Iodine-123 β-methyl-P-iodophenyl-pentadecanoic Acid (123I-BMIPP) Myocardial Scintigraphy for Breast Cancer Patients and Possible Early Signs of Cancer-Therapeutics-Related Cardiac Dysfunction (CTRCD)
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Patients
3.2. UCG Evaluation
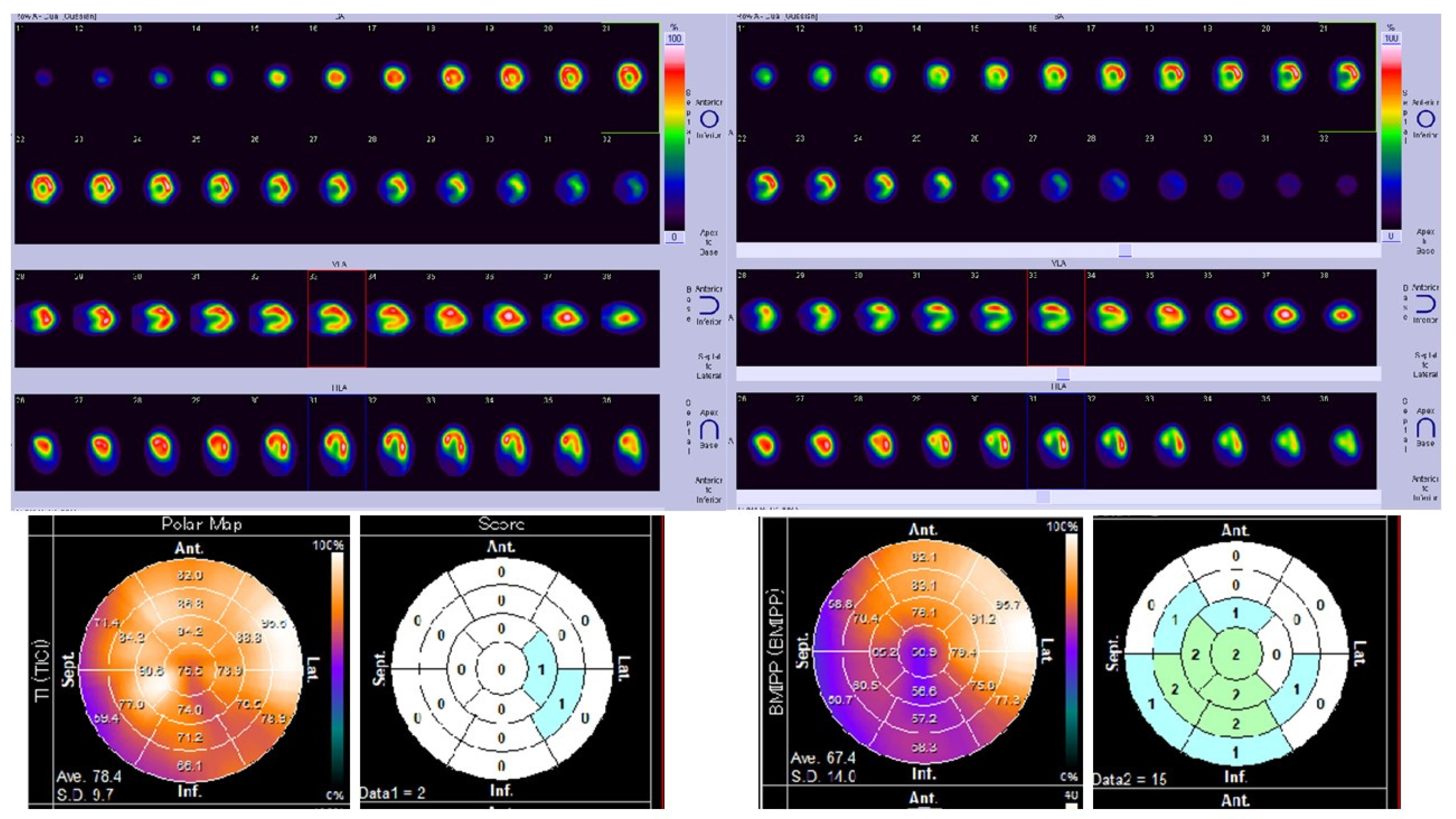
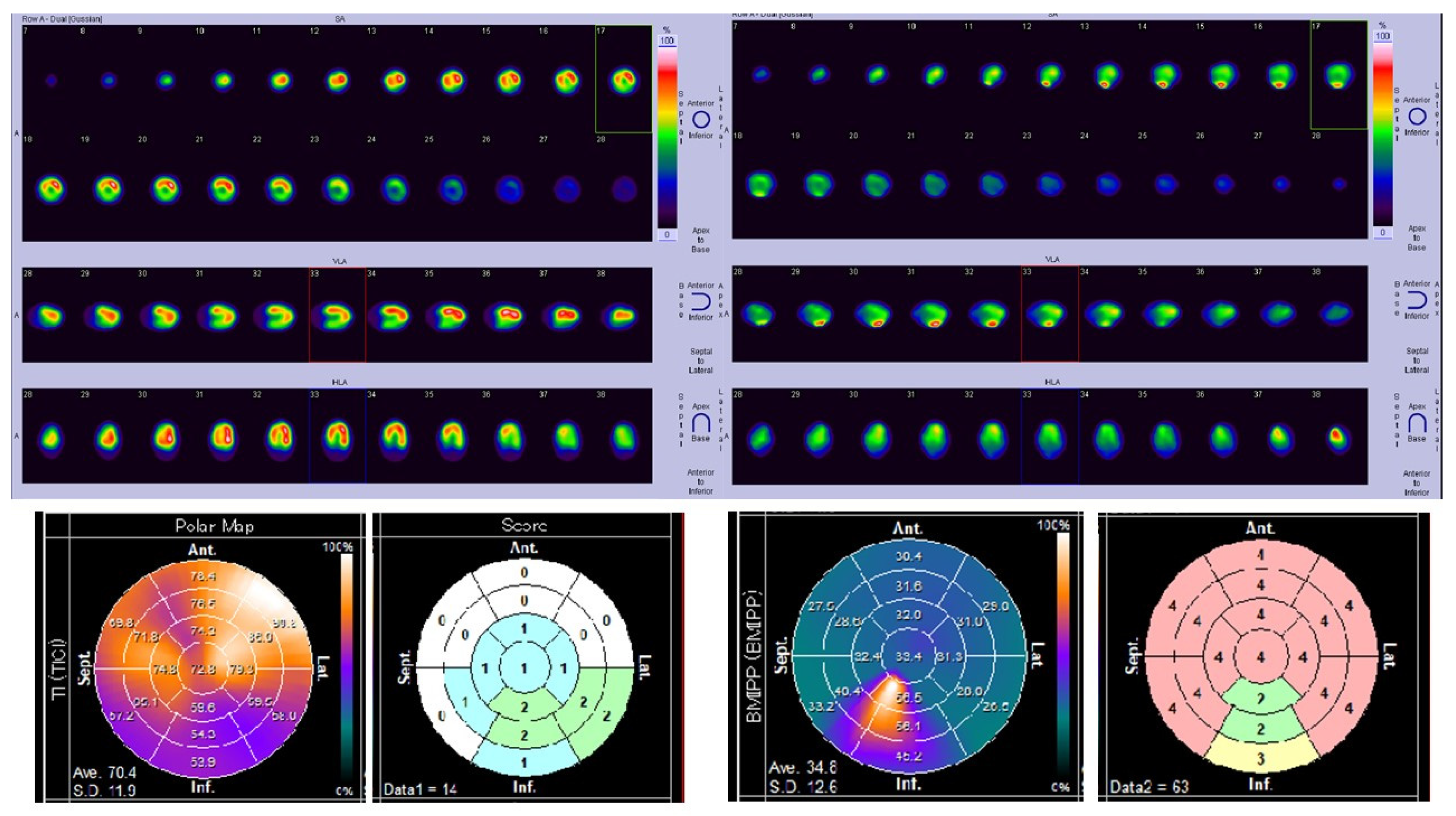
3.3. Myocardial Scintigraphy
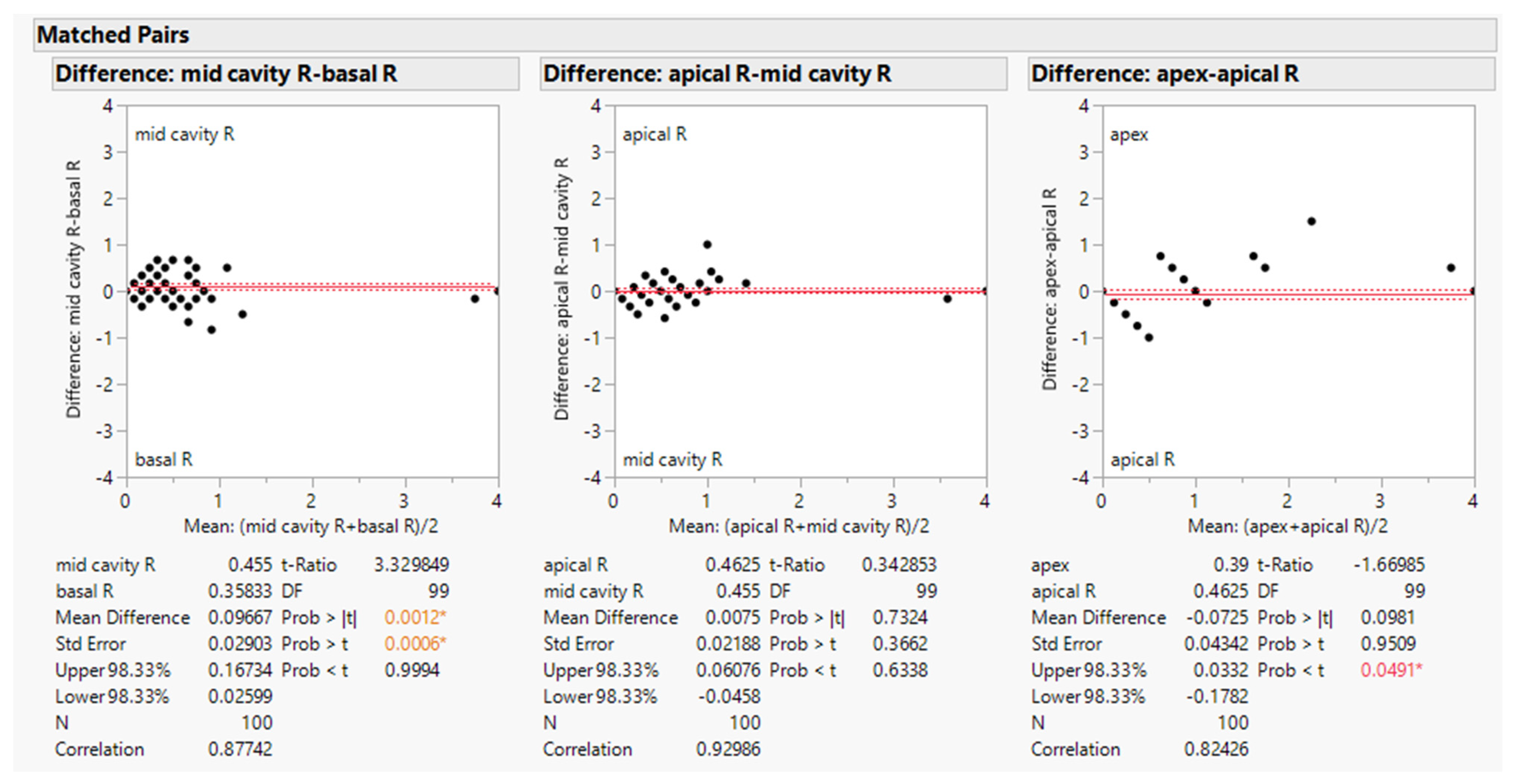
3.4. Mathematical Analysis of Myocardial Scintigraphy
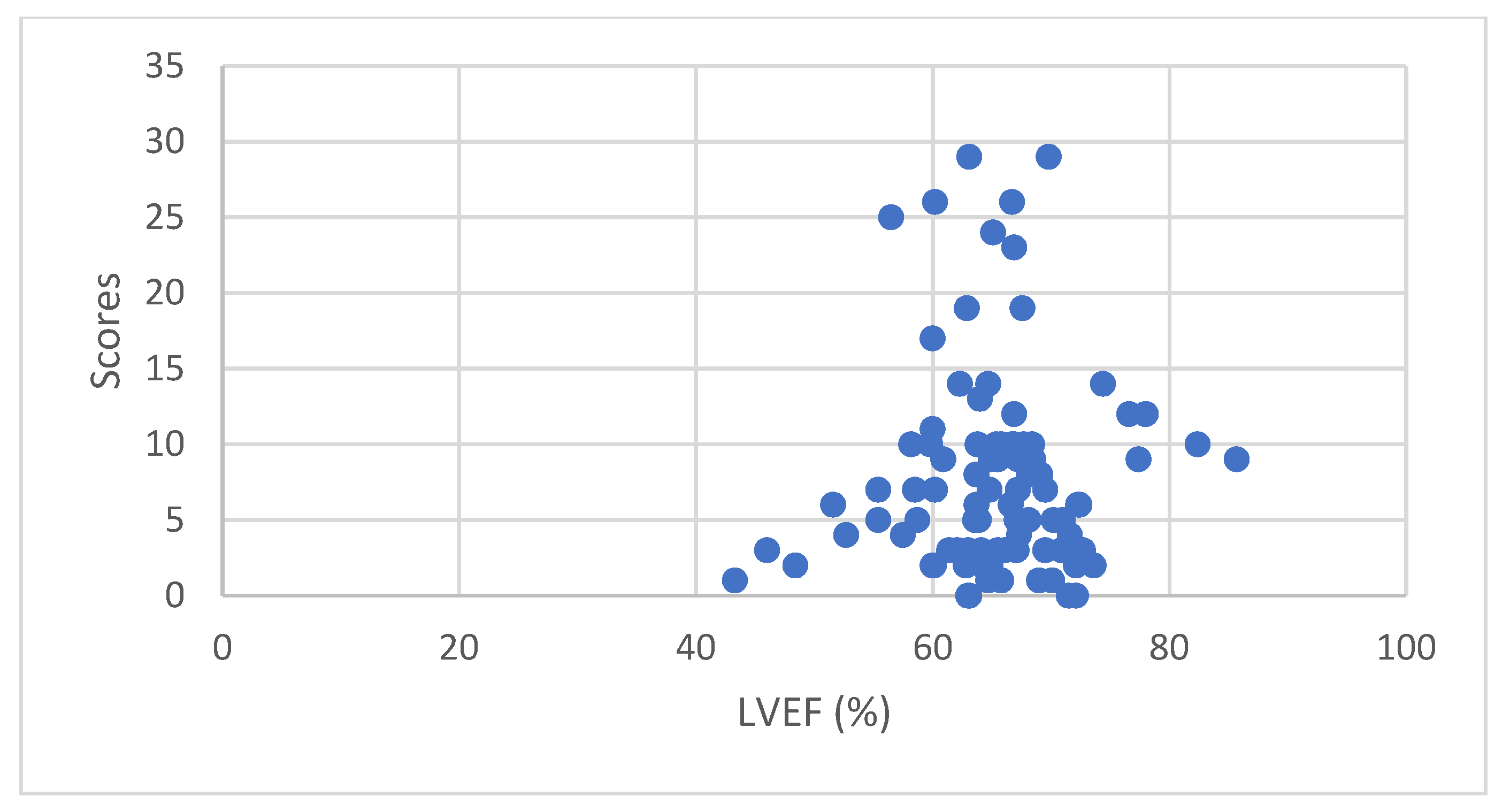
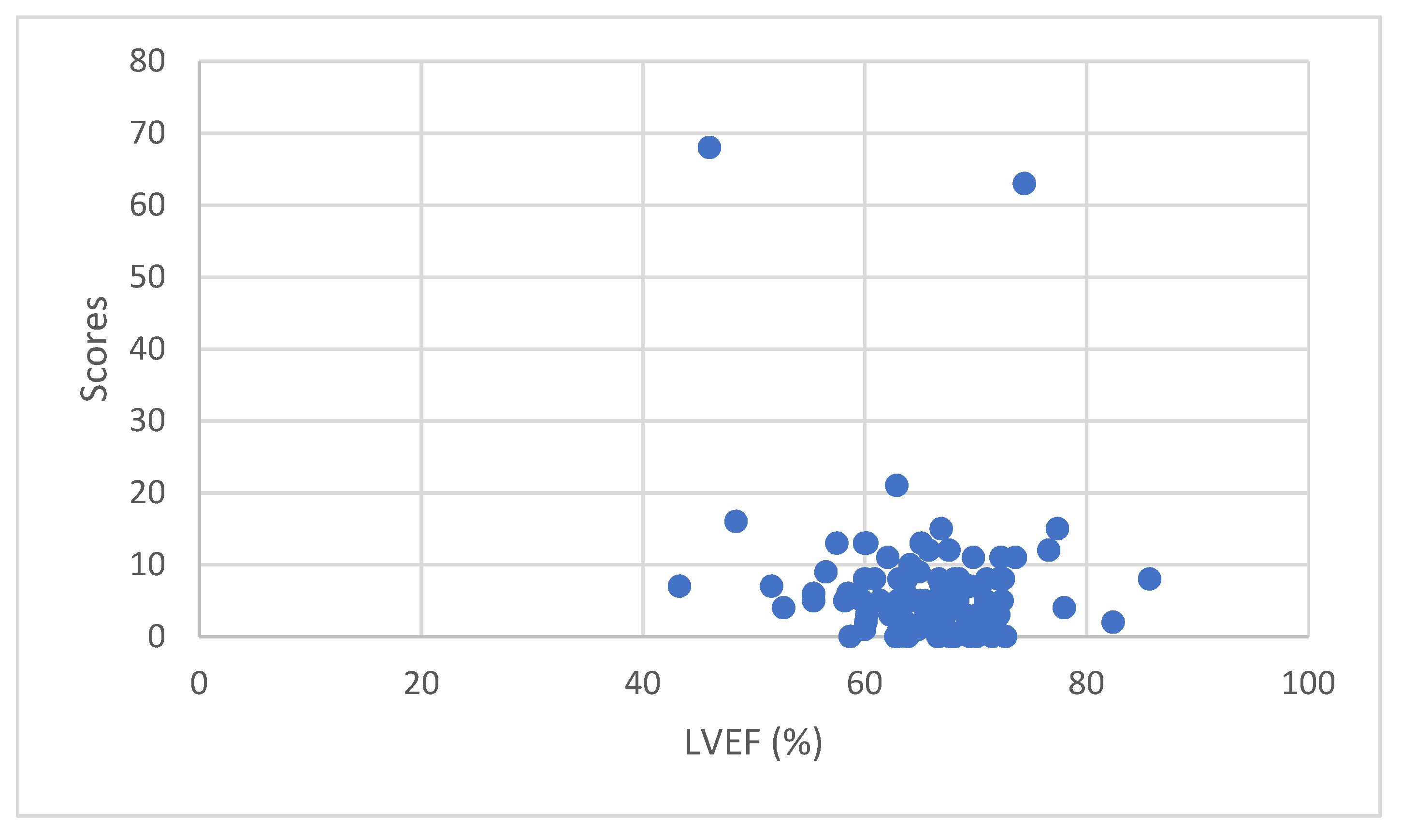
3.4.1. Correlation between LVEF and Isotope Uptake
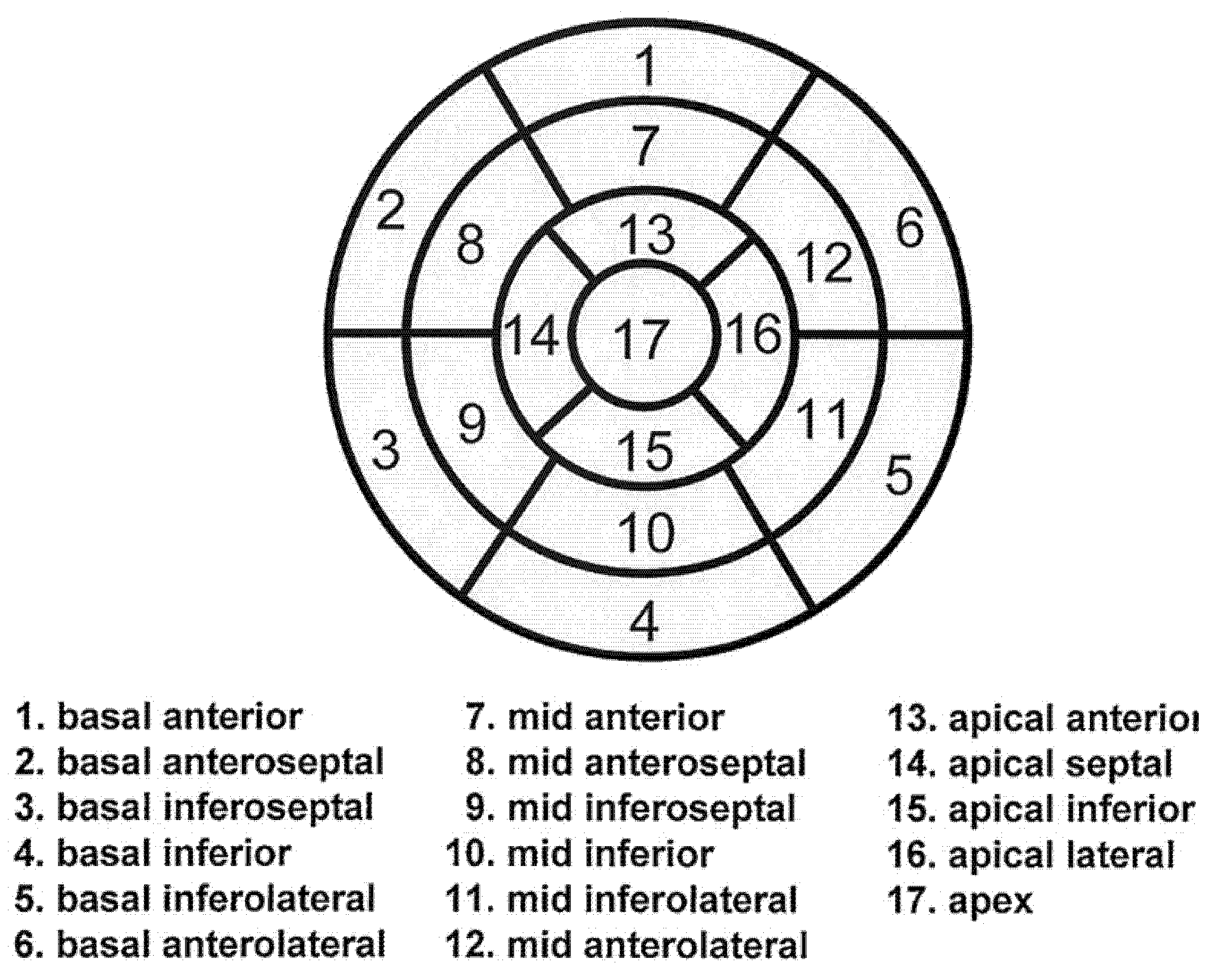
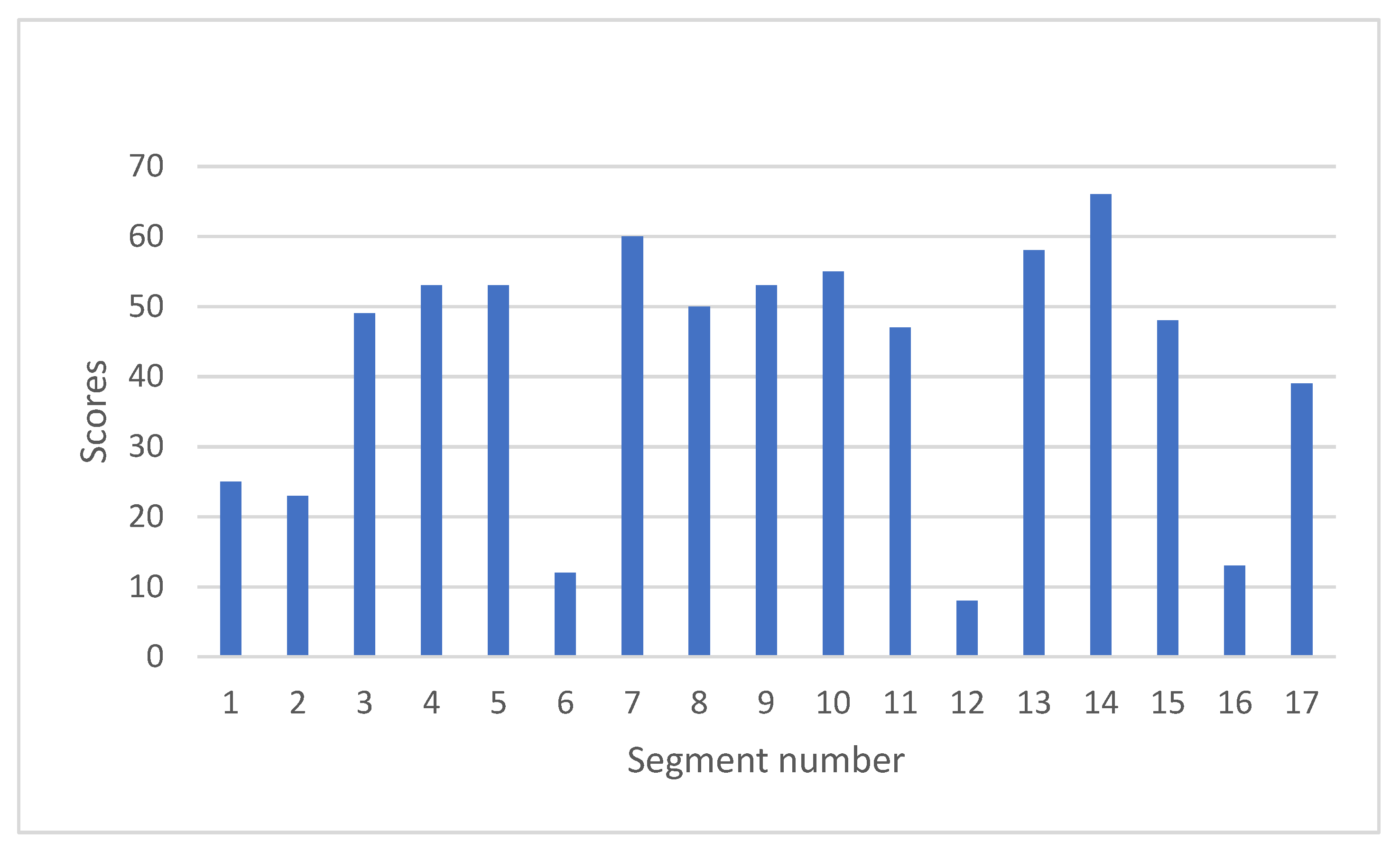
3.4.2. Evaluating the Pattern of 123I-BMIPP Uptake Reduction in Patients’ Hearts
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Breast Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/breast-cancer (accessed on 20 September 2022).
- Zamorano, J.L.; Lancellotti, P.; Munoz, D.R.; Aboyans, V.; Asteggiano, R.; Galderisi, M.; Habib, G.; Lenihan, D.J.; Lip, G.Y.H.; Lyon, A.R.; et al. ESC Scientific Document Group. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 2768–2801. [Google Scholar] [CrossRef] [PubMed]
- Campia, U.; Moslehi, J.J.; Amiri-Kordestani, L.; Barac, A.; Beckman, J.A.; Chism, D.D.; Cohen, P.; Groarke, J.D.; Herrmann, J.; Reilly, C.M.; et al. Cardio-Oncology: Vascular and metabolic perspectives: A scientific statement from the American Heart Association. Circulation 2019, 139, e579–e602. [Google Scholar] [CrossRef] [PubMed]
- Plana, J.C.; Galderisi, M.; Barac, A.; Ewer, M.S.; Ky, B.; Scherrer-Crosbie, M.; Gename, J.; Sebag, I.A.; Agler, D.A.; Badano, L.P.; et al. Expert consensus for multimodality imaging evaluation of adult patients during ad after cancer therapy: A report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 1063–1093. [Google Scholar] [CrossRef]
- De Geus-Oei, L.F.; Mavinkurve-Groothuis, A.M.; Bellersen, L.; Gotthardt, M.; Oyen, W.J.; Kapusta, L.; van Laarhoven, H.W. Scintigraphic techniques for early detection of cancer treatment-induced cardiotoxicity. J. Nucl. Med. Technol. 2013, 41, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Jokar, N.; Amini, A.; Ravanbod, M.; Barekat, M.; Shooli, H.; Gholamrezanezhad, A.; Assadi, M. State-of-the-art modalities in cardio-oncology: Insight from a nuclear medicine approach. Nucl. Med. Rev. 2021, 24, 82–92. [Google Scholar] [CrossRef]
- Takeishi, Y.; Suekawa, H.; Sakurai, T.; Saito, H.; Nishimura, S.; Shibu, T.; Sasaki, Y.; Tomoike, H. Noninvasive identification of anthracycline cardiotoxicity: Comparison of 123 I-MIBG and 123I-BMIPP imaging. Ann. Nucl. Med. 1994, 8, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Garver, P.R.; Wasnich, R.D.; Shibuya, A.M.; Yeh, F. Appearance of breast attenuation artifacts with thallium myocardial SPECT imaging. Clin. Nucl. Med. 1985, 10, 694–696. [Google Scholar] [CrossRef] [PubMed]
- Iwata, K.; Committee of Clinical Practice Guidelines. The Japanese Breast Cancer Society Clinical Practice Guidelines for Breast Cancer 2018; The Japanese Breast Cancer Society: Kanahara-shuppan: Tokyo, Japan, 2018. [Google Scholar]
- Cerqueira, M.D.; Weissman, N.J.; Dilsizian, V.; Jacobs, A.K.; Kaul, S.; Laskey, W.K.; Pennell, D.J.; Rumberger, J.A.; Ryan, T.; Verani, M.S. America Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002, 105, 539–542. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, K.; Okuda, K.; Kawano, S.; Slomka, P.; Germano, G.; Kinuya, S. The importance of population-specific normal database for quantification of myocardial ischemia; comparison between Japanese 360 and 180-degree databases and a US database. J. Nucl. Cardiol. 2009, 16, 422–430. [Google Scholar] [CrossRef]
- Nakajima, K.; Kumita, S.; Ishida, Y.; Momose, M.; Hashimoto, J.; Morita, K.; Taki, J.; Yamashita, S.; Maruno, H.; Ogawa, M.; et al. Creation and characterization of Japanese standards for myocardial perfusion SPECT: Database from the Japanese Society of Nuclear Medicine Working Group. Ann. Nucl. Med. 2007, 21, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Yoshinaga, K.; Matsuki, T.; Hashimoto, A.; Tsukamoto, K.; Nakata, T.; Tamaki, N. Validation of automated quantification of myocardial perfusion and fatty acid metabolism abnormalities on SPECT images. Circ. J. 2011, 75, 2187–2195. [Google Scholar] [CrossRef] [PubMed]
- Dilsizian, V. Challenging nuclear cardiology research: Stimulating discovery, validation, and clinical relevance. J. Nucl. Med. 2018, 59, 13–14. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; Takeda, K.; Okamoto, S.; Okamoto, R.; Makino, K.; Tameda, Y.; Nomura, Y.; Maeda, H.; Ichihara, T.; Nakano, T. Detection of doxorubicin cardiology by using iodine-123 BMIPP early dynamic SPECT: Quantitative evaluation of early abnormality of fatty acid metabolism with the Rutland method. J. Nucl. Cardiol. 2000, 7, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; Takeda, K.; Imanaka-Yoshida, K.; Imai, H.; Sekine, T.; Kamikura, Y. Assessment of fatty acid metabolism in taxan-induced myocardial damage with iodine-123 BMIPP SPECT: Comparative study with myocardial perfusion, left ventricular function, and histopathological findings. Ann. Nucl. Med. 2003, 17, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Nakata, T.; Oka, T.; Ogawa, T.; Okamoto, F.; Kusaka, Y.; Sohmiya, K.; Shimamoto, K.; Itakura, K. Defect in human myocardial long-chain fatty acid uptake is caused by FAT/CD36 mutations. J. Lipid Res. 2001, 42, 751–759. [Google Scholar] [CrossRef]
- Kashiwagi, H.; Tomiyama, Y.; Kosugi, S.; Shiraga, M.; Lipsky, R.H.; Kanayama, Y.; Kurata, Y.; Matsuzawa, Y. Identification of molecular defects in a subject with type 1 CD36 deficiency. Blood 1994, 83, 3545–3552. [Google Scholar] [CrossRef] [PubMed]
- Hirano, K.; Ikeda, Y.; Sugimura, K.; Sakata, Y. Cardiomyocyte steatosis and defective washout of iodine-123-β-methyl iodophenyl-pentadecanoic acid in genetic deficiency of adipose triglyceride lipase. Eur. Heart J. 2015, 36, 580. [Google Scholar] [CrossRef] [PubMed]
- Rosa, G.M.; Gigli, L.; Tagliasacchi, M.I.; Iorio, C.D.; Carbone, F.; Nencioni, A.; Montecucco, F.; Brinelli, C. Update on cardiotoxicity of anti-cancer treatments. Eur. J. Clin. Investig. 2016, 46, 264–284. [Google Scholar] [CrossRef] [PubMed]
- Seraphim, A.; Westwood, A.; Bhuva, A.N.; Crake, T.; Moon, J.C.; Menezes, L.J.; Lloyd, G.; Ghosh, A.K.; Slater, S.; Oakervee, H.; et al. Advanced imaging modalities to monitor for cardiotoxicity. Curr. Treat. Options Oncol. 2019, 20, 73. [Google Scholar] [CrossRef] [PubMed]
- Lyon, A.R.; Lopez-Fernandez, T.; Couch, L.S.; Asteggiano, R.; Aznar, M.C.; Bergler-Klein, J.; Boriani, G.; Cardinale, D.; Cordoba, R.; Cosyns, B.; et al. ESC Scientific Document Group. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur. Heart J. 2022, 23, e333–e465. [Google Scholar] [CrossRef]
| Treatment Therapy | Percentage (%) |
|---|---|
| Trastuzumab | 49 |
| Pertuzumab | 21 |
| Trastuzumab Emtansine (T-DM1) | 13 |
| Epirubicin | 62 |
| Paclitaxel (PTX) | 90 |
| Radiation therapy | 36 |
| Patient | Age | LVEF at Onset (%) | Latest LVEF (%) | Anti-Cancer Drugs 1 |
|---|---|---|---|---|
| Case A | 67 | 46.6 | 59.8 | Epirubicin, PTX |
| Case B | 66 | 48 | 78 | Epirubicin, PTX, Trastuzumab, Pertuzumab, T-DM1 |
| Case C | 76 | 43.3 | 43.3 | Epirubicin, PTX |
| Case D | 72 | 46 | 46 | Epirubicin, PTX, Trastuzumab, Pertuzumab |
| Case E | 78 | 48.4 | 48.4 | PTX, Trastuzumab, T-DM1 |
| Case F | 60 | 51.6 | 51.6 | PTX, Trastuzumab |
| Patient | Age | LVEF at Onset (%) | Latest LVEF (%) | 201Tl Scores 1 | 123I-BMIPP Scores 1 | Anti-Cancer Drugs 2 |
|---|---|---|---|---|---|---|
| Case A | 67 | 46.6 | 59.8 | 10 | 5 | Epirubicin, PTX |
| Case B | 66 | 48 | 78 | 12 | 4 | Epirubicin, PTX, Trastuzumab, Pertuzumab, T-DM1 |
| Case C | 76 | 43.3 | 43.3 | 1 | 7 | Epirubicin, PTX |
| Case D | 72 | 46 | 46 | 3 | 68 | Epirubicin, PTX, Trastuzumab, Pertuzumab |
| Case E | 78 | 48.4 | 48.4 | 2 | 16 | PTX, Trastuzumab, T-DM1 |
| Case F | 60 | 51.6 | 51.6 | 6 | 7 | PTX, Trastuzumab |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harada, Y.; Shimada, K.; Harada, S.J.; Sato, T.; Kubota, Y.; Yamashita, M. Iodine-123 β-methyl-P-iodophenyl-pentadecanoic Acid (123I-BMIPP) Myocardial Scintigraphy for Breast Cancer Patients and Possible Early Signs of Cancer-Therapeutics-Related Cardiac Dysfunction (CTRCD). J. Imaging 2022, 8, 296. https://doi.org/10.3390/jimaging8110296
Harada Y, Shimada K, Harada SJ, Sato T, Kubota Y, Yamashita M. Iodine-123 β-methyl-P-iodophenyl-pentadecanoic Acid (123I-BMIPP) Myocardial Scintigraphy for Breast Cancer Patients and Possible Early Signs of Cancer-Therapeutics-Related Cardiac Dysfunction (CTRCD). Journal of Imaging. 2022; 8(11):296. https://doi.org/10.3390/jimaging8110296
Chicago/Turabian StyleHarada, Yuko, Kyosuke Shimada, Satoshi John Harada, Tomomi Sato, Yukino Kubota, and Miyoko Yamashita. 2022. "Iodine-123 β-methyl-P-iodophenyl-pentadecanoic Acid (123I-BMIPP) Myocardial Scintigraphy for Breast Cancer Patients and Possible Early Signs of Cancer-Therapeutics-Related Cardiac Dysfunction (CTRCD)" Journal of Imaging 8, no. 11: 296. https://doi.org/10.3390/jimaging8110296
APA StyleHarada, Y., Shimada, K., Harada, S. J., Sato, T., Kubota, Y., & Yamashita, M. (2022). Iodine-123 β-methyl-P-iodophenyl-pentadecanoic Acid (123I-BMIPP) Myocardial Scintigraphy for Breast Cancer Patients and Possible Early Signs of Cancer-Therapeutics-Related Cardiac Dysfunction (CTRCD). Journal of Imaging, 8(11), 296. https://doi.org/10.3390/jimaging8110296










