AIDA (Artificial Intelligence Dystocia Algorithm) in Prolonged Dystocic Labor: Focus on Asynclitism Degree
Abstract
1. Introduction
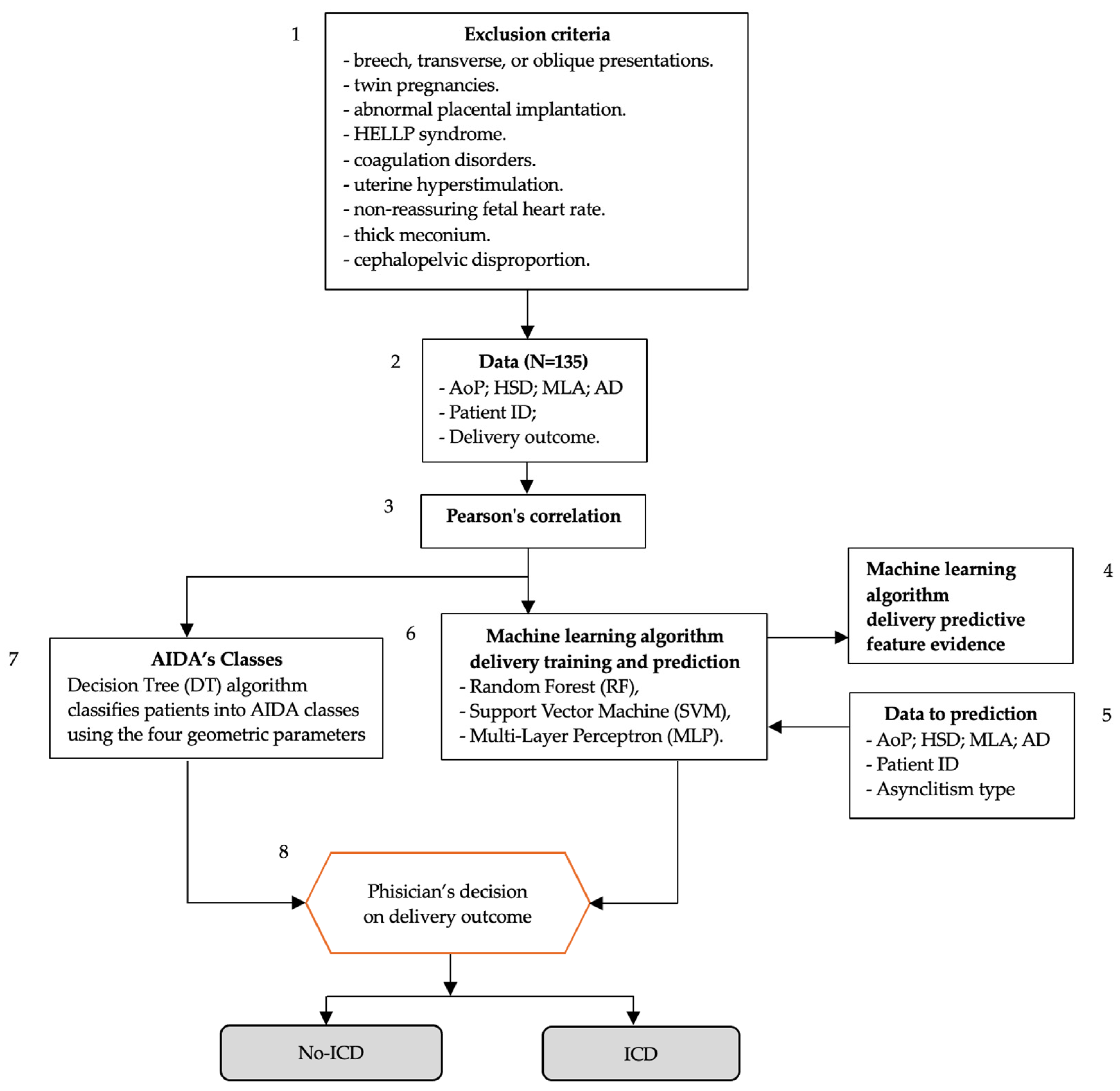
2. Materials and Methods
- (a)
- Correlation analysis: Pearson’s correlation was used to measure the linear relationship between AD and other parameters, verifying their statistical correlation and significance.
- (b)
- Feature importance assessment: the importance of AD as a feature in the three supervised machine learning algorithms applied to the four geometric parameters and physician-determined delivery outcomes was evaluated.
- (c)
- AIDA class definition: The role of AD cutoff values, in conjunction with the other three geometric parameters, in defining AIDA classes was identified. These cutoffs were associated with either intrapartum cesarean delivery (ICD) or non-ICD outcomes.
- (d)
- Delivery outcome and asynclitism type analysis: The role of asynclitism type (anterior or posterior) in delivery outcomes was examined, and potential scenarios physicians might encounter when using AIDA to predict delivery outcomes were highlighted.
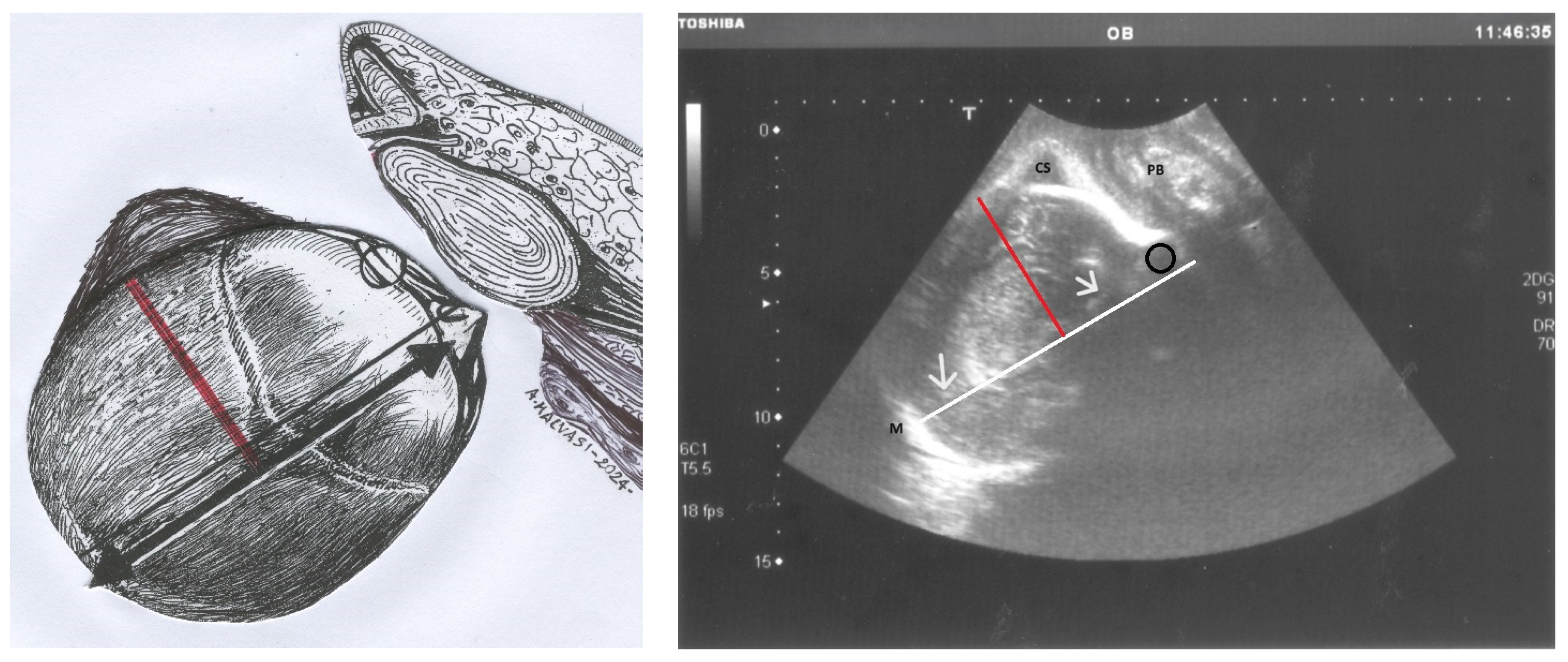
2.1. AD and Pearson’s Correlation
2.2. AD as a Predictive Feature in AIDA Machine Learning Algorithms
2.3. AD and AIDA Classes
2.4. AD and AIDA Machine Learning Algorithm Delivery Prediction
3. Results
3.1. Findings from AD and Pearson’s Correlation
3.2. Findings from AD as a Predictive Feature in AIDA Machine Learning Algorithms
3.3. Findings from AD and AIDA Classes
3.4. Findings from AD and AIDA Machine Learning Algorithm Delivery Prediction
- (a)
- For AIDA class 0, comprising 38 patients with 68 predictions and all four parameters in the green zone, both the random forest (RF) and multi-layer perceptron (MLP) algorithms performed exceptionally well, achieving perfect scores in accuracy, NPV, and specificity, all at 1.0;
- (b)
- In AIDA class 4, which included 18 patients with 31 predictions and all four parameters in the red or yellow zones, the RF and support vector machine (SVM) algorithms demonstrated optimal performance. Both achieved perfect scores in accuracy, PPV, recall, and F1 score, all at 1.0;
- (c)
- For AIDA class 3, consisting of 30 patients with 50 predictions, three parameters in the red or yellow zones, and one parameter in the green zone, the RF algorithm emerged as the top performer. It achieved high accuracy at 0.92, PPV at 0.9167, perfect NPV and recall at 1.0, specificity at 0.3333, and a strong F1 score of 0.9565.
4. Discussion
4.1. Asynclitism, Asynclitism Degree and Other Diagnosis
4.2. Asynclitism Degree, Geometric Dystocia and AIDA
4.3. Highlights from the AIDA2
4.4. Potential Clinical Implications
- Early identification of high-risk cases: accurate prediction of ICD likelihood in AIDA class 4 cases could facilitate timely intervention, potentially reducing the risks associated with prolonged labor.
- Reduction in unnecessary interventions: reliable identification of low-risk cases (AIDA class 0) could help avoid unnecessary cesarean deliveries.
- Personalized labor management: the integration of multiple parameters allows for a more nuanced assessment of individual cases, potentially leading to more tailored management strategies.
- Targeted interventions: understanding the degree of asynclitism could guide the use of specific interventions aimed at promoting fetal head rotation and descent, such as maternal positioning or manual rotation techniques.
- Optimizing the timing of interventions: in cases of severe asynclitism with other unfavorable parameters, earlier decision-making for cesarean delivery could potentially reduce the risks associated with prolonged, unproductive labor.
- Reducing unnecessary interventions: conversely, in cases where AD and other parameters are favorable, clinicians might feel more confident in allowing labor to continue, potentially reducing unnecessary interventions.
- Improved communication: the quantitative nature of the AIDA predictions could facilitate clearer communication between healthcare providers and patients regarding the likelihood of different delivery outcomes.
- Enhanced training: the AIDA method could serve as an educational tool for training obstetricians and midwives in interpreting intrapartum ultrasound findings and assessing labor progress.
4.5. Study Limitations and Future Research Directions
- Standardization of measurement techniques: to ensure reproducibility and comparability of AD measurements across different settings, standardized protocols for intrapartum ultrasonography need to be established and widely adopted.
- Training and education: widespread implementation of AD assessment would require training programs for clinicians to ensure competence in both the technical aspects of measurement and the interpretation of results.
- Technology integration: the successful implementation of AI-assisted tools like AIDA will depend on their seamless integration into existing clinical workflows and electronic health record systems.
- Validation in diverse populations: While this study provides valuable insights, larger-scale studies across diverse patient populations are needed to validate the predictive value of AD and refine the AIDA algorithm.
- Ethical considerations: as with any AI-assisted decision support tool, careful consideration must be given to issues of transparency, accountability, and the potential for algorithmic bias.
- Large-scale, prospective validation studies across diverse healthcare settings and patient populations.
- Investigation of the AIDA method’s performance in different clinical scenarios, including multiparous women and labors of shorter duration.
- Integration of additional clinical parameters (e.g., maternal characteristics, labor progress metrics, and maternal and fetal complications) to potentially enhance the predictive accuracy of the algorithm.
- Evaluation of the impact of AIDA implementation on clinical outcomes, including cesarean delivery rates, maternal and neonatal morbidity, and patient satisfaction.
- Cost-effectiveness analyses to assess the economic implications of implementing the AIDA method in routine clinical practice.
- Exploration of the potential role of the AIDA method in reducing healthcare disparities by providing more objective assessment tools.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barbera, A.F. Intrapartum Sonography Dystocia, from Diagnosis to Operative Delivery: Use of the Right Tool at the Right Time. Intrapartum Ultrason. Labor Manag. Labor Deliv. Puerperium 2021, 347–358. Available online: https://link.springer.com/chapter/10.1007/978-3-030-57595-3_30 (accessed on 31 May 2024).
- Hung, C.M.; Chan, V.Y.; Ghi, T.; Lau, W. Asynclitism in the second stage of labor: Prevalence, associations, and outcome. Am. J. Obstet. Gynecol. MFM 2021, 3, 100437. [Google Scholar] [CrossRef] [PubMed]
- Akmal, S.; Paterson–Brown, S. Malpositions and malpresentations of the foetal head. Obstet. Gynaecol. Reprod. Med. 2009, 19, 240–246. [Google Scholar] [CrossRef]
- Malvasi, A.; Barbera, A.; Di Vagno, G.; Gimovsky, A.; Berghella, V.; Ghi, T.; Di Renzo, G.C.; Tinelli, A. Asynclitism: A literature review of an often forgotten clinical condition. J. Matern. Fetal. Neonatal Med. 2015, 28, 1890–1894. [Google Scholar] [CrossRef] [PubMed]
- Buchmann, E.J.; Libhaber, E. Sagittal suture overlap in cephalopelvic disproportion: Blinded and non-participant assessment. Acta Obstet. Gynecol. Scand. 2008, 87, 731–737. [Google Scholar] [CrossRef]
- Malvasi, A.; Vinciguerra, M.; Lamanna, B.; Cascardi, E.; Damiani, G.R.; Muzzupapa, G.; Kosmas, I.; Beck, R.; Falagario, M.; Vimercati, A.; et al. Asynclitism and Its Ultrasonographic Rediscovery in Labor Room to Date: A Systematic Review. Diagnostics 2022, 12, 2998. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Tinelli, A.; Barbera, A.; Eggebø, T.; Mynbaev, O.; Bochicchio, M.; Pacella, E.; Di Renzo, G. Occiput posterior position diagnosis: Vaginal examination or intrapartum sonography? A clinical review. J. Matern. Fetal. Neonatal Med. 2014, 27, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Chan, V.Y.T.; Lau, W.L. Intrapartum ultrasound and the choice between assisted vaginal and cesarean delivery. Am. J. Obstet. Gynecol. MFM 2021, 3, 100439. [Google Scholar] [CrossRef] [PubMed]
- Bellussi, F.; Ghi, T.; Youssef, A.; Salsi, G.; Giorgetta, F.; Parma, D.; Simonazzi, G.; Pilu, G. The use of intrapartum ultrasound to diagnose malpositions and cephalic malpresentations. Am. J. Obstet. Gynecol. 2017, 217, 633–641. [Google Scholar] [CrossRef]
- Malvasi, A.; Stark, M.; Ghi, T.; Farine, D.; Guido, M.; Tinelli, A. Intrapartum sonography for fetal head asynclitism and transverse position: Sonographic signs and comparison of diagnostic performance between transvaginal and digital examination. J. Matern. Neonatal Med. 2011, 25, 508–512. Available online: https://www.tandfonline.com/doi/abs/10.3109/14767058.2011.648234 (accessed on 31 May 2024). [CrossRef]
- Malvasi, A.; Giacci, F.; Gustapane, S.; Sparic, R.; Barbera, A.; Tinelli, A. Intrapartum sonographic signs: New diagnostic tools in malposition and malrotation. J. Matern. Neonatal Med. 2015, 29, 2408–2413. Available online: https://www.tandfonline.com/doi/abs/10.3109/14767058.2015.1092137 (accessed on 31 May 2024). [CrossRef] [PubMed]
- Vlasyuk, V. Compression-hypoxic birth injuries and skull configuration. Arkhiv Patol. 2021, 83, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Malgieri, L.E.; Cicinelli, E.; Vimercati, A.; D’amato, A.; Dellino, M.; Trojano, G.; Difonzo, T.; Beck, R.; Tinelli, A. Artificial Intelligence, Intrapartum Ultrasound and Dystocic Delivery: AIDA (Artificial Intelligence Dystocia Algorithm), a Promising Helping Decision Support System. J. Imaging 2024, 10, 107. [Google Scholar] [CrossRef] [PubMed]
- Beck, R.; Malvasi, A.; Kuczkowski, K.M.; Marinelli, E.; Zaami, S. Intrapartum sonography of fetal head in second stage of labor with neuraxial analgesia: A literature review and possible medicolegal aftermath. Eur. Rev. Med. Pharmacol. Sci. 2021, 23, 3159–3166. Available online: https://iris.uniroma1.it/handle/11573/1477762 (accessed on 31 May 2024).
- Operative Vaginal Birth: ACOG Practice Bulletin, Number 219. Obstet Gynecol. 2020, 135, e149–e159. [CrossRef]
- Bonet, M.; Ciabati, L.; De Oliveira, L.; Souza, R.; Browne, J.; Rijken, M.; Fawcus, S.; Hofmeyr, G.; Liabsuetrakul, T.; Gülümser, Ç.; et al. Constructing evidence-based clinical intrapartum care algorithms for decision-support tools. BJOG Int. J. Obstet. Gynaecol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Usman, S.; Hanidu, A.; Kovalenko, M.; Hassan, W.A.; Lees, C. The sonopartogram. Am. J. Obstet. Gynecol. 2023, 228, S997–S1016. [Google Scholar] [CrossRef]
- Skinner, S.M.; Giles-Clark, H.J.; Higgins, C.; Mol, B.W.; Rolnik, D.L. Prognostic accuracy of ultrasound measures of fetal head descent to predict outcome of operative vaginal birth: A comparative systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2023, 229, 10–22.e10. [Google Scholar] [CrossRef]
- Bofill, J.A.; Rust, O.A.; Schorr, S.J.; Brown, R.C.; Martin, R.W.; Martin, J.N., Jr.; Morrison, J.C. A randomized prospective trial of the obstetric forceps versus the M-cup vacuum extractor. Am. J. Obstet. Gynecol. 1996, 175, 1325–1330. [Google Scholar] [CrossRef]
- Vlasyuk, V. Fetal and Neonatal Trauma in Dystocic Labor and Delivery. Intrapartum Ultrasonography for Labor Management: Labor, Delivery and Puerperium [Internet]. 4 January 2021, pp. 715–726. Available online: https://link.springer.com/chapter/10.1007/978-3-030-57595-3_56 (accessed on 31 May 2024).
- Ghi, T.; Youssef, A.; Pilu, G.; Malvasi, A.; Ragusa, A. Intrapartum sonographic imaging of fetal head asynclitism. Ultrasound Obstet. Gynecol. 2012, 39, 238–240. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/uog.9034 (accessed on 31 May 2024). [CrossRef]
- Malvasi, A.; Tinelli, A.; Stark, M. Intrapartum sonography sign for occiput posterior asynclitism diagnosis. J. Matern. Neonatal Med. 2011, 24, 553–554. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Tinelli, A. The smartphone use during intrapartum ultrasound: A useful tool to diagnose the persistent asynclitism and occiput posterior position before and during birth. J. Matern.-Fetal Neonatal Med. 2016, 29, 3488–3489. [Google Scholar] [CrossRef] [PubMed]
- Ghi, T.; Dall’asta, A. Sonographic evaluation of the fetal head position and attitude during labor. Am. J. Obstet. Gynecol. 2024, 230, S890–S900. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Tinelli, A.; Brizzi, A.; Guido, M.; Laterza, F.; De Nunzio, G.; Bochicchio, M.; Ghi, T.; Stark, M.; Benhamou, D.; et al. Intrapartum sonography head transverse and asynclitic diagnosis with and without epidural analgesia initiated early during the first stage of labor. Eur. Rev. Med. Pharmacol. Sci. 2011, 15, 518–523, Erratum in: Eur. Rev. Med. Pharmacol. Sci. 2011, 15, 1428. [Google Scholar] [PubMed]
- Gustapane, S.; Malvasi, A.; Tinelli, A. The use of intrapartum ultrasound to diagnose malpositions and cephalic malpresentations. Am. J. Obstet. Gynecol. 2018, 218, 540–541. Available online: http://www.ajog.org/article/S0002937818300772/fulltext (accessed on 31 May 2024). [CrossRef]
- Gimovsky, A.C. Intrapartum ultrasound for the diagnosis of cephalic malpositions and malpresentations. Am. J. Obstet. Gynecol. MFM 2021, 3, 100438. [Google Scholar] [CrossRef]
- Malvasi, A.; Gustapane, S.; Malvasi, M.; Vinciguerra, M.; Tinelli, A.; Beck, R. Semeiotics of Intrapartum Ultrasonography: New Diagnostic Sonographic Sign of Fetal Malpositions and Malrotations. Intrapartum Ultrason. Labor Manag. Labor Deliv. Puerperium 2021, 251–273. Available online: https://link.springer.com/chapter/10.1007/978-3-030-57595-3_22 (accessed on 2 June 2024).
- Ghi, T.; Bellussi, F.; Pilu, G. Sonographic diagnosis of lateral asynclitism: A new subtype of fetal head malposition as a main determinant of early labor arrest. Ultrasound Obstet. Gynecol. 2014, 45, 229–231. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/uog.13385 (accessed on 2 June 2024). [CrossRef] [PubMed]
- Malvasi, A.; Barbera, A.; Ghi, T.; Tinelli, A. Lateral asynclitism: Introduction of a new terminolgy associated to specific fetal position of the fetal head diagnosed by ultrasound in the second stage of labor. J. Matern. Neonatal Med. 2014, 28, 1839–1841. Available online: https://www.tandfonline.com/doi/abs/10.3109/14767058.2014.969237 (accessed on 2 June 2024). [CrossRef]
- Malvasi, A.; Di Renzo, G.C.; Tinelli, A. Is twisted head position lateral asynclitism in the first stage of labor? Ultrasound Obstet. Gynecol. 2014, 46, 251–252. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/uog.14747 (accessed on 2 June 2024). [CrossRef]
- Blayney, M.P. Asynclitism—A cause of prolonged labour in African multiparae. East Afr. Med. J. 1989, 66, 280–284. [Google Scholar] [PubMed]
- Tinelli, A.; Di Renzo, G.C.; Malvasi, A. The intrapartum ultrasonographic detection of the Bandl ring as a marker of dystocia. Int. J. Gynecol. Obstet. 2015, 131, 310–311. Available online: https://pubmed.ncbi.nlm.nih.gov/26384791/ (accessed on 2 June 2024). [CrossRef] [PubMed]
- Malvasi, A.; Vimercati, A.; Ricci, I.; Picardi, N.; Cicinelli, E.; Kosmas, I.; Baldini, G.M.; Tinelli, A. Dystocic Labor and Adrenergic and Noradrenergic Neurotransmitters: A Morphological Experimental Study. Int. J. Mol. Sci. 2022, 23, 11379. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Cicinelli, E.; Baldini, G.M.; Vimercati, A.; Beck, R.; Dellino, M.; Damiani, G.R.; Cazzato, G.; Cascardi, E.; Tinelli, A. Prolonged Dystocic Labor in Neuraxial Analgesia and the Role of Enkephalin Neurotransmitters: An Experimental Study. Int. J. Mol. Sci. 2023, 24, 3767. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Ballini, A.; Tinelli, A.; Fioretti, B.; Vimercati, A.; Gliozheni, E.; Baldini, G.M.; Cascardi, E.; Dellino, M.; Bonetti, M.; et al. Oxytocin augmentation and neurotransmitters in prolonged delivery: An experimental appraisal. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2024, 21, 100273. [Google Scholar] [CrossRef] [PubMed]
- Hinkson, L.; Henrich, W.; Tutschek, B. Intrapartum ultrasound during rotational forceps delivery: A novel tool for safety, quality control, and teaching. Am. J. Obstet. Gynecol. 2020, 224, 93.e1–93.e7. [Google Scholar] [CrossRef]
- Malvasi, A.; Tinelli, A. Intrapartum sonography: Two sings to detect asynclitism degree. J. Matern. Neonatal Med. 2016, 29, 1289–1290. [Google Scholar] [CrossRef]
- Birol Ilter, P.; Yassa, M.; Timur, H.; Dogan, O.; Tekin, A.B.; Haydar, A.; Gulumser, C.; Tug, N.; Malvasi, A.; Tinelli, A. Intrapartum ultrasound for fetal head asynclitism: Is it possible to establish a degree of asynclitism to correlate to delivery outcome? Int. J. Gynecol. Obstet. 2023, 163, 271–276. [Google Scholar] [CrossRef]
- Vlasyuk, V.; Malvasi, A. The importance of asynclitism in birth trauma and intrapartum sonography. J. Matern. Neonatal Med. 2022, 35, 2188–2194. Available online: https://www.tandfonline.com/doi/abs/10.1080/14767058.2020.1777270 (accessed on 2 June 2024). [CrossRef]
- Ghi, T.; Eggebø, T.; Lees, C.; Kalache, K.; Rozenberg, P.; Youssef, A.; Salomon, L.J.; Tutschek, B. ISUOG Practice Guidelines: Intrapartum ultrasound. Ultrasound Obstet. Gynecol. 2018, 52, 128–139. [Google Scholar] [CrossRef]
- Ahn, K.H.; Oh, M.-J. Intrapartum ultrasound: A useful method for evaluating labor progress and predicting operative vaginal delivery. Obstet. Gynecol. Sci. 2014, 57, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Bofill, J.A.; Rust, O.A.; Devidas, M.; Roberts, W.E.; Morrison, J.C.; Martin, J.N. Neonatal cephalohematoma from vacuum extraction. J. Reprod. Med. 1997, 42, 565–569. [Google Scholar]
- Malvasi, A.; Damiani, G.R.; Edoardo, D.N.; Vitagliano, A.; Dellino, M.; Achiron, R.; Ioannis, K.; Vimercati, A.; Gaetani, M.; Cicinelli, E.; et al. Intrapartum ultrasound and mother acceptance: A study with informed consent and questionnaire. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2023, 20, 100246. [Google Scholar] [CrossRef] [PubMed]
- Habek, D.; Orešković, N.; Mikelin, N.; Vulić, L. Internal manual rotation in intrapartal arrest of fetal head engagement. Eur. J. Obstet. Gynecol. Reprod. Biol. 2024, 292, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Raimondo, P.; Beck, R.; Tinelli, A.; Kuczkowski, K.M. Intrapartum ultrasound monitoring of malposition and malrotation during labor neuraxial analgesia: Maternal outcomes. J. Matern. Neonatal Med. 2020, 33, 3584–3590. Available online: https://www.tandfonline.com/doi/abs/10.1080/14767058.2019.1579193 (accessed on 2 June 2024). [CrossRef] [PubMed]
- Jung, J.E.; Lee, Y.J. Intrapartum transperineal ultrasound: Angle of progression to evaluate and predict the mode of delivery and labor progression. Obstet. Gynecol. Sci. 2024, 67, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Malvasi, A.; Marinelli, E.; Ghi, T.; Zaami, S. ISUOG Practice Guidelines for intrapartum ultrasound: Application in obstetric practice and medicolegal issues. Ultrasound Obstet. Gynecol. 2021, 54, 421. Available online: https://iris.uniroma1.it/handle/11573/1477683 (accessed on 3 June 2024). [CrossRef] [PubMed]
- Malvasi, A.; Montanari Vergallo, G.; Tinelli, A.; Marinelli, E. “Can the intrapartum ultrasonography reduce the legal liability in distocic labor and delivery?”. J. Matern. Neonatal Med. 2017, 31, 1108–1109. Available online: https://www.tandfonline.com/doi/abs/10.1080/14767058.2017.1306514 (accessed on 3 June 2024). [CrossRef]
- Malgieri, L.E. Ontologies, Machine Learning and Deep Learning in Obstetrics. Pract. Guide Simul. Deliv. Room Emergencies 2023, 29–64. Available online: https://link.springer.com/chapter/10.1007/978-3-031-10067-3_3 (accessed on 2 June 2024).
- Eggebø, T.M.; Hjartardottir, H. Descent of the presenting part assessed with ultrasound. Am. J. Obstet. Gynecol. 2024, 230, S901–S912. [Google Scholar] [CrossRef]

| Characteristic | Mean | Standard Deviation |
|---|---|---|
| Age (years) | 31.62 | 5.28 |
| Gestational age (weeks) | 40.16 | 1.02 |
| Gestational age (days) | 283.09 | 7.15 |
| BMI | 27.52 | 2.95 |
| Neonatal weight (grams) | 3926.68 | 309.66 |
| Apgar Score (1 min) | 6.65 | 1.22 |
| Apgar Score (5 min) | 8.74 | 1.12 |
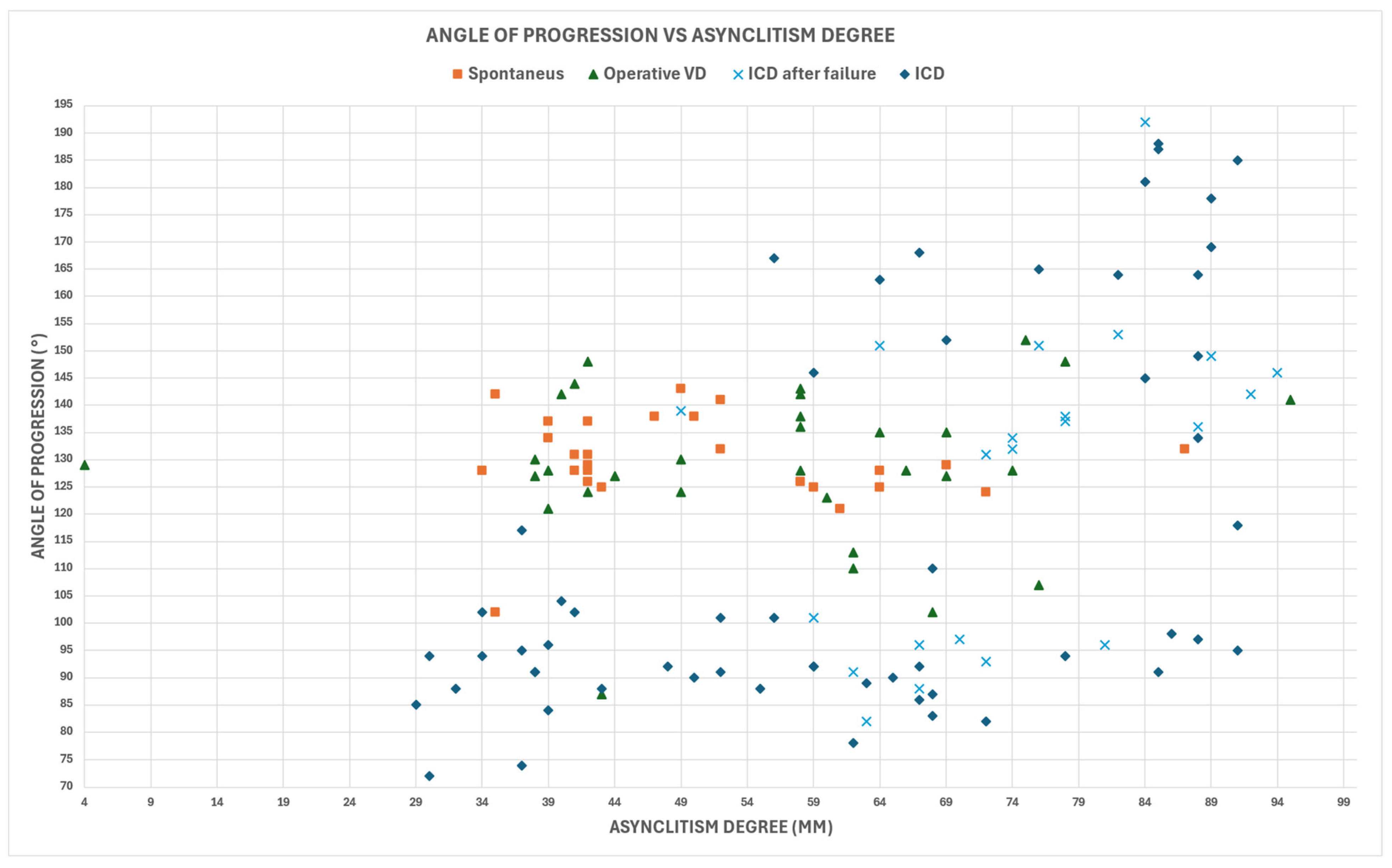
| Characteristic | Minimum | Maximum | Mean | Standard Deviation |
|---|---|---|---|---|
| Head-Symphysis Distance (HSD) (mm) | 10 | 51 | 21.47 | 9.265 |
| Asynclitism Degree (AD) (mm) | 4 | 95 | 60.18 | 18.866 |
| Midline Angle (MLA) (°) | 26 | 90 | 62.59 | 14.986 |
| Angle of Progression (AoP) (°) | 72 | 192 | 122.75 | 27.454 |
| Pearson’s Correlations | PC | p | ||
|---|---|---|---|---|
| Apgar Score at 1 min. | Apgar Score at 5 min. | 0.8 | very strong | 8.42 × 10−32 |
| Angle of Progression | Asynclitism Degree | 0.36 | weak | 0.00002 |
| Head-Symphysis Distance | Asynclitism Degree | 0.18 | very weak | 0.03 |
| Midline angle | Asynclitism Degree | 0.14 | very weak | 0.09 |
| Apgar Score at 1 min. | Asynclitism Degree | −0.2 | weak | 0.02 |
| Apgar Score at 5 min. | Asynclitism Degree | −0.19 | very weak | 0.02 |
| ALGORITHM | AD |
|---|---|
| MLP | fourth |
| Random Forest | third |
| SVM | second |
| XGBoost | second |
| Logistic Regression | fourth |
| Decision Tree | third |
| AoP (°) | AD (mm) | HSD (mm) | |
|---|---|---|---|
| AD–AoP | <101.5 | ≥67 | |
| ≥144.5 | |||
| AD–HSD | ≥70.5 | ≥19.5 | |
| AD–MLA | ≥65.5 |
| AIDA CLASS | Algorithms | Accuracy | PPV | NPV | Recall | Specificity | F1 Score | TP | FP | FN | TN |
|---|---|---|---|---|---|---|---|---|---|---|---|
| CLASS 0 | RF | 1 | NA | 1 | NA | 1 | NA | 0 | 0 | 0 | 68 |
| SVM | 0.9853 | 0.00 | 1 | NA | 0.9853 | NA | 0 | 1 | 0 | 67 | |
| MLP | 1 | NA | 1 | NA | 1 | NA | 0 | 0 | 0 | 68 | |
| CLASS 3 | RF | 0.920 | 0.9167 | 1 | 1 | 0.3333 | 0.9565 | 44 | 4 | 0 | 2 |
| SVM | 0.880 | 0.880 | NA | 1 | 0.00 | 0.9362 | 44 | 6 | 0 | 0 | |
| MLP | 0.780 | 0.8667 | 0.00 | 0.8864 | 0.00 | 0.8764 | 39 | 6 | 5 | 0 | |
| CLASS 4 | RF | 1 | 1 | NA | 1 | NA | 1 | 31 | 0 | 0 | 0 |
| SVM | 1 | 1 | NA | 1 | NA | 1 | 31 | 0 | 0 | 0 | |
| MLP | 0.9677 | 1 | 0.00 | 0.9677 | NA | 0.9836 | 30 | 0 | 1 | 0 |
| Number of Predictions | ID Patient | Delivery Outcome | AIDA AD | AIDA AoP | AIDA MLA | AIDA SPD | Predicted Outcome (SVM) | Predicted Outcome (RF) | Predicted Outcome (MLP) |
|---|---|---|---|---|---|---|---|---|---|
| Anterior Asynclitism | |||||||||
| 2 | 26 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 29 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 110 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 2 | 115 | NOICD | RED | RED | RED | GREEN | ICD | NOICD | ICD |
| 1 | 127 | ICD | YELLOW | RED | GREEN | RED | ICD | ICD | ICD |
| 2 | 127 | ICD | YELLOW | RED | GREEN | RED | ICD | ICD | NOICD |
| Posterior Asynclitism | |||||||||
| 1 | 12 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 1 | 28 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 1 | 33 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 3 | 39 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 1 | 42 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 44 | ICD | GREEN | RED | YELLOW | RED | ICD | ICD | ICD |
| 1 | 50 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 51 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 63 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 77 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 1 | 96 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 3 | 7 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 20 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 24 | NOICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 43 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 1 | 46 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 2 | 118 | ICD | GREEN | RED | RED | RED | ICD | ICD | ICD |
| 1 | 59 | ICD | RED | RED | GREEN | RED | ICD | ICD | ICD |
| 1 | 88 | ICD | RED | RED | GREEN | RED | ICD | ICD | ICD |
| 1 | 99 | ICD | RED | GREEN | RED | RED | ICD | ICD | ICD |
| 2 | 100 | NOICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 1 | 126 | ICD | RED | RED | RED | GREEN | ICD | ICD | ICD |
| 1 | 135 | ICD | RED | RED | RED | GREEN | ICD | ICD | NOICD |
| 1 | 124 | ICD | YELLOW | RED | GREEN | RED | ICD | ICD | ICD |
| 2 | 38 | ICD | YELLOW | RED | GREEN | RED | ICD | ICD | NOICD |
| Number of Predictions | ID Patient | Delivery Outcome | AIDA AD | AIDA AoP | AIDA MLA | AIDA SPD | Predicted Outcome (SVM) | Predicted Outcome (RF) | Predicted Outcome (MLP) |
|---|---|---|---|---|---|---|---|---|---|
| Anterior Asynclitism | |||||||||
| 3 | 3 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 17 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 21 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 23 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 30 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 35 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 3 | 37 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 40 | NOICD | GREEN | GREEN | GREEN | GREEN | ICD | NOICD | NOICD |
| 1 | 45 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 3 | 48 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 3 | 87 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 105 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 109 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 125 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 6 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 14 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 19 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 41 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 3 | 62 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 75 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 95 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 103 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 134 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| Posterior Asynclitism | |||||||||
| 1 | 1 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 3 | 5 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 27 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 3 | 49 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 56 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 3 | 80 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 108 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 3 | 130 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 16 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 31 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 54 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 81 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 2 | 89 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 90 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| 1 | 132 | NOICD | GREEN | GREEN | GREEN | GREEN | NOICD | NOICD | NOICD |
| Number of Predictions | ID Patient | Delivery Outcome | AIDA AD | AIDA AoP | AIDA MLA | AIDA SPD | Predicted Outcome (SVM) | Predicted Outcome (RF) | Predicted Outcome (MLP) |
|---|---|---|---|---|---|---|---|---|---|
| Anterior Asynclitism | |||||||||
| 1 | 74 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 2 | 83 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 1 | 2 | ICD | YELLOW | RED | YELLOW | RED | ICD | ICD | ICD |
| 3 | 4 | ICD | YELLOW | RED | RED | RED | ICD | ICD | ICD |
| 4 | 22 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 1 | 67 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 1 | 121 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| Posterior Asynclitism | |||||||||
| 1 | 102 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 3 | 60 | ICD | YELLOW | RED | RED | RED | ICD | ICD | ICD |
| 2 | 69 | ICD | YELLOW | RED | RED | RED | ICD | ICD | ICD |
| 1 | 84 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 1 | 85 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 1 | 93 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 3 | 117 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 3 | 18 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 1 | 71 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
| 1 | 78 | ICD | RED | RED | RED | RED | ICD | ICD | NOICD |
| 1 | 114 | ICD | RED | RED | RED | RED | ICD | ICD | ICD |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malvasi, A.; Malgieri, L.E.; Cicinelli, E.; Vimercati, A.; Achiron, R.; Sparić, R.; D’Amato, A.; Baldini, G.M.; Dellino, M.; Trojano, G.; et al. AIDA (Artificial Intelligence Dystocia Algorithm) in Prolonged Dystocic Labor: Focus on Asynclitism Degree. J. Imaging 2024, 10, 194. https://doi.org/10.3390/jimaging10080194
Malvasi A, Malgieri LE, Cicinelli E, Vimercati A, Achiron R, Sparić R, D’Amato A, Baldini GM, Dellino M, Trojano G, et al. AIDA (Artificial Intelligence Dystocia Algorithm) in Prolonged Dystocic Labor: Focus on Asynclitism Degree. Journal of Imaging. 2024; 10(8):194. https://doi.org/10.3390/jimaging10080194
Chicago/Turabian StyleMalvasi, Antonio, Lorenzo E. Malgieri, Ettore Cicinelli, Antonella Vimercati, Reuven Achiron, Radmila Sparić, Antonio D’Amato, Giorgio Maria Baldini, Miriam Dellino, Giuseppe Trojano, and et al. 2024. "AIDA (Artificial Intelligence Dystocia Algorithm) in Prolonged Dystocic Labor: Focus on Asynclitism Degree" Journal of Imaging 10, no. 8: 194. https://doi.org/10.3390/jimaging10080194
APA StyleMalvasi, A., Malgieri, L. E., Cicinelli, E., Vimercati, A., Achiron, R., Sparić, R., D’Amato, A., Baldini, G. M., Dellino, M., Trojano, G., Beck, R., Difonzo, T., & Tinelli, A. (2024). AIDA (Artificial Intelligence Dystocia Algorithm) in Prolonged Dystocic Labor: Focus on Asynclitism Degree. Journal of Imaging, 10(8), 194. https://doi.org/10.3390/jimaging10080194










