection
2.2. Image Acquisition
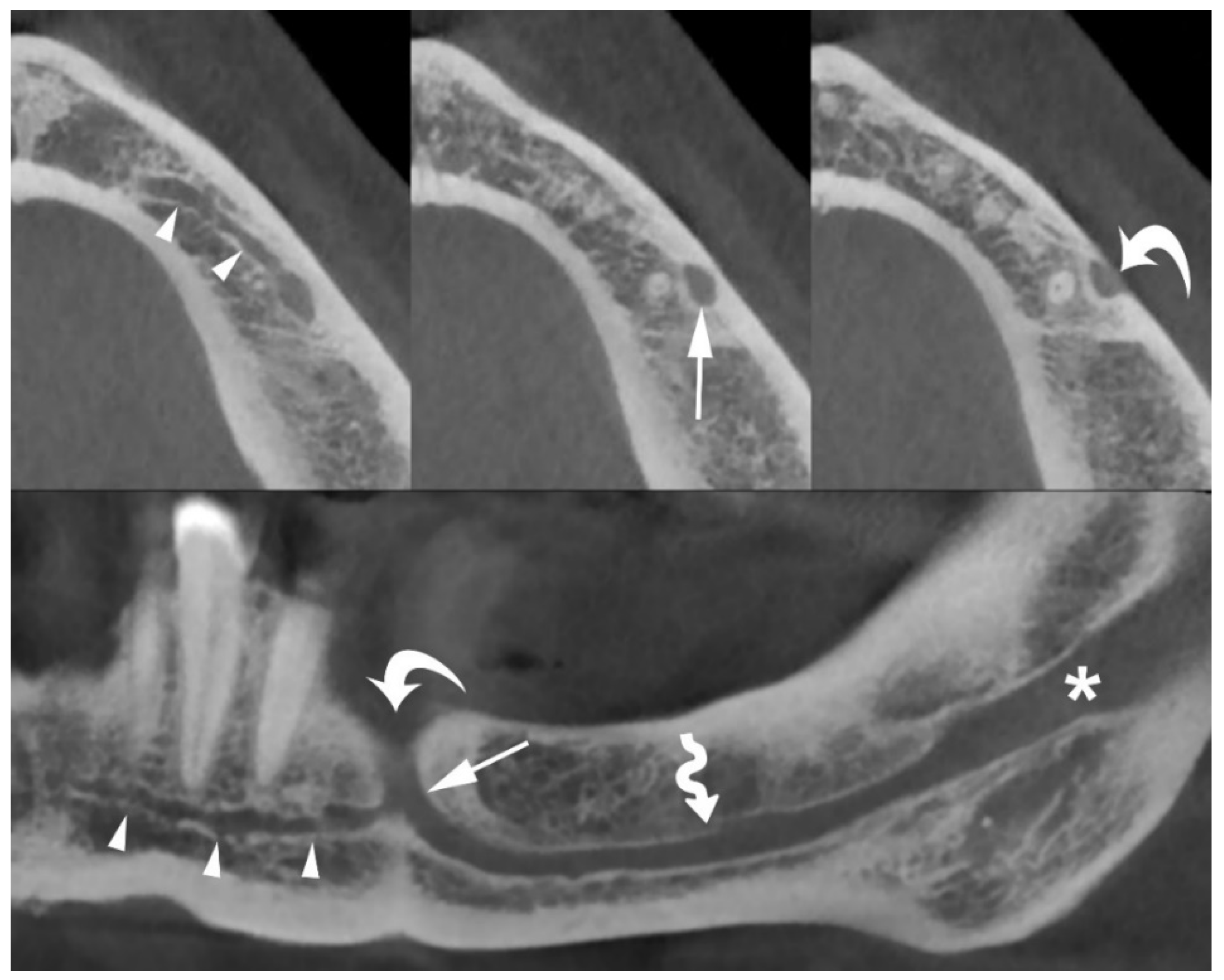
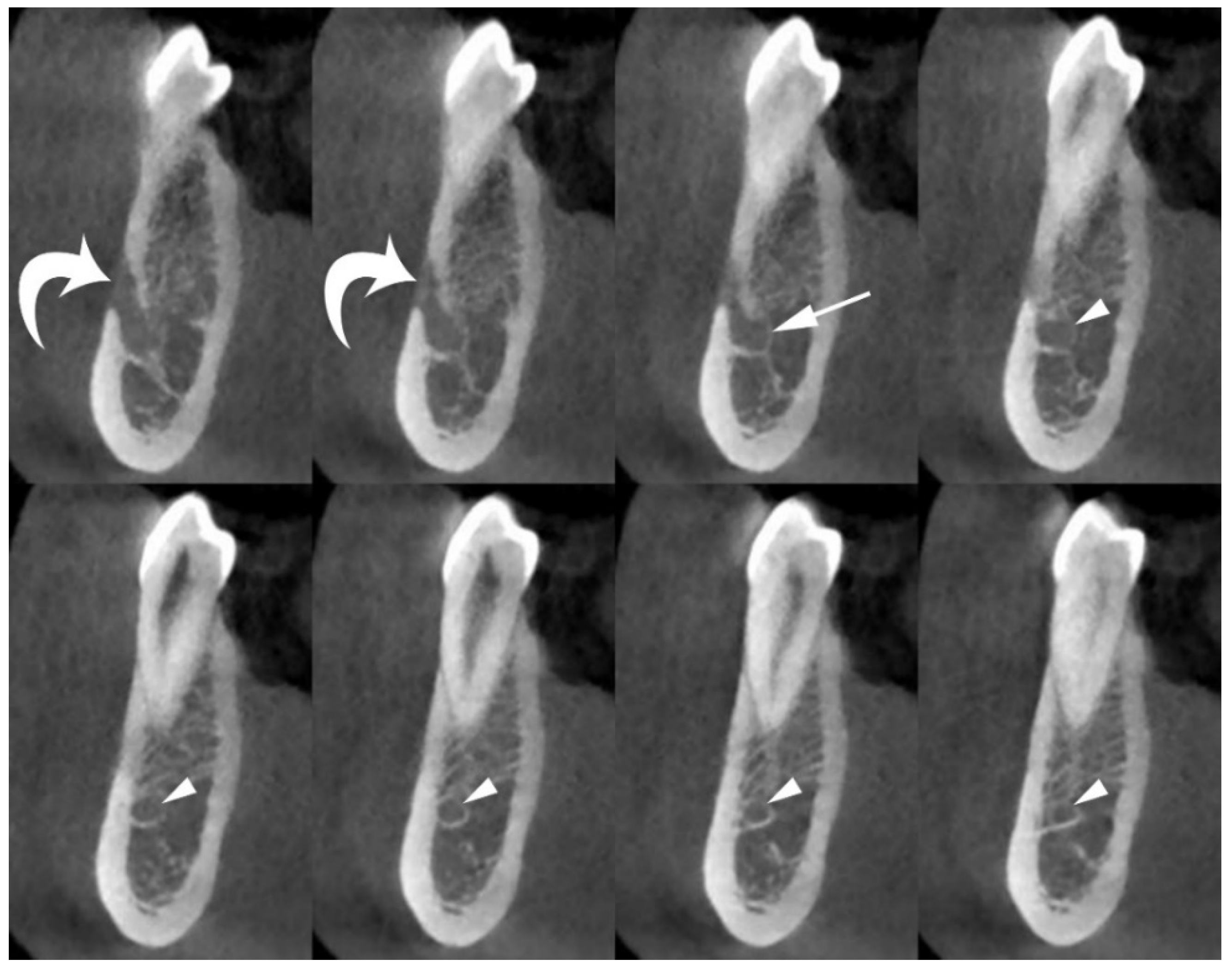
2.3. Image Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Al-Ani, O.; Nambiar, P.; Ha, K.O.; Ngeow, W.C. Safe zone for bone harvesting from the interforaminal region of the mandible. Clin. Oral. Implant. Res. 2013, 24 (Suppl. A100), 115–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Juodzbalys, G.; Wang, H.L.; Sabalys, G. Anatomy of Mandibular Vital Structures. Part II: Mandibular Incisive Canal, Mental Foramen and Associated Neurovascular Bundles in Relation with Dental Implantology. J. Oral. Maxillofac. Res. 2010, 1, e3. [Google Scholar] [CrossRef]
- Pires, C.A.; Bissada, N.F.; Becker, J.J.; Kanawati, A.; Landers, M.A. Mandibular incisive canal: Cone beam computed tomography. Clin. Implant. Dent. Relat. Res. 2012, 14, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Sener, E.; Onem, E.; Akar, G.C.; Govsa, F.; Ozer, M.A.; Pinar, Y.; Mert, A.; Baksi Sen, B.G. Anatomical landmarks of mandibular interforaminal region related to dental implant placement with 3D CBCT: Comparison between edentulous and dental mandibles. Surg. Radiol. Anat. 2018, 40, 615–623. [Google Scholar] [CrossRef]
- Caughey, J.A.; Do, Q.; Shen, D.; Ohyama, H.; He, P.; Tubbs, R.S.; Iwanaga, J. Comprehensive review of the incisive branch of the inferior alveolar nerve. Anat. Cell Biol. 2021, 54, 409–416. [Google Scholar] [CrossRef]
- Kqiku, L.; Weiglein, A.H.; Pertl, C.; Biblekaj, R.; Städtler, P. Histology and intramandibular course of the inferior alveolar nerve. Clin. Oral. Investig. 2011, 15, 1013–1016. [Google Scholar] [CrossRef]
- Rodella, L.F.; Buffoli, B.; Labanca, M.; Rezzani, R. A review of the mandibular and maxillary nerve supplies and their clinical relevance. Arch. Oral. Biol. 2012, 57, 323–334. [Google Scholar] [CrossRef] [PubMed]
- do Carmo Oliveira, M.; Tedesco, T.K.; Gimenez, T.; Allegrini, S., Jr. Analysis of the frequency of visualization of morphological variations in anatomical bone features in the mandibular interforaminal region through cone-beam computed tomography. Surg. Radiol. Anat. 2018, 40, 1119–1131. [Google Scholar] [CrossRef]
- Mraiwa, N.; Jacobs, R.; van Steenberghe, D.; Quirynen, M. Clinical assessment and surgical implications of anatomic challenges in the anterior mandible. Clin. Implant. Dent. Relat. Res. 2003, 5, 219–225. [Google Scholar] [CrossRef]
- Parnia, F.; Moslehifard, E.; Hafezeqoran, A.; Mahboub, F.; Mojaver-Kahnamoui, H. Characteristics of anatomical landmarks in the mandibular interforaminal region: A cone-beam computed tomography study. Med. Oral. Patol. Oral. Cir. Bucal. 2012, 17, e420–e425. [Google Scholar] [CrossRef] [Green Version]
- Kütük, N.; Demirbaş, A.E.; Gönen, Z.B.; Topan, C.; Kiliç, E.; Etöz, O.A.; Alkan, A. Anterior mandibular zone safe for implants. J. Craniofac. Surg. 2013, 24, e405–e408. [Google Scholar] [CrossRef]
- Lee, C.Y.; Yanagihara, L.C.; Suzuki, J.B. Brisk, pulsatile bleeding from the anterior mandibular incisive canal during implant surgery: A case report and use of an active hemostatic matrix to terminate acute bleeding. Implant. Dent. 2012, 21, 368–373. [Google Scholar] [CrossRef]
- Uchida, Y.; Noguchi, N.; Goto, M.; Yamashita, Y.; Hanihara, T.; Takamori, H.; Sato, I.; Kawai, T.; Yosue, T. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: A second attempt introducing cone beam computed tomography. J. Oral. Maxillofac. Surg. 2009, 67, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.W.; Zhang, F.F.; Li, Y.H.; Wei, B.; Gong, Y. Characteristics of intrabony nerve canals in mandibular interforaminal region by using cone-beam computed tomography and a recommendation of safe zone for implant and bone harvesting. Clin. Implant. Dent. Relat. Res. 2017, 19, 530–538. [Google Scholar] [CrossRef]
- Kabak, S.L.; Zhuravleva, N.V.; Melnichenko, Y.M.; Savrasova, N.A. Study of the mandibular incisive canal anatomy using cone beam computed tomography. Surg. Radiol. Anat. 2017, 39, 647–655. [Google Scholar] [CrossRef]
- Gomes, L.T.; de Almeida Barros Mourão, C.F.; Braga, C.L.; de Almeida, L.F.D.; de Mello-Machado, R.C.; Calasans-Maia, M.D. Anatomic evaluation of the incisive canal with cone beam computed tomography and its relevance to surgical procedures in the mental region: A retrospective study in a Brazilian population. Oral. Maxillofac. Surg. 2018, 22, 379–384. [Google Scholar] [CrossRef]
- Gilis, S.; Dhaene, B.; Dequanter, D.; Loeb, I. Mandibular incisive canal and lingual foramina characterization by cone-beam computed tomography. Morphologie 2019, 103, 48–53. [Google Scholar] [CrossRef]
- Lim, J.T.S.; Kang, W.J.; Ajit Bapat, R.; Kanneppady, S.K.; Pandurangappa, R. Evaluation of Mandibular Incisive Canal using Cone Beam Computed Tomography in Malaysians. J. Maxillofac. Oral. Surg. 2019, 18, 596–603. [Google Scholar] [CrossRef]
- Zhang, Y.Q.; Yan, X.B.; Zhang, L.Q.; Xie, X.Y.; Liu, D.G.; Zhang, Z.Y. Prevalence and Morphology of Mandibular Incisive Canal: Comparison among Healthy, Periodontitis and Edentulous Mandibles in a Population of the Beijing Area Using Cone-beam Computed Tomography. Chin. J. Dent. Res. 2019, 22, 241–249. [Google Scholar] [CrossRef]
- Ayesha, R.T.; Pachipulusu, B.; Govindaraju, P. Assessment of prevalence and position of mandibular incisive canal: A cone beam computed tomography study. Ci Ji Yi Xue Za Zhi 2019, 32, 205–210. [Google Scholar] [CrossRef]
- Puri, A.; Verma, P.; Mahajan, P.; Bansal, A.; Kohli, S.; Faraz, S.A. CBCT Evaluation of the Vital Mandibular Interforaminal Anatomical Structures. Ann. Maxillofac. Surg. 2020, 10, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, D.A.; Kurita, L.M.; Pimenta, A.V.; Teixeira, R.C.; Silva, P.G.; Ribeiro, T.R.; Melo, D.P.; Costa, F.W. Mandibular incisive canal-related prevalence, morphometric parameters, and implant placement implications: A multicenter study of 847 CBCT scans. Med. Oral. Patol. Oral. Cir. Bucal. 2020, 25, e337–e345. [Google Scholar] [CrossRef]
- Alshamrani, A.S.; Tokhtah, R.A.; Al-Omar, A. Cone-beam computed tomography evaluation of prevalence and location of mandibular incisive canal in patients attending King Saud University Dental Hospital. J. Orthod. Sci. 2021, 10, 21. [Google Scholar] [CrossRef]
- Jacobs, R.; Mraiwa, N.; vanSteenberghe, D.; Gijbels, F.; Quirynen, M. Appearance, location, course, and morphology of the mandibular incisive canal: An assessment on spiral CT scan. Dentomaxillofac. Radiol. 2002, 31, 322–327. [Google Scholar] [CrossRef]
- Idiyatullin, D.; Corum, C.; Moeller, S.; Prasad, H.S.; Garwood, M.; Nixdorf, D.R. Dental magnetic resonance imaging: Making the invisible visible. J. Endod. 2011, 37, 745–752. [Google Scholar] [CrossRef] [Green Version]
- Krasny, A.; Krasny, N.; Prescher, A. Study of inferior dental canal and its contents using high-resolution magnetic resonance imaging. Surg. Radiol. Anat. 2012, 34, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Reda, R.; Zanza, A.; Cicconetti, A.; Bhandi, S.; Miccoli, G.; Gambarini, G.; Di Nardo, D. Ultrasound Imaging in Dentistry: A Literature Overview. J. Imaging 2021, 7, 238. [Google Scholar] [CrossRef] [PubMed]
- Borghesi, A.; Pezzotti, S.; Nocivelli, G.; Maroldi, R. Five mental foramina in the same mandible: CBCT findings of an unusual anatomical variant. Surg. Radiol. Anat. 2018, 40, 635–640. [Google Scholar] [CrossRef]
- Borghesi, A.; Bondioni, M.P. Unilateral triple mandibular canal with double mandibular foramen: Cone-beam computed tomography findings of an unexpected anatomical variant. Folia Morphol. 2021, 80, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.J.; Zhong, W.H.; Liu, Y.X.; Miao, H.Z.; Li, Y.C.; Ji, M.H. Sample Size for Assessing Agreement between Two Methods of Measurement by Bland-Altman Method. Int. J. Biostat. 2016, 12. [Google Scholar] [CrossRef] [Green Version]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Patcas, R.; Müller, L.; Ullrich, O.; Peltomäki, T. Accuracy of cone-beam computed tomography at different resolutions assessed on the bony covering of the mandibular anterior teeth. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Ruetters, M.; Kim, T.S.; Hagenfeld, D.; Kronsteiner, D.; Gehrig, H.; Lux, C.J.; Sen, S. Ex vivo assessment of the buccal and oral bone by CBCT. J. Orofac. Orthop. 2021; Online ahead of print. [Google Scholar] [CrossRef]

| Site | MIC Detection Rate (%) | p Value * | ||
|---|---|---|---|---|
| Man | Woman | Total | ||
| First premolar | 55/70 (78.6) | 126/150 (84.0) | 181/220 (82.3) | 0.327 |
| Canine | 43/70 (61.4) | 83/150 (55.3) | 126/220 (57.3) | 0.396 |
| Lateral incisor | 11/70 (15.7) | 28/150 (18.7) | 39/220 (17.7) | 0.594 |
| Central incisor | 0/70 (0.0) | 1/150 (0.7) | 1/220 (0.5) | NA |
| Site | MIC Diameter (mm) | p Value * | ||
|---|---|---|---|---|
| Man | Woman | Total | ||
| First premolar | 1.68 (1.33–1.97) | 1.54 (1.29–1.84) | 1.63 (1.33–1.92) | 0.213 |
| Canine | 1.22 (1.00–1.34) | 1.23 (1.01–1.40) | 1.22 (1.01–1.40) | 0.425 |
| Lateral incisor | 1.00 (0.96–1.22) | 0.92 (0.83–1.26) | 1.00 (0.83–1.22) | 0.387 |
| Central incisor | - | 1.22 | 1.22 | NA |
| Site | Round of Measurement (mm) | Mean (mm) | CR (mm) | |
|---|---|---|---|---|
| First | Second | |||
| First premolar | 1.63 (1.33–1.92) | 1.54 (1.31–1.84) | 0.05 | 0.27 |
| Canine | 1.22 (1.01–1.40) | 1.20 (1.00–1.38) | 0.03 | 0.24 |
| Lateral incisor | 1.00 (0.83–1.22) | 1.00 (0.80–1.20) | 0.03 | 0.21 |
| Central incisor | 1.22 | 1.25 | NA | NA |
| Site | Round of Measurement (mm) | Mean (mm) | CR (mm) | |
|---|---|---|---|---|
| First | Second | |||
| First premolar | 5.85 ± 2.58 | 5.89 ± 2.55 | −0.02 | 0.74 |
| Canine | 6.58 ± 3.00 | 6.62 ± 3.01 | −0.04 | 0.63 |
| Lateral incisor | 8.02 ± 3.41 | 8.06 ± 3.39 | −0.04 | 0.73 |
| Central incisor | 11.95 | 11.84 | NA | NA |
| Site | Round of Measurement (mm) | Mean (mm) | CR (mm) | |
|---|---|---|---|---|
| First | Second | |||
| First premolar | 8.68 ± 1.62 | 8.67 ± 1.62 | 0.02 | 0.60 |
| Canine | 6.79 ± 1.68 | 6.77 ± 1.69 | 0.02 | 0.45 |
| Lateral incisor | 6.67 ± 1.53 | 6.65 ± 1.53 | 0.01 | 0.48 |
| Central incisor | 6.32 | 6.38 | NA | NA |
| Site | Round of Measurement (mm) | Mean (mm) | CR (mm) | |
|---|---|---|---|---|
| First | Second | |||
| First premolar | 3.12 ± 1.21 | 3.11 ± 1.23 | 0.02 | 0.65 |
| Canine | 4.90 ± 1.63 | 4.87 ± 1.64 | 0.03 | 0.45 |
| Lateral incisor | 5.23 ± 1.44 | 5.19 ± 1.47 | 0.04 | 0.52 |
| Central incisor | 4.06 | 4.02 | NA | NA |
| Site | Round of Measurement (mm) | Mean (mm) | CR (mm) | |
|---|---|---|---|---|
| First | Second | |||
| First premolar | 5.30 ± 1.72 | 5.29 ± 1.71 | 0.01 | 0.67 |
| Canine | 4.72 ± 1.86 | 4.68 ± 1.84 | 0.04 | 0.51 |
| Lateral incisor | 5.07 ± 1.60 | 5.02 ± 1.63 | 0.05 | 0.48 |
| Central incisor | 5.61 | 5.67 | NA | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borghesi, A.; Di Salvo, D.; Ciolli, P.; Falcone, T.; Ravanelli, M.; Farina, D.; Carapella, N. Detection Rate and Variability in Measurement of Mandibular Incisive Canal on Cone-Beam Computed Tomography: A Study of 220 Dentate Hemi-Mandibles from Italy. J. Imaging 2022, 8, 161. https://doi.org/10.3390/jimaging8060161
Borghesi A, Di Salvo D, Ciolli P, Falcone T, Ravanelli M, Farina D, Carapella N. Detection Rate and Variability in Measurement of Mandibular Incisive Canal on Cone-Beam Computed Tomography: A Study of 220 Dentate Hemi-Mandibles from Italy. Journal of Imaging. 2022; 8(6):161. https://doi.org/10.3390/jimaging8060161
Chicago/Turabian StyleBorghesi, Andrea, Diego Di Salvo, Pietro Ciolli, Teresa Falcone, Marco Ravanelli, Davide Farina, and Nicola Carapella. 2022. "Detection Rate and Variability in Measurement of Mandibular Incisive Canal on Cone-Beam Computed Tomography: A Study of 220 Dentate Hemi-Mandibles from Italy" Journal of Imaging 8, no. 6: 161. https://doi.org/10.3390/jimaging8060161
APA StyleBorghesi, A., Di Salvo, D., Ciolli, P., Falcone, T., Ravanelli, M., Farina, D., & Carapella, N. (2022). Detection Rate and Variability in Measurement of Mandibular Incisive Canal on Cone-Beam Computed Tomography: A Study of 220 Dentate Hemi-Mandibles from Italy. Journal of Imaging, 8(6), 161. https://doi.org/10.3390/jimaging8060161






